Abstract
Adults with limited health literacy have difficulty managing chronic conditions, higher hospitalization rates, and more healthcare expenditures. Simple screening tools have been developed, but limited work has evaluated instruments among low-income populations. This study assessed health literacy among primary care patients of a federally qualified health center, and compared a single screening question about perceived difficulty completing medical forms.
A cross-sectional survey was administered to English-speaking patients ≥40 years. Both the Newest Vital Sign (NVS), a 6-item questionnaire, and a single-item screening question about perceived difficulty with completing medical forms, assessed health literacy. Logistic regression was used to identify predictors of inadequate health literacy and receiver operator curves compared the NVS and single-item question.
Participants (n = 406) were, on average, aged 58.5 years (±11.3), 72.2% female, and identified as Hispanic/Latino (19.2%), non-Hispanic white (31.0%), non-Hispanic black (40.9%), or other (8.9%). Of the 406 participants, 335 (82.5%) completed the NVS. Patients who declined NVS were more likely to be older (P < .001) and male (P = .01). Only 13.7% had adequate health literacy. Older adults, Hispanic and non-Hispanic black patients, patients with missed office visits, and those reporting less confidence completing medical forms were significantly more likely to have inadequate health literacy. Perceived confidence completing medical forms demonstrated low sensitivity but high specificity at multiple thresholds.
This is the first investigation to compare the NVS and confidence completing medical forms question. Many patients declined health literacy assessments, but health literacy screening may identify patients who need additional health education and resources.
Keywords: health literacy, primary care, screening
1. Introduction
Approximately 80 million adults in the United States have limited health literacy,[1] defined as “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.”[2] Limited health literacy is more common among older populations, race/ethnic minority groups, people living in poverty, and persons with less than a high school education.[1] Adults with limited health literacy are more likely to engage in high-risk health behaviors,[3,4] have more difficulty managing chronic conditions through intervention and medication adherence,[5] have higher rates of hospitalization,[6] and generate higher healthcare expenditures per person[7] than those with adequate health literacy. Notably, health literacy interventions appear to have a greater effect on improving nonmedication, healthy lifestyle adherence in low-income patient samples compared to higher income samples,[5] suggesting that low-income and other vulnerable populations should be the focus of health literacy identification in the clinical setting.
Rising healthcare costs and hospital accountability measures have led to several national action plans to address limited health literacy. Most notably, the National Action Plan to Improve Health Literacy,[8]Healthy People 2020,[9] and the Institute of Medicine's Health Literacy: A Prescription to End Confusion[10] highlight a national commitment to address healthcare access and disease management barriers caused by limited health literacy and subsequently improve population health outcomes. Within each action plan, health literacy is broadly defined as a multidimensional concept that includes social, cognitive, economic, and personal skills,[11,12] yet there is no consensus about a single, best health literacy instrument.
Multiple screening instruments for health literacy are available. Commonly used instruments such as the Test of Functional Health Literacy in Adults (TOFHLA)[13] and the Rapid Estimate of Adult Literacy in Medicine (REALM)[14] are largely considered the “gold standards” in measuring health literacy, yet these instruments only measure reading and pronunciation skills, and may be culturally insensitive or inappropriate for non-native English speakers.[15–17] The US Health Literacy Scale (HALES)[18,19] is a more comprehensive tool designed to differentiate between health-related competencies in multiple domains and between health literacy tasks and skills. Likewise, the Health Literacy Questionnaire (HLQ)[20] is designed to conceptualize cultural and conceptual knowledge, speaking and listening skills, writing and reading skills, and numeracy. Both the HALES and HLQ can be used to identify individuals with limited health literacy, but the length of both instruments limit their practical utility in time-conscious clinical settings.
Several brief instruments to screen for health literacy have been developed as well. In 2005, the Newest Vital Sign (NVS) was developed to measure reading, comprehension, and numeracy using a nutritional label and a 6-item questionnaire.[21] The NVS is used frequently as a clinical screening tool with high sensitivity to detect limited literacy.[22] In addition to the NVS, Chew et al[23] identified 3 questions regarding perceived level of difficulty understanding, reading, or reporting medical information; all 3 brief questions were validated with the short form-TOFHLA and the REALM.[23,24] In particular, perceived difficulty completing medical forms has been identified as a valid screening question by multiple studies.[23,24] Although the shorter length of the NVS or a single screening question may be more appropriate for routine use in busy clinical settings, limited work has evaluated these simple screening tools among low-income patient populations. Thus, the primary purpose of this study was to assess health literacy using the NVS instrument in a low-income patient population from a large, federally qualified health center. The secondary purpose of this study was to compare the NVS and a single screening question about perceived difficulty completing medical forms in order to identify patients with inadequate health literacy.
