Abstract
The U.S. physician-scientist (PS) workforce is invaluable to the nation’s biomedical research effort. It is through biomedical research that certain diseases have been eliminated, cures for others have been discovered, and medical procedures and therapies that save lives have been developed. Yet, the U.S. PS workforce has both declined and aged over the last several years. The resulting decreased inflow and outflow to the PS pipeline renders the system vulnerable to collapsing suddenly as the senior workforce retires. In November 2015, the Alliance for Academic Internal Medicine hosted a consensus conference on the PS workforce to address issues impacting academic medical schools, with input from early-career PSs based on their individual experiences and concerns. One of the goals of the conference was to identify current impediments in attracting and supporting PSs and to develop a new set of recommendations for sustaining the PS workforce in 2016 and beyond. This Article reports on the opportunities and factors identified and presents five recommendations designed to increase entry into the PS pipeline and nine recommendations designed to decrease attrition from the PS workflow.
The United States is currently the world’s leader in biomedical research,1 due in large measure to the contributions of the nation’s physician-scientist (PS) workforce.2–5 PSs are estimated to account for only 1.5% of the nation’s total physician workforce;5 however, they are invaluable to the nation’s biomedical research effort.5–13 Because of their training, PSs are a “vital force in transforming clinical observations into testable research hypotheses and translating research findings into medical advances.”10 It is through biomedical research that certain diseases have been eliminated, cures for others have been discovered, and medical procedures and therapies that save lives have been developed.1–3,14,15 Such discoveries have led to the lengthening of life spans, quality of life improvements, and the betterment of public health throughout the world.1–7,13–15
Importantly, the advances made thus far through biomedical research have positioned the PS workforce to make greater contributions to the enhancement of human health at an increasingly faster pace. The Human Genome Project, which began in 1989, changed the landscape for conducting research and ushered in an era of sharing data and using multidisciplinary approaches to address health issues.16 It also opened the doors to projects based on team science, big data, and precision medicine. As a result of these three initiatives, the PS workforce is able to implement large-scale, coordinated biomedical research programs, such as the Brain Research through Advancing Innovative Neurotechnologies Initiative, which is designed to better understand the brain and treat its disorders.4,17 Another example of this is the Precision Medicine Initiative Cohort Program, a longitudinal study of one million volunteers, which will enhance understanding of microbiome science, using mobile health technologies to better understand the pharmacogenetics of disease and empowering participants to improve their own health.4,18 As a final example, there is the National Cancer Moonshot, which uses big data to accelerate the ability to prevent, detect, and treat all types of cancer.4,19
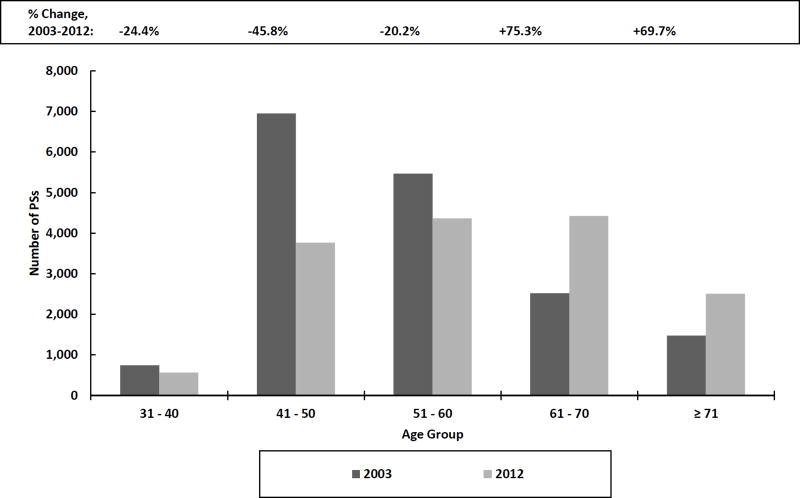
Concerns about sustaining the nation’s PS workforce have been publicly voiced by policymakers and others for the past four decades,5–13 and those concerns are growing in scope and intensity.5–13,20 The size of the PS workforce has declined over the past several years,5 as young physicians choose to focus their careers on being clinicians or clinician-educators rather than PSs. Perhaps of even greater concern is the aging of the current PS workforce. During the ten-year period between 2003 and 2012, the number of PSs aged 60 or younger declined, while the number of those aged 61 or older rose (see Figure 1).5 These data are striking; they suggest (1) the entry and sustained engagement of new PSs into the workforce are in unprecedented decline and (2) senior members of the workforce have postponed retirement. In terms of a PS pipeline model, the decreased inflow and outflow renders the system vulnerable to collapsing suddenly as the senior workforce retires.
Figure 1.
Numbers and percentage changes of the U.S. physician-scientist workforce by age group, 2003–2012. Adapted from Chapters 2 and 3 of National Institutes of Health, Physician-Scientist Workforce (PSW) Report 2014 (available at http://report.nih.gov/workforce/psw/index.aspx).
During 2007 and 2008, the Association of Professors of Medicine (APM) and the Association of American Medical Colleges (AAMC) held a series of conferences resulting in published and disseminated recommendations to expand the pool of funds to retain and foster the careers of young PSs, improve the approach for mentorship of young PSs, promote the advancement of women PSs, and identify and foster the career development of future PSs.12,13
In response to growing concerns about existing National Institutes of Health (NIH) support for PSs, in 2014, Director Francis Collins charged a Physician-Scientist Workforce Working Group to assess the current mechanisms of career support and make recommendations for improvement. In June 2014, the working group issued its report with a series of recommendations that, among other things, urged the NIH to sustain strong training of PSs, shift the balance in federally funded postdoctoral training for physicians to include more individual fellowships, continue to mitigate the gap in award rates between new and established investigators, and adopt rigorous tools to assess the strength of the PS workforce.5
The working group also estimated, to maintain the nation’s current workforce of approximately 14,000 PSs, “about 1,000 individuals will need to enter the pipeline each year.”5 (This calculation assumes half of those who “enter the pipeline will not succeed.”)5 This projection carries with it significant weight, since this could threaten the nation’s role as the global leader in biomedical research, as in 2015, Moses et al21 noted, if current trends continue, China will assume this role within the next ten years.
