Abstract
Concerned partners (CPs) of service members and veterans who misuse alcohol face help-seeking barriers and mental health problems. We used multiple regression to evaluate the efficacy of Partners Connect, a 4-session web-based intervention (WBI) to address military CPs’ mental health and communication. We randomized 312 CPs to the WBI or a control group. Five months later, WBI CPs reported significant reductions in their anxiety and increases in their social support compared to control CPs. Intervention dose was also associated with improved CP outcomes. There was no intervention effect on perceived partner drinking. Partners Connect appears to fill a need for families who face help-seeking barriers and provides an alternative to traditional care for those who may not otherwise seek help.
Keywords: military, alcohol misuse, hazardous drinking, web intervention, computer-assisted intervention, CRAFT
Alcohol misuse is a problem in the military and is associated with numerous problems including fitness for duty, absenteeism, depression, anxiety (LeardMann et al., 2013; Mattiko, Olmsted, Brown, & Bray, 2011), suicide (LeardMann et al., 2013), and sexual violence (Morral et al., 2016). Alcohol misuse, or drinking that is quantified as at-risk or heavy drinking, precedes more severe alcohol use disorders (National Institute on Alcohol Abuse and Alcoholism, 2005). Misuse of alcohol is most common among younger service members (Institute of Medicine, 2012) with over a quarter of 18 to 35 year-olds reporting binge drinking in the past month (Ramchand et al., 2011). Over half of service members are married (Karney & Crown, 2007), and some research suggests that married service members report alcohol misuse at a higher rate (40%; Paul, Grubaugh, Frueh, Ellis, & Egede, 2011) than married civilians (13%; Bray et al., 2009, & Karney and Crown, 2007).
The mental health of spouses is a growing concern among the military, specifically during the deployment cycle (Booth et al., 2007; De Burgh, White, Fear, & Iversen, 2011; Eaton et al., 2008; Verdeli et al., 2011). Military spouses are an at-risk population for mental health problems because they face the stressors of military life, including frequent moves to new military bases, frequent spousal separations for military training, assignments, and combat deployments (Drummet, Coleman, & Cable, 2003). Furthermore, these stressors can erode the social support available to military spouses due to loss of social networks through changes in residence (Drummet et al., 2003), and loss of support from partners with combat-related mental health issues (e.g., PTSD) (Karney & Trail, 2017).
Spouses in relationships with a heavy drinking service member partner often report high levels of depression, anxiety, and social impairment (Erbes, Meis, Polusny, & Arbisi, 2012; Rodriguez, Osilla, Trail, Gore, & Pedersen, in press). Depressive and anxiety symptoms in spouses affect the mental health of children and increase rates of marital conflict (Verdeli et al., 2011), and may interfere with healthy partnerships involving mutual support. Interventions for military spouses are important because if the mental health needs of spouses are met and they are able to receive more social support for their stress, these improvements may improve the health of the family.
COMMUNITY REINFORCEMENT AND FAMILY TRAINING FOR MILITARY CONCERNED PARTNERS
Preventive interventions have been shown to address the needs of spouses—concerned partners (CPs)—in relationships with partners who misuse alcohol, but have not been tested in military samples. The Community Reinforcement and Family Training (CRAFT) intervention targets the CP and is typically composed of 12 individual in-person sessions that focus on positive communication and other behavioral reinforcement and punishment strategies to help the CP influence their partner’s drinking and change their negative interactions (Meyers & Wolfe, 2004; Smith & Meyers, 2007). CRAFT was developed to engage treatment-resistant partners into alcohol treatment by teaching the CP supportive and non-confrontational skills to cope with their partner’s drinking (e.g., positive communication, social skills, pleasant activity planning), and ways to interact with their partner through positive reinforcement (e.g., rewards for sobriety) and punishment (e.g., letting natural consequences happen from drinking). CRAFT utilizes functional analysis so that CPs learn about the context around their partner’s drinking (e.g., triggers, rewards) and offers support for how CPs can help reduce their partner’s drinking and encourage help-seeking. CRAFT is an ideal intervention for CPs with behavioral health concerns because it focuses on CP self-care and CP interactions with their partner. Moreover, the research supports the efficacy of CRAFT. CPs in CRAFT reported significant improvements in their depression, anger expression toward partner, relationship satisfaction, and family conflict (Meyers, Miller, Smith, & Tonigan, 2002; Miller, Meyers, & Tonigan, 1999; Roozen, de Waart, & van der Kroft, 2010). One of the desired outcomes of CRAFT is for the partner to enter treatment, and CRAFT studies show that when a CP receives CRAFT, their partner who misuses alcohol is two to three times more likely to enter alcohol treatment compared to when CPs attend Johnson and Al-Anon interventions (Meyers et al., 2002; Miller et al., 1999; O'Farrell & Fals-Stewart, 2003; Roozen et al., 2010).
