Abstract
HIV-positive pregnant and postpartum women’s status disclosure to male sexual partners is associated with improved HIV and maternal and child health outcomes. Yet, status disclosure remains a challenge for many women living with HIV in sub-Saharan Africa, particularly those who are fearful of violence. The objective of the present study is to advance the current understanding of the relationship between intimate partner violence against women and their HIV status disclosure behaviors. We specifically evaluate how the severity, frequency, and type of violence against postpartum HIV-positive women affect status disclosure within married/cohabiting couples. A cross-sectional survey was administered by trained local research assistants to 320 HIV-positive postpartum women attending a large public health center for pediatric immunizations in Lusaka, Zambia. Survey data captured women’s self-reports of various forms of intimate partner violence and whether they disclosed their HIV status to the current male partner. Multiple logistic regression models determined the odds of status disclosure by the severity, frequency, and type of violence women experienced. Our findings indicate a negative dose-response relationship between the severity and frequency of intimate partner violence and status disclosure to male partners. Physical violence has a more pronounced affect on status disclosure than sexual or emotional violence. Safe options for women living with HIV who experience intimate partner violence, particularly severe and frequent physical violence, are urgently needed. This includes HIV counselors’ ability to evaluate the pros and cons of status disclosure among women and support some women’s decisions not to disclose.
Keywords: HIV status disclosure, couples affected by HIV, intimate partner violence, sub-Saharan Africa, Zambia
INTRODUCTION
Disclosure of an HIV-positive status to sexual partners among couples in sub-Saharan Africa has important implications for the health outcomes of the individual living with HIV, their sexual partners, and public health. For the HIV-positive individual, status disclosure is associated with improved social support and reduced feelings of anxiety and perceived stigma [1]. For the sexual partners of HIV-positive individuals, knowing their partner’s HIV status enhances risk awareness, and may promote increased uptake of voluntary HIV counseling and testing (VCT) and safer sex practices [2]. For women living with HIV (WLWH) who are pregnant or breastfeeding, status disclosure to male partners is also linked to health behaviors, such as adherence to antiretroviral therapy (ART) during and after pregnancy, which is critical for prevention of mother-to-child transmission (PMTCT) [3–5].
Despite the potential benefits, HIV status disclosure remains a challenge for many WLWH in African settings. A recent systematic review by Tam, Amzel, and Phelps (2015) showed that only 64% of pregnant/postpartum WLWH disclosed their diagnosis to male partners across multiple African settings. A critical barrier to status disclosure often cited by WLWH is fear of a negative reaction from the male partner, including accusations of infidelity, abandonment, or intimate partner violence (IPV) [6–9]. Indeed, multiple studies have indicated that WLWH are more likely to disclose their HIV status to the male partner if the couple has no history of IPV [10]. There is a lack of understanding, however, regarding how different forms of violence (i.e., emotional, physical, or sexual) or the severity/frequency of IPV may affect HIV-positive women’s decisions regarding status disclosure to male partners around the time of pregnancy.
Zambia has a high prevalence of both HIV among women of reproductive age and violence against women. In the country, 15% of women ages 15-49 years were HIV-positive in 2014 [11] with many women newly diagnosed during pregnancy or postpartum. In addition, almost half of the female population has experienced some form of IPV in their lifetime with 10% reporting physical violence specifically during pregnancy [11]. Although the majority of women testing for HIV (either positive or negative) during antenatal care (ANC) in Zambia report disclosing their status to male partners [11], more research is needed into the interconnecedness between different forms of IPV and lack of status disclosure among pregnant/postpartum WLWH in this setting. This knowledge is critically important for the development of effective interventions that can promote both positive clinical outcomes, such as PMTCT, and the safety of WLWH. The objective of the present study is to establish how different experiences with IPV, including varying levels of frequency/severity and different types of IPV, affect status disclosure to male partners among a clinic-based cohort of postpartum WLWH in Lusaka, Zambia.
METHODS
Participants and Procedures
This study is a secondary analysis of cross-sectional data collected in 2014 from a clinic-based survey within the Maternal and Child Health Department of a large public health center in a low-socioeconomic neighborhood of Lusaka. The original aim of the study was to explore the relationship between gender power dynamics and HIV-positive women’s adherence across the PMTCT cascade of care, including ART adherence during and after pregnancy [12], safe infant feeding [13], and pediatric HIV testing [14]. All of the participants from the parent study are included in our sub-analysis, which expands the previous work by exploring status disclosure to male partners as the outcome of interest. In the prior published analyses using data from the parent study, status disclosure is considered a control variable. The a priori sample size calculation is powered to detect a two-tailed medium-effect odds ratio of 2.74 at a power of 0.80 and alpha of 0.05 using a sample of 320 participants [15, 16].
The clinic where recruitment took place provides ANC, including PMTCT, as well as postpartum care, such as height and weight, pediatric immunizations, vitamin supplements, and deworming treatment. All participants (n=320) were HIV-positive postpartum women who were at least 18 years of age. These women were either married or cohabiting with a male partner. Additionally, study participants had to have at least one biological child between the ages of 3 and 9 months to be eligible. Infant age criterion was selected to capture all of the essential PMTCT protocols, match the immunization schedule in Zambia, and limit recall bias. To ensure the safety of women in abusive relationships, those who attended the clinic with their male partners were excluded from participation. This was, however, extremely rare with only two participants being excluded because the male partner was present for the child’s clinic visit.
Potential participants were approached during the routine pediatric immunizations clinic. Nurses identified eligible mothers using the child’s “Under-Five Card” (i.e., a mother’s copy of her child’s health record that she is required to bring to all health care visits) and asked women who met the inclusion criteria to proceed to a designated area in the health center. Here, trained local research assistants individually briefed potential participants on the study in a private exam room, conducted informed consent, and verbally administered the survey in their preferred language (i.e., English, Bemba, or Nyanja) on paper forms. The response rate for invited women was 85%. Participants provided information about their demographic characteristics; relationship dynamics, including HIV status disclosure and IPV (discussed in detail below); and adherence to various PMTCT protocols. The survey questionnaire was developed by the primary investigator (KH), based on existing validated instruments [17, 18], evaluated by a panel of experts in Lusaka, and pretested during a pilot study in March of 2014.