2. Methods
2.1. Setting and sample
The Baylor University Institutional Review Board approved the survey and informed consent procedures used in this research study, which was nested within a larger study designed to assess self-reported health behaviors and the prevalence of perceived health symptoms. The target population were patients of the Family Health Center (FHC), a large federally qualified health center in central Texas. At the health center in 2016, 165,784 primary medical care encounters were provided to 49,581 patients by 68 physicians (21 family physicians, 38 resident/fellow family physicians, 2 pediatricians, 3 internists, 4 obstetrician/gynecologists), 14 nurse practitioners, and 5 physician assistants. Approximately 1 out of every 5 county residents is a health center patient, and over 90% of FHC patients live at or below 200% of federal poverty guidelines.[25]
Between February 15 and June 15, 2016, patients were approached in FHC waiting rooms to determine eligibility. Eligible patients were English-speaking adult patients ≥40 years of age. Patients who met inclusion criteria and provided consent were administered orally a 10-minute survey by study staff. After the survey was complete, study staff accessed electronic medical records to obtain laboratory, medication, and healthcare utilization data. When the patient completed the survey, his/her name was included in a drawing for a 1 in 10 chance of winning a $20 gift card to a local grocery store.
2.2. Measures
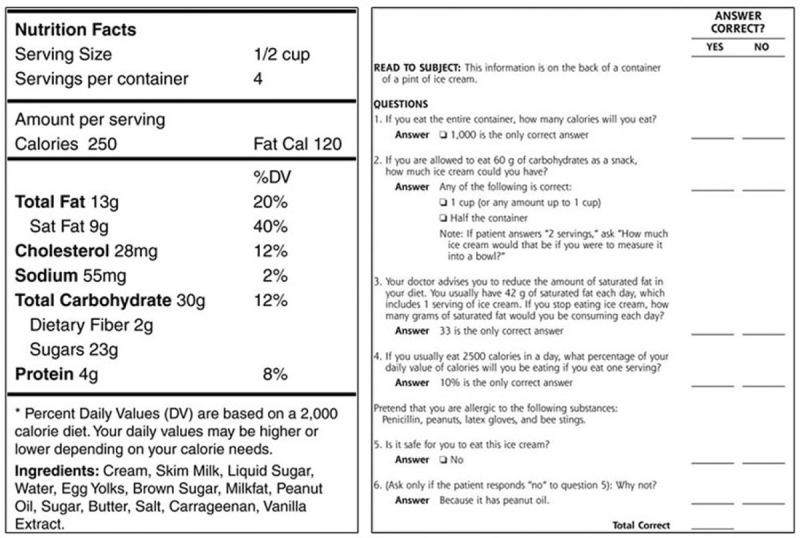
Health literacy was assessed with 2 tools: the NVS and a single-item screening question. The NVS is a quick and valid functional health literacy assessment.[21] Administration time ranges from 2 to 6 minutes and it has a high sensitivity to detect limited healthy literacy.[22] Patients are given an ice cream nutrition label and asked subsequent 6 questions. Questions focus on caloric and nutritional intake (testing reading and numeracy) and ingredients (testing functional health literacy); responses are scored as correct or incorrect and correct responses are summed (see Appendix 1). According to previous work, patients who respond with 4 or more correct responses are likely to have adequate health literacy, patients who respond with 2 or 3 correct responses have a possibility of limited health literacy, and patients who respond with 0 or 1 correct responses have a high likelihood of limited health literacy. In addition to the NVS, a single-item screening question was also used to identify perceived difficulty with medical information. Patients were asked “How confident are you filling out medical forms by yourself?”[23] Response choices included Extremely, Quite a bit, Somewhat, A little bit, and Not at all. Patients completed this single question during a telephone call after they completed the oral survey to obtain all other data in 2016.
Patients were also asked to provide self-rated health status, determined from the question “In general, would you say your health is excellent, very good, good, fair, or poor?”[26] Demographic data were obtained from the electronic medical record and included age, sex, and race/ethnicity (categorized as Hispanic/Latino, non-Hispanic white, non-Hispanic black, or non-Hispanic other (which included Asian)). Health data from the electronic medical record included body mass index (BMI; kg/m2), diabetes status (yes/no), and number of current medications. Healthcare utilization in the previous 24 months included number of office visits and number of missed appointments, defined as the number of “no shows” plus the number of canceled appointments.