In November 2015, the Alliance for Academic Internal Medicine (AAIM) hosted a consensus conference, Re-examining the Physician Investigator Workforce: New and Evolving Areas of Research and Pathways to Success in Academic Institutions. The AAIM is a consortium of five organizations: the APM, Association of Subspecialty Professors, Association of Program Directors in Internal Medicine, Clerkship Directors in Internal Medicine, and Administrators of Internal Medicine. The focus of this conference was different than the charge given to the NIH Physician-Scientist Workforce Working Group—that is, while the major concern of the working group was to address issues impacting NIH programs and policies, the major concern of the AAIM consensus conference was to address issues impacting academic medical schools, with input from early-career PSs based on their individual experiences and concerns.
The conference provided an opportunity for thought-leaders and early-career PSs to discuss a series of critical topics relating to the early identification of individuals with a potential for serious engagement in biomedical research, as well as optimal mechanisms for developing the careers of these individuals. Additionally, one of the goals of the conference was to identify current impediments to attracting and supporting PSs and to develop a new set of recommendations for sustaining the PS workforce in 2016 and beyond.
More than 100 individuals attended the conference, representing a cross section of academic administrators, department chairs, program directors, and early-career PSs (see below), as well as representatives from national foundations, the NIH, the National Academy of Medicine, and the pharmaceutical industry. Fourteen early-career PSs attended the conference, representing ten academic medical centers. All of them were recipients of either an NIH mentored career development award or a Department of Veterans Affairs (VA) career development award. All of them were MDs, three had additional master’s-level degrees, and none had a PhD.
The conference included five plenary presentations on key topics to focus discussion during its ten breakout sessions. Each breakout session developed a series of recommendations targeted to academic health leaders and to the NIH and other funding agencies, with the goal of sustaining and potentially expanding the nation’s PS workforce. The recommendations from each breakout session were then presented to all of the conference attendees. Although there were slight differences of opinion among the conference participants on certain recommendations, the recommendations included in this article are those on which the conference reached unanimous consensus and which were subsequently approved by the AAIM Board of Directors. These recommendations are categorized within two major strategies: (1) increasing entry into the PS pipeline and (2) reducing attrition from the PS workforce (see List 1).
List 1.
Recommendations of the Alliance for Academic Internal Medicine Consensus Conference on the PS Workforce, November 2015
Increasing entry into the PS pipeline
|
Reducing attrition from the PS workforce
|
Abbreviations: PS indicates physician-scientist; NIH, National Institutes of Health; VA, Department of Veterans Affairs; P&T, promotion and tenure.
For the purposes of this consensus statement, PSs were defined as physicians who devote the majority of their professional effort to a defined area within the broad continuum of biomedical research (inclusive of basic, translational, clinical, epidemiological, outcomes, and medical educational research) conducted in academic institutions, government agencies, industry, and independent research centers and institutes. Many of these individuals have a professional degree in the sciences, in addition to an MD, and continue to provide patient care in their capacity as clinicians.
Opportunities for Increasing Entry Into the PS Pipeline
Developing and implementing strategies to increase the number of PSs in the U.S. workforce is essential. Opportunities to achieve this goal include facilitating better and early promotion of the value of biomedical research, increasing the diversity of the PS workforce, using role models and mentors to increase diversity, and streamlining the PS training process and expanding research training opportunities.
Facilitating better and early promotion of the value of biomedical research
It is important to promote the value of biomedical research as early as elementary school—while children’s brains are still being developed. Despite a focus on implementing programs to increase students’ skills in science, technology, engineering, and mathematics (STEM), the United States is not ranked in the top 20 on science scores from standardized tests among industrialized nations.22 Allen and Kamen23 argue this low ranking can, in part, be attributed to the nation as a whole placing greater value on its athletes and entertainers than it does on research and innovation. Collaborations between government agencies, community-based organizations, private-sector research organizations, and schools are necessary to effectively promote both the value of biomedical research and the goals of existing STEM programs.
Increasing the diversity of the PS workforce
Data compiled by the AAMC demonstrate a lack of diversity in the PS pipeline. In 2015, women accounted for 47.8% of those matriculating into medical school;24 however, for each of the past five years, they have consistently accounted for between 37% and 38% of those enrolled in the nation’s MD/PhD programs.25 The lower representation of women in the MD/PhD pipeline reflects both fewer female applicants to start with and greater levels of attrition among women.26–28 There are several factors reported by women as to why they are less likely to pursue the MD/PhD career path, which include concerns about child rearing or other family responsibilities; a sense of bias in the workplace resulting in the perception that there is a need to “outcompete” relative to male counterparts; encountering, on multiple fronts, a lack of encouragement to become a PS; and a lack of role models.27–31
The pipeline for racial/ethnic underrepresented groups also needs to be expanded.8,32 Of the 616 graduates of MD/PhD programs in the United States during the 2014–2015 academic year, only 79 (12.8%) reported themselves as being from a racially/ethnically underrepresented group: 26 (4.2%) self-identified as black or African American; 12 (1.9%) as Hispanic, Latino, or of Spanish origin; and 41 (6.7%) as multiple race/ethnicity.33
Additionally, while large numbers of talented and aspiring PSs from other countries attempt to enter research training in the United States, only a small percentage of them are successful in entering the nation’s PS workforce.5 Of the 626 matriculates to the nation’s MD/PhD programs in 2015, only 16 (2.6%) came from countries outside the United States.34 This small number of international matriculates can be partially explained by funding restrictions imposed on slightly less than one-half of the nation’s MD/PhD programs—that is, the federally funded Medical Scientist Training Programs (MSTPs) are open only to U.S. citizens and permanent residents of the United States. Facilitating the recruitment and retention of members from diverse populations, including efforts to enhance opportunities for international students to enter and remain in the United States, could be an effective strategy for increasing the PS workforce.