The study was designed and implemented in accordance with the World Health Organization Ethical and Safety Recommendations for Research on Domestic Violence Against Women (WHO, 2001). Women who reported IPV were offered referrals to a local domestic violence organization in Lusaka for counseling and victim support services. The study was approved by the Colorado Multiple Institutional Review Board (COMIRB) and the Excellence in Research Ethics and Science (ERES) Converge Zambia. Consent forms were translated into local languages and read aloud to each participant. All participants provided written informed consent or a thumbprint (in cases where women had difficulty reading or writing) prior to participating in the survey.
Survey Measures
HIV status disclosure, the main outcome of interest, was measured by asking participants the following binary (yes/no) question: “Have you notified your husband/partner about your HIV status?” IPV perpetrated by current male partner, the main independent variables of interest, was measured using a version of the Revised Conflict Tactics Scale (CTS2). The CTS2 is one of the most widely used IPV measurement tools and has strong reported psychometric properties [19]. The version of the CTS2 used in this study came directly from the Demographic and Health Survey’s Domestic Violence Module [20], which was first developed and standardized in 2000 and has been previously used in numerous settings throughout sub-Saharan Africa, including Zambia [21].
The IPV module contained 12 items with binary response options (e.g., yes/no) and was divided into three subscales (emotional, physical, and sexual IPV) to capture if the participant’s current male partner had perpetrated any of these types of violence against her ever in the relationship. Emotional IPV was measured using three items (e.g., “Does your husband/partner ever say or do something to humiliate you in front of others?”). Physical violence was measured using seven items (e.g., “Does your husband/partner ever slap you?”). Sexual violence was measured using two items (e.g., “Does your husband/partner ever physically force you to have sexual intercourse with him even when you do not want to?”). If a woman answered “yes” to any of the IPV experiences, she was additionally asked how frequently that particular IPV item occurred in the past year, using three possible response choices (often in the past year=3, sometimes in the past year=2, rarely/never in the past year=1). Lastly, we used a four-item scale to capture if women experienced any injuries (e.g., “cuts, bruises, or aches?”) in the course of the current relationship as a result of IPV.
From these data, we created a set of binary dummy and ordinal variables to estimate various dimensions of postpartum women’s experiences with IPV in their current relationship. First, we created a dummy variable (yes/no) to indicate if women ever experienced any form of IPV in the current relationship. Similarly, we created three dummy variables (yes/no) capturing: any physical IPV, any emotional IPV, and any sexual IPV in the current relationship. Lastly, we created a dummy variable (yes/no) indicating if the woman ever experienced any injuries as a result of IPV in the current relationship. We additionally created two ordinal variables to capture the severity and frequency of IPV. First, the total number of IPV events ever experienced in the current relationship was calculated by summing the number of specific IPV events women reported (scale of 0-12 events). We also created a frequency of IPV in the past year score by summing how often each violent event occurred in the past year using an ordered list of possibilities (often=3, sometimes=2, rarely/never=1), yielding a score from 0 (no violent events in the past year) to 36 (experiencing every possible violent event often in the past year).
Household wealth, a standard control variable, was calculated using a list of 21 household assets (e.g., “does your household have (yes/no): a television, a car, electricity,” etc.) [20], which was used to generate a standardized relative wealth index (range: −2.5 to 2.5) using principal component analysis (PCA) [11, 18, 20]. The PCA procedure yields a wealth index that assigns a larger weight to assets that vary the most across households [22]. We also included the following additional control variables: participant’s age (years); parity (number of biological children the woman had birthed); completion of primary education (yes/no), when the woman was diagnosed with HIV (either during the most recent pregnancy or before becoming pregnant), and length of relationship with the current male partner (years). Women also indicated the male partner’s HIV status: male partner also HIV-positive (seroconcordant), male partner HIV-negative (serodiscordant), or male partner’s status unknown. Three dummy variables were created based on these response categories for male partner status and included in the regression models.
Data Analysis
To detect data entry errors, survey data were entered twice into a CSPro database and exported into Stata 12 for analysis. Surveys with more than 50% missing data were not included in the analyses (n=4). Missing data (see Table 1) were imputed using multiple chained equations in Stata 12 (Raghunathan, Lepkowski, Hoewyk, & Solenberger, 2001). A total of 21 auxiliary variables that were either significantly associated with the missing data or considered standard control variables (e.g., age, education, and wealth) were included in the imputation model as auxiliary variables. Through chained imputation, 20 datasets were created and pooled for missing values among the variables of interest. Data converged, indicating that the multiple chained model was a good fit for the dataset (StataCorp, 2009).
Table 1.