2.3. Statistical analysis
Descriptive statistics, including mean (standard deviation) for continuous variables and percent for categorical variables, were calculated for all variables in the total study population. We also described the study population by NVS assessment results, using 4 categories: missing (i.e., patient declined NVS assessment), high likelihood of limited health literacy, possibility of limited health literacy, and adequate health literacy. We compared the 4 categories, which included the “missing” health literacy category, using analysis of variance (ANOVA) for continuous variables and Chi-square tests for categorical variables. We generated odds ratios (OR) and corresponding 95% confidence intervals (CI) from logistic regression to determine the association between each predictor variable separately and the possibility or high likelihood of limited health literacy (NVS < 4). We also used multivariate logistic regression to simultaneously adjust for all other predictor variables. Data management, descriptive statistics, and logistic regression models were conducted using SAS v9.4 (SAS Institute Inc., Cary, NC).
Receiver operating curves (ROC) were constructed using MedCalc software (v17.7.2) to determine the perceived level of confidence completing medical forms that has the best balance of sensitivity and specificity in comparison to the NVS instrument used as the reference standard. The larger the area under the receiver operating curve (AUROC)—that is, the closer the curve follows the left and top borders of the plot—the more accurate the test.[24,27] We also calculated the sensitivity, specificity, and positive and negative likelihood ratios as predictors of possibly or high likelihood of limited health literacy (NVS < 4). Statistical significance was defined a priori at the 2-sided α = 0.05 level.
3. Results