Using role models and mentors to increase diversity
Role models and mentors function differently, and both are important to increasing entry into the PS pipeline. Role models, according to Cruess et al,35 can “inspire and teach by example.” Role models can be, for example, sports heroes, celebrities, or PSs, and their impact on others can occur in an elementary school classroom as easily as on a television show or during a Grand Rounds lecture.
Exposure to role models is key. Qualitative research of racially/ethnically underrepresented high-school students revealed many had never had interactions with a PS.30,36 They voiced this as an underlying reason for why they did not consider a research career. Furthermore, similar research conducted on MD/PhD medical students indicated exposure to role models as early as middle- and/or high-school influenced their decisions to enter a research career.5,36 Students spoke of the role models they encountered during their science courses, exposure to PSs in their families, and exposure to professionals during a family health crisis. These studies emphasize the critical importance of role models in addressing racial/ethnic disparities in the MD/PhD pipeline.
Mentors differ from role models, according to Paice et al,37 in that a “mentor is actively engaged in an explicit two way relationship” with a trainee or a less-experienced colleague. It is “a relationship that evolves and develops over time and can be terminated by either party.”37 Programs such as the National Research Mentoring Network (NRMN) exist to offer mentoring not only in specific areas of inquiry but also in areas of professional development. Some of the NRMN’s programs “emphasize the benefits and challenges of diversity, inclusivity and culture within mentoring relationships, and more broadly the research workforce.”38
Streamlining the PS training process and expanding research training opportunities
Preparation for a career in biomedical research is a lengthy process requiring well over a decade of undergraduate, medical school, and postgraduate training, which may include formal graduate education in a scientific discipline. To expedite this process, combined MD/PhD curricula (including federally funded MSTPs) were developed with the idea of better integrating and expediting medical and research training during medical school. The results of a national survey from 2014 show these programs have had success with >80% of MD/PhD program graduates pursuing research-oriented careers.39 As an alternative to MSTP enrollment (a commitment of over seven years),39 a subset of medical students take advantage of formal research tracts, which offer enrollees a one-year mentored research experience during medical school (with institutional or external funding support). Limited anecdotal data supports the effectiveness of some of these formal research tracts.40,41
After gaining research experience in medical school, many graduates opt to complete their professional education with a lengthy period of postgraduate clinical and research training. To expedite this process, supplemental mechanisms have been developed to streamline this postdoctoral experience. One such approach, sanctioned by the American Board of Internal Medicine, is a residency research pathway which combines expedited clinical training (and often subspecialty fellowship) with three years of mentored postdoctoral research. Despite a shortened duration of clinical training (two years instead of three), the clinical competency (as measured by board exam pass rate) of these graduates was not sacrificed,42 and more than 80% went on to pursue funded biomedical research.43 Other medical specialty boards (e.g., pediatrics and pathology) have sanctioned similar streamlined postdoctoral training pathways. Finally, since not all physicians with a budding interest in research have completed graduate-level scientific training prior to or during medical school, several research-intensive medical schools have developed formal postdoctoral research training programs (often leading to a MS or PhD degree) to provide this rigorous training to a select group of committed physicians who are in the later stages of clinical training or who are junior faculty.44–46
Recommendations Aimed at Increasing Entry Into the PS Pipeline
The AAIM consensus conference recommendations for increasing entry into the PS pipeline were to (1) promote to young people the value of biomedical research and the important and unique role that PSs play in biomedical advances; (2) facilitate the recruitment and retention of members from diverse populations as PSs through wide-scale implementation of programs that provide access to a network of role models and mentors; (3) enhance opportunities for international PSs to enter and remain in the United States as members of the nation’s workforce; (4) promote efficiency and curricular best practices in the training of PSs; and (5) enhance undergraduate and postgraduate research training opportunities for trainees who do not matriculate into MD/PhD programs (List 1).
Promote to young people the value of biomedical research and the important and unique role that PSs play in biomedical advances
Innovative educational interventions should be established to provide enrichment in science and math as well as to provide support for young learners, especially those from disadvantaged backgrounds. To this end, collaborations between government agencies, community-based organizations, private-sector research organizations, and schools should be encouraged.
Facilitate the recruitment and retention of members from diverse populations as PSs through wide-scale implementation of programs that provide access to a network of role models and mentors
Creating a network of role models, comprising PSs and other professionals, to routinely visit K–12 and undergraduate classes would help expose students to the value of biomedical research and its viability as a career. Similarly, programs such as the NRMN should be widely used to recruit and retain members from diverse populations as they pursue training as a PS.
Enhance opportunities for international PSs to enter and remain in the United States as members of the nation’s workforce
Research awards and grants are frequently dependent on residency status. Universities sponsoring foreign medical school graduates’ postdoctoral studies should provide assistance with applications for permanent residence in the United States. Additionally, the NIH should work with other government agencies to amend policies on eligibility requirements for its National Research Service Award fellowships, training grants, and career development awards to include graduates of foreign medical schools who have been admitted to the United States for postgraduate study but who have not yet been granted permanent resident status.
