Abstract
Objective
This study examined the influence of prescription on hearing aid (HA) fitting characteristics and 5-year developmental outcomes of children.
Design
A randomised controlled trial implemented as part of a population-based study on Longitudinal Outcomes of Children with Hearing Impairment (LOCHI).
Study sample
Two-hundred and thirty-two children that were fit according to either the NAL or DSL prescription.
Results
Deviation from targets and root-mean-square (rms) error in HA fitting revealed no significant difference between fitting prescriptions. Aided audibility quantified by using the Speech Intelligibility Index (SII) model showed that DSL provided higher audibility than NAL at low and medium input levels but not at high input level. After allowing for hearing loss desensitization, differences in audibility between prescription groups were significant only at low input level. The randomised trial of prescription that was implemented for 163 children revealed no significant between-group differences in speech production, perception, and language; but parent-rated functional performance was higher for the DSL than for the NAL group.
Conclusions
Proximity to prescriptive targets were similar between fitting prescriptions. The randomised trial revealed differences in aided audibility at low input level between prescription groups, but no significant differences in speech and language abilities.
Keywords: children, hearing loss, hearing aids, hearing-aid prescription, audibility, outcomes
Introduction
It has been widely accepted that provision of amplification is a crucial component of early intervention for children with permanent childhood hearing loss (PCHL). Best-practice clinical guidelines for pediatric hearing aid (HA) fitting have recommended the use of a validated prescriptive procedure, the National Acoustic Laboratories (NAL, Byrne et al, 2001; Dillon et al, 2011) or the Desired Sensation Level (DSL, Seewald et al, 1997; Scollie et al, 2005) prescription (American Academy of Audiology Task Force on Pediatric Amplification, 2013); and protocols have been published (Bagatto et al., 2010; King, 2010). The NAL prescription aims to maximise predicted speech intelligibility while limiting total loudness to be no greater than that perceived by a normal-hearing listener, and the DSL prescription aims to normalise loudness at different frequencies to achieve desired sensation levels. For a certain audiogram, the rationales underlying the respective prescriptions result in different prescribed gain targets for children (Ching et al., 2010b; Ching et al., 2013b). Despite this, there is some evidence to indicate that speech perception performance was similar between the fitting prescriptions (Scollie et al., 2010; Ching et al., 2013a). Recent versions of the two prescriptions have incorporated empirical evidence (for details on DSLv.5, see Scollie et al, 2005; on NAL-NL2, see Dillon et al, 2011, Ching & Dillon, 2013). In a comparison of NAL-NL2 and DSL v.5 for a certain audiogram, Ching et al (2013b) showed that the DSL procedures (DSL v.4 [Seewald et al, 1997] and DSL v.5) prescribed more low-frequency gain than the NAL procedures (NAL-NL1 [Byrne et al, 2001] and NAL-NL2) for children. Consequently, the prescribed overall gain is higher for the DSL than for the NAL procedures. Figure 1 gives a snapshot of the differences in real-ear-aided gain targets prescribed by the respective procedures.
Figure 1.
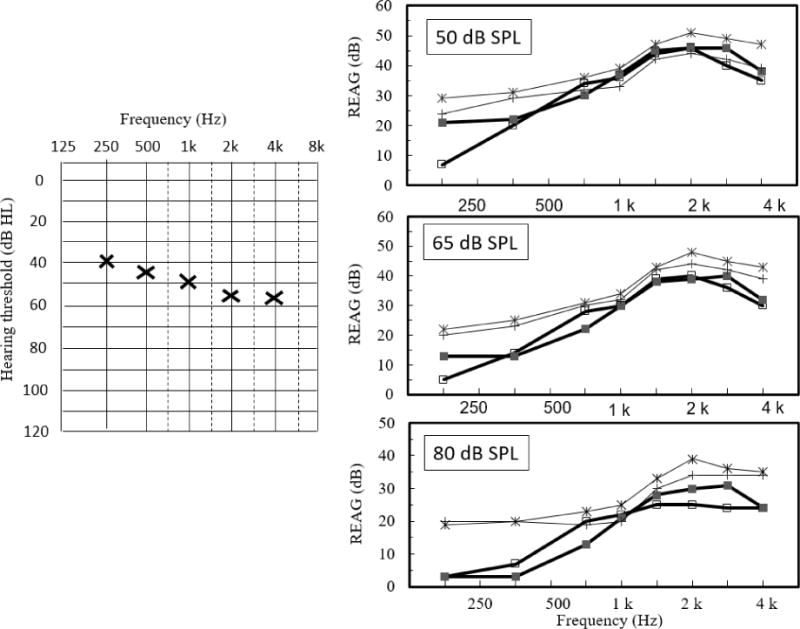
The audiogram on the left panel represents the averaged hearing threshold levels of children participating in the randomised trial of prescription. The right panels show real-ear-aided gain (REAG) prescribed by NAL-NL1 (open squares), NAL-NL2 (filled squares), DSL v.4 (crosses), and DSL v.5 (asterisks) at low (50 dB SPL), medium (65 dB SPL), and high (80 dB SPL) input levels.
An increased understanding of how the prescriptions influence fitting outcomes and developmental outcomes of young children with PCHL is crucial for guiding rehabilitation. Fitting outcomes are typically specified in terms of how closely prescribed targets are met in HAs, and how much audibility (often quantified by adopting the Speech Intelligibility Index or SII, ANSI 1997) is provided with amplification (e.g. Ching et al, 2013b; McCreery et al, 2013; McCreery et al, 2015a; Bagatto et al, 2016). How aided audibility relates to speech and language outcomes underpins effective rehabilitation. This article reports a comparison of fitting outcomes in a large clinical population of 5-year-old children who were fitted with HAs according to either the NAL or the DSL prescription. The influence of choice of prescription on the proximity of fitting to target and aided audibility will be examined, together with an investigation of the impact on speech and language outcomes of children.
Hearing aid fitting outcomes
Data from two previous studies on HA fitting to DSL prescriptive targets in clinical populations of children have shown considerable variability. In a recent multi-site study that included 195 children with mild to severe hearing losses (aged 5 to 85 months), McCreery et al (2013) reported that the root-mean-square (rms) error across 4 frequencies (0.5, 1, 2, 4 kHz) for fit-to-targets was 6.6 dB on average, with about 55% of children using HAs in both ears that exceeded 5 dB rms error. It was found that study sites that included participants fit at multiple clinics had larger HA deviations from prescriptive target than the site where participants were fit at a single clinic. An earlier study on a small clinical sample of 20 children (aged 3 to 6 years) with moderate to profound hearing loss showed deviations that were greater than 5 dB across three or more frequencies in 75% of the HA fittings (Strauss & Van Dijk, 2008). In both studies, the authors found an association between deviations from prescriptive target and verification procedure. On the other hand, a recent study that evaluated HA fitting to the NAL and DSL prescriptions in 218 children with mild to severe hearing loss at 3 years of age reported an overall mean of 3 dB rms error (Ching et al., 2013a). However, the rms error between the fitting prescriptions has not been compared.
As the proximity to target does not reflect how much speech is audible with amplification, a common approach has been the adoption of the SII model (American National Standards Institute, 1997) for quantifying audibility with amplification (Stelmachowicz et al., 1994; Johnson & Dillon, 2011; Ching et al., 2013b; McCreery et al., 2013). The SII depicts the proportion of the long-term average speech spectrum that is above a listener’s hearing thresholds or noise, whichever is higher. The amount of speech that is audible in each frequency band is weighted by the relative importance of the band to speech intelligibility. The sum of weighted audibility across all bands has a maximal value of 1, which indicates that all speech information is available; and a minimal value of 0, which denotes that no speech information is available. The SII can be related to speech scores by a transfer function. Using this method, the SII predicted speech recognition successfully in people with normal hearing and those with mild hearing loss, but has been shown to over-estimate performance of people with more severe hearing loss (Pavlovic et al., 1986; Studebaker et al., 1997; Ching et al., 1998). As hearing loss increased, the amount of speech information that could be extracted from an audible signal decreased. This is commonly referred to as hearing loss desensitization. For this reason, a modification of the ANSI standard for calculating SII to include a hearing loss desensitization has been proposed (Ching et al., 2001; Johnson & Dillon, 2011; Ching et al., 2013b). The factor was empirically derived (Ching et al., 2001), and applied in the derivation of the NAL-NL2 prescriptive method (Dillon et al., 2011). When the standard SII was applied to estimating speech scores in children, it has been shown that speech scores were over-estimated (Scollie, 2008; Gustafson & Pittman, 2011; McCreery & Stelmachowicz, 2011). For a certain amount of audibility, children extracted less speech information than was accessible by adults. This has been referred to as an age proficiency factor.