There were 406 eligible patients who participated in the study, ranging in age from 40 to 96 years (mean age = 58.5 ± 11.3 years), and 72.2% were female. In terms of race/ethnicity, 19.2% (n = 78) identified as Hispanic/Latino, 31.0% (n = 126) identified as non-Hispanic white, 40.9% (n = 166) identified as non-Hispanic black, and 8.9% (n = 36) identified as non-Hispanic other. Mean BMI was 32.8 kg/m2, and patients had, on average, 10 active prescriptions each. Within the previous 24 months, patients had almost 12 primary healthcare encounters, and on average, 7 missed visits (Table 1).
Table 1.
Patient characteristics for the total sample and by health literacy status.
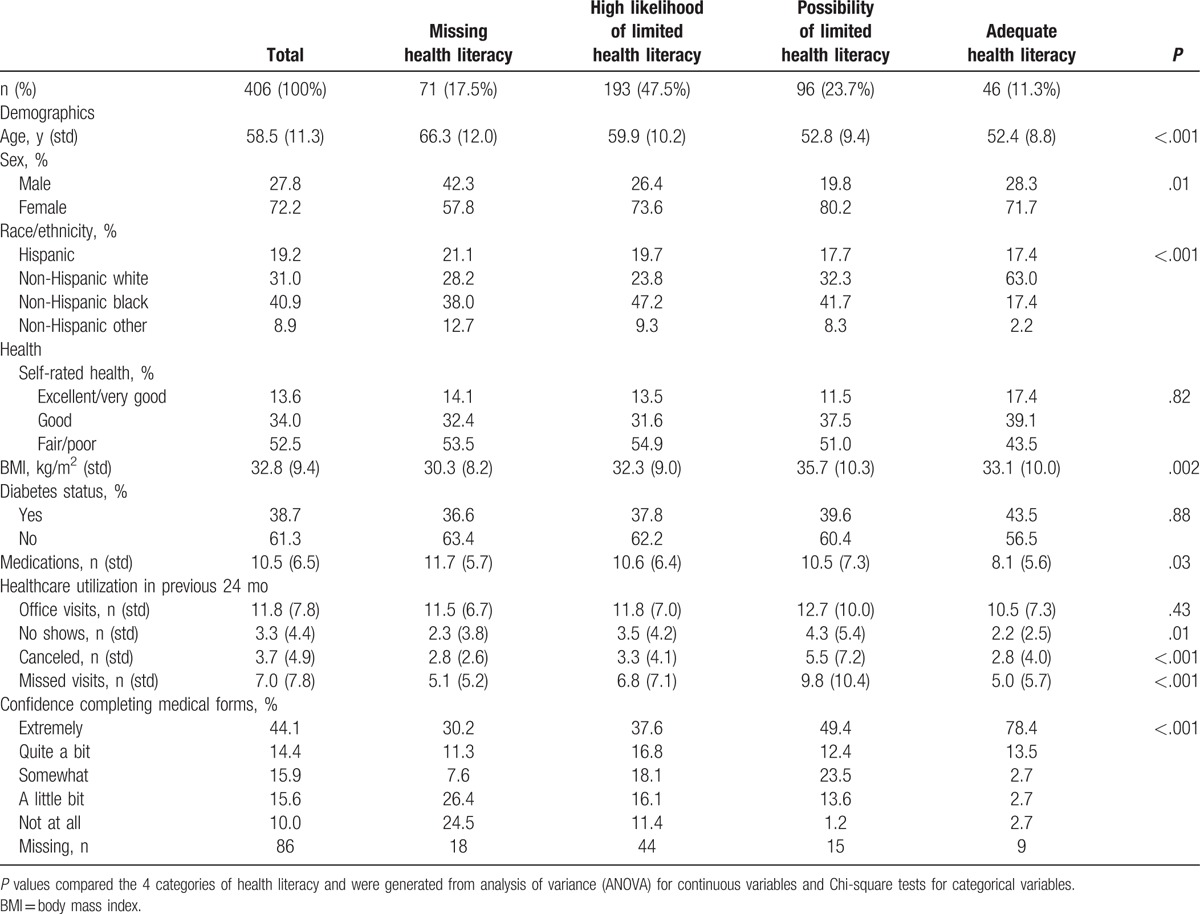
Of the 406 patients who participated in the larger survey, 335 patients (82.5%) completed the NVS health literacy assessment and 71 patients (17.5%) declined to participate in the NVS assessment. Patients who declined participation were more likely to be older (P < .001) and male (P = .01), but there did not appear to be any race/ethnic differences between patients who completed the NVS and those who did not. Among patients who completed the NVS health literacy assessment, 193 out of 335 (57.6%) had a high likelihood of limited health literacy (0 ≤ NVS ≤ 1), 96 out of 335 (28.7%) had a possibility of limited health literacy (2 ≤ NVS ≤ 3), and 46 out of 335 (13.7%) had adequate health literacy (NVS ≥ 4).
Overall, 44.1% of patients reported that they were extremely confident completing medical forms. There appeared to be a dose–response pattern between extreme confidence completing medical forms and the NVS health literacy assessment: 30.2% of patients who declined the NVS assessment, 37.6% of patients with a high likelihood of limited health literacy, 49.4% of patients with a possibility of limited health literacy, and 78.4% of patients with adequate health literacy reported they were extremely confident completing medical forms (P < .001). Likewise, there appeared to be an inverse relationship between lack of confidence completing medical forms and NVS health literacy (Table 1).
