Abstract
Background:
Heterotopic gastric tissue can be found in the entire gastrointestinal tract. It is usually located in the upper intestine. Rarely, it can be found in the gallbladder. This study describes several clinically, imaging features as well as histopathology findings of heterotopic gastric tissue in gallbladder (HGM).
Methods:
The radiologic database of 1 tertiary university hospital was retrospectively screened for HGM. Additionally, a systemic review of the Medline database was conducted to identify previously published cases reports. In all cases clinical, imaging as well as histopathology features were retrieved from the papers.
Results:
In our databases, 1 patient with HGM was identified. Additionally, the systemic review yielded 32 suitable papers with 34 patients. Clinically, most of the patients suffered from abdominal discomfort. Most of the lesions were located in the lower gallbladder, especially (n = 14, 40%) in the gallbladder neck. On sonography, in 20.7% a broad-based mass was described. In 10.3% a sessile polyp was identified. In 5 cases, the mass was characterized as hyperechoic (55.5%), as isoechoic in 3 (33.3%) cases, and hypoechoic in 1 (11.1%). On computed tomography (CT), the lesions were most frequently hyperdense and all of them showed a slightly enhancement after application of contrast medium. On histopathology, most cases revealed heterotopic gastric mucosa of body-fundic type (60%) with chief and parietal cells, followed by pyloric type glands (20%). Every patient was treated with cholecystectomy and all had an uneventful recovery.
Conclusion:
HGM is a rare disorder with several differential diagnoses. Typically features were described to identify HGM in clinical routine and rule out malignant diseases like gallbladder carcinoma.
Keywords: gallbladder mass, heterotopic gastric mucosa, sonography, ultrasound
1. Introduction
1.1. Case report
During a vascular surgery visit, the 63-year-old patient with a strong cachexia without abdominal discomfort attracted attention. In terms of laboratory chemistry, only slightly increased cholestasis parameters were noticeable. (Aspartate aminotransferase [ASAT] 0.8 μkat/L, alanine aminotransferase [ALAT] 0.7 μkat/L, alkaline phosphatase [AP] 3.6 μkat/L, gamma-glutamyltransferase [GT] 6.7 μkat/L). A staging examination of the thorax and abdomen was carried out on suspicion of a consuming disease by means of computed tomography (CT). This showed a space requirement at the gallbladder infundibulum (hyperdens to gallbladder, isodens to liver, inhomogeneous low contrast medium uptake; 2.8 × 1.6 × 0.5 cm) and ovary masses on both sides. In sonography the mass was isoechoic and there were dilated bile ducts and Ductus hepaticus communis detectable. Magnetic resonance imaging (MRI) revealed a T1 inhomogeneous hyperintens, T2 hyperintens mass compared with liver with slightly inhomogeneous contrast medium uptake.
A laparoscopic cystectomy was performed on suspected gallbladder carcinoma. The space requirements of the ovaries were also removed. Histological examination of the gallbladder space requirement revealed a heterotopic gastric mucosa (HGM). In the left-sided ovary a granulosa cell tumor was detected. After an uncomplicated postoperative course, the patient was discharged into the home.
1.2. Background
Heterotopia is defined as physiological tissue in an aberrant localization.[1] Heterotopic gastric mucosa can be found in the whole gastrointestinal tract from the tongue to the rectum.[2,3] It is most often localized in the upper intestine.[4] A clinically well-known localization is Meckel diverticula, which can mimic an acute appendicitis.[5]
However, heterotopic gastric mucosa can also be localized in the gallbladder, first described by Egyedi in 1934.[6] Other heterotopic tissues of the gallbladder can be of various types like liver tissue, pancreatic tissue, adrenal, or thyroid tissue.[7] Clinically, HMG is often asymptomatic and is most often an incidental finding.[8] On the other side, it can also become symptomatic and can even present as an acute abdomen with possible hazardous perforation.[5]
Due to its rare incidence, systemic data regarding heterotopic gastric mucosa in the gallbladder are still lacking to this date. Therefore, the aim of this present study was to conduct a systemic review of heterotopic gastric mucosa to present a case series of this rare disorder. Furthermore, typically clinically findings and imaging features of HMG were identified
2. Material and methods
2.1. Data acquisition
In our department, we identified 1 patient with heterotopic gastric tissue in the gallbladder. Furthermore, we conducted a systemic review to identify every published case report within the time period 1989 to 2017 in the Medline database. Following search words were used: heterotopic gastric tissue with 557 items and gastric heterotopia with 151 items. Therefore, 708 abstracts were screened for suitable case reports. Due to the retrospective design an ethical approval was not necessary.