In quantifying fitting outcomes in terms of SII, McCreery et al (2013) found that an increase in rms error of fitting was associated with a reduction in aided SII in a large sample of children. Those with the greatest degrees of hearing loss or largest deviations from prescriptive targets had the lowest audibility. In a subsequent study, McCreery et al (2015a) found that about 35% of the 288 children in the study had aided audibility that was below the average for the normative range for SII based on degree of hearing loss as described by Bagatto et al (2011) for 68 children fitted to DSL targets. In a randomised controlled trial of hearing aid prescription for 200 children, Ching et al (2013b) found that the aided SII was on average higher for children fit to DSL prescriptive target than those fit to NAL target at low (50 dB SPL) and medium (65 dB SPL) input levels, but were similar at high input level (80 dB SPL). However, when the SII calculations included hearing loss desensitization, there was no significant difference between the fitting prescriptions at medium input level, with the desensitized SII being higher for NAL than for DSL at high input level. As the study included children’s HA fittings that were progressively being updated via routine clinical service to new versions of the respective prescriptions, an update of the comparison with current versions of the prescriptions is warranted.
Effect of aided audibility on performance outcomes
Speech cannot be understood if it cannot be heard. Therefore, higher audibility would be expected to be associated with better performance outcomes. However, findings on hearing loss desensitization suggest that the contribution of an audible signal to speech intelligibility is limited by factors relating to the resolution of the impaired auditory system. As such, an amplification scheme that provides higher gain than alternative schemes would invariably lead to greater loudness but may not result in better functional performance. This may explain the mixed findings reported in the literature regarding the relationship between SII and outcomes in speech and language skills in children. Whereas some studies have reported a significant relationship between SII and speech perception in children (Davidson & Skinner, 2006; McCreery et al., 2015b), others have not found a consistent relationship between SII and speech performance (Scollie et al., 2010; Stiles et al., 2012; Ching et al., this issue).
Davidson & Skinner (2006) found that speech perception scores of 26 children with moderate to severe hearing loss were correlated with aided SII and also with hearing thresholds. As hearing loss increased, aided SII decreased, and speech scores were reduced. In a similar vein, McCreery et al (2015b) found that higher aided audibility or SII, together with lesser hearing loss and higher receptive language ability were significant factors accounting for variance in speech perception scores in quiet. For a subset of 49 children who contributed longitudinal data, higher aided SII and higher vocabulary at 3 years contributed to higher speech perception scores at 5 years. As there were no significant differences in hearing thresholds, aided audibility or deviation of HA fitting from prescriptive targets across the measurement points at 3 and 5 years (McCreery et al., 2015a), this finding is consistent with the concurrent relationship between aided audibility and speech perception in quiet or in noise (McCreery et al., 2015b). On the other hand, Stiles et al (2012) showed that after allowing for the effects of hearing loss, SII did not account for significant variations in speech perception scores in 14 children (aged 6–9 years). Scollie et al (2010) reported on equally high speech perception scores for 48 school-aged children (6 to 19 years) using HAs fit according to the NAL or the DSL prescription, despite differences in prescriptive targets and HA gains (Ching et al., 2010b). Calculations of audibility in terms of standard SII in a subsequent study showed higher SII for DSL than for NAL prescriptive targets and HA gains fit to the respective prescriptions (Ching et al., 2013b). However, there were no significant differences between prescriptions when SII incorporated hearing loss desensitization, a finding that is consistent with the equivalent speech perception results observed in children using the two prescriptions in HAs. In a recent study on 252 5-year-old children with PCHL, Ching et al (this issue) adopted a method proposed by Tomblin et al (2014) to normalise aided audibility for degree of hearing loss (by regressing aided SII against unaided SII and taking the difference between the predicted aided SII and the observed aided SII) to derive ‘residualised SII’ or ‘rSII’) and investigated its effect together with a range of demographic variables, including but not limited to degree of hearing loss, on speech perception in noise. On average, the effect of rSII was not significant after controlling for other variables.
Investigations of the contribution of aided SII to language development in children also have mixed findings. Stiles et al (2012) found a significant association between aided SII and non-word repetition and receptive vocabulary, when controlling for the effect of hearing loss in 14 children with moderate to profound hearing loss who were using HAs fit to DSL targets. On the other hand, a recent multi-site study that evaluated children using HAs fit according to the DSL prescription showed that the association of audibility (corrected for unaided hearing, expressed in terms of rSII) with language development skills was inconsistent. Tomblin et al (2014) reported that rSII was significantly associated with speech production and language skills in children who had used HAs for more than 33 months at the time of evaluation (either 3 or 5 years of age), but not for those who had used HAs for a shorter duration. As duration of use was confounded with age at initial HA fitting, the authors concluded that the association between audibility provided by HAs and better developmental outcomes was more reliably observed in children who had used HAs longer or received HAs earlier. In a subsequent report, Tomblin et al (2015) found that the overall effect of rSII on language ability evaluated during a 2- to 6-year-old period was not significant (p=0.88). However, they found an association between rSII and language growth trajectories during the period. Relative to children of similar unaided hearing, those who received above-average audibility demonstrated language growth over time, whereas those with below-average audibility exhibited little growth or decline. As implied by the finding in a related article showing that the poorest audibility was associated with greatest rms error in fitting (McCreery et al., 2015a), children with below-average audibility might have been those with HA fittings that had the greatest deviation from prescriptive targets.
Although validation studies of the NAL and the DSL prescription have attested to the positive influence of matching prescriptive targets in HA fitting according to well-established protocols, the variation in targets between prescriptions for a given hearing loss raises the question of how audibility provided by the respective prescriptions might influence developmental outcomes. We aimed to investigate this question by drawing on data from participants in a prospective study on outcomes of children with hearing impairment, the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study (Ching et al., 2013c).
The current study
The research questions were: 1) Do HA fitting outcomes vary in proximity to targets and aided audibility, depending on which prescription was used for fitting? 2) Do developmental outcomes at 5 years of age vary according to the prescription used in fitting HAs?
To address the first question, we compared HA fitting outcomes of children whose HAs were fit according to either the NAL or the DSL prescription. As all children were fit by clinical audiologists of a single government-funded national hearing service provider, Australian Hearing (AH), we controlled for variability due to service provision and technology. For each prescription group, we examined the deviation from targets and the rms error of fitting. We computed aided audibility in terms of standard SII as well as a modified version of SII that incorporated hearing loss desensitization. To address the second question, we drew on a randomised controlled trial of prescription in the LOCHI study to compare 5-year developmental outcomes of children who were randomly assigned to fitting with either the NAL or the DSL prescription after diagnosis of PCHL.
We hypothesized that measures of HA fitting outcomes in terms of deviation from targets and rms error would be greater for DSL than for NAL, based on current reports on DSL fitting in clinical settings (McCreery et al., 2013; 2015a). In line with our previous studies, we hypothesized that audibility for DSL fitting would be higher than that for NAL fitting at average input level when standard SII was used in calculation, but would be similar when the SII included hearing loss desensitization. Further, we hypothesized that speech and language outcomes of children would not differ between fitting prescription groups.
Methods
This study was approved by institutional review boards. Parents provided informed consent for their children’s participation.
Participants
Participants included 232 children who were diagnosed with bilateral hearing loss and first received HAs before 3 years of age. All were fitted with bilateral air-conduction behind-the ear multi-channel hearing aids with wide-dynamic-range compression. Table 1 provides a summary of their demographic characteristics.
Table 1.
Demographic characteristics of participants.
| Characteristics | Participants (N=232) |
|---|---|
| Gender (Male) | |
| No. (percentage) | 138 (59.5%) |
| Presence of additional disabilities (AD) | |
| No. (percentage) | 81 (34.9%) |
| Age at HA fitting (months) | |
| Mean (SD) | 10.5 (10.1) |
| Median | 6.0 |
| Interquartile range | 2.8–16.3 |
| Degree of Hearing Loss* (4FA HL in better ear) | |
| No. (percentage): Mild (≤ 40 dB) | 57 (24.6%) |
| No. (percentage): Moderate (41–60 dB) | 127 (54.7%) |
| No. (percentage): Severe (61–80 dB) | 48 (20.7%) |
| Prescription | |
| No. (percentage) fitted with NAL@ prescription | 158 (68.1%) |
| No. (percentage) fitted with DSL# prescription | 74 (31.9%) |
Note:
4FA HL= Four frequency average hearing loss (average of hearing threshold levels at 0.5, 1, 2, and 4 kHz).
NAL prescription = children fitted with either NAL-NL1 or NAL-NL2.
DSL prescription = children fitted with either DSL v.4 or DSL v.5.