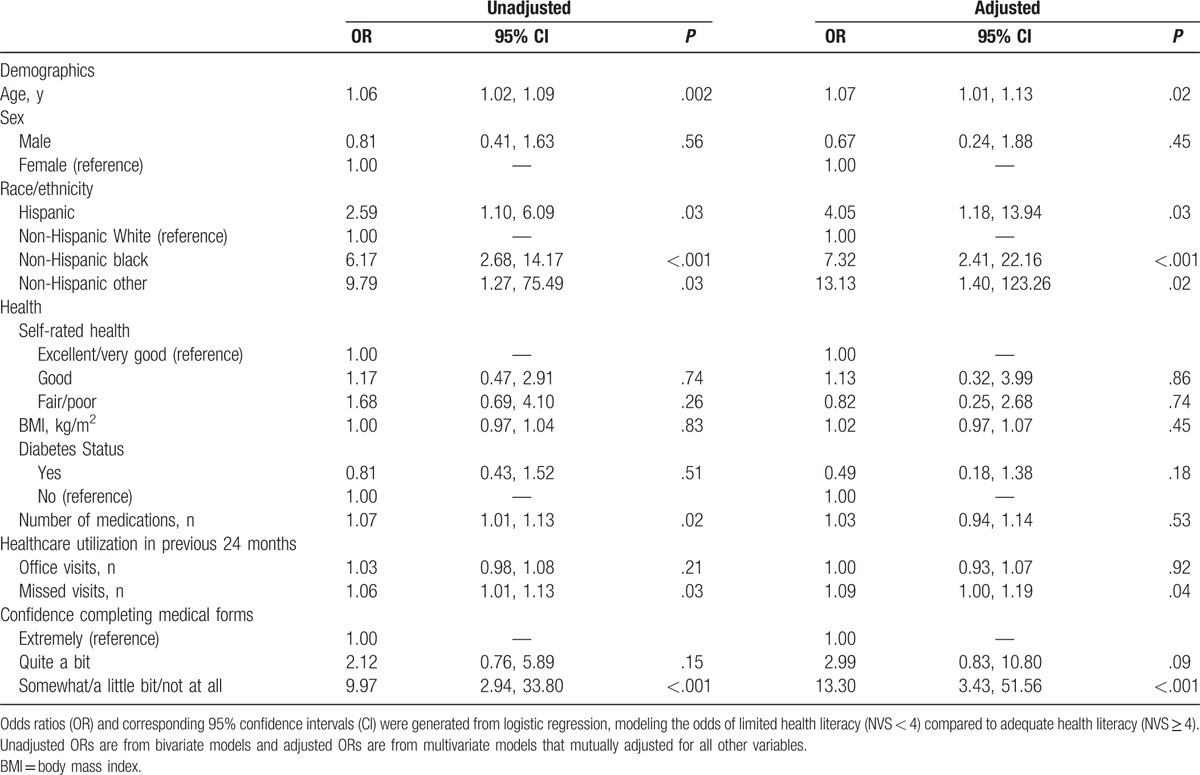
As shown in Table 2, multiple demographic, health, and healthcare utilization variables were associated with inadequate health literacy (defined as NVS < 4). After adjustment for all other factors, older adults, race/ethnic minority groups, and people with more missed office visits were significantly more likely to have inadequate health literacy. For example, Hispanic patients were four times more likely (OR = 4.05; 95% CI: 1.18, 13.94; P = .03) and non-Hispanic black patients were 7 times more likely (OR = 7.32; 95% CI: 2.41, 22.16; P = <.001) to have inadequate health literacy (NVS < 4) compared to non-Hispanic white patients, even after adjusting for age, sex, self-rated health, BMI, diabetes status, number of medications, healthcare utilization, and confidence completing medical forms. Patients who reported they were somewhat, a little bit, or not at all confident completing medical forms were also significantly more likely to have NVS scores <4, but small sample sizes and large confidence intervals caution the interpretation.
Table 2.
Association between demographic, health, healthcare utilization, and confidence completing medical forms and high or possible likelihood of limited health literacy, defined as Newest Vital Sign (NVS) score < 4.
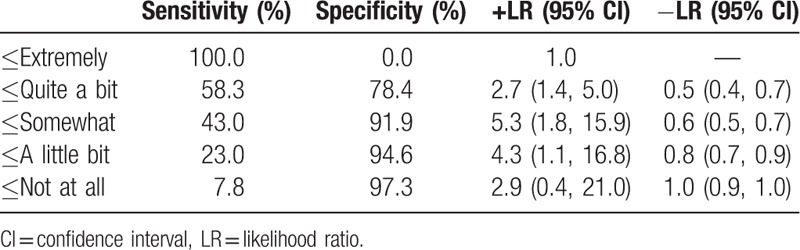
We constructed a receiver operating curve for perceived level of confidence completing medical forms in detecting inadequate health literacy (NVS < 4), as shown in Fig. 1. The AUROC was 0.70 (95% CI: 0.64, 0.76). Sensitivity, specificity, and positive and negative likelihood ratios as predictors of inadequate health literacy (NVS < 4) are shown in Table 3 for different thresholds of confidence completing medical forms. The screening question about confidence completing medical forms demonstrated low sensitivity but high specificity at multiple thresholds.
Figure 1.