Inclusion criteria were as follows: histopathologic confirmed HGM in gallbladder, paper in English and German language as well as a full case report. Excluded were reports on HGM in other localizations than gallbladder.
After thorough analysis we identified 32 suitable papers with 34 patients.[1,7–38] Finally, the study sample consisted of 35 patients. Clinical parameters, imaging features as well as histopathological features were retrieved from the papers.
2.2. Statistical analysis
Collected data were analyzed by means of descriptive statistics (absolute and relative frequencies). Continuous variables were expressed as mean ± standard deviation (SD), and categorical variables as percentages.
3. Results
3.1. Patients and background
There were 17 female (48.6%) and 18 male (51.4%) patients with a median age of 36.6 years (range, 3–80 years). Furthermore, 31.4% (n = 11) of the patients were younger than 18 years.
An overview about the clinical presentation is given by Table 1. The patients showed various symptoms, most of them suffered from abdominal discomfort. For example, 26 (74.3%) patients had abdominal pain, with half of them (n = 13) had a history longer than 3 month. The intensity differed from mild pain (n = 4, 15%) to intense colic (50%). In 7 patients the pain was associated with food intake.
Table 1.
Overview about clinical symptoms of the identified patients.
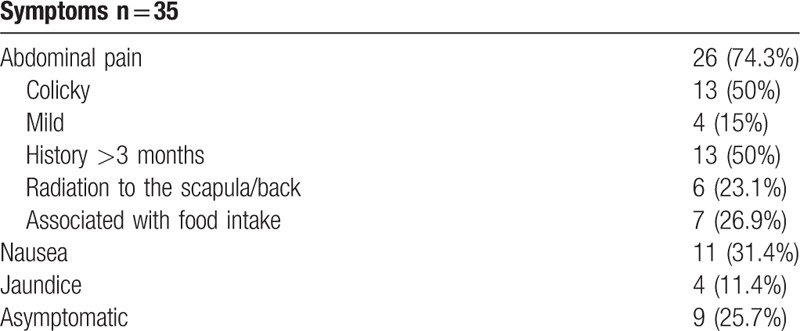
Furthermore, 11 patients suffered from nausea and vomiting (31.4%), and 4 patients presented with jaundice (11.4%). In 25.7% of all cases (n = 9) HGM was diagnosed incidentally.
3.2. Diagnosis
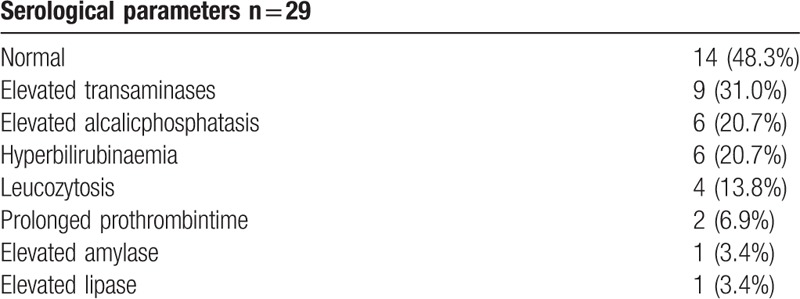
3.2.1. Serological parameters
The laboratory data were documented in 29 (82.9%) cases. Elevated liver enzymes were found in most cases with almost one-third showed elevated transaminases (n = 9). Furthermore, 20.7% had an elevated alkaline phosphatase level and hyperbilirubinemia. However, in half of the cases laboratory data were within normal limits. The serological parameters are summarized in Table 2.
Table 2.
Overview about the serological parameters in the identified patients.