Promote efficiency and curricular best practices in the training of PSs
Trainees who have demonstrated a commitment to careers in research should be strongly encouraged to take full advantage of educational initiatives that shorten and streamline the training process, such as formal MD/PhD programs during medical school and coordinated residency/subspecialty research pathways during postgraduate training. Continued NIH funding for MSTPs should be provided.
Enhance undergraduate and postgraduate research training opportunities for trainees who do not matriculate into MD/PhD programs
Medical students who have an interest in research but who are not enrolled in a formal MD/PhD program should consider participating in a one-year mentored research experience. Clinically trained physicians who develop an interest in pursuing research later in their professional education (e.g., subspecialty fellowship) or as junior faculty should consider participating in formal research training opportunities that may lead to a master’s and/or doctoral degree. Currently, there is limited published data on the effectiveness of these undergraduate and postgraduate training programs,40,41,44–46 so comprehensive surveys of these alternative research curricula (including content, mechanisms of support, and career outcomes of graduates) should be conducted by relevant professional organizations, such as the AAIM or AAMC, and a mechanism for program leaders to convene and exchange best practices should be provided.
Factors to Address to Reduce Attrition From the PS Workforce
Many PSs, especially those in the early and middle stages of their careers, leave behind their original plans to pursue biomedical research opportunities to enter full-time clinical practice. Reasons for attrition are numerous and complex; however, there are identifiable factors that can be causally linked to the attrition of PSs from academia, including inadequate mentoring, a narrow perception of success as a PS, increasing competition for external support, financial pressures, inadequate institutional support, and difficulties with work-life balance.
Inadequate mentoring
Achieving success as an independently funded PS can be challenging. Strong, active mentoring is a crucial element of that success.43 While the mentor-apprentice dyad has been the traditional model of mentorship, several institutions have developed initiatives designed to provide centralized oversight, mentorship support, and career development. Established researchers, while having the expertise to perform research, may require additional educational support to develop the skillset needed to actively mentor an apprentice. Training programs for research mentors have been shown to be effective.47–49 Such programs should be implemented in all medical schools and should include formalized training in areas such as career negotiation, grant-writing, publication of manuscripts, and work-life balance.47 Home institutions, the NIH, and other funding agencies should allocate adequate resources to mentors in terms of both time and compensation.
A narrow perception of success as a PS
A widely-held view is that a successful PS is funded by the NIH as a principal investigator for bench or early translational research.50 This notion does not take into account the broader definition of a PS as posited by the NIH and others5 nor does it take into account the evolution occurring within the research arena that requires multidisciplinary research teams to use big data and advance precision medicine initiatives. Nonetheless, these antiquated notions of what constitutes a successful PS continue to pose the possibility of negative career consequences when it comes to decisions about research funding and promotion and tenure (P&T). Accordingly, both funding agencies and academic medical centers will need to develop broader criteria for what constitutes success as a PS.50
Increasing competition for external support
The first-time award rate among PSs for an NIH-funded R01 grant was 14% in 2012, an all-time low.5 The process to receive a grant from the NIH has become more competitive, with overall success rates for all research project grants dropping from 31% in 1997 to 18% in 2014.5 The failure to successfully obtain or continue funding is a common and unpredictable occurrence. The resulting sense of researcher vulnerability, as compared to other career pathways, can contribute to attrition. It makes a strong case for the NIH to establish a program similar to its K99/R00 Pathway to Independence Award initiative to facilitate PSs during their transition from training to an independent research career.
Academic institutions need to consider partnering with other sources of funding, such as federal and state agencies, professional associations and societies, and the private-sector, including the pharmaceutical industry. With the growth of big data, opportunities also exist to partner with companies such as Google and Amazon. Effective mentorship and career development will be needed to provide PSs with the knowledge and tools to be able to access these diverse funding sources.
Financial pressures
During both medical school and postgraduate training, there is a financial disincentive to pursue a PS career relative to a career in clinical practice—that is, there is the potential for a much greater burden of educational debt and a significant delay in eligibility for stable, paid employment.7,51,52 Even if an MD/PhD student is supported through a fellowship, the significant duration of medical school training (seven years or longer), coupled with incremental postdoctoral research training, is sufficient to sway all but the most committed young scientists away from a career in biomedical research. In a best-case scenario, a PS becomes a candidate for a tenure-track position at the age of 36.5 However, many PSs retain their postdoctoral status for several additional years because the demand for tenure-track positions exceeds the supply.52 Often, their employment and appointment as assistant professor is formally or informally contingent on successful funding from the NIH (such as a K or R award), yet the average age of PSs with an MD receiving their first R01 is 43.8 years, for those with an MD/PhD the average age is 44.3 years.5 Many PSs have large debt burdens when beginning their first faculty appointment, a situation that creates substantial financial duress and does not provide the means for the stable support of a family.
Inadequate institutional support
Institutional support can take several forms, and is often the result of the unique needs of PSs when compared to others, such as clinicians or PhD researchers. PSs are asked to generate increasing amounts of clinical revenue, which affects the time they can spend on their research or apply to securing research funding.52 Similarly, PSs are often paid less than their clinician counterparts and are often expected to obtain a large portion of their salary, and the salaries of others on their research team, through external funding. Unfortunately, their home institutions are often not optimally forthcoming with bridge funding when lapses of external funding occur.7 Finally, the metrics for P&T for PSs are often outdated and fail to take into account contributions to team science, the ever-increasing length of time needed to establish a career as an independent PS, or the demands that will need to be met within the arenas of big data, precision medicine, and team science.