In the cohort, families of 163 children consented to participating in a randomised controlled trial of HA prescription (Ching et al., 2010a). These children were randomly assigned to fitting with either the NAL or the DSL prescription after diagnosis of PCHL. All remaining children who did not participate in the trial were fitted according to the NAL prescription after diagnosis. At initial fitting, the NAL prescription used was NAL-NL1 (Byrne et al., 2001), and the DSL prescription used was DSL v.4 (Seewald et al., 1997). As part of the routine clinical service, the children’s HAs would be updated according to individual needs, with changes in HA fittings according to changes in hearing levels and/or new versions of the respective prescriptions (either NAL-NL2 or DSL v.5) (Dillon et al., 2011; Scollie et al., 2005).
Hearing-aid fitting
HAs were fit by clinical audiologists across all AH hearing centres according to the national paediatric amplification protocol (King, 2010). The fitting procedure involved the use of individually measured or age-appropriate real-ear-to-coupler differences (RECD) from children to derive custom prescriptive targets, and the measurement of hearing aids in an HA2-2cc coupler to verify that targets were matched to within 5 dB at 4 of the 5 octave frequencies between 0.25 and 4 kHz. A broadband speech-weighted stimulus was used to verify gain-frequency responses at low, mid, and high input levels; and a swept pure tone presented at 90 dB SPL was used as stimulus to verify maximum power output of hearing aids. Verification was achieved by comparing the measured 2cc coupler gains and output to custom targets.
Fit-to-target
To report on the proximity of fitting to prescriptive target, the deviations (dB) of measured gains/outputs from prescriptive targets for individual ears at each frequency for each of low (50 dB SPL), medium (65 dB SPL) and high (80 dB SPL) input level were calculated. For each input level, the averaged rms error was calculated by taking the square root of the mean of the squared differences between the HA gain and prescriptive target across four frequencies (0.5, 1, 2, and 4 kHz).
Audibility calculation
For each of low, medium and high input level, two versions of SII, ANSI SII and Desensitized SII, were calculated. The ANSI SII followed the calculation method as specified by the American National Standards Institute (ANSI, S3.5, 1997). Briefly, the measured coupler gains of individual HAs were added to the individual’s RECDs to give measured real-ear-aided gain (REAG). The input speech spectra was the international long-term average speech spectrum (ILTASS; Byrne et al, 1994) at an overall level of 65 dB SPL for medium input level, and the long-term average speech spectra at overall levels of 50 dB SPL and 80 dB SPL respectively for low and high input levels (Scollie et al., 2005). The REAGs were added to the respective speech spectra to yield measured real-ear-aided responses (REAR). The available octave and inter-octave frequency hearing thresholds and REAR were interpolated to one-third-octave band levels. The audibility of speech at each band was the difference between the aided speech level and the hearing threshold level, converted to equivalent SPL in the ear canal using the free field to eardrum transfer function (Bentler & Pavlovic, 1989). The audibility at each band was weighted by the average speech importance function (Pavlovic, 1994), and summed across frequency bands from 160 to 8000 Hz to give an overall SII.
In addition, a modified version that included hearing loss desensitization, Desensitized SII, was calculated. This method included the same transforms and steps as specified in the ANSI S3.5 (1997), together with the addition of a hearing loss desensitization factor. The factor reduces the contribution of audibility to speech intelligibility as hearing loss increases (for a detailed description, see Johnson & Dillon, 2011; Ching et al, 2013b).
Evaluation of speech and language ability
As part of the 5-year-old assessment battery in the LOCHI study, a team of qualified research speech pathologists who were blinded to children’s hearing aid characteristics provided direct assessments of language and speech production. All evaluations were completed between 57 and 69 months (mean: 61, SD: 1.8). The tests included the Preschool Language Scale version 4 (PLS-4; Zimmerman et al, 2002) for assessing expressive and receptive language; the Peabody Picture Vocabulary test version 4 (PPVT-4; Dunn & Dunn, 2007) for assessing receptive vocabulary; and the Articulation and Phonology subtest of the Diagnostic Evaluation of Articulation and Phonology test (DEAP; Dodd et al, 2002) for assessing speech production. Children’s nonverbal cognitive ability were evaluated by a psychologist using the Wechsler Nonverbal Scale of Ability (WNV; Wechsler & Naglieri, 2006). These tests have been widely used to assess abilities of children with PCHL. The PLS-4 incorporates interactive play, picture pointing, and verbal elicitation activities targeting children’s knowledge of English semantics, morphology, and syntax. It gives an overall total language score, and two subscale scores – Auditory Comprehension (AC) and Expressive Communication (EC). The PPVT-4 is based on a four-alternative, forced-choice, picture-pointing format. It gives an overall score of receptive vocabulary. The DEAP phonology subtest requires a child to produce single-word utterances, elicited using pictures or verbal cues. It gives an overall total phoneme correct score, as well as a vowel score and a consonant score. For all measures, published normative data were used to derive standard scores.
In addition, research audiologists evaluated speech perception in noise. The tests were conducted in a sound-treated room. Speech reception thresholds (SRTs) for 50% correct perception of words (NU-CHIPS test, Elliott & Katz, 1980) or sentences (the Bamford–Kowal–Bench (BKB) sentence test, Bench & Bamford, 1979; Bench et al., 1979) were measured in two test conditions. In one condition, speech was presented from a loudspeaker positioned at 0° azimuth, with 8-talker babble from the same loudspeaker (S0N0). In a second condition, speech was presented from 0° azimuth as before, with uncorrelated 4-talker babble presented from each of two loudspeakers positioned on the left and right side of the listener simultaneously at ±90° azimuth giving effectively an 8-talker babble (S0N±90). The difference in SRTs between the two test conditions gives a measure of spatial release from masking (SRM).
Parents were asked to rate their children’s auditory functional performance using the PEACH scale (Ching & Hill, 2007). The PEACH is a measure of children’s functional auditory/communicative performance in real-world situations. Parents were asked to observe their child and provide information about usage of hearing device and listening comfort, and rate their child’s auditory behaviour and communicative performance in a range of quiet and noisy situations in real-world environments. The scale gives an overall functional performance score, as well as subscale scores for performance in quiet and noisy situations. Parents also provided information on demographic characteristics by completing a custom questionnaire.
Audiological information and HA fitting information within 6 months of the evaluations were obtained from participants’ clinical files held at the AH client database.
Data analyses
Descriptive statistics were used to summarize the demographic characteristics and aided SII values. Independent t-tests or Analyses of Variance (ANOVA, MANOVA) were used to determine the significance of difference between groups. For the purpose of analyses investigating the effect of prescription, the NAL group included children fitted according to either NAL-NL1 or NAL-NL2, and the DSL group included children using either DSL v.4 or DSL v.5. Post-hoc analyses included Bonferroni corrections for multiple comparisons. All analyses used two-tailed tests, with statistical significance set at p <0.05. The statistical analysis was done using Statistica v.10 (Statsoft Inc, 2011) and SPSS for Windows v.16 (SPSS Inc., 2007).
Results
HA fitting outcomes
At the 5-year evaluation interval, 152 children were using HAs fit according to the NAL prescription (106 NAL-NL1; 52 NAL-NL2); and 74 were using HAs fit according to the DSL prescription (4 DSLv.4; 70 DSLv.5).
Fit-to-target
Table 2 shows the mean deviation from targets at three input levels at different frequencies. To determine whether there were significant differences in deviation from targets across frequency, level and prescription, a MANOVA was completed with level (low, medium, high), ear (left, right), and frequency (0.5, 1, 2, and 4 kHz) as repeated measures, and prescription (NAL-NL1, NAL-NL2, DSLv.4, DSLv.5) as between-group factor. The main effects that were significant included input level (F(2, 454) = 7.28, p <0.001), and frequency (F(4,908) = 2.59, p = 0.035). The main effect of prescription was not significant (p = 0.46). There were significant interactions between input level and prescription. Post-hoc analyses indicated that deviations at high input level were significantly greater for NAL-NL1 than DSLv.5 (p <0.001), but not at low and medium input levels. There were significant interactions between frequency and prescription. Post-hoc tests showed that deviation at 4 kHz for fitting to NAL-NL1 were significant less than those fit to DSLv.5 at the same frequency (p <0.01). Post-hoc analyses of interactions among input level, frequency and prescription did not reveal further information. As we did not find significant differences between versions of the DSL prescription or between versions of the NAL prescription in terms of deviation from target, all subsequent analyses on effects of prescription combined the versions for each prescription.
Table 2.