3.2.2. Imaging
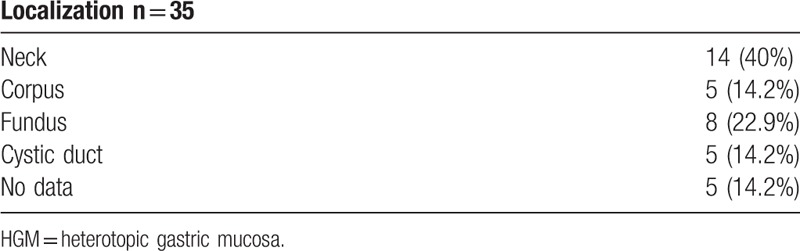
Several different imaging modalities showed gallbladder masses with the mean diameter of 1.6 cm, ranging from 0.5 to 3 cm. Most of the lesions were located in the lower gallbladder, especially (n = 14, 40%) in the gallbladder neck (Table 3). Three masses (8.6%) were only located in the cystic duct. The second common localization was in the gallbladder fundus (n = 8, 22.9%). Rarely, it was in the gallbladder corpus (n = 5, 14.2%). Five papers (14.2%) did not give information about localization.
Table 3.
Different localizations of the identified HGM.
3.2.3. Ultrasound
In most cases (85.7%, n = 30) ultrasound was performed (Table 4). As in our case (Fig. 1), in 20.7% a broad-based mass was described. In 10.3% a sessile polyp was identified. Other rarer findings were a focal thickening of the gallbladder wall and cystic alterations. In 5 cases, the mass was characterized as hyperechoic (55.5%), in 3 as isoechoic (33.3%), and hypoechoic in 1 patient (11.1%).
Table 4.
Ultrasound findings of the identified HGM.
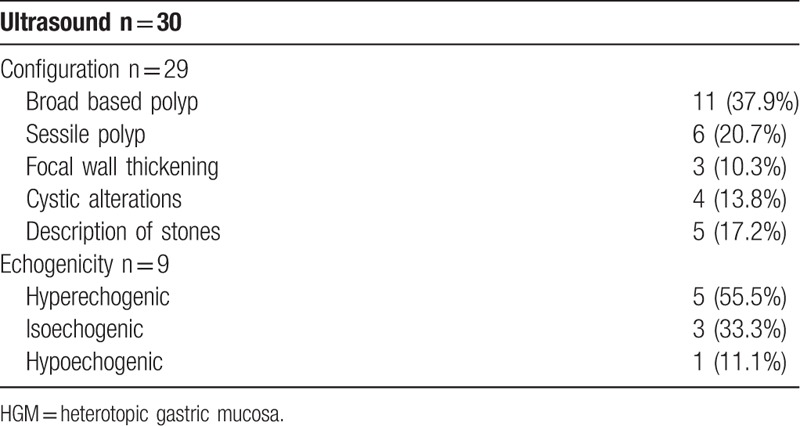
Figure 1.
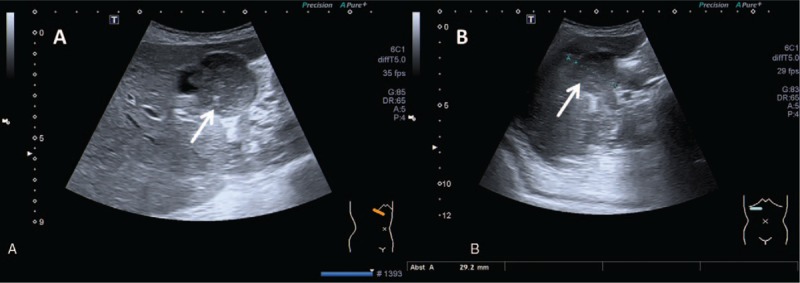
Ultrasound images (Toshiba Apolio 500) showing a broad based, hyperechoic lesion within the gallbladder (arrow).
3.2.4. Computed tomography
Twelve patients (34.3%) were investigated by CT. There were 3 patients with a hyperdense mass in CT (Fig. 2). One author identified a hypodense lesion. In 7 cases (58.3% of the CT cases), iodinated contrast medium was used. All of them showed slightly enhancement.
Figure 2.