Difficulties with work-life balance
PSs are generally entering the workforce at a time when many of them are also starting families. Episodic noncareer responsibilities (e.g., family and health issues) can often demand that PSs temporarily remove themselves from the workforce. PSs’ home institutions need to accommodate the competing demands that work and family often present, provide flexible options whenever possible, and assure the career trajectory of their PS faculty are not adversely affected as a result. Generational differences may lead to work environments that are unappealing to junior faculty. For example, individuals now entering medical school and those entering academia as junior faculty increasingly value a balance between work and life. Supporting this value system, studies have demonstrated that achieving a work-life balance can reduce stress, emotional exhaustion, and burnout.47,53,54
Recommendations Aimed at Reducing Attrition From the PS Workforce
The AAIM consensus conference recommendations for reducing attrition from the PS pipeline were to (1) implement formalized mentoring programs, including “mentoring the mentor” training, and periodic reviews of mentoring results; (2) establish grant programs specifically targeted to supporting the PS transitioning from training to an independent research career; (3) expand student loan repayment opportunities for individuals who are awarded an NIH or a VA career development grant; (4) provide salary support for mentors named on career development awards; (5) assure department-wide salary equity among PSs; (6) provide a stable environment for PS faculty to become independent researchers through provision of protected time and, when necessary, bridge funding; (7) reconsider criteria for P&T to accommodate the changing environment for PSs’ contributions to biomedical advances and be transparent in P&T decision-making processes; (8) pursue new avenues for research and research funding, including expanding partnerships with industry; and (9) establish a repository for PS career development data (List 1).
Implement formalized mentoring programs, including “mentoring the mentor” training, and periodic reviews of mentoring results
Formalized mentoring programs may help not only the protégé; they may also ultimately enhance the reputation of the institution through the successes of its faculty. Team-based, multigenerational, multi-institutional, and multicultural mentoring groups, therefore, could have a wide-reaching and positive impact on an institution’s junior faculty members. Mentoring topics should cover several areas; in addition to specific research topics, mentoring should be provided on the responsible conduct of research, grant-writing, publication of manuscripts, leadership, career negotiation, and work-life balance. Training of mentors and periodic evaluations of mentoring results should be required components of an institution’s mentoring program.
Establish grant programs specifically targeted to supporting the PS transitioning from training to an independent research career
Periods of transition are a particularly vulnerable time for young PSs, and the period when a PS is transitioning from training to an independent research career is one in which attrition may be more likely occur. The NIH must set aside funds specifically designated for PSs with the purpose of protecting them in this transition phase, similar in nature to the current K99/R00 program. NIH study sections need to recalibrate their expectations to accommodate highly promising individuals who may not have amassed a large body of preliminary data.
Expand student loan repayment opportunities for individuals who are awarded an NIH or a VA career development grant
Many PSs have amassed large amounts of student loan debt, which can factor into their decision to leave academia for a more lucrative profession. NIH loan repayment programs are designed to help recruit and retain highly qualified health professionals into biomedical research careers. Participants in these loan repayment programs have been shown to remain in research careers longer, apply for and receive more research grants, and be more likely to become independent investigators.55 Loan repayment opportunities for these individuals should be enhanced.
Provide salary support for mentors named on career development awards
Young investigators with mentored career development awards note they often overreport the time spent with their mentors to their funding agency,5 mainly because their mentors’ other commitments sometimes take precedence over their mentoring needs. The NIH and other funding agencies need to recognize the important and time-consuming role that mentors play in the development of young investigators looking to establish independent research careers. Mentors should be compensated for their time and allowed to formally record the percentage of time spent mentoring when reporting on their levels of effort and productivity.
Assure department-wide salary equity among PSs
It is widely recognized that salary equity remains unresolved in several of the nation’s medical schools, with gender as the highest source of disparity.56,57 Department chairs should be transparent in their salary policies, discuss salary distribution and start-up packages when offering a salaried position to a PS, and report salary distributions to department faculty on a periodic basis thereafter.
Provide a stable environment for PS faculty to become independent researchers through provision of protected time and, when necessary, bridge funding
The career development of a PS is a long-term investment; income generation usually increases only after a latency period that is measured in years. Department chairs and their institutions must embrace a broad vision of the function and trajectory of the young PS and construct a long-term budget that reflects this delay. This may include providing mentorship oversight, career development programming, grant reviews, and funding support for the transition from fellow to faculty.58 The expectation that new PS faculty members can generate clinical revenue sufficient to support their salaries while simultaneously developing their research careers is unrealistic. Additionally, department chairs should actively consider providing flexible options to accommodate their PS faculty members’ long-term work-life balance.
Reconsider criteria for P&T to accommodate the changing environment for PSs’ contributions to biomedical advances and be transparent in P&T decision-making processes
Team-based research must be valued appropriately in P&T deliberations. Traditionally, individual research has been the gold standard; however, team-based research is becoming increasingly common and more important in an era where advancement of knowledge requires the contributions of multiple disciplines. In support of the current direction of research, P&T committees must develop policies that recognize a researcher’s status as an indispensable contributor and consider a successfully funded grant proposal as evidence of scholarship regardless of who is named as the principal investigator. Within the model of team science research, competition for first-author position on a publication should be deemphasized. Finally, P&T considerations for PSs needing additional time for promotion and the award of tenure should be provided without penalty.
Pursue new avenues for research and research funding, including expanding partnerships with industry
Although the NIH provides the majority of research support for PSs, it should not be considered the only source of support. In addition to other federal and state agencies, private and public foundations, professional societies and associations, industry, and foreign sources are often willing to fund research. As big data initiatives become more commonplace, institutions would be well-served to accommodate partnerships that can be mutually beneficial.