Mean deviations (in dB) of hearing aid gain measured in HA2-2cc coupler from prescriptive gain targets at each frequency for low (50 dB SPL), medium (65 dB SPL), and high (80 dB SPL) input levels.
| Frequency (Hz) | |||||||
|---|---|---|---|---|---|---|---|
| Input level | 250 | 500 | 1000 | 2000 | 3000 | 4000 | |
| Low (50 dB SPL) | Mean | −2.0 | −1.4 | −1.2 | 0.8 | −1.7 | −0.9 |
| SD | 4.2 | 3.8 | 3.5 | 3.7 | 4.1 | 4.6 | |
| Medium (65 dB SPL) | Mean | −0.9 | −0.1 | 0.0 | −0.1 | −2.0 | −1.0 |
| SD | 3.6 | 3.3 | 3.1 | 3.3 | 4.1 | 4.7 | |
| High (80 dB SPL) | Mean | −1.7 | −0.5 | 0.5 | 0.9 | 0.1 | 1.0 |
| SD | 4.3 | 3.4 | 3.4 | 3.6 | 4.8 | 5.1 | |
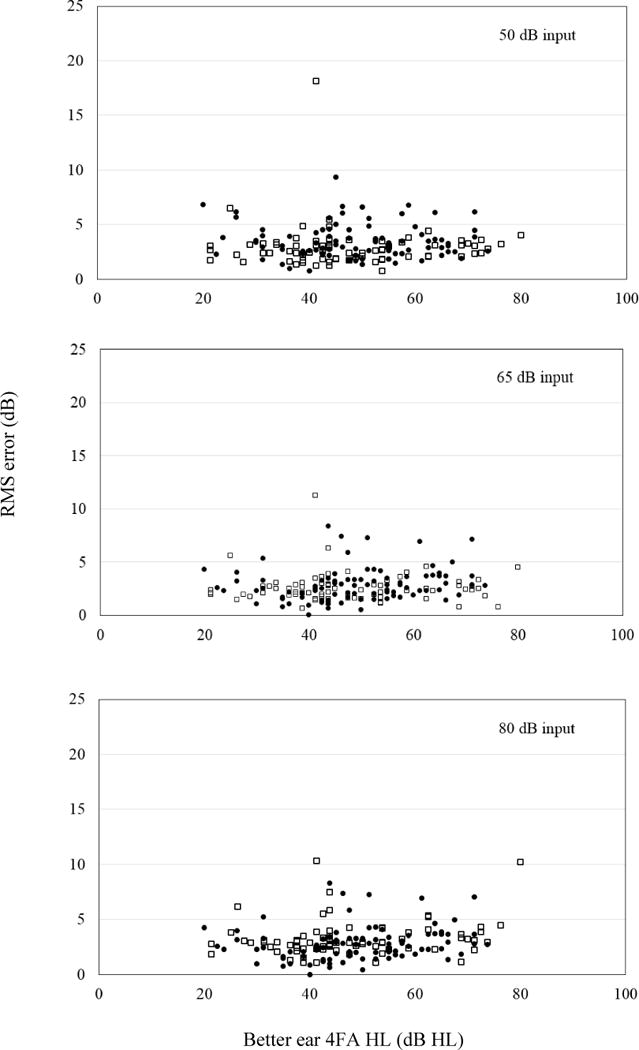
Figure 2 shows the mean rms error of the fit to NAL and DSL prescriptive target obtained for low, medium and high input level. Product moment correlations revealed that rms errors increased with increase in hearing level (<0.001). Adopting a generally accepted criterion that an rms error less than 5 dB was considered to be an optimal fit to prescription (Byrne & Cotton, 1988), 12.9 % (n = 30) of the fittings exceeded the criterion for the left ear, and 10.3% (n = 24) had rms errors that exceeded the criterion in the right ear at medium input level. Overall, 16.4% (n = 38) of children had HA fit-to-target that exceeded the criterion in at least one ear at medium input level.
Figure 2.
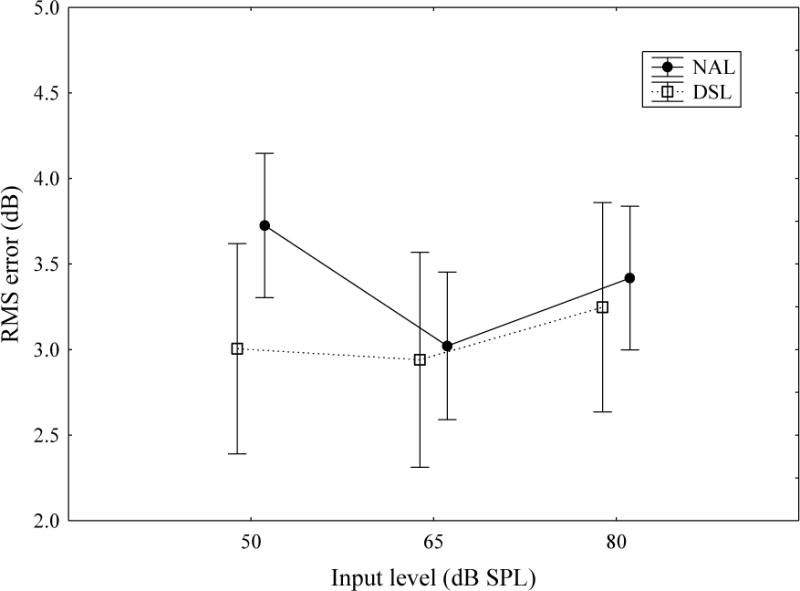
Mean rms error (across 0.5, 1, 2, 4 kHz) for children fitted according to NAL (filled circles) or DSL (open squares) prescription at low (50 dB SPL), medium (65 dB SPL), and high (80 dB SPL) input levels.
To determine whether the rms error for fit-to-target for different input levels were significantly different between fitting prescriptions, a repeated measures ANOVA was carried out with input level (low, medium, high) and ear (left, right) as repeated measures, and prescription (NAL, DSL) as between-group factor. The main effect of prescription was not significant (p = 0.19), but the main effect of input level was significant (F(2,458) = 10.99, p <0.0001). There were significant interactions between input level and prescription. Post-hoc analyses revealed that rms errors for fitting to NAL targets at low input level were greater than those for medium input level (p <0.01) and high input level (p = 0.045). There were no other significant main effects or interactions.
Aided speech audibility
Table 3 shows the mean aided audibility in terms of ANSI SII and Desensitized SII at different input levels for the respective prescriptions.
Table 3.
Mean aided audibility in terms of ANSI SII and desensitized SII at low (50 dB SPL), medium (65 dB SPL), and high (80 dB SPL) input levels for the respective prescriptions.
| Input level | ANSI SII | Desensitized SII | ||
|---|---|---|---|---|
|
| ||||
| NAL (n=158) |
DSL (n=74) |
NAL (n=158) |
DSL (n=74) |
|
| Low (50 dB SPL) | 0.44 | 0.60 | 0.43 | 0.57 |
| Medium (65 dB SPL) | 0.66 | 0.77 | 0.59 | 0.64 |
| High (80 dB SPL) | 0.77 | 0.78 | 0.61 | 0.61 |
MANOVA with SII type in the better ear (ANSI, Desensitized) and input level (low, medium, high) as repeated measures, prescription (NAL, DSL) as between-group variable, and hearing level (4FA) as covariate revealed that the main effects of prescription, hearing level, input level, and SII type were significant (p <0.001). There were significant interactions between input level and hearing level, and also between input level and prescription. Post-hoc analyses revealed that on average, the aided SII for the DSL prescription at low input level was significantly lower than those at medium and high input level, but the aided SII at medium input level was not significantly different from that at high input level. On the other hand, the aided SII for the NAL prescription at the three input levels were significantly different from each other. Between prescriptions, the aided SII for the DSL prescription was significantly higher than that for the NAL prescription at low and medium input level, but were not significantly different at high input level. There were also significant interactions among input level, SII type, and hearing level; and also among input level, SII type, and prescription. Post-hoc analyses revealed that for DSL prescription, the Desensitized SII were significantly lower than the ANSI SII at low, medium and high input levels. The same was found for the NAL prescription. Comparing the two prescriptions in terms of ANSI SII, there were significant differences between prescriptions at low and medium input levels, but not at high input level. The same was found when comparing the prescriptions in terms of Desensitized SII.
Randomised trial: Comparing fitting outcomes and developmental outcomes
This analysis asked whether there were differences in fitting outcomes and developmental outcomes in children who participated in a randomised trial of prescription. The sample comprised a subset of 163 children, who were randomly assigned to fitting with either the NAL or the DSL prescription after diagnosis of PCHL. Of these, 89 were fit according to the NAL prescription (43 NAL-NL1, 46 NAL-NL2), and 74 were fit according to the DSL prescription (70 DSLv.5, 4 DSLv.4) at the 5-year assessment interval. Table 4 shows the demographic characteristics of the sample.
Table 4.