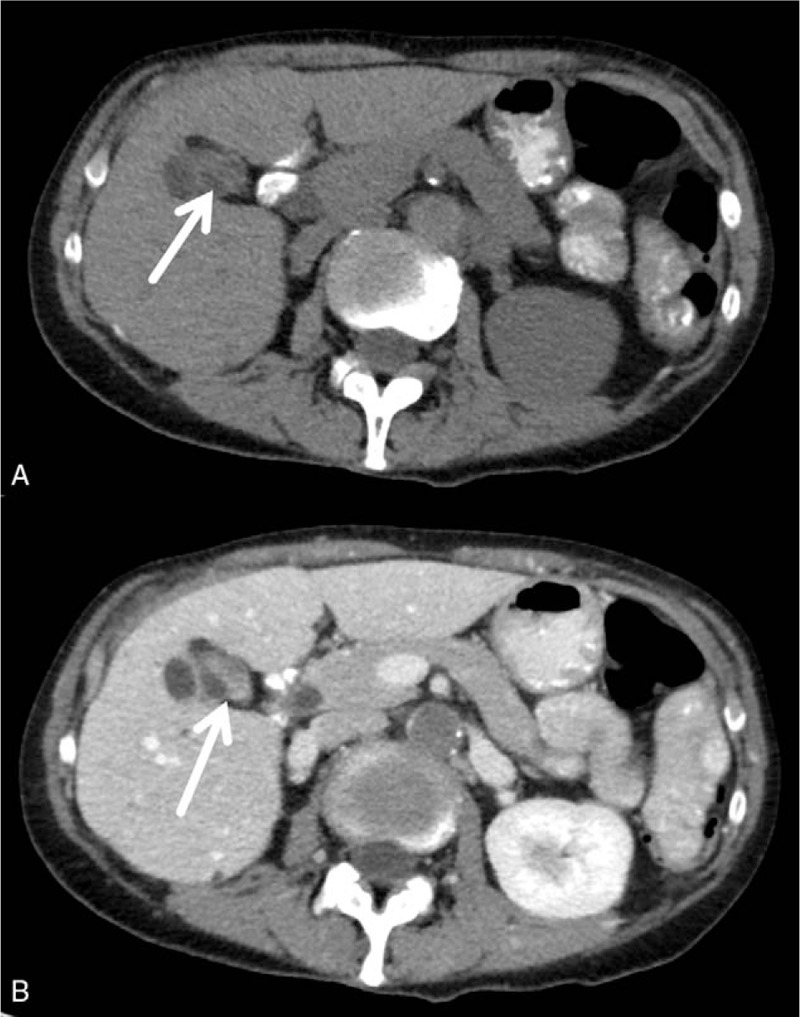
Computed tomographic (CT) findings. A—precontrast axial CT demonstrating a slightly hyperdense mass (arrow) in the gallbladder. B—postcontrast axial CT, showing a slightly enhancement of the lesion (arrow).
3.2.5. Magnetic resonance imaging
MRI was performed in only 1 case (Fig. 3). The identified HGM mass was hyper intense on T1-weighted images and slightly hyper intense on T2-weighted images. It showed slight enhancement after application of contrast medium. On diffusion weighted imaging, a diffusion restriction was noticed.
Figure 3.
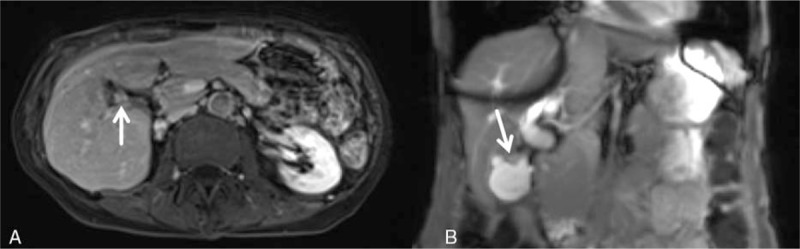
Siemens, 3T, A—axial T1w vibe (volume interpolated breathhold examination) sequence after intravenous Primovist administration, axial: showing a slightly enhanced mass within gallbladder neck/corpus. B—coronal T2w trufi (true fast imaging with steady precession) sequence documenting a slightly hyper intense lesion (arrow).
3.3. Treatment
In all patients, cholecystectomy was performed and all had an uneventful recovery.