Establish a repository for PS career development data
There is a paucity of data with which to make rational plans for improvement in the research career development process for PSs. A data repository would provide a strong foundation for future decisions. At a minimum, the repository should include (1) a description of training pathways used, (2) external grant applications, (3) external grants successfully funded, and (4) appointment and employment data for PSs collected for a period of at least five years after completion of all training.
Summary
The proper valuing of the PS workforce is critical to maintaining the status of the United States as the world leader in biomedical research. Moving forward, academic institutions, the government, and the private sector must work together to promote the general field of biomedical research as a career option through the enhancement of science and math curricula in the K–12 education system and the promotion of the PS as a career choice to diverse groups that are currently underrepresented in the workforce.
Academic medicine must also embrace the new ways in which biomedical advances are achieved by fostering team science, big data, and precision medicine, and establishing mechanisms for researchers involved in these initiatives to be recognized. Measures must be implemented to support young PS faculty through strong, viable mentorship programs and the provision of the support necessary to establish desirable independent research careers. Academia must create and oversee efficient career tracks that encourage interested young physicians to pursue a research pathway and provide robust levels of support so that all career pathways will flourish. Finally, new and creative partnerships with industry and other sources could help fund biomedical advances.
Acknowledgments
The views expressed this publication and related written conference materials or publications do not necessarily reflect the official policies of the Department of Health and Human Services; nor do mentions of trade names, commercial practices, or organizations imply endorsement by the U.S. Government.
Funding/Support: Funding for this conference was made possible (in part) by National Institutes of Health grant #1R13TR001399-01 from the National Center for Advancing Translational Sciences.
Footnotes
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Contributor Information
Robert A. Salata, Department of Medicine, Case Western Reserve University, University Hospitals Cleveland Medical Center, Cleveland, Ohio.
Mark W. Geraci, Department of Medicine, Indiana University School of Medicine, Indianapolis, Indiana.
Don C. Rockey, Department of Internal Medicine, Medical University of South Carolina, Charleston, South Carolina.
Melvin Blanchard, Department of Internal Medicine, Washington University School of Medicine, St. Louis, Missouri.
Nancy J. Brown, Department of Medicine, Vanderbilt University School of Medicine, Nashville, Tennessee.
Lucien J. Cardinal, Internal Medicine Residency Program, Stony Brook University School of Medicine, Stony Brook, and John T. Mather Memorial Hospital, Port Jefferson, New York.
Maria Garcia, Internal Medicine Residency Program, University of Massachusetts Medical School, Worcester, Massachusetts.
Michael P. Madaio, Department of Medicine, Medical College of Georgia, Augusta, Georgia.
James D. Marsh, Department of Medicine, University of Arkansas for Medical Science, Little Rock, Arkansas.
Robert F. Todd, III, Department of Medicine, Baylor College of Medicine, Houston, Texas.
References
- 1.Dzau VJ, Fineberg HV. Restore the US lead in biomedical research. JAMA. 2015;313:143–144. doi: 10.1001/jama.2014.17660. [DOI] [PubMed] [Google Scholar]
- 2.Collins FS. Exceptional opportunities in medical science: a view from the National Institutes of Health. JAMA. 2015;313:131–132. doi: 10.1001/jama.2014.16736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dzau VJ. The National Academy of Medicine’s vision: Leadership, innovation, and impact for a healthier future. JAMA. 2015;314:2127–2128. doi: 10.1001/jama.2015.15820. [DOI] [PubMed] [Google Scholar]
- 4.Collins FS. [Accessed July 19, 2017];Testimony on the Fiscal Year 2017 Budget Request before the House Committee. 2016 Mar 16; http://www.nih.gov/about-nih/who-we-are/nih-director/fiscal-year-2017-budget-request.
- 5.National Institutes of Health. [Accessed July 19, 2017];Physician-Scientist Workforce (PSW) Report 2014: Executive Summary. http://report.nih.gov/workforce/psw/index.aspx.
- 6.Wyngaarden JB. The clinical investigator as an endangered species. N Engl J Med. 1979;301:1254–1259. doi: 10.1056/NEJM197912063012303. [DOI] [PubMed] [Google Scholar]
- 7.Schafer AI. The vanishing physician-scientist? Transl Res. 2010;155:1–2. doi: 10.1016/j.trsl.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Milewicz DM, Lorenz RG, Dermody TS, Brass LF. Rescuing the physician-scientist workforce: The time for action is now. J Clin Invest. 2015;125:3742–3747. doi: 10.1172/JCI84170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daye D, Patel CB, Ahn J, Nguyen FT. Challenges and opportunities for reinvigorating the physician-scientist pipeline. J Clin Invest. 2015;125:883–887. doi: 10.1172/JCI80933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zemlo TR, Garrison HH, Partridge NC, Ley TJ. The physician-scientist: career issues and challenges at the year 2000. FASEB J. 2000;14:221–230. doi: 10.1096/fasebj.14.2.221. [DOI] [PubMed] [Google Scholar]
- 11.Morel PA, Ross G. The physician scientist: Balancing clinical and research duties. Nat Immunol. 2014;15:1092–1094. doi: 10.1038/ni.3010. [DOI] [PubMed] [Google Scholar]
- 12.Alliance for Academic Internal Medicine. [Accessed July 19, 2017];Recommendations for Revitalizing the Nation’s Physician-Scientist Workforce. http://www.im.org/p/cm/ld/fid=645.
- 13.Alliance for Academic Internal Medicine. [Accessed July 19, 2017];Physician-Scientist Imitative. http://www.im.org/p/cm/ld/fid=204.