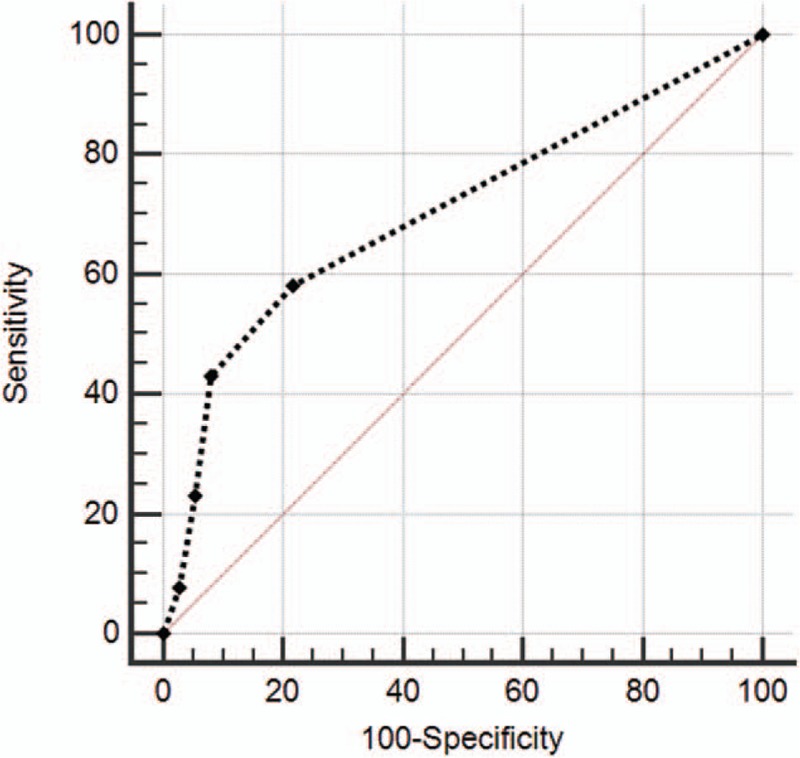
Receiver operating curve (ROC) for perceived confidence completing medical forms using the Newest Vital Sign for detecting possibility or high likelihood of limited health literacy. ROC = 0.70 (95% CI: 0.64, 0.76).
Table 3.
Performance of screening question “How confident are you filling out medical forms by yourself?” for detecting possibility or high likelihood of limited health literacy.
4. Discussion
Many health literacy assessment instruments lack practical utility and the length of assessments preclude routine use in the busy clinical setting. The purpose of this study was to compare 2 brief instruments, the NVS[21] and a screening question about perceived confidence completing medical forms,[23] in a low-income patient population at a federally qualified health center. NVS is a brief, 6-item assessment of reading, basic numeracy, and comprehension of straightforward allergen information using a simplified ice cream nutrition label.[21] Based on the number of correct responses, respondents can be categorized in 1 of 3 categories: high likelihood of limited health literacy, possibility of limited health literacy, and adequate health literacy. National estimates indicate that only 12% of adults have proficient health literacy. Inadequate health literacy is more common in low-income and Hispanic and black minority populations.[1] Thus, perhaps unsurprisingly, a very low proportion of patients (46 out of 335 with NVS data; 13.7%) in our study demonstrated 4 or more correct responses on the NVS instrument. Both Hispanic and non-Hispanic black patients were more likely than non-Hispanic white patients to have inadequate health literacy. These findings are particularly troubling, given that the average patient in our study was using ten medications, and national data indicate that inadequate health literacy is associated with poorer medication and nonmedication adherence while managing chronic conditions.[5]
Notably, although 86.2% (289 out of 335 with NVS data) of those who completed the NVS assessment had inadequate health literacy (NVS < 4), we also observed a high proportion of patients who declined participation in the NVS assessment altogether but otherwise completed the preceding and following survey questions. Patients with missing NVS data were more likely to be older and male, and over half reported that they were a little bit or not at all confident completing medical forms. Although we did not collect information on reasons for declining the NVS assessment, we hypothesize that literacy shame, stigmatization, and embarrassment may play a role,[28–30] but more work is needed in this population to understand participation avoidance.
ROCs are most commonly used as a quantitative method to evaluate how well a screening test performs to identify an outcome measured with a “gold standard.” The area under the receiver operating curve (AUROC; also called the c-statistic) can range from 0.5, indicating that a test is no better than chance alone, to 1.0, indicating a perfect test with no false positives and no false negatives.[24,27] Previous work has shown that the NVS correlates well with the TOFHLA (AUROC = 0.88 for English speakers).[21] In our study, which compared a single screener question to the NVS, the AUROC was 0.70, indicating a “reasonable” or “fair” test; on average, the confidence completing medical forms screener question correctly predicted inadequate health literacy (NVS < 4) 70% of the time.[27,31] These results are fairly consistent with other investigations. In a study of approximately 300 English-speaking adults in a university-based primary care clinic, the confidence completing medical forms screener question correctly predicted limited or marginal health literacy defined with the REALM 79% of the time.[24] In another study of mostly male English-speaking patients from a VA healthcare system, the confidence completing medical forms screener question correctly predicted inadequate or marginal health literacy defined with the short form-TOFHLA 66% of the time.[23] To our knowledge, our investigation is the first to compare the confidence completing medical forms screener question to the NVS instrument.