Demographic characteristics of participants in the randomised prescription trial. Independent Samples t tests were used to compare the cognitive ability (WNV) scores and age at hearing aid fitting between the two prescription groups. Chi-square tests were used to compare the percentage differences between the two prescription groups on gender, presence of additional disabilities, and degree of hearing loss.
| Characteristics | NAL group (n=89) |
DSL group (n=74) |
Difference p value |
|---|---|---|---|
| Gender (Male) | |||
| No. (percentage) | 57 (64.0%) | 40 (54.1%) | 0.64 |
| Presence of additional disabilities (AD) | |||
| No. (percentage) | 30 (33.7%) | 22 (29.7%) | 0.99 |
| Age at hearing aid fitting (months) | |||
| Mean (SD) | 11.2 (10.7) | 10.0 (10.5) | |
| Median | 6.0 | 4.0 | 0.49 |
| Interquartile range | 3.0–17.0 | 2.0–18.8 | |
| Degree of Hearing Loss* (4FA HL in better ear) | |||
| No. (percentage):Mild (≤ 40 dB): | 20 (22.5%) | 23 (31.1%) | |
| No. (percentage): Moderate (41–60 dB) | 51 (57.3%) | 36 (48.6%) | 0.43 |
| No. (percentage): Severe (61–80 dB) | 18 (20.2%) | 15 (20.3%) | |
| Cognitive ability (WNV)@ | |||
| N | 76 | 63 | |
| Mean (SD) | 100.9(17.2) | 104.1(16.0) | 0.24 |
| Median | 100.0 | 105.0 | |
| Interquartile range (IQR) | 91.0–116.0 | 95.5–116.5 |
Note:
4FA HL= Four frequency average hearing loss (average of hearing threshold levels at 0.5, 1, 2, and 4 kHz).
WNV = Wechsler Non-Verbal Full Scale IQ. Due to missing data, scores are based on the numbers of participants as specified.
Fitting outcomes between groups: fit-to-target, rms error
Figure 3 shows the deviation from target, separately for the two prescriptions.
Figure 3.
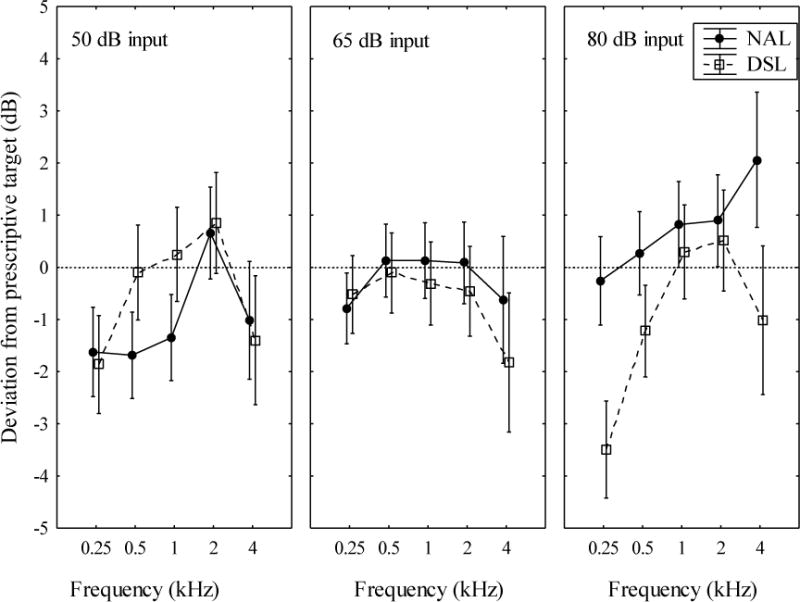
Mean deviations (dB) of measured couple gains from prescriptive targets as a function of frequency at low (50 dB SPL), medium (65 dB SPL), and high (80 dB SPL) input levels. The filled circles depict mean values for the NAL prescription group in the randomised trial, and the open squares depict mean values for the DSL prescription group. Vertical bars indicate 95% confidence intervals.
MANOVA using deviation from target as dependent variable, ear (left, right), input level (low, medium, high) and frequency (0.5, 1, 2, 4 kHz) as repeated measures, and prescription (NAL, DSL) as between-group variable showed that the main effects of prescription (p = 0.036), input level (p <0.001), and frequency (p <0.001) were significant. There were significant interactions between input level and prescription (p<0.001), between frequency and prescription (p <0.01), and between input level and frequency (p <0.001). Also, the interactions among input level, frequency, and prescription were significant. Post-hoc analyses revealed that deviations were significantly greater for DSL than for NAL at 0.5 and 1 kHz for a low input level (p = 0.04); and greater at 0.25 and 4 kHz for a high input level (p <0.001).
Figure 4 gives the rms error for fitting to prescriptive targets. MANOVA using rms error as dependent variable, with ear (left, right) and input level (low, medium, high) as repeated measures, and prescription (NAL, DSL) as a between-group variable revealed that the main effect of prescription was not significant. There were significant interactions between input level and prescription (p = 0.002). Post-hoc analyses revealed that within the NAL group, rms errors for fitting to target at low input level was significantly different from that at medium input level, but not at high input level. The rms error for fitting at the medium input level was also significantly different from that at high input level (p = 0.009). No significant differences in rms error for fitting across input levels were found for the DSL group. Between prescription groups, there were no significant differences in rms errors at any of the three input levels.
Figure 4.
Root-mean-square (rms) errors averaged across four frequencies (0.5, 1, 2, 4 kHz) as a function of better ear four-frequency average hearing level (4FA HL) at low, medium and high input levels The filled circles depict values for the NAL prescription group (n=89 children) in the randomised trial, and the open squares depict values for the DSL prescription group (n=74 children).
Aided audibility between groups
Figure 5 shows the mean aided SII in the better ear for the two prescription groups.
Figure 5.
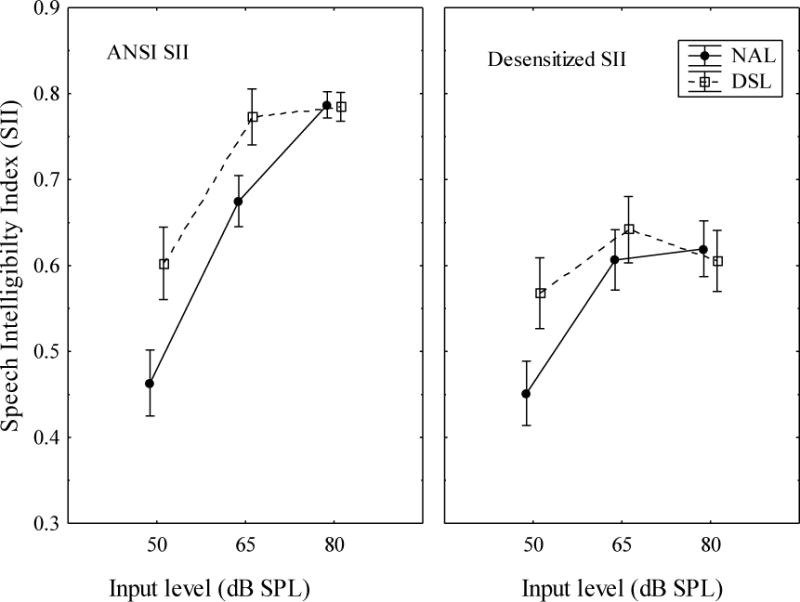
Mean aided SII values for children at low (50 dB SPL), medium (65 dB SPL), and high (80 dB SPL) input levels. The left panel shows ANSI SII values, and the right panel shows desensitized SII values. The filled circles depict mean values for the NAL prescription group in the randomised trial, and the open squares depict mean values for the DSL prescription group. Vertical bars indicate 95% confidence intervals.
MANOVA using SII as dependent variable, with SII type (ANSI, Desensitized), input level (low, medium, high) as repeated measures, hearing level as a covariate, and prescription (NAL, DSL) as between group variable revealed that the main effect of prescription was significant (p <0.001). The interaction between input level and prescription was significant (p<0.001). Post-hoc tests showed that on average, aided SII was higher for the DSL group than for the NAL group at low and medium input levels, but not at high input level. Also, there were significant interactions among input level, SII type, and prescription. Post-hoc analyses showed that for ANSI SII, the aided SII was significantly higher for the DSL group than for the NAL group at low and medium input levels but not at high input level. For Desensitized SII, the aided SII was significantly higher for the DSL group than for the NAL group at low input level, but there were no significant differences between prescription groups at medium and high input levels.
Developmental outcomes between groups
Table 5 shows the language, speech production, speech perception, and functional performance outcomes of children. As shown in the table, the difference between groups did not reach significance level for most measures, except for PEACH (p = 0.02). On average, children who were using HAs fit to DSL prescription had higher PEACH scores than those using the NAL prescription.
Table 5.