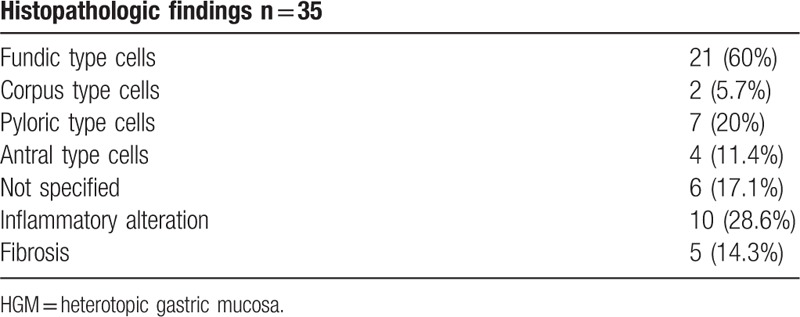
3.4. Histological findings
Most cases revealed heterotopic gastric mucosa of body-fundic type (60%) with chief and parietal cells, followed by pyloric type glands (20%). Less frequently, antral type mucosa (11.4%, Fig. 4) and body mucosa (5.7%) was found. No cardia type mucosa occurred. In 6 cases (17.1%), there were any details about the type of gastric mucosa. Four patients (11.4%) revealed a mixed histologic finding with fundic and pyloric glands. One patient (0.3%) showed fundic and antral cells. In 28.6%, inflammation was reported and even half of them were diagnosed with fibrotic findings. Histopathology details are given with Table 5.
Figure 4.
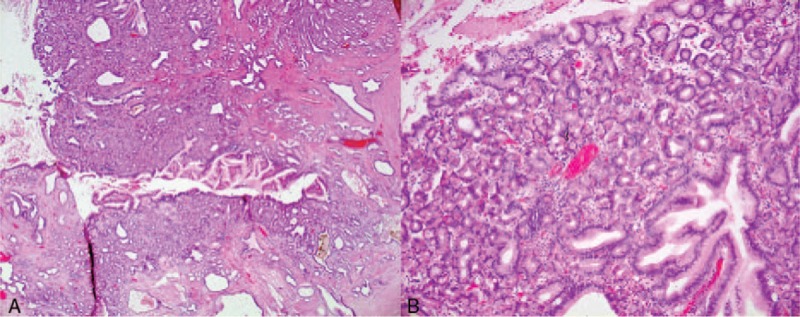
Histopathological examination of the lesion after surgical resection (H&E staining), (A—2.5×, B—20×) revealed an corpus type—gastric mucosa.
Table 5.
Histopathologic findings of the identified HGM.
4. Discussion
HMG is a rare disorder affecting the gallbladder. Therefore, systemic data about it are still lacking to this date. This present study provides data regarding clinically and imaging features as well as histopathology of HGM.
Previously, a male predominance was described in the literature.[15] Contrary to this, the rate of male and female was equal in the present study. We identified an extensive age-span with the median age of 36.4 years. However, heterotopic gastric mucosa in gallbladder can become symptomatically in every age, indicated by the identified range of 3 to 80 years.
Some authors described a predominantly incidental discovery of heterotopic gastric mucosa.[8] However, our analysis showed that 74.3% of the patients were symptomatic. Yet, this finding might be influenced by a possible publication bias.
Previously, findings regarding serological parameters have been rarely described in the literature.[38] Almost half of the patients revealed a normal blood examination. The identified alterations were cholestasis with elevated transaminases and gamma GT or in terms of inflammatory reactions with leukocytosis caused by complications. The cause of this is most likely to be seen in the disturbed bile flow through the HMG with subsequent inflammatory changes.
The diagnosis of heterotopic gastric mucosa in gallbladder can be difficult. For example, the differential diagnosis of polypoid lesions in gallbladder comprises various disorders. However, it is clinically relevant to distinguish heterotopic gastric mucosa from benign polyps, gall bladder carcinoma, or gallbladder metastasis.
Regarding localization, the Ductus cysticus and gallbladder neck are predilection locations.[14] This finding is underlined by the present study in 40% of cases. However, heterotopia can also occur in different locations, as was shown in this study.
Imaging modalities are of special importance in gallbladder diagnostics. The most common and most accessible modality is ultrasound. In our systemic review almost every patient was examined with ultrasound. In ultrasound, heterotopic gastric mucosa depicts itself as a polypoid mass either broad based or sessile. Another form can be shown as a focal wall thickening. Sometimes, it can present as a cystic lesion in the event of secreting gastric mucus without a possibility of draining. The solid mass is usually hyperechoic, less commonly isoechoic, ranging in size from 0.5 to 3 cm.
Regarding CT-findings, lesions were slightly hyperdens and all of them, as far as contrast medium was applicated, revealed a slightly enhancement.