This study has several limitations. First, sampling from waiting rooms generates a convenience sample and may not represent the entire patient population of this health center. We were also limited to only English-speaking patients due to study staff and resources. Thus, results may not be generalizable to all patients or to non-English speaking adults. Given the high proportion of Spanish-speaking residents in central Texas, we performed a sensitivity analysis using a four-item language acculturation scale to evaluate in what language the participant usually reads/speaks, speaks at home, thinks, and speaks with friends. Over 90% of participants reported “only English” or “more English than Spanish.” Although these questions are of primary interest only for Hispanic patients, which is appropriate since our study population resides in central Texas, there was no association between language acculturation and adequate health literacy in our study. Second, although we described the health survey for the purposes of informed consent, we did not explicitly indicate the focus of health literacy to potential respondents. Although survey questions were administered orally by study staff, the NVS includes a reading component when participants are given the ice cream nutritional label. Patients with poor literacy skills may have declined to participate in the entire survey and/or the health literacy assessment, which may explain the high refusal rate for this survey portion. As such, we suspect that inadequate health literacy is underestimated in our study. Finally, our investigation explored associations between common demographic, health, and healthcare utilization variables that were easy to ask or obtain in electronic medical records. Unmeasured confounders are likely, which may bias the results of our multivariate models. For example, future studies should likely include comprehensive assessments of educational attainment and/or household income.
Despite these limitations, our findings emphasize the potential utility of screening for health literacy in the clinical setting. In particular, patients with inadequate health literacy appeared more likely to miss healthcare visits, use a higher number of medications, and report less confidence completing medical forms than patients with adequate health literacy. In our large federally qualified health center, older adults, Hispanic and non-Hispanic black patients, patients with missed appointments, and those who report difficulty completing medical forms are more likely to have inadequate health literacy. We also observed a high proportion of patients who declined health literacy assessments with the NVS, which deserves further attention. Furthermore, we extended findings on the reasonable use of a single screening question about confidence completing medical forms, which may be useful to busy clinicians as a simple, less stigmatizing tool to assess health literacy.
Health literacy screening may identify patients who need additional health education and resources. Providers who are aware of poor health literacy skills are more likely to employ strategies like involvement of family members, use of pictures and diagrams, and checking for understanding of medications.[32] Multiple health literacy screening and assessment tools are available to healthcare providers, yet the choice of the instrument is complicated by patient population characteristics and time availability.
Appendix 1. Newest Vital Sign nutrition label and scoring instrument.[21]
Footnotes
Abbreviations: ANOVA = analysis of variance, AUROC = area under the receiver operating curve, BMI = body mass index, CI = confidence interval, FHC = Family Health Center, HALES = United States Health Literacy Scale, HLQ = Health Literacy Questionnaire, LR = likelihood ratio, NVS = Newest Vital Sign, OR = odds ratio, REALM = Rapid Estimate of Adult Literacy in Medicine, TOFHLA = Test of Functional Health Literacy in Adults.
The authors have no conflicts of interest to disclose.