Summary of outcomes of participants in the randomised prescription trial. Independent Samples t tests were used to compare the outcome scores between the two prescription groups.
| NAL | DSL | Difference | |||
|---|---|---|---|---|---|
|
|
|||||
| n | Mean (SD) | n | Mean (SD) | p value | |
| PLS-4_AC | 77 | 85.6 (19.4) | 71 | 88.2 (18.2) | 0.39 |
| PLS-4_EC | 77 | 85.6 (18.6) | 71 | 85.4 (18.35) | 0.95 |
| PPVT | 74 | 91.0 (16.2) | 67 | 90.9 (17.9) | 0.98 |
| DEAP_PCC | 78 | 4.1 (2.1) | 70 | 4.0 (1.6) | 0.95 |
| DEAP_PVC | 78 | 5.0 (2.6) | 70 | 5.1 (2.6) | 0.81 |
| PEACH-quiet | 66 | 79.4 (15.3) | 60 | 86.3 (11.5) | 0.01 |
| PEACH-noise | 66 | 71.7 (18.5) | 60 | 75.8 (13.8) | 0.16 |
| PEACH_Total | 66 | 75.9 (15.5) | 60 | 81.5 (11.0) | 0.02 |
| SNR_ S0N0 | 59 | 4.1 (3.2) | 60 | 3.6 (3.3) | 0.35 |
| SNR_ S0N±90 | 59 | 1.2 (3.3) | 60 | 1.2 (3.8) | 0.98 |
| SRM | 59 | 2.7 (3.3) | 60 | 2.3 (3.0) | 0.43 |
Note: PLS-AC=Auditory Comprehension standard score; PLS-EC=Expressive Communication standard score; PPVT = Receptive Vocabulary standard score; DEAP_PCC=Consonant Correct standard score; DEAP_PVC=Vowel Correct standard score; PEACH-quiet = PEACH score in quiet condition; PEACH-noise = PEACH score in noise condition; PEACH_Total = PEACH total score. SNR_ S0N0= speech reception threshold in signal-to-noise ratio for the S0N0 condition; SNR_S0N±90 = speech reception threshold in signal-to-noise ratio for the S0N±90 condition; SRM = spatial release from masking.
Data for all 8 measures (PLS-receptive language, PLS-expressive language, PPVT-receptive vocabulary, PEACH-quiet score, PEACH-noise score, DEAP-consonant score, DEAP-vowel score, speech perception in collocated noise – SRT, speech perception in spatially separated noise – SRT) were available for 90 children (44 NAL, 46 DSL). There were no significant difference in rms error for fitting or aided SII between children who provided evaluation data and those who did not. MANOVA with the performance scores as repeated measures, better-ear 4FA as a covariate, and prescription (NAL, DSL) as a between-group variable revealed that the main effect of prescription was not significant (F(1,87) = 0.3, p = 0.58).
Discussion
The purpose of this study was to compare NAL and DSL fitting outcomes in hearing aids fit to a population sample of children in clinical settings. Compared to a previous report on the cohort at 3 years of age (Ching et al., 2013b), many of the HA fittings have been updated to current versions. Of the children who were using HAs fit to DSL, about 62% were using DSLv.5 at 3 years of age, compared to 95% in the present report. Of the children who were using HAs fit to NAL, all were using NAL-NL1 at 3 years of age, but 33% of them were using NAL-NL2 in the present report.
Do HA fit-to-target outcomes vary according to prescription?
We found that there was no significant effect of prescription on deviation from prescriptive targets, both in terms of absolute deviations across frequencies, and rms error for fitting across the range from 0.5 to 4 kHz. This suggests that HA fitting and verification protocols with a criterion for matching targets within 5 dB can be consistently achieved in clinics for fitting HAs to both the NAL and the DSL prescriptions. The proximity of HA fittings to prescriptive targets was 3.3 dB (SD = 2.2) on average across three input levels (3 dB rms at medium input level only). This is consistent with our earlier report on the cohort at 3 years of age (Ching et al, 2013), and well within the 5 dB criterion reported in previous studies (Ching et al., 2010a; Snik et al., 1995). The rms error across fittings to DSL target in the present cohort was 3.2 dB (SD = 2.4) on average across three input levels, which is well below the 6.6 dB error reported in a previous multi-centre study on paediatric HA fitting to DSL targets (McCreery et al., 2013). This discrepancy in clinical fitting outcomes may be related to the adoption of consistent HA fitting protocols by paediatric audiologists who served the present cohort under a single government-funded organisation, rather than the diversified practice across clinical sites in the multi-centre study. This is consistent with findings of McCreery et al (2013) that showed a significant difference in rms error across study sites, with the site that provided clinical fitting through a single clinic reporting less rms error in fitting to targets compared to other sites that provided fitting through multiple clinics.
Does aided audibility vary according to prescription?
We found that aided audibility as calculated by the standard SII method was significantly higher for HA fittings to the DSL targets than those to the NAL targets at low and medium input levels, but there were no significant differences at high input levels. This is consistent with current knowledge about the variation in gain targets between the prescriptions. A comparison of the mean REAG prescribed by the NAL-NL2 and the DSLv.5 procedures for the same audiograms showed that at low input levels, DSL prescribed more gain than NAL for frequencies below 3 kHz, but slightly less gain than NAL at 4 kHz. For medium and high input levels, DSL prescribed more gain than NAL below 3 kHz, but similar gain at 4 kHz (Ching et al., 2013b). The finding that the ANSI SII were similar at high input levels possibly reflect the contribution of the level distortion factor in the standard SII calculation method. This factor reduces the contribution of an audible signal to speech intelligibility when the overall sound pressure level exceeds 73 dB SPL (ANSI, 1997). The level distortion factor has reduced the contribution of audibility (resulting from a DSL fitting relative to an NAL fitting) with increase in input level, such that the ANSI SII for the HAs fit with the respective prescriptions at high input levels were similar. Additionally, the Desensitized SII allowed for further reduction in contribution of an audible signal to speech intelligibility with increase in hearing loss. This has resulted in an overall reduction of values.
Randomised trial: Do fitting outcomes vary according to prescription?
This study was also aimed to compare fitting and developmental outcomes of children in a randomised trial of prescription. Although there were no significant differences in rms error between prescription groups, aided audibility was on average higher for the DSL group than for the NAL group, at low and medium input levels. When desensitization was considered, the DSL prescription provided greater audibility than NAL at low input level, but there were no significant differences at medium or high input levels.
Randomised trial: Do developmental outcomes vary according to prescription?
Developmental outcomes in terms of receptive and expressive language, speech production, and speech perception in noise were not significantly different between the two groups at 5 years of age. This finding is consistent with a previous report on the cohort at 3 years of age (Ching et al., 2013a), and extended the earlier study by adding direct assessments of speech perception in either collocated babble or spatially separated babble. These tests approximate listening in real-world environments, and results from the two test conditions allowed an estimate of how well children can make use of the spatial separation between speech and noise for improving speech perception in noise (see companion article, Ching et al., this issue). As shown in Table 5, there were no significant differences in SRTs for listening to speech in babble, or in their abilities to make use of spatial separation between speech and babble for understanding speech as depicted by the measure of SRM. The parent-rated functional performance scores were higher for the DSL than for the NAL group, on average. This difference was greater in quiet situations (PEACH – Quiet score) than in noisy situations (PEACH – Noise Score), suggesting that higher HA gain for low input level than that prescribed by the NAL prescription may improve listening to soft spoken speech in the real world.
An explanation of the equivalent speech and language performance despite difference in aided audibility as calculated by the standard ANSI SII between prescriptions may be attributed to the usefulness of the additional audibility to speech intelligibility provided by the DSL compared to the NAL prescription. Adoption of the Desensitized SII allowed for this to some extent, as desensitized SIIs for medium and high input levels were similar between prescriptions. From ANSI SII to Desensitized SII, the mean difference between prescriptions was reduced from 0.14 to 0.12 units at low input level, and from 0.09 to 0.04 units at medium input level. Also, these small differences in SII between prescription groups were not associated with significant differences in speech perception results in this study, consistent with previous reports that related SII to speech scores using a transfer function (e.g. Ching et al, 1998; Scollie, 2008). Speech intelligibility is predominantly affected by the amount of audible signal above the listener’s hearing thresholds or background noise, whichever is higher. In situations when background noise determines the SNR across most of the speech frequencies, for speech inputs at typical conversational levels, the gain-frequency response can be varied considerably without affecting audibility at each frequency, and hence speech intelligibility (Alcantara et al, 2004; Van Buuren et al,, 1995). Consequently, the choice of a prescription is not critical for maximising intelligibility, provided that the alternatives result in similar audibility of the speech components that are not masked by background noise. Future investigations into whether the hearing loss desensitization factor that was incorporated in the calculation of Desensitized SII may need to be modified for children would be necessary to guide clinical management. An accurate quantification of the role of audibility for speech intelligibility in young children would form the basis for optimising amplification to maximise speech intelligibility. Any increase in audible signal necessarily results in increased loudness, and the increase can be substantial when hearing loss becomes severe (Ching et al., 2013b). Therefore, an important consideration is also to constrain the overall loudness to be within the range of listening comfort.