There is paucity of MRI data regarding heterotopic gastric mucosa. Our presented patient showed a hyper intense lesion in T1-weighted images, and was slightly hyper intense in T2-weighted imaged. Moreover, a slight enhancement after contrast medium application was identified. Furthermore, this is the first report regarding diffusion weighted imaging in heterotopic gastric mucosa indicating a diffusion restriction in these lesions. This might be caused by increased cellularity as it was shown in several tumors.[39]
Further diagnostic examination is cholecystography or rarely used a technetium scintigraphy for detection of ectopic gastric mucosa.[16]
The main differential diagnosis is a benign polyp. As well as HGM, they present as an echogenic polypoid or sessile mass without acoustic shadowing. They are described as masses, predominantly <10 mm.[40] The identified HGM can be bigger in size and size might, therefore, be a possible criteria to rule out benign polyps as a potential diagnosis.
Important differential diagnoses are malignant neoplasms, especially gallbladder carcinoma, which would cause a different treatment regime than HGM.
No malignant transformation was found in the identified cases, although it was described previously in 12% to 52% of cases.[11]
Since HGM can present with a transmural manifestation, infiltrative growth of gallbladder carcinoma might not be a reliable sign for malignancy. We identified calcification of the gallbladder wall and calcified gallstones, which was not mentioned previously. Gallbladder carcinoma can infiltrate the gallbladder fossa, whereas HGM is commonly located in the gallbladder neck. Therefore, we propose that localization is an important imaging feature to distinguish between HGM and gallbladder carcinoma. Furthermore, in contrast to HGM, gallbladder carcinoma is hypovascularized on CT and MRI.[41]
Another differential diagnosis is gallbladder metastasis. Especially malignant melanoma can spread to the gallbladder.[42] It commonly appears as a transmural mass. Furthermore, metastasis can be a polypoid mass as well as a bulky mass. Anamnestic history about a malignancy is the most important suggestion for gallbladder metastasis.[42]
There are several limitations of our study to address. Firstly, it is a case series of published case reports. Therefore, publication bias might influence this study. For example, asymptomatic patients are not published as a case report and cannot be identified in a systemic review. This is primarily caused by the low incidence of this disorder which thus cannot be investigated by prospective studies. Secondly, CT and especially MRI images were not performed in all patients.
In conclusion HGM is a rare entity which concerns all ages, and is presenting either asymptomatically or with abdominal discomfort, often with cholecystitis like pain. The final diagnosis is made by histopathology. Regarding imaging, it is most frequently examined in ultrasound with a usually hyperechoic focal wall thickening or polypoid mass without acoustic shadowing. On CT, HGM is slightly hyperdense with a slightly enhancement, which is an unspecific finding and does not allow for further differential diagnosis. However, MRI might have diagnostic benefit with possible features to distinguish between malignant entities and HGM.
Footnotes
Abbreviations: ALAT = alanine aminotransferase, AP = alkaline phosphatase, ASAT = aspartate aminotransferase, CT = computed tomography, DWI = diffusion weighted imaging, gamma GT = gamma-glutamyltransferase, HGM = heterotopic gastric mucosa, MRI = magnetic resonance imaging, SD = standard deviation.
The authors report no conflicts of interest.