- 14.Institute of Medicine. Informing the Future: Critical Issues in Health. 7. Washington, DC: National Academies Press; 2013. [Google Scholar]
- 15.Collins FS, Wilder EL, Zerhouni E. Funding transdisciplinary research. NIH Roadmap/Common Fund at 10 years. Science. 2014;345:274–276. doi: 10.1126/science.1255860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Green ED, Watson JD, Collins FS. Human Genome Project: Twenty-five years of big biology. Nature. 2015;526:29–31. doi: 10.1038/526029a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Insel TR, Landis SC, Collins FS. Research priorities. The NIH BRAIN Initiative. Science. 2013;340:687–688. doi: 10.1126/science.1239276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khoury MJ, McBride CM, Schully SD, et al. The Scientific Foundation for personal genomics: Recommendations from a National Institutes of Health-Centers for Disease Control and Prevention multidisciplinary workshop. Genet Med. 2009;11:559–567. doi: 10.1097/GIM.0b013e3181b13a6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The White House Office President Barack Obama. [Accessed July 19, 2017];Fact Sheet: Investing in the National Cancer Moonshot. 2016 Feb 1; https://www.whitehouse.gov/the-press-office/2016/02/01/fact-sheet-investing-national-cancer-moonshot.
- 20.Jeffe DB, Andriole DA, Wathington HD, Tai RH. The emerging physician-scientist workforce: Demographic, experiential, and attitudinal predictors of MD-PhD program enrollment. Acad Med. 2014;89:1398–1407. doi: 10.1097/ACM.0000000000000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moses H, 3rd, Matheson DH, Cairns-Smith S, George BP, Palisch C, Dorsey ER. The anatomy of medical research: US and international comparisons. JAMA. 2015;313:174–189. doi: 10.1001/jama.2014.15939. [DOI] [PubMed] [Google Scholar]
- 22.National Science Foundation. [Accessed July 19, 2017];How Do U.S. 15-Year-Olds Compare With Students From Other Countries in Math and Science? https://www.nsf.gov/nsb/sei/edTool/data/highschool-08.html.
- 23.Allen JR, Kamen D. [Accessed July 19, 2017];Order From Chaos: Investing in America’s Future Through STEM Education. 2016 Jun 3; https://www.brookings.edu/blog/order-from-chaos/2016/06/03/investing-in-americas-future-through-stem-education/
- 24.Association of American Medical Colleges. [Accessed July 19, 2017];Table A-7: Applicants, First-Time Applicants, Acceptees, and Matriculants to U.S. Medical Schools by Sex, 2007– 2008 through 2016– 2017. https:www.aamc.org/download/321470/data/factstablea7.pdf.
- 25.Association of American Medical Colleges. [Accessed July 19, 2017];Table B-11.2: Total M.D.-Ph.D. Enrollment by U.S. Medical School and Sex, 2012–2013 through 2016–2017. https://www.aamc.org/download/321554/data/factstableb11-2.pdf.
- 26.Andriole DA, Whelan AJ, Jeffe DB. Characteristics and career intentions of the emerging MD/PhD workforce. JAMA. 2008;300:1165–1173. doi: 10.1001/jama.300.10.1165. [DOI] [PubMed] [Google Scholar]
- 27.Andrews NC. The other physician-scientist problem: Where have all the young girls gone? Nat Med. 2002;8:439–441. doi: 10.1038/nm0502-439. [DOI] [PubMed] [Google Scholar]
- 28.Schaffer AI. Perspective: The Successful Physician-Scientist of the 21st Century. [Accessed July 19, 2017];Science. 2010 May 28; http://www.sciencemag.org/careers/2010/05/perspective-successful-physician-scientist-21st-century.
- 29.Wasserman E. The Door in the Dream: Conversations With Eminent Women in Science. Washington, DC: Joseph Henry Press; 2000. [DOI] [PubMed] [Google Scholar]
- 30.Merchant JL, Omary MB. Underrepresentation of underrepresented minorities in academic medicine: The need to enhance the pipeline and the pipe. Gastroenterology. 2010;138:19–26. doi: 10.1053/j.gastro.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 31.Pauff JM, Richards MC. Perspective: Ensuring Retention of Women in Physician-Scientist Training. [Accessed July 19, 2017];Science. 2009 Jan 30; http://www.sciencemag.org/careers/2009/01/perspective-ensuring-retention-women-physician-scientist-training.
- 32.National Institutes of Health. [Accessed July 19, 2017];Biomedical Research Workforce Working Group Report: A Working Group of the Advisory Committee to the Director. 2012 Jun 14; https://acd.od.nih.gov/biomedical_research_wgreport.pdf.
- 33.Association of American Medical Colleges. [Accessed July 19, 2017];Table B-13: M.D.-Ph.D. Graduates of U.S. Medical Schools by Race/Ethnicity, 2015–2016. https://www.aamc.org/download/450638/data/factstableb13.pdf.
- 34.Association of American Medical Colleges. [Accessed July 19, 2017];Table B-9: M.D.-Ph.D. Matriculants to U.S. Medical Schools by Race/Ethnicity and State of Legal Residence, 2016–2017. https://www.aamc.org/download/321546/data/factstableb9.pdf.
- 35.Cruess SR, Cruess RL, Steinert Y. Role modelling—Making the most of a powerful teaching strategy. BMJ. 2008;336:718–721. doi: 10.1136/bmj.39503.757847.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.NIH Research Portfolio Online Reporting Tools (RePORT) [Accessed July 19, 2017];Physician-Scientist Workforce (PSW) Report 2014: Research About Medical Students’ Decision to Pursue a Research Career. https://report.nih.gov/Workforce/PSW/research.aspx.