Participant Characteristics Stratified by Women’s HIV Status Disclosure to Male Partners
| Total | Disclosed HIV-Positive Status | Did Not Disclose HIV-Positive Status | T-Test/Chi Square Test | N | |
|---|---|---|---|---|---|
| Demographic Characteristics | |||||
| Age (years): mean (SD) | 29.1 (5.8) | 29.0 (5.8) | 30.2 (6.0) | t = 1.06 | 317 |
| Parity: mean (SD) | 3.4 (1.7) | 3.5 (1.8) | 3.3 (1.3) | t = −0.44 | 320 |
| Completed primary education (yes): (%) | 230 (71.8%) | 211 (72.0%) | 19 (73.1%) | χ2 = 0.01 | 319 |
| Diagnosed with HIV during most recent pregnancy (yes): n (%) | 193 (60.3%) | 169 (57.8%) | 24 (88.6%) | χ2 = 9.44** | 320 |
| Standardized wealth index: mean (SD) | 0.0 (1.0) | 0.5 (1.0) | −0.5 (0.8) | t = −2.81 | 310 |
| Length of relationship (years): mean (SD) | 6.7 (5.4) | 6.9 (5.4) | 4.3 (4.4) | t = −2.01* | 301 |
| Male partner HIV status | |||||
| HIV positive (seroconcordant): n (%) | 165 (51.6%) | 164 (56.0%) | 1 (3.9%) | χ2 = 26.0*** | 320 |
| HIV negative (serodiscordant): n (%) | 89 (27.9%) | 86 (29.4%) | 3 (11.5%) | χ2 = 3.8 | 320 |
| Unknown: n (%) | 65 (20.4%) | 43 (14.7%) | 22 (84.6%) | χ2 = 72.0*** | 320 |
| IPV perpetrated by current male partner | |||||
| Experienced any IPV in current relationship (yes): n (%) | 196 (60.1%) | 173 (58.9%) | 23 (83.5%) | χ2 = 6.63* | 319 |
| Total number of IPV events ever experienced in current relationship: mean (SD)a | 1.7 (2.0) | 1.6 (1.9) | 3.5 (2.4) | t = 4.94*** | 317 |
| Ever had injuries as a result of IPV in current relationship (yes): n (%) | 89 (27.8%) | 72 (24.5%) | 17 (64.6%) | χ2 = 19.77*** | 320 |
| Frequency of IPV in the past year score: mean (SD) b | 3.6 (4.3) | 3.3 (4.0) | 7.6 (5.3) | t = 5.22*** | 320 |
| Experienced any physical IPV in current relationship (yes): n (%) | 101 (31.6%) | 84 (28.8%) | 17 (61.5%) | χ2 = 11.89** | 319 |
| Experienced any emotional IPV in current relationship (yes): n (%) | 129 (40.3%) | 114 (38.9%) | 15 (57.7%) | χ2 = 3.50+ | 320 |
| Experienced any sexual IPV in current relationship (yes): n (%) | 110 (34.4%) | 93 (31.9%) | 17 (61.5%) | χ2 = 9.34** | 319 |
| TOTAL: N % | 319 (100%) | 293 (91.7%) | 26 (8.3%) | —— | 320 |
Level of statistical significance:
p<0.10
p<0.05
p<0.01
p<0.001
Range: 0-9
Range: 0-18
Prior to imputation, descriptive statistics captured the mean and standard deviations for interval/ordinal variables, and proportions for binary variables. Next, bivariate analysis explored the association between HIV status disclosure to male partners and our independent and control variables. For the continuous variables, an independent group t-test was conducted. For binary variables, Pearson chi-squared was applied. We subsequently conducted a series of multiple logistic regression analyses using both case-analysis and imputed data to determine the adjusted odds of HIV status disclosure by each measure of IPV, after adjusting for standard control variables (i.e., age, parity, education, and wealth) and variables that were significantly associated with HIV status disclosure in the bivariate models. For the ordinal IPV measures, number of IPV events and frequency of IPV in the past year score, we tested models with both the ordinal measures described above, as well as with categorical versions (shown in figures 1 and 2) with results remaining consistent.
Figure 1.
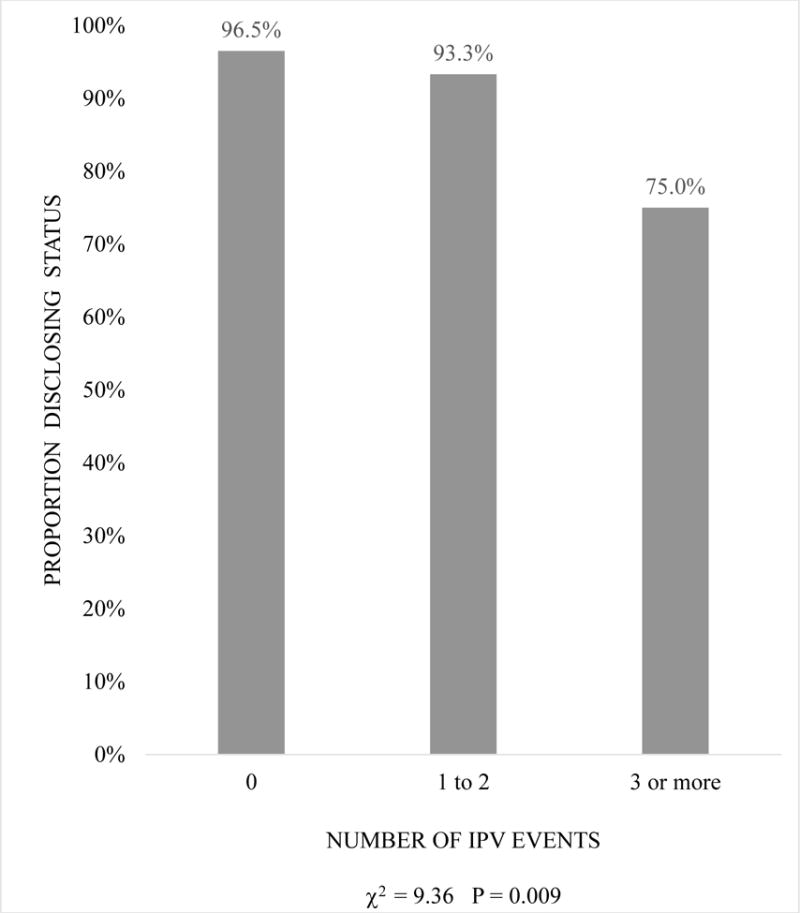
Proportion of Postpartum WLWH Disclosing HIV Status to Male Partners by Number of Violent Events Ever Experienced in Current Relationship
Figure 2.