References
- [1].Sciumè C, Geraci G, Pisello E, et al. Heterotopic gastric mucosa in the gallbladder: case report and literature review. Ann Ital Chir 2005;76:93–7. [PubMed] [Google Scholar]
- [2].Melato M, Ferlito A. Heterotopic gastric mucosa of the tongue and the oesophagus. ORL J Othorhinolaryngol Relat Spec 1975;37:244–54. [DOI] [PubMed] [Google Scholar]
- [3].Jordan FT, Mazzeo RJ, Soiderer MH. Heterotopic gastric mucosa of the rectum: a rare cause of rectals bleeding. Arch Surg 1983;118:878–80. [DOI] [PubMed] [Google Scholar]
- [4].Schmidt G, Börsch G, Wegener M. Heterotopic gastric mucosa of the gastrointestinal tract. Z Gastroenterol 1985;23:545–50. [PubMed] [Google Scholar]
- [5].Bunni J, Barrett HL, Cook TA. Perforated jejunal ulcer associated with gastric mucosa in a jejunal diverticulum. World J Clin Cases 2014;2:209–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Egyedi L. Case of polypus of gallbladder containing aberrant gastric mucous membrane. Gyogyaszat (Gyogyastat) 1934;74:596–9. [Google Scholar]
- [7].Madrid C, Berrocal T, Gorospe L, et al. Heterotopic gastric mucosa involving the gallbladder and biliary tree. Pediatr Radiol 2003;33:129–32. [DOI] [PubMed] [Google Scholar]
- [8].Hayama S, Suzuki Y, Takahashi M, et al. Heterotopic gastric mucosa in the gallbladder: report of two cases. Surg Today 2010;40:783–7. [DOI] [PubMed] [Google Scholar]
- [9].Özgün G, Adim ŞB, Uğraş N, et al. A mimicker of gallbladder carcinoma: cystic gastric heterotopia with intestinal metaplasia. Turk Patoloji Derg 2017;33:58–61. [DOI] [PubMed] [Google Scholar]
- [10].Kim J, Jarboe MD, Arnold MA, et al. Biliary duplication cyst with heterotopic gastric mucosa resulting in obstruction of the biliary system: a case report. J Pediatr Surg 2012;47:e5–8. [DOI] [PubMed] [Google Scholar]
- [11].Orizio P, Villanacci V, Bassotti G, et al. Heterotopic gastric mucosa in the cystic duct. Int J Surg Pathol 2011;19:364–5. [DOI] [PubMed] [Google Scholar]
- [12].Popkharitov A, Gulubova MV, Dandov AD, et al. Heterotopic gastrointestinal cyst mimicking chronic cholecystitis: a case report. J Med Case Rep 2008;2:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Cöl C, Boran C, Turkeli V, et al. Heterotopic gastric mucosa in gallbladder associated with kidney agenesis and congenital hip dysplasia. Acta Clin Belg 2007;62:120–2. [DOI] [PubMed] [Google Scholar]
- [14].Daud MS, Salomão FC, Salomão EC, et al. Gastric heterotopia together with squamous metaplasia in the gallbladder. Acta Gastroenterol Latinoam 2007;37:164–7. [PubMed] [Google Scholar]
- [15].Verbo A, Manno A, Mattana C, et al. Peptic ulcer in gastric heterotopia of the gallbladder without evidence of Helicobacter pylori infection. Dig Dis Sci 2007;52:2201–3. [DOI] [PubMed] [Google Scholar]
- [16].Yoon AJ, Cowles RA, Stylianos S, et al. Heterotopic gastric mucosa in the gallbladder: a rare cause of massive hemobilia. J Pediatr Gastroenterol Nutr 2005;40:606–8. [DOI] [PubMed] [Google Scholar]
- [17].Quispel R, Schwartz MP, Schipper ME, et al. Heterotopic gastric tissue mimicking malignant biliary obstruction. Gastrointest Endosc 2005;62:170–2. [DOI] [PubMed] [Google Scholar]
- [18].Tavli L, Belviranli M, Erikoğlu M, et al. Gastric heterotopia together with intestinal metaplasia in the gallbladder: case report and review of literature. Turk J Gastroenterol 2005;16:160–2. [PubMed] [Google Scholar]
- [19].Lombay B, Kiss A, Szabo L. Heterotopic gastric mucosa in the gallbladder. Pediatr Radiol 2003;33:587. [DOI] [PubMed] [Google Scholar]
- [20].Bailie AG, Wyatt JI, Sheridan MB, et al. Heterotopic gastric mucosa in a duplicate gallbladder. J Pediatr Surg 2003;38:1401–3. [DOI] [PubMed] [Google Scholar]
- [21].Işik I, Sezer C, Dursun A. Gastric heterotopia in the gallbladder: a case report. Turk J Gastroenterol 2002;13:172–4. [PubMed] [Google Scholar]