Implications
The current study shows that when the fitting practice uses real-ear measurements to verify that custom prescriptive targets are met in HAs to within 5 dB at 4 of 5 octave frequencies between 0.25 and 4 kHz, clinicians achieved a proximity to target that is on average within 3 dB rms of the fitting prescription. This applies irrespective of whether the NAL or DSL prescription was used. When hearing aids match NAL or DSL targets, there was no significant difference in speech intelligibility and language development between prescriptions. The match to prescription is necessary – previous studies have shown that the greater the deviation of HAs from prescriptive targets, the lower the audibility and speech intelligibility in children (McCreery et al, 2013; 2015b), and the more poorly the effectiveness of the HA was rated by adult listeners (Baumfield & Dillon, 2001). The present findings lend support to the recommendations for best practice in fitting and verification of HAs for infants and children by the American Academy of Audiology (American Academy of Audiology Task Force on Pediatric Amplification, 2013).
Limitations and future research
The proximity to targets reported in this study may have underestimated the deviations from prescriptive targets of HA fittings among children with hearing loss in the population. As the frequency of routine clinical service likely reduces as children increase in age, longer-term follow up of the children would reveal whether HA deviation from targets may change over time.
The present study reported data from a randomised trial of prescription to investigate its effect on aided audibility on speech and language outcomes of children at 5 years. As children start formal schooling, they spend a large proportion of their time learning in real-world environments that are acoustically complex. Longitudinal follow-up of children in the randomised trial during school years would shed light on the long-term effect of prescription on developmental outcomes.
Conclusion
This study compared HA fitting outcomes in 232 children using HAs fit according to either the NAL or the DSL prescription. We found that the overall rms error for fitting to targets was within 3.3 dB, regardless of the fitting prescription. In a randomised trial of prescription by 163 children, we compared the HA fitting outcomes and developmental outcomes. The trial revealed significant difference in aided audibility between prescriptions at low but not at medium and high input levels when hearing loss desensitization was considered. Parent-rated functional performance scores were higher for the DSL than for the NAL group suggesting that the HA gain required by children for low level input may need to be higher than that provided by the NAL prescription. The speech production, speech perception, receptive and expressive language were not significantly different between prescription groups.
Acknowledgments
We gratefully thank all the children, their families and their teachers for participation in this study. We are also indebted to the many persons who served as clinicians for the study participants or assisted in other clinical or administrative capacities at Australian Hearing, Catherine Sullivan Centre, Hear and Say Centre, Royal Institute for Deaf and Blind Children, and the Shepherd Centre. We also thank Julia Day for input and assistance with data collection.
Sources of funding
This work was partly supported by the National Institute on Deafness and Other Communication Disorders (Award Number R01DC008080). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Deafness and Other Communication Disorders or the National Institutes of Health, or the U.S. Department of Veterans Affairs.
The project was also partly supported by the Commonwealth of Australia through the Office of Hearing Services. We acknowledge the financial support of the HEARing CRC, established and supported under the Cooperative Research Centres Program of the Australian Government. We also acknowledge the support provided by New South Wales Department of Health, Australia; Phonak Ltd; and the Oticon Foundation.
Abbreviations
- 4FA HL
Four frequency average hearing loss (averaged hearing loss at 0.5, 1, 2, and 4 kHz)
- AH
Australian Hearing
- ANSI SII
Speech Intelligibility Index (SII) calculated with the American National Standards Institute (ANSI) S3.5 (1997) method
- DEAP
Diagnostic Evaluation of Articulation and Phonology
- Desensitized SII
Speech Intelligibility Index (SII) calculated with the ANSI S3.5 (1997) method with a revised desensitization factor
- DSL
Desired Sensation Level
- DSL v.5
Desired Sensation Level procedure multi-stage input-output algorithm
- DSL v.4
Desired Sensation Level procedure version 4.1
- HAs
Hearing aids
- HA2-2cc
Type 2 hearing-aid coupler with 2 cubic centimeter volume
- ILTASS
International long-term average speech spectrum
- LOCHI
Longitudinal Outcomes of Children with Hearing Impairment
- NAL
National Acoustic Laboratories
- NAL-NL1
National Acoustic Laboratories’ hearing aid prescription for non-linear hearing aids, version 1
- NAL-NL2
National Acoustic Laboratories’ hearing aid prescription for non-linear hearing aids, version 2
- PEACH
Parents’ Evaluation of Aural/oral Performance of Children
- PCHL
Permanent childhood hearing loss
- PLS-4
Pre-school Language Scale, 4th edition
- PPVT-4
Peabody Picture Vocabulary Test, 4th edition
- REAG
Real-ear aided gain
- REAR
Real-ear aided response
- RECD
Real-ear-to-coupler Difference
- rms
Root-mean-square
- rSII
Residualised SII
- SII
Speech Intelligibility Index
- SRM
Spatial release from masking
- SRT
Speech reception thresholds
- WNV
Wechsler Nonverbal Scale of Ability
Footnotes
Conflicts of interest
Authors one and two are employees of the National Acoustics Laboratories.
The third author has a part-time Audiology practice, Johnson Hearing Technology and Communication, PLLC.
References
- Alcantara JI, Moore BC, Marriage J. Comparison of three procedures for initial fitting of compression hearing aids. II. Experienced users, fitted unilaterally. Int J Audiol. 2004;43:3–14. doi: 10.1080/14992020400050003. [DOI] [PubMed] [Google Scholar]
- American Academy of Audiology Task Force on Pediatric Amplification. American Academy of Audiology Clinical Practice Guidelines: Pediatric Amplification 2013 [Google Scholar]
- American National Standards Institute. Methods for calculation of the speech intelligibility index, (ANSI S3.5-1997) New York, USA: American National Standards Institute; 1997. [Google Scholar]
- Bagatto M, Moodie S, Brown C, Malandrino A, Richert FM, et al. Prescribing and verifying hearing aids applying the American Academy of Audiology pediatric amplification guideline: Protocols and outcomes from the Ontario infant hearing program. J Am Acad Audiol. 2016;27:188–203. doi: 10.3766/jaaa.15051. [DOI] [PubMed] [Google Scholar]
- Bagatto M, Scollie SD, Hyde M, Seewald RC. Protocol for the provision of amplification within the Ontario infant hearing program. Int J Audiol. 2010;49:70S–79S. doi: 10.3109/14992020903080751. [DOI] [PubMed] [Google Scholar]
- Bagatto MP, Moodie ST, Malandrino AC, Richert FM, Clench DA, et al. The University of Western Ontario Pediatric Audiological Monitoring Protocol (UWO PedAMP) Trends Amplif. 2011;15:57–76. doi: 10.1177/1084713811420304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumfield A, Dillon H. Factors affecting the use and perceived benefit of ITE and BTE hearing aids. Br J Audiol. 2001;35:247. doi: 10.1080/00305364.2001.11745243. [DOI] [PubMed] [Google Scholar]
- Bench J, Bamford J. Speech-hearing tests and the spoken language of hearing-impaired children. London: Academic Press; 1979. [Google Scholar]
- Bench J, Kowal A, Bamford J. The BKB (Bamford-Kowal-Bench) sentence lists for partially hearing children. Br J Audiol. 1979;13:108–112. doi: 10.3109/03005367909078884. [DOI] [PubMed] [Google Scholar]
- Bentler RA, Pavlovic CV. Transfer functions and correction factors used in hearing aid evaluation and research. Ear Hear. 1989;10:58–63. doi: 10.1097/00003446-198902000-00010. [DOI] [PubMed] [Google Scholar]
- Byrne D, Cotton S. Evaluation of the National Acoustic Laboratories’ new hearing aid selection procedure. J Speech Hear Res. 1988;31:178. doi: 10.1044/jshr.3102.178. [DOI] [PubMed] [Google Scholar]
- Byrne D, Dillon H, Ching TYC, Katsch R, Keidser G. NAL-NL1 procedure for fitting nonlinear hearing aids: Characteristics and comparisons with other procedures. J Am Acad Audiol. 2001;12:37–51. [PubMed] [Google Scholar]
- Byrne D, Dillon H, Tran K, Arlinger S, Wilbraham K, et al. An international comparison of long-term average speech spectra. J Acoust Soc Am. 1994;96:2108–2120. [Google Scholar]
- Ching TYC, Dillon H. A brief overview of factors affecting speech intelligibility of people with hearing loss: Implications for amplification. Am J Audiol. 2013;22:306–309. doi: 10.1044/1059-0889(2013/12-0075). [DOI] [PubMed] [Google Scholar]