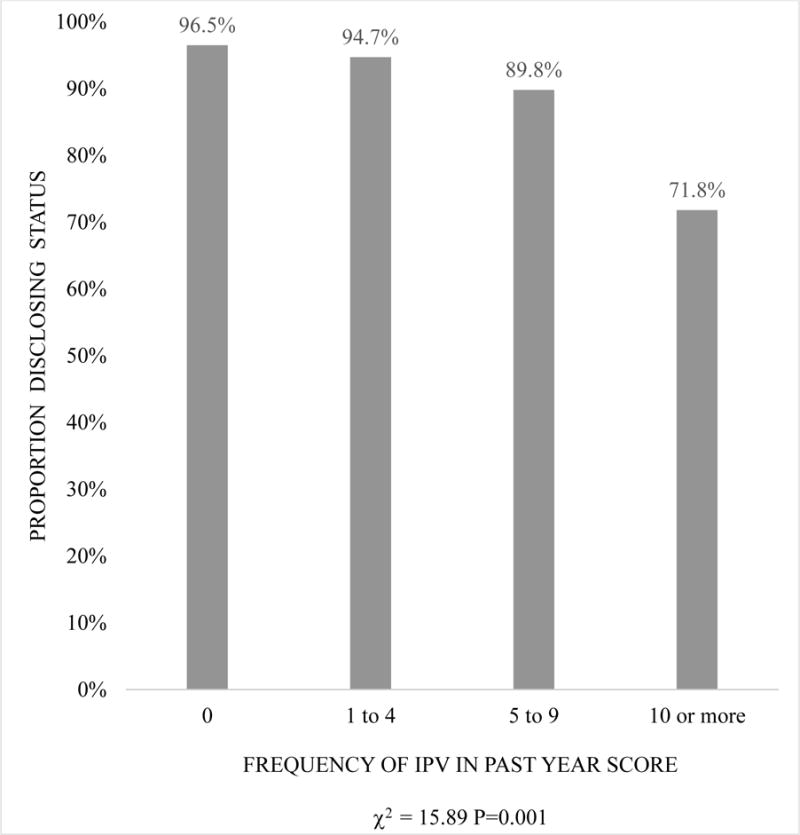
Proportion of Postpartum WLWH Disclosing HIV Status to Male Partners by Frequency of IPV in the Past Year
RESULTS
Table 1 displays participant characteristics stratified by whether or not women disclosed their HIV-positive status to the male partner. On average, the postpartum women in this study were 29 years of age and had three biological children. The majority of women (72%) completed a primary education. The majority of women (60%) were also diagnosed with HIV during their most recent pregnancy (compared to knowing their status before becoming pregnant). Women had been in their current relationship for an average of 7 years and the vast majority (92%) reported disclosing their HIV-positive status to the male partner. The majority (52%) of women were in seroconcordant relationships with a male partner who was also diagnosed as HIV-positive. However, 20% of women reported they did not know their partner’s HIV status (or he had never been tested for HIV). The prevalence of IPV in women’s current relationships was 60%, meaning that these women had experienced at least one IPV event perpetrated by the current male partner at some point in their relationship. On average, women reported a total of 2 violent events in the course of their current relationship and 28% had experienced an injury due to IPV. The average frequency of IPV in the past year score was four (range 0-18). To put this score into perspective, there are four scenarios that could result in a frequency of IPV in the past year score of four: 1) experiencing two violent events often in the past year; 2) experiencing three violent events often and one violent event rarely in the past year; 3) experiencing two violent events sometimes and two violent events rarely in the past year; or 4) experiencing four violent events rarely in the past year. The most common type of IPV women experienced was emotional IPV with 40% of women reporting at least one emotionally violent event in their current relationship, followed by sexual IPV (34%), and lastly, physical IPV (32%).
Table 1 also summarizes the t-test and chi-squared results. Demographic characteristics associated with HIV status disclosure to the male partner include being diagnosed with HIV prior to the most recent pregnancy (χ2 = 9.44; p<0.01) and longer length of the relationship (t = −2.01, p<0.05). In addition, having an HIV-positive male partner (χ2 = 26.0; p<0.001) and knowing the partner’s status (χ2 = 72.0, p<0.001) were also associated with status disclosure. Lastly, all of the IPV measures, with the exception of emotional violence (χ2 = 3.50; p=0.06), were negatively associated with HIV status disclosure: experienced any IPV in current relationship (χ2 = 6.63; p<0.05); total number of IPV events in current relationship (t = 4.94; p<0.001), ever had injuries as a result of IPV in current relationship (χ2 = 19.77; p<0.001), frequency of IPV in the past year score (t = 5.22; p<0.001), experienced physical IPV in current relationship (χ2 = 11.89; p<0.01), and experienced sexual IPV in current relationship (χ2 = 9.34; p<0.01).
Table 2 displays the first set of multiple logistic regression results from the imputed data and the case-analysis for the adjusted odds of HIV status disclosure across different measures of the severity and frequency of IPV. The imputed data and the case-analysis display similar trends with the imputed models providing slightly more statistical power to detect significant relationships. In the imputed models, experiencing any IPV in the current relationship was marginally associated with lower odds of HIV status disclosure (aOR 0.31; 95%CI 0.08 – 1.22; p=0.09). There was, however, a significant association between the number of IPV events a woman experienced from her current male partner and the odds of status disclosure: for each additional IPV event a woman experienced, there was a 23% decrease in the odds that she disclosed her HIV-positive status (aOR 0.77; 95%CI 0.61 – 0.98; p<0.05). This suggests a dose-response relationship, where more violence of any type corresponds to a reduced likelihood of disclosure. Figure 1 highlights this dose-response relationship; women with no IPV events in their current relationship disclosed their HIV status 97% of the time compared to women reporting three or more violent events, who only disclosed their status 75% of the time (c2 =9.36, p<0.01).
Table 2.