- 37.Paice E, Heard S, Moss F. How important are role models in making good doctors? BMJ. 2002;325:707–710. doi: 10.1136/bmj.325.7366.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.National Research Mentoring Network. [Accessed July 19, 2017];About the National Research Mentoring Network (NRMN) https://nrmnet.net/about-nrmn-2/
- 39.Brass LF, Akabas MH, Burnley LD, Engman DM, Wiley CA, Andersen OS. Are MD-PhD programs meeting their goals? An analysis of career choices made by graduates of 24 MD-PhD programs. Acad Med. 2010;85:692–701. doi: 10.1097/ACM.0b013e3181d3ca17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fang D, Meyer RE. Effect of two Howard Hughes Medical Institute research training programs for medical students on the likelihood of pursuing research careers. Acad Med. 2003;78:1271–1280. doi: 10.1097/00001888-200312000-00017. [DOI] [PubMed] [Google Scholar]
- 41.Laskowitz DT, Drucker RP, Parsonnet J, Cross PC, Gesundheit N. Engaging students in dedicated research and scholarship during medical school: The long-term experiences at Duke and Stanford. Acad. Med. 2010;85:419–428. doi: 10.1097/ACM.0b013e3181ccc77a. [DOI] [PubMed] [Google Scholar]
- 42.Lipner RS, Lelieveld C, Holmboe ES. Performance of physicians trained through the research pathway in internal medicine. Acad Med. 2012;87:1594–1599. doi: 10.1097/ACM.0b013e31826cba57. [DOI] [PubMed] [Google Scholar]
- 43.Todd RF, 3rd, Salata RA, Klotman ME, Weisfeldt ML, Katz JT, Xian SX, Hearn DP, Lipner RS. Career outcomes of the graduates of the American Board of Internal Medicine Research Pathway, 1995–2007. Acad. Med. 2013;88:1747–1753. doi: 10.1097/ACM.0b013e3182a7f627. [DOI] [PubMed] [Google Scholar]
- 44.Comeau DL, Escoffery C, Freedman A, Ziegler TR, Blumberg HM. Improving clinical and translational research training: A qualitative evaluation of the Atlanta Clinical and Translational Science Institute KL2-mentored research scholars program. J Investig Med. 2017;65:23–31. doi: 10.1136/jim-2016-000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Robinson GE, Schwartz LS, DiMeglio LA, Ahluwalia JS, Gabrilove JL. Understanding career success and its contributing factors for clinical and translational investigators. Acad. Med. 2016;91:570–582. doi: 10.1097/ACM.0000000000000979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Goldhamer ME, Cohen AP, Bates DW, et al. Protecting an endangered species: Training physicians to conduct clinical research. Acad. Med. 2009;84:439–445. doi: 10.1097/ACM.0b013e31819a7cb1. [DOI] [PubMed] [Google Scholar]
- 47.Strong EA, De Castro R, Sambuco D, Stewart A, Ubel PA, Griffith KA, Jagsi R. Work-life balance in academic medicine: narratives of physician-researchers and their mentors. J Gen Intern Med. 2013;28:1596–1603. doi: 10.1007/s11606-013-2521-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dhami G, Gao W, Gensheimer MF, Trister AD, Kane G, Zeng J. Mentorship programs in radiation oncology residency training programs: A critical unmet need. Int J Radiat Oncol Biol Phys. 2016;94:27–30. doi: 10.1016/j.ijrobp.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 49.Law AV, Bottenberg MM, Brozick AH, et al. A checklist for the development of faculty mentorship programs. Am J Pharm Educ. 2014;78:98. doi: 10.5688/ajpe78598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marsh JD, Todd RF., 3rd Training and sustaining physician scientists: What is success? Am J Med. 2015;128:431–436. doi: 10.1016/j.amjmed.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 51.Lemoine NR. The clinician-scientist: A rare breed under threat in a hostile environment. Dis Model Mech. 2008;1:12–14. doi: 10.1242/dmm.000752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alberts B, Kirschner MW, Tilghman S, Varmus H. Rescuing US biomedical research from its systemic flaws. Proc Natl Acad Sci U S A. 2014;111:5773–5777. doi: 10.1073/pnas.1404402111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morparia K. Work-life balance: Striking the right chords for harmony. Front Pediatr. 2016;3:122. doi: 10.3389/fped.2015.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fernandez Nievas IF, Thaver D. Work-life balance: A different scale for doctors. Front Pediatr. 2015;3:115. doi: 10.3389/fped.2015.00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.National Institutes of Health Division of Loan Repayment. [Accessed July 19, 2017];Trends and Evaluations. https://www.lrp.nih.gov/data-reports#DataReportsFindingsandAnalysesTile.
- 56.Rotbart HA, McMillen D, Taussig H, Daniels SR. Assessing gender equity in a large academic department of pediatrics. Acad Med. 2012;87:98–104. doi: 10.1097/ACM.0b013e31823be028. [DOI] [PubMed] [Google Scholar]
- 57.Wright AL, Ryan K, St Germain P, Schwindt L, Sager R, Reed KL. Compensation in academic medicine: Progress toward gender equity. J Gen Intern Med. 2007;22:1398–1402. doi: 10.1007/s11606-007-0329-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brown AM, Morrow JD, Limbird LE, et al. Centralized oversight of physician-scientist faculty development at Vanderbilt: Early outcomes. Acad Med. 2008;83:969–975. doi: 10.1097/ACM.0b013e3181850950. [DOI] [PMC free article] [PubMed] [Google Scholar]