- Ching TYC, Dillon H, Byrne D. Speech recognition of hearing-impaired listeners: Predictions from audibility and the limited role of high-frequency amplification. J Acoust Soc Am. 1998;103:1128–40. doi: 10.1121/1.421224. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Dillon H, Hou S, Zhang V, Day J, et al. A randomised controlled comparison of NAL and DSL prescriptions for young children: Hearing aid characteristics and performance outcomes at 3 years of age. Int J Audiol. 2013a;52:17S–28S. doi: 10.3109/14992027.2012.705903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TYC, Dillon H, Katsch R, Byrne D. Maximizing effective audibility in hearing aid fitting. Ear Hear. 2001;22:212–224. doi: 10.1097/00003446-200106000-00005. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Hill M. The parent’s evaluation of aural/oral performance of children (PEACH) scale: Normative data. J Am Acad Audiol. 2007;18:220–235. doi: 10.3766/jaaa.18.3.4. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Johnson EE, Hou S, Dillon H, Zhang V, et al. A comparison of NAL and DSL prescriptive methods for paediatric hearing aid fitting: Predicted speech intelligibility and loudness. Int J Audiol. 2013b;52:29S–38S. doi: 10.3109/14992027.2013.765041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TYC, Leigh G, Dillon H. Introduction to the longitudinal outcomes of children with hearing impairment (LOCHI) study: Background, design, sample characteristics. Int J Audiol. 2013c;52:4S–9S. doi: 10.3109/14992027.2013.866342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TYC, Scollie SD, Dillon H, Seewald R. A cross-over, double-blind comparison of the NAL-NL1 and the DSL v4.1 prescriptions for children with mild to moderately severe hearing loss. Int J Audiol. 2010a;49:4S–15S. doi: 10.3109/14992020903148020. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Scollie SD, Dillon H, Seewald R, Britton L, et al. Prescribed real-ear and achieved real-life differences in children’s hearing aids adjusted according to the NAL-NL1 and the DSL v.4.1 prescriptions. Int J Audiol. 2010b;49:16S–25S. doi: 10.3109/14992020903082096. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Zhang VW, Flynn C, Burns L, Button L, et al. Factors influencing speech perception in noise for 5-year-old children using hearing aids or cochlear implants. Int J Audiol. doi: 10.1080/14992027.2017.1346307. this issue. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson LS, Skinner MW. Audibility and speech perception of children using wide dynamic range compression hearing aids. Am J Audiol. 2006;15:141–53. doi: 10.1044/1059-0889(2006/018). [DOI] [PubMed] [Google Scholar]
- Dillon H, Keidser G, Ching TYC, Flax M, Brewer S. The NAL-NL2 prescription procedure. Phonak Focus. 2011;40:1–10. doi: 10.4081/audiores.2011.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd BJ, Hua Z, Crosbie S, Holm A, Ozanne A. Diagnostic Evaluation of Articulation and Phonology. London: The Psychological Corporation; 2002. [Google Scholar]
- Dunn LM, Dunn DM. Peabody Picture Vocabulary Test. Minneapolis, MN: Pearson Assessments; 2007. [Google Scholar]
- Elliott LL, Katz DR. Northwestern University children’s perception of speech (NU-CHIPS) St. Louis: Auditec; 1980. [Google Scholar]
- Gustafson SJ, Pittman AL. Sentence perception in listening conditions having similar speech intelligibility indices. Int J Audiol. 2011;50:34–40. doi: 10.3109/14992027.2010.521198. [DOI] [PubMed] [Google Scholar]
- Johnson EE, Dillon H. A comparison of gain for adults from generic hearing aid prescriptive methods: Impacts on predicted loudness, frequency bandwidth, and speech intelligibility. J Am Acad Audiol. 2011;22:1–19. doi: 10.3766/jaaa.22.7.5. [DOI] [PubMed] [Google Scholar]
- King AM. The national protocol for paediatric amplification in Australia. Int J Audiol. 2010;49:64S–69S. doi: 10.3109/14992020903329422. [DOI] [PubMed] [Google Scholar]
- McCreery RW, Bentler RA, Roush PA. Characteristics of hearing aid fittings in infants and young children. Ear Hear. 2013;34:701–710. doi: 10.1097/AUD.0b013e31828f1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreery RW, Stelmachowicz P. Audibility-based predictions of speech recognition for children and adults with normal hearing. J Acoust Soc Am. 2011;130:4070–4081. doi: 10.1121/1.3658476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreery RW, Walker EA, Spratford M, Bentler R, Holte L, et al. Longitudinal predictors of aided speech audibility in infants and children. Ear Hear. 2015a;36:24S–37S. doi: 10.1097/AUD.0000000000000211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreery RW, Walker EA, Spratford M, Oleson J, Bentler R, et al. Speech recognition and parent ratings from auditory development questionnaires in children who are hard of hearing. Ear Hear. 2015b;36:60S–75S. doi: 10.1097/AUD.0000000000000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlovic CV. Band importance functions for audiological applications. Ear Hear. 1994;15:100–104. doi: 10.1097/00003446-199402000-00012. [DOI] [PubMed] [Google Scholar]
- Pavlovic CV, Studebaker GA, Sherbecoe RL. An articulation index based procedure for predicting the speech recognition performance of hearing-impaired individuals. J Acoust Soc Am. 1986;80:50–7. doi: 10.1121/1.394082. [DOI] [PubMed] [Google Scholar]
- Scollie SD. Childrens speech recognition scores: The speech intelligibility index and proficiency factors for age and hearing level. Ear Hear. 2008;29:543–556. doi: 10.1097/AUD.0b013e3181734a02. [DOI] [PubMed] [Google Scholar]
- Scollie SD, Ching TYC, Seewald RC, Dillon H, Britton L, et al. Children’s speech perception and loudness ratings when fitted with hearing aids using the DSL v.4.1 and the NAL-NL1 prescriptions. Int J Audiol. 2010;49:26S–34S. doi: 10.3109/14992020903121159. [DOI] [PubMed] [Google Scholar]
- Scollie SD, Seewald RC, Cornelisse LE, Moodie S, Bagatto M, et al. The desired sensation level multistage input/output algorithm. Trends Amplif. 2005;9:39. doi: 10.1177/108471380500900403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seewald R, Cornelisse LE, Ramji KV. Users’ manual. London, Ontario: University of Western Ontario Hearing Health Care Research Unit; 1997. DSL v4.1 for Windows: a software implementation of the Desired Sensation Level (DSL[i/o]) method for fitting linear gain and wide-dynamic-range compression hearing instruments. [Google Scholar]
- Snik AF, van den Borne S, Brokx JP, Hoekstra C. Hearing-aid fitting in profoundly hearing-impaired children. Comparison of prescription rules. Scand Audiol. 1995;24:225–30. doi: 10.3109/01050399509047540. [DOI] [PubMed] [Google Scholar]
- SPSS Inc. SPSS for Windows (version 16.0) Chicago, USA: SPSS Inc; 2007. [Google Scholar]
- Statsoft Inc. Statistica Software (version 10.0) Tulsa, OK: USA: Statsoft Inc; 2011. [Google Scholar]
- Stelmachowicz PG, Lewis DE, Carney E. Preferred hearing-aid frequency responses in simulated listening environments. J Speech Hear Res. 1994;37:712. doi: 10.1044/jshr.3703.712. [DOI] [PubMed] [Google Scholar]
- Stiles DJ, Bentler RA, McGregor KK. The Speech Intelligibility Index and the pure-tone average as predictors of lexical ability in children fit with hearing aids. J Speech Lang Hear Res. 2012;55:764–778. doi: 10.1044/1092-4388(2011/10-0264). [DOI] [PubMed] [Google Scholar]
- Strauss S, Van Dijk C. Hearing instrument fittings of pre-school children: do we meet the prescription goals? Int J Audiol. 2008;47:S62–71. doi: 10.1080/14992020802300904. [DOI] [PubMed] [Google Scholar]
- Studebaker GA, Sherbecoe RL, McDaniel DM, Gray GA. Age-related changes in monosyllabic word recognition performance when audibility is held constant. J Am Acad Audiol. 1997;8:150–62. [PubMed] [Google Scholar]
- Tomblin JB, Harrison M, Ambrose SE, Walker EA, Oleson JJ, et al. Language outcomes in young children with mild to severe hearing loss. Ear Hear. 2015;36:76S–91S. doi: 10.1097/AUD.0000000000000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin JB, Oleson JJ, Ambrose SE, Walker E, Moeller MP. The influence of hearing aids on the speech and language development of children with hearing loss. JAMA Otolaryngol Head Neck Surg. 2014;140:403–409. doi: 10.1001/jamaoto.2014.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren RA, Festen JM, Plomp R. Evaluation of a wide range of amplitude-frequency responses for the hearing impaired. J Speech Hear Res. 1995;38:211–221. doi: 10.1044/jshr.3801.211. [DOI] [PubMed] [Google Scholar]
- Wechsler D, Naglieri JA. Wechsler nonverbal scale of ability. San Antonio, TX: Harcourt Assessment; 2006. [Google Scholar]
- Zimmerman I, Steiner VG, Pond RE. Preschool Language Scale. 4th. San Antonio, TX: The Psychological Corporation; 2002. [Google Scholar]