Adjusted Odds of HIV Status Disclosure to Male Partners by Frequency of IPV in the Past Year, Number of IPV Events, and Injuries from IPV
| Imputed Models: Adjusted Odds of HIV Status Disclosure aOR (95% CI) |
Case-Analysis Models: Adjusted Odds of HIV Status Disclosure aOR (95% CI) |
|||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| IPV Experiences | N=320 | N=320 | N=320 | N=320 | N=288 | N=287 | N=288 | N=288 |
| Experienced any IPV in current relationship | 0.31+ (0.08 – 1.22) |
— | — | — | 0.32 (0.07 – 1.37) |
— | — | — |
| Total number of IPV events ever experienced in current relationship | — | 0.77* (0.61 – 0.98) |
— | — | — | 0.78+ (0.60 – 1.00) |
— | — |
| Frequency of IPV in the past year score | — | — | 0.89* (0.80 – 0.99) |
— | — | — | 0.90+ (0.80 – 1.01) |
— |
| Ever had injuries as a result of IPV in current relationship | — | — | — | 0.22** (0.07 – 0.67) |
— | — | — | 0.21* (0.06 – 0.73) |
| Controls | ||||||||
| Age | 0.88+ (0.77 – 1.00) |
0.89+ (0.79 – 1.02) |
0.89 (0.78 – 1.02) |
0.89+ (0.78 – 1.02) |
0.90 (0.78 – 1.03) |
0.92 (0.79 – 1.06) |
0.92 (0.79 – 1.06) |
0.92 (0.79 – 1.06) |
| Parity | 1.27 (0.77 – 2.09) |
1.17 (0.70 – 1.96) |
1.16 (0.69 – 1.94) |
1.15 (0.68 – 1.93) |
1.17 (0.69 – 1.98) |
1.06 (0.61 – 1.83) |
1.06 (0.61 – 1.82) |
1.03 (0.60 – 1.78) |
| Completed primary education | 0.70 (0.21 – 2.38) |
0.67 (0.20 – 2.27) |
0.64 (0.19 – 2.19) |
0.83 (0.24 – 2.84) |
0.71 (0.19 – 2.69) |
0.68 (0.18 – 2.57) |
0.64 (0.17 – 2.47) |
0.93 (0.24 – 3.65) |
| Diagnosed with HIV during most recent pregnancy | 0.17* (0.04 – 0.70) |
0.20* (0.05 – 0.81) |
0.19* (0.05 – 0.81) |
0.19* (0.04 – 0.79) |
0.18* (0.03 – 0.90) |
0.19* (0.04 – 0.99) |
0.20+ (0.04 – 1.01) |
0.20+ (0.04 – 1.02) |
| Standardized wealth index | 1.56 (0.89 – 2.72) |
1.11 (0.82 – 2.43) |
1.41 (0.82– 2.43) |
1.23 (0.68 – 2.17) |
1.43 (0.79 – 2.59) |
1.30 (0.72 – 2.34) |
1.29 (0.72 – 2.32) |
1.06 (0.56 – 2.00) |
| Length of relationship | 1.10 (0.95 – 1.28) |
1.11 (0.95 – 1.28) |
1.10 (0.95 – 1.28) |
1.12 (0.96 – 1.30) |
1.09 (0.94 – 1.28) |
1.11 (0.95 – 1.30) |
1.10 (0.94 – 1.29) |
1.13 (0.96 – 1.33) |
| Male partner HIV status: | ||||||||
| HIV positive | ref | ref | ref | ref | ref | ref | ref | ref |
| HIV negative | 0.28 (0.03 – 2.83) |
0.28 (0.03 – 2.83) |
0.28 (0.03 – 2.89) |
0.26 (0.02 – 2.69) |
0.34 (0.03 – 4.00) |
0.35 (0.03 – 4.15) |
0.35 (0.03 – 4.17) |
0.34 (0.03 – 4.14) |
| Unknown | 0.02*** (0.00 – 0.14) |
0.02*** (0.00 – 0.16) |
0.02*** (0.00 – 0.17) |
0.02*** (0.00 – 0.13) |
0.03** (0.00 – 0.21) |
0.03** (0.00 – 0.23) |
0.03** (0.00 – 0.23) |
0.02*** (0.00 – 0.19) |
Level of statistical significance:
p<0.10
p<0.05
p<0.01
p<0.001
The results in Table 2 also indicate a dose-response relationship between the frequency of IPV in the past year score and women’s HIV status disclosure to the male partner (aOR 0.89; 95%CI 0.80 – 0.99; p<0.05). That is, for each one-unit increase in a participant’s frequency of IPV in the past year score, she had 11% lower adjusted odds of disclosing her status. In Figure 2, which displays this dose-response, women with a frequency of IPV in the past year score of zero disclosed their status 97% of the time compared to women with a frequency of IPV score greater than 10, who only disclosed their status 72% of the time (c2 =15.89, p<0.01). Lastly, women who experienced injuries as a result of IPV in their current relationship, another measure of the severity of IPV, had 78% lower adjusted odds of disclosing their HIV-positive status to the male partner (aOR 0.22; 95%CI 0.07 – 0.67; p<0.01), compared to women who did not experience any injuries from IPV.
Table 3 presents the results of the second set of adjusted logistic regressions, which summarized the relationship between women’s HIV-positive status disclosure to male partners and experiencing specific types of IPV (i.e., physical, emotional, or sexual). In the imputed models, only physical IPV in the current relationship remained negatively associated with the odds of HIV status disclosure to the male partner. Women who experienced physical IPV had 68% reduced odds of status disclosure (aOR 0.32; 95%CI 0.11 – 0.95; p<0.05), compared to women who did not experience physical IPV.
Table 3.