References
- [1].Kutner M, Greenberg E, Jin Y, et al. The Health Literacy of America's Adults: Results From The 2003 National Assessment Of Adult Literacy. National Center for Education Statistics; 2006. Available at: http://files.eric.ed.gov/fulltext/ED493284.pdf. [Google Scholar]
- [2].Ratzan SC, Parker RM. Introduction. In: Selden CR, Zorn M, Ratzan SC, Parker, RM, eds. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services; 2000. [Google Scholar]
- [3].Hoover DS, Vidrine JI, Shete S, et al. Health literacy, smoking, and health indicators in African American adults. J Health Commun 2015;20(suppl 2):24–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Stewart DW, Cano MA, Correa-Fernández V, et al. Lower health literacy predicts smoking relapse among racially/ethnically diverse smokers with low socioeconomic status. BMC Public Health 2014;14:716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ Couns 2016;99:1079–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Baker D, Gazmararian J, Williams M, et al. Functional health literacy and the risk of hospital admission among medicare managed care enrollees. Am J Public Health 2002;92:1278–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Howard D, Gazmararian J, Parker R. The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am J Med 2005;118:371–7. [DOI] [PubMed] [Google Scholar]
- [8].National Action Plan to Improve Health Literacy. Washington, DC: U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Health.gov. Available at: https://health.gov/communication/hlactionplan/pdf/Health_Literacy_Action_Plan.pdf. Published 2010. Accessed July 6, 2017. [Google Scholar]
- [9].Health Communication and Health Information Technology | Healthy People 2020. Healthy People. Healthypeople.gov. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/health-communication-and-health-information-technology. Published 2017. Accessed July 8, 2017. [Google Scholar]
- [10].Health Literacy: A Prescription to End Confusion. Institute of Medicine (IOM) Committee on Health Literacy. Health Literacy: A Prescription to End Confusion. Nielsen-Bohlman L, Panswer AM, Kindig DA, eds. Washington, DC, National Academies Press; 2004. [PubMed] [Google Scholar]
- [11].Buchbinder R, Batterham R, Ciciriello S, et al. Health literacy: what is it and why is it important to measure? J Rheumatol 2011;38:1791–7. [DOI] [PubMed] [Google Scholar]
- [12].Jordan J, Buchbinder R, Osborne R. Conceptualising health literacy from the patient perspective. Patient Educ Couns 2010;79:36–42. [DOI] [PubMed] [Google Scholar]
- [13].Parker R, Baker D, Williams M, et al. The test of functional health literacy in adults: a new instrument for measuring patient's literacy skills. J Gen Intern Med 1995;10:537–41. [DOI] [PubMed] [Google Scholar]
- [14].Davis T, Long S, Jackson R, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med 1993;25:391–6. [PubMed] [Google Scholar]
- [15].Han HR, Kim J, Kim MT, et al. Measuring health literacy among immigrants with a phonetic primary language: a case of Korean American women. J Immigr Minor Health 2011;13:253–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Nguyen TH, Park H, Han HR, et al. State of the science of health literacy measures: validity implications for minority populations. Patient Educ Couns 2015;98:1492–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Zun LS, Sadoun T, Downey L. English-language competency of self-declared English-speaking Hispanic patients using written tests of health literacy. J Natl Med Assoc 2006;98:912–7. [PMC free article] [PubMed] [Google Scholar]
- [18].Test content for health activities literacy tests. Educational Testing Service. Available at: http://www.ets.org. Published 2006. Accessed July 6, 2017. [Google Scholar]
- [19].Rudd RE. Health literacy skills of US adults. Am J Health Behav 2007;31:S1–8. [DOI] [PubMed] [Google Scholar]
- [20].Osborne R, Batterham R, Elsworth G, et al. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013;13:658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Weiss B. Quick assessment of literacy in primary care: the Newest Vital Sign. Ann Fam Med 2005;3:514–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Osborn C, Weiss B, Davis T, et al. Measuring adult literacy in health care: performance of the newest vital sign. Am J Health Behav 2007;31:S36–46. [DOI] [PubMed] [Google Scholar]
- [23].Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med 2004;36:588–94. [PubMed] [Google Scholar]
- [24].Wallace LS, Rogers ES, Roskos SE, et al. Brief report: screening items to identify patients with limited health literacy skills. J Gen Intern Med 2006;21:874–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Waco Family Medicine Residency Program. Wacofhc.org. Available at: http://www.residency.wacofhc.org/mission-history. Published 2017. Accessed July 15, 2017. [Google Scholar]
- [26].Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav 1997;38:21–37. [PubMed] [Google Scholar]
- [27].Carter JV, Pan J, Rai SN, et al. ROC-ing along: evaluation and interpretation of receiver operating characteristic curves. Surgery 2016;159:1638–45. [DOI] [PubMed] [Google Scholar]
- [28].Farrell TW, Chandran R, Gramling R. Understanding the role of shame in the clinical assessment of health literacy. Fam Med 2008;40:235–6. [PubMed] [Google Scholar]
- [29].Parikh NS, Parker RM, Nurss JR, et al. Shame and health literacy: the unspoken connection. Patient Educ Couns 1996;27:33–9. [DOI] [PubMed] [Google Scholar]
- [30].Wolf MS, Williams MV, Parker RM, et al. Patients’ shame and attitudes toward discussing the results of literacy screening. J Health Commun 2007;12:721–32. [DOI] [PubMed] [Google Scholar]
- [31].Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982;143:29–36. [DOI] [PubMed] [Google Scholar]
- [32].Seligman HK, Wang FF, Palacios JL, et al. Physician notification of their diabetes patients’ limited health literacy: a randomized, controlled trial. J Gen Intern Med 2005;20:1001–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