- [22].Xeropotamos N, Skopelitou AS, Batsis C, et al. Heterotopic gastric mucosa together with intestinal metaplasia and moderate dysplasia in the gall bladder: report of two clinically unusual cases with literature review. Gut 2001;48:719–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hamazaki K, Fujiwara T. Heterotopic gastric mucosa in the gallbladder. J Gastroenterol 2000;35:376–81. [DOI] [PubMed] [Google Scholar]
- [24].Inoue Y, Shibata T, Niinobu T, et al. Heterotopic gastric mucosa in the gallbladder: sonographic and CT findings. Abdom Imaging 2000;25:198–200. [DOI] [PubMed] [Google Scholar]
- [25].Murakami M, Tsutsumi Y. Aberrant pancreatic tissue accompanied by heterotopic gastric mucosa in the gall-bladder. Pathol Int 1999;49:580–2. [DOI] [PubMed] [Google Scholar]
- [26].Wakiyama S, Yoshimura K, Shimada M, et al. Heterotopic gastric mucosa in a gallbladder with an anomalous union of the pancreatobiliary duct: a case report. Hepatogastroenterology 1998;45:1488–91. [PubMed] [Google Scholar]
- [27].Leyman P, Saint-Marc O, Hannoun L, et al. Heterotopic gastric mucosa presenting as gallbladder polyps. Acta Chir Belg 1996;96:128–9. [PubMed] [Google Scholar]
- [28].Uchiyama S, Imai S, Suzuki T, et al. Heterotopic gastric mucosa of the gallbladder. J Gastroenterol 1995;30:543–6. [DOI] [PubMed] [Google Scholar]
- [29].Schimpl G, Schaffler G, Sorantin E, et al. Polypoid gastric heterotopia in the gallbladder: clinicopathological findings and review of the literature. J Pediatr Gastroenterol Nutr 1994;19:129–31. [DOI] [PubMed] [Google Scholar]
- [30].Martinek V, Keller HW, Vössing R, et al. Congenital duodenal obstruction in combination with heterotopic gastric mucosa in the gallbladder. Case report and etiology. Chirurg 1994;65:807–9. [PubMed] [Google Scholar]
- [31].Vallera DU, Dawson PJ, Path FR. Gastric heterotopia in the gallbladder. Case report and review of literature. Pathol Res Pract 1992;188:49–52. [DOI] [PubMed] [Google Scholar]
- [32].Boyle L, Gallivan MV, Chun B, et al. Heterotopia of gastric mucosa and liver involving the gallbladder. Report of two cases with literature review. Arch Pathol Lab Med 1992;116:138–42. [PubMed] [Google Scholar]
- [33].Lamont N, Winthrop AL, Cole FM, et al. Heterotopic gastric mucosa in the gallbladder: a cause of chronic abdominal pain in a child. J Pediatr Surg 1991;26:1293–5. [DOI] [PubMed] [Google Scholar]
- [34].Martinez-Urrutia MJ, Vasques Estevez J, Larrauri J, et al. Gastric heterotopy of the biliary tract. J Pediatr Surg 1990;25:356–7. [DOI] [PubMed] [Google Scholar]
- [35].Pradines P, Brauner M, Legrand I, et al. Heterotopic gastric mucosa in the gallbladder. AJR Am J Roentgenol 1989;152:432. [DOI] [PubMed] [Google Scholar]
- [36].Günter E, Ell C, Heyder N, et al. Ectopic tissue as polypoid lesions of the gallbladder. Dtsch Med Wochenschr 1989;114:1984. [PubMed] [Google Scholar]
- [37].Yamamoto M, Murakami H, Ito M, et al. Ectopic gastric mucosa of the gallbladder: comparison with metaplastic polyp of the gallbladder. Am J Gastroenterol 1989;84:1423–6. [PubMed] [Google Scholar]
- [38].Wlaź J, Mądro A, Kaźmierak W, et al. Pancreatic and gastric heterotopy in the gastrointestinal tract. Postepy Hig Med Dosw (Online) 2014;68:1069–75. [DOI] [PubMed] [Google Scholar]
- [39].Surov A, Meyer HJ, Wiencke A. Correlation between apparent diffusion coefficient (ADC) and cellularity is different in several tumors: a meta-analysis. Oncotarget 2017;8:59492–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Lee KF, Wong J, Li JC, et al. Polypoid lesions of the gallbladder. Am J Surg 2004;188:186–90. [DOI] [PubMed] [Google Scholar]
- [41].Gore RM, Thakrar KH, Newmark GM, et al. Gallbladder imaging. Gastroenterol Clin North Am 2010;39:265–87. [DOI] [PubMed] [Google Scholar]
- [42].Martel JP, McLean CA, Rankin RN. Melanoma of the gallbladder. Radiographics 2009;29:291–6. [DOI] [PubMed] [Google Scholar]