Adjusted Odds of HIV Status Disclosure to Male Partners by Specific Types of IPV Experienced in the Current Relationship
| Imputed Models: Adjusted Odds of HIV Status Disclosure aOR (95% CI) |
Case-Analysis Models: Adjusted Odds of HIV Status Disclosure aOR (95% CI) |
|||||
|---|---|---|---|---|---|---|
| IPV Experiences | N=320 | N=320 | N=320 | N=288 | N=288 | N=288 |
| Experienced any physical IPV in current relationship | 0.32* (0.11 – 0.95) |
— | — | 0.32+ (0.10 – 1.07) |
— | — |
| Experienced any emotional IPV in current relationship | — | 0.64 (0.23 – 1.82) |
— | — | 0.99 (0.32 – 3.04) |
— |
| Experienced any sexual IPV in current relationship | — | — | 0.50 (0.17 – 1.44) |
— | — | 0.43 (0.14 – 1.38) |
| Controls | ||||||
| Age | 0.88+ (0.78 – 1.02) |
0.88+ (0.78 – 1.01) |
0.88+ (0.77 – 1.01) |
0.91 (0.79 – 1.05) |
0.89 (0.78 – 1.03) |
0.90 (0.78 – 1.04) |
| Parity | 1.18 (0.70 – 1.98) |
1.23 (0.76 – 2.03) |
1.25 (0.76 – 2.06) |
1.09 (0.63 – 1.87) |
1.18 (0.70 – 1.99) |
1.16 (0.68 – 1.96) |
| Completed primary education | 0.66 (0.19 – 2.22) |
0.74 (0.23 – 2.42) |
0.75 (0.22 – 2.49) |
0.66 (0.18 – 2.50) |
0.78 (0.21 – 2.88) |
0.74 (0.19 – 2.82) |
| Diagnosed with HIV during most recent pregnancy | 0.21* (0.05 – 0.88) |
0.18* (0.04 – 0.72) |
0.18* (0.05 – 0.77) |
0.22+ (0.04 – 1.11) |
0.18 (0.04 – 0.90) |
0.18* (0.03 – 0.89) |
| Standardized wealth index | 1.42 (0.83 – 2.42) |
1.42 (0.83 – 2.44) |
1.48 (0.86 – 2.55) |
1.31 (0.73 – 2.34) |
1.30 (0.74 – 2.31) |
1.38 (0.77 – 2.48) |
| Length of relationship | 1.12 (0.96 – 1.30) |
1.11 (0.96 – 1.28) |
1.10 (0.95 – 1.27) |
1.12 (0.95 – 1.32) |
1.10 (0.94 – 1.28) |
1.09 (0.94 – 1.27) |
| Male partner HIV status: | ||||||
| HIV positive | ref | ref | ref | ref | ref | ref |
| HIV negative | 0.25 (0.02 – 2.55) |
0.26 (0.02 – 2.62) |
0.27 (0.03 – 2.71) |
0.29 (0.02 – 3.43) |
0.34 (0.03 – 3.92) |
0.35 (0.03 – 4.09) |
| Unknown | 0.02*** (0.00 – 0.14) |
0.02*** (0.00 – 0.13) |
0.02*** (0.00 – 0.15) |
0.02*** (0.00 – 0.19) |
0.02*** (0.00 – 0.19) |
0.03** (0.00 – 0.23) |
Level of statistical significance:
p<0.10
p<0.05
p<0.01
p<0.001
Lastly, two control variables were significantly associated with the odds of women disclosing their HIV-positive status to the current male partner in the adjusted logistic regression models (see Tables 2 and 3). First, being diagnosed with HIV during the most recent pregnancy was negatively associated with the adjusted odds of HIV status disclosure in all of the imputed models (aOR 0.17 – 0.21; p<0.05). Second, having a male partner with an unknown HIV status was also strongly associated with lower adjusted odds of women disclosing their status to him in the all of the imputed models and case-analysis models (aOR 0.02 – 0.03; p<0.001), compared to women in seroconcordant relationships whose male partner was also HIV-positive.
DISCUSSION
In this study, the vast majority (92%) of WLWH reported disclosing their HIV-positive status to their current male partner, which is similar to disclosure rates observed in other similar settings among long-term committed couples. In Zimbabwe, for instance, Shamu et al. (2014) found that 89% of HIV-positive women disclosed their status to their male partner [23]. Importantly, the postpartum WLWH in the present study who knew they were HIV-positive for longer periods of time (i.e., before their most recent pregnancy) were more likely to disclose their status to their current male partner, compared to more recently diagnosed women. This finding highlights that newly diagnosed women often need time to psychologically adjust prior to engaging in optimal health behaviors, potentially including notifying significant others of their HIV diagnosis [24, 25]. This finding also underscores the importance of quality counseling, particularly for newly diagnosed women.
More effort should be given to developing effective social interventions that shorten the duration of time it takes pregnant/postpartum WLWH to inform male partners of their status, as well as assist couples in mutual status disclosure. In the present study, having a male partner with an unknown HIV status dramatically reduced the odds of women disclosing their positive status to him, compared to women whose male partner was known to also be living with HIV. One promising intervention is home-based couples HIV counseling and testing (CHCT), which has the potential to serve as an acceptable and safe method to assist couples with mutual HIV status disclosure inside the privacy of their homes assisted by a trained counselor [26, 27].
Severe IPV against HIV-positive women, however, may prevent women from participating in interventions such as CHCT if they are fearful about a violent reaction from the male partner, regardless of the testing location. In the present study, we found strong evidence of a negative relationship between the severity/frequency of IPV against WLWH and the odds of HIV status disclosure to male partners. For each violent event a woman experienced in her current relationship, she had signifincatly reduced odds of status disclosure; this was also true with respect to the frequency of IPV in the past year score. To our knowledge, this is the first study to report a dose-response relationship between the number of IPV events and frequency of IPV in the past year and non-disclosure to male sexual partners among WLWH in an African setting.
An additional measure for the severity of IPV, experiencing any injuries as a result of IPV, also showed a strong negative relationship with status disclosure. Hatcher et al. (2014) report that disclosure among pregnant/postpartum women can lead to IPV because it causes relationship conflict, which is often related to perceived infidelity of women and the notion that women have brought the disease into the relationship [28]. Therefore, it is understandable that women with a history of severe and frequent IPV would be less likely to disclose their HIV-positive status because of the fear – and likely potential real repurcussion – of the male partner having a violent reaction that could result in injury.
An additional important finding from the present study is that not all forms of IPV are equally detrimental to women’s status disclosure to male partners. Emotional and sexual violence appear to have a much less pronounced affect on status discosure compared to physical IPV. The WLWH in this study who reported experiencing physical IPV had reduced odds of disclosing their HIV status to their current male partner. This relationship was not observed, however, for women who experiened emotional or sexual IPV after adjusting for control variables, inlcuding the male partner’s HIV status. As noted above, women who expereinced injuries from IPV were also less likely to disclose their status. Given these combined findings, we infere that fear of bodily harm is a major deterrent to male partner HIV status disclosure among postpartum WLWH.
Based on these findings, we predict that non-disclosure of an HIV-positive status to male partners among WLWH may be a marker for problematic aspects within sexual relationships, such as severe physical IPV [29]. Consequently, we question whether all WLWH should be told to disclose their HIV-positive status to male partners, since this could jeopardize their safety, in some cases. Standard counseling protocols, during ANC in particular, should screen WLWH for IPV and focus on helping them identify the pros and cons of disclosure and supporting some women’s decisions not to disclose [6, 29, 30]. Additionally, health care workers within ANC and maternal and child health settings should be equipped to offer women in abusive relationships referrals to local organizations that provide services, such as safe havens and legal counseling.
Two recent trials from sub-Saharan Africa provide support for incorporating screening for IPV into HIV testing services and training counselors to facilitate discussions about disclosure around women’s risk of IPV: The Safe Homes and Respect for Everyone Trail in Uganda [31] and the South Africa HIV/AIDS Antenatal Post-Test Support Study [32]. Unfortunately, with the exception of these two programs, evidence-based interventions that facilitate safe HIV status disclosure to male partners among women who fear or experience IPV are lacking in sub-Saharan Africa [30]. The present study highlights the need for increased effort into developing effective IPV screening procedures during ANC and postpartum care, as well as interventions that can promote both positive health behaviors and the safety of WLWH who are experincing severe IPV.
The findings of this study should be interpreted within its limitations. First, the study was cross-sectional and could not establish causality or the timing of events. Therefore, we were unable to determine if IPV or status disclosure/lack of status disclosure occurred first. Second, the sample was recruited from a maternal child health clinic, which may introduce selection bias. Women in the study may have different outcomes with respect to IPV than women who do not present for maternal child health care. This sample was also a convenience sample and as such, the results may not be generalizable outside of low-socioeconomic settings in urban Zambia. Third, the results were based on women’s self-reports, which are vulnerable to recall and social desirability biases. Women may have over-reported status disclosure to male partners because they believed this is something they should do. Additionally, rates of HIV disclosure to male partners in our sample may be higher than in the general population of WLWH because all participants were either married or cohabiting with a male partner. Women in these types of long-term committed relationships are more likely to disclose their HIV status than women in less committed sexual relationships [33]. Lastly, quantifying the severity and frequency of IPV is challenging using available validated instruments and our variables for these constructs are restricted by the quality of the input measures. We recommend future research explore additional survey measures to advance the measurement of IPV, particularly the severity and frequency of IPV.
CONCLUSIONS
This study indicates that the severity, frequency, and type of IPV against postpartum WLWH influence the likelihood of HIV status disclosure to male partners. Women who experienced more severe and frequent IPV had reduced odds of HIV status disclosure to their current male partner. Physical IPV, in particular, appears to be the type of violence that is the largest deterrent of status disclosure. Non-disclosure among WLWH, in some instances, may indicate an unsafe home environment. Safe options for women in these violent relationships are urgently needed. This could include training HIV counselors to help women evaluate the pros and cons of disclosure and supporting some women’s decisions not to disclose. Programs that integrate screening for IPV into HIV testing services and training counselors to facilitate discussions with women based on their risk of IPV should also be further evaluated in sub-Saharan Africa. Still, the authors recognize that identifying IPV and providing disclosure support to women in abusive relationships is not enough, since this merely addresses one symptom of a much larger problem. Interventions to prevent IPV, and empower and support women who wish to improve or leave abusive relationships are also urgently needed.
Acknowledgments
The authors would like to thank Dr. Yusuf Ahmed, Christine Chewe Sakala, Grace Lungeani Phiri, Franklin Munsanje, and Bibi Lambert Manda for their contribution to the study. Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health (Award Number F31MH107348) and the University of Colorado Center for Global Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Compliance with Ethical Standards:
This study was funded by the National Institute of Mental Health of the National Institutes of Health (Award Number F31MH107348) and the University of Colorado Center for Global Health. Dr. Hampanda declares that she has no conflict of interest. Dr. Rael declares that she has no conflict of interest. All procedures performed involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. The study was approved by the Colorado Multiple Institutional Review Board (COMIRB) and the Excellence in Research Ethics and Science (ERES) Converge Zambia. Informed written consent (or a thumbprint) was obtained from all individual participants included in the study.
Footnotes
Conflict of interest
The authors declare no conflicting interests.
References
- 1.Maman S. (NIMH Project Accept/HPTN 043).HIV Status Disclosure to Families for Social Support in South Africa. 2014;26(2):226–32. doi: 10.1080/09540121.2013.819400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matthews C, et al. Disclosure of HIV status and its consequences. South African Medical Journal. 1999;89:1238. [PubMed] [Google Scholar]
- 3.Peltzer K, et al. Promoting male involvement to improve PMTCT uptake and reduce antenatal HIV infection: a cluster randomized controlled trial protocol. BMC Public Health. 2011;11:778. doi: 10.1186/1471-2458-11-778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hampanda KM. Intimate partner violence and HIV-positive women’s non-adherence to antiretroviral medication for the purpose of prevention of mother-to-child transmission in Lusaka, Zambia. Social Science & Medicine. 2016;153:123–130. doi: 10.1016/j.socscimed.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stirratt MJ, et al. The role of HIV serostatus disclosure in antiretroviral medication adherence. AIDS Behav. 2006;10(5):483–93. doi: 10.1007/s10461-006-9106-6. [DOI] [PubMed] [Google Scholar]
- 6.Medley A, et al. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: Implications for prevention of mother-to-child transmission programmes. Bulletin of the World Health Organization. 2004;82(4):299–307. [PMC free article] [PubMed] [Google Scholar]
- 7.Etiebet MA, et al. Integrating prevention of mother-to-child HIV transmission into antenatal care: learning from the experiences of women in South Africa. AIDS Care. 2004;16(1):37–46. doi: 10.1080/09540120310001633958. [DOI] [PubMed] [Google Scholar]
- 8.Msellati P. Improving mothers’ access to PMTCT programs in West Africa: a public health perspective. Soc Sci Med. 2009;69(6):807–12. doi: 10.1016/j.socscimed.2009.05.034. [DOI] [PubMed] [Google Scholar]
- 9.Mucheto P, et al. Determinants of nondisclosure of HIV status among women attending the prevention of mother to child transmission programme, Makonde district, Zimbabwe, 2009. Pan Afr Med J. 2011;8:51. doi: 10.4314/pamj.v8i1.71169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tam M, Amzel A, Phelps BR. Disclosure of HIV serostatus among pregnant and postpartum women in sub-Saharan Africa: a systematic review. AIDS Care. 2015;27(4):436–50. doi: 10.1080/09540121.2014.997662. [DOI] [PubMed] [Google Scholar]
- 11.CSO. Zambia Demographic and Health Survey 2013–14. Central Statistical Office, Ministry of Health, and ICF International; Rockville, Maryland, USA: 2014. [Google Scholar]
- 12.Hampanda K. Intimate partner violence and HIV-positive women’s non-adherence to antiretroviral medication for the purpose of prevention of mother-to-child transmission in Lusaka, Zambia. Soc Sci Med. 2016;153:123–30. doi: 10.1016/j.socscimed.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hampanda K. Intimate Partner Violence Against HIV-Positive Women is Associated with Sub-Optimal Infant Feeding Practices in Lusaka, Zambia. Maternal and Child Health Journal. 2016:1–8. doi: 10.1007/s10995-016-2087-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hampanda KM, Nimz AM, Abuogi LL. Barriers to uptake of early infant HIV testing in Zambia: the role of intimate partner violence and HIV status disclosure within couples. AIDS Res Ther. 2017;14(1):17. doi: 10.1186/s12981-017-0142-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen HN, Cohen P, Chen S. How Big is a Big Odds Ratio? Interpreting the Magnitudes of Odds Ratios in Epidemiological Studies. Communications in Statistics-Simulation and Computation. 2010;39(4):860–864. [Google Scholar]
- 16.Faul F, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavioral Research Methods. 2007;39(2):175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 17.Simoni JM, et al. Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS and behavior. 2006;10(3):227–45. doi: 10.1007/s10461-006-9078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Statistical Office and ICF Macro. Malawi Demographic and Health Survey 2010. NSO and ICF Macro; Zomba, Malawi, and Calverton, Maryland, USA: 2011. [Google Scholar]
- 19.Straus MA, et al. The revised Conflict Tactics Scales (CTS2) - Development and preliminary psychometric data. Journal of Family Issues. 1996;17(3):283–316. [Google Scholar]
- 20.CSO. Zambia Demographic and Health Survey 2007. Central Statistical Office (CSO), Ministry of Health (MOH), Tropical Diseases Research Centre (TDRC), University of Zambia, & Macro International Inc.; Calverton, Maryland, USA: 2009. [Google Scholar]
- 21.MacQuarrie KL, Winter R, Kishor S. Population Association of America Annual Meeting. Boston, MA: 2014. Spousal Violence in Sub-Saharan Africa: Structure, Forms, and Levels. [Google Scholar]
- 22.Filmer D, Pritchett L. Estimating Wealth Effect Without Expenditure Data or Tears: An Application to Educational Enrollments in States of India. Demography. 2001;38:115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 23.Shamu S, et al. Intimate partner violence after disclosure of HIV test results among pregnant women in Harare, Zimbabwe. PLoS One. 2014;9(10):e109447. doi: 10.1371/journal.pone.0109447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kiula ES, Damian DJ, Msuya SE. Predictors of HIV serostatus disclosure to partners among HIV-positive pregnant women in Morogoro, Tanzania. BMC Public Health. 2013;13:433. doi: 10.1186/1471-2458-13-433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Antelman G, et al. Predictors of HIV-1 serostatus disclosure: a prospective study among HIV-infected pregnant women in Dar es Salaam, Tanzania. AIDS. 2001;15(14):1865–74. doi: 10.1097/00002030-200109280-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walcott MM, et al. Facilitating HIV status disclosure for pregnant women and partners in rural Kenya: a qualitative study. BMC Public Health. 2013;13:1115. doi: 10.1186/1471-2458-13-1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Osoti AO, et al. Home visits during pregnancy enhance male partner HIV counselling and testing in Kenya: a randomized clinical trial. AIDS. 2014;28(1):95–103. doi: 10.1097/QAD.0000000000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hatcher AM, et al. Bidirectional links between HIV and intimate partner violence in pregnancy: implications for prevention of mother-to-child transmission. J Int AIDS Soc. 2014;17:19233. doi: 10.7448/IAS.17.1.19233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maman S, et al. Diagnosis and Disclosure of HIV Status: Implications for Women’s Risk of Physical Partner Violence in the Postpartum Period. J Acquir Immune Defic Syndr. 2016;72(5):546–51. doi: 10.1097/QAI.0000000000001012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kennedy CE, et al. Safer disclosure of HIV serostatus for women living with HIV who experience or fear violence: a systematic review. J Int AIDS Soc. 2015;18(6 Suppl 5):20292. doi: 10.7448/IAS.18.6.20292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wagman JA, et al. Effectiveness of an integrated intimate partner violence and HIV prevention intervention in Rakai, Uganda: analysis of an intervention in an existing cluster randomised cohort. Lancet Glob Health. 2015;3(1):e23–33. doi: 10.1016/S2214-109X(14)70344-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maman S, et al. Efficacy of enhanced HIV counseling for risk reduction during pregnancy and in the postpartum period: a randomized controlled trial. PLoS One. 2014;9(5):e97092. doi: 10.1371/journal.pone.0097092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jasseron C, et al. Non-disclosure of a pregnant woman’s HIV status to her partner is associated with non-optimal prevention of mother-to-child transmission. AIDS Behav. 2013;17(2):488–97. doi: 10.1007/s10461-011-0084-y. [DOI] [PubMed] [Google Scholar]