Although the effects on both CP and partner outcomes are promising, CRAFT needs to be adapted for military populations where service members rarely seek formal help for their drinking (Burnett-Zeigler et al., 2011; Golub, Vazan, Bennett, & Liberty, 2013). Barriers to help-seeking include a culture in which treatment for substance use may be judged unfavorably, administrative rules that require involvement of commanding officers in treatment plans, and potential recording of treatment in their personnel file (Burnett-Zeigler et al., 2011; Department of Defense Instruction, 2014; Department of the Army, 2012). The in-person format of CRAFT may be less appealing to military CPs who may similarly be reluctant to seek in-person help. In a small study, military CPs reported that one of their biggest fears to seeking care is that someone in their tight-knit community would see them entering a treatment center or that seeking care would have negative implications on their partner’s military career (Hoge, Auchterlonie, & Milliken, 2006; Hoge et al., 2004; Osilla et al., 2016). Innovative interventions to effectively help this population are needed (Tanielian, Trail, & Cory, in press). If an intervention could efficaciously reduce CP problems, CPs may be better equipped to help their heavy drinking service member or veteran, but understanding the direct effects of the intervention on the CP is an essential first step and the primary focus of this paper.
PARTNERS CONNECT: A WEB-BASED ADAPTION OF CRAFT FOR MILITARY CPS
We developed a web-based adaptation of CRAFT, called Partners Connect, that was designed for military CPs who were concerned about their service member or veteran partner’s drinking (Osilla, Pedersen, Gore, Trail, & Howard, 2014; Osilla et al., 2016). The web-based intervention (WBI) utilized the behavioral skills promoted in CRAFT, such as self-care (e.g., engaging in healthy activities, increasing social support) and use of healthy communication with their partner. Unlike CRAFT’s goal of helping the CP’s partner initiate treatment, our more modest goal with Partners Connect was to help address the CP’s own mental health concerns and to enhance their communication skills. Because this intervention was about one-third as long as CRAFT and because this population may not otherwise seek services, we envisioned the intervention as a first step to help primarily the CP. In doing so, we hypothesized that improved communication over time would in turn help their partner who misuses alcohol reduce their drinking and potentially seek care.
Partners Connect utilizes Motivational Interviewing (MI)-based language (Miller & Rollnick, 2012) and Cognitive Behavioral Therapy (CBT) strategies (Dobson, 2010). MI techniques help engage the CP by building self-efficacy and intrinsic motivation to change, both of which are essential to facilitate actual behavior change for both CPs and their partners (Franks et al., 2012). CPs learn self-care skills such as identifying areas in their life they want more happiness in, engaging in pleasant activities away from home, and talking with a support person they trust and can practice their skills with. CPs also learn CBT skills to modify their own behaviors and interactions toward their partner, and to improve their own psychological functioning and social support, which equips CPs to help improve the relationship with their partner while encouraging their partner to change their drinking behavior.
In social learning theory, CP communication and behavior either rewards or punishes their partner’s drinking, thus making similar future behaviors more or less likely (Stuart, 1969; Weiss, Hops, & Patterson, 1973). For example, going to happy hour regularly with their partner may perpetuate drinking habits. Although a CP’s behaviors can reward positive relationship behaviors, making them more likely to recur, they can also unintentionally reinforce undesirable behaviors such as drinking using unhealthy spousal communication and interaction (Gottman, 1993; Patterson & Hops, 1972; Rodriguez, DiBello, & Neighbors, 2013). The CBT skills CPs learn in Partners Connect include communication skills training and behavioral strategies for CPs to use before and when their service member or veteran partner drinks (Meyers, Mille, Hill, & Tonigan, 1998; Meyers et al., 2002; Miller et al., 1999; Roozen et al., 2010). CPs also use these skills to decrease their own depression and anxiety. Thus, Partners Connect encourages the CP to change their own behaviors to improve mood and increase social support.
This is the first study that evaluates a web-based intervention for military CPs concerned about their service member or veteran partner’s drinking. The focus on military CPs is important because military populations rarely seek help for alcohol problems and are in need of care. We fill significant gaps in the literature by examining whether access to a stand-alone WBI helps reduce CP mental health concerns (e.g., depression, anxiety) compared to CPs in a waitlist control group that received no intervention. We also asked CPs to estimate the quantity and frequency of their service member or veteran partner’s drinking to assess the intervention’s effect on service member and veteran outcomes. Based on prior research with CRAFT, we hypothesized that WBI CPs would report lower mental health symptoms, lower anger expression, and higher social support at follow-up compared to control CPs.
METHOD
Participants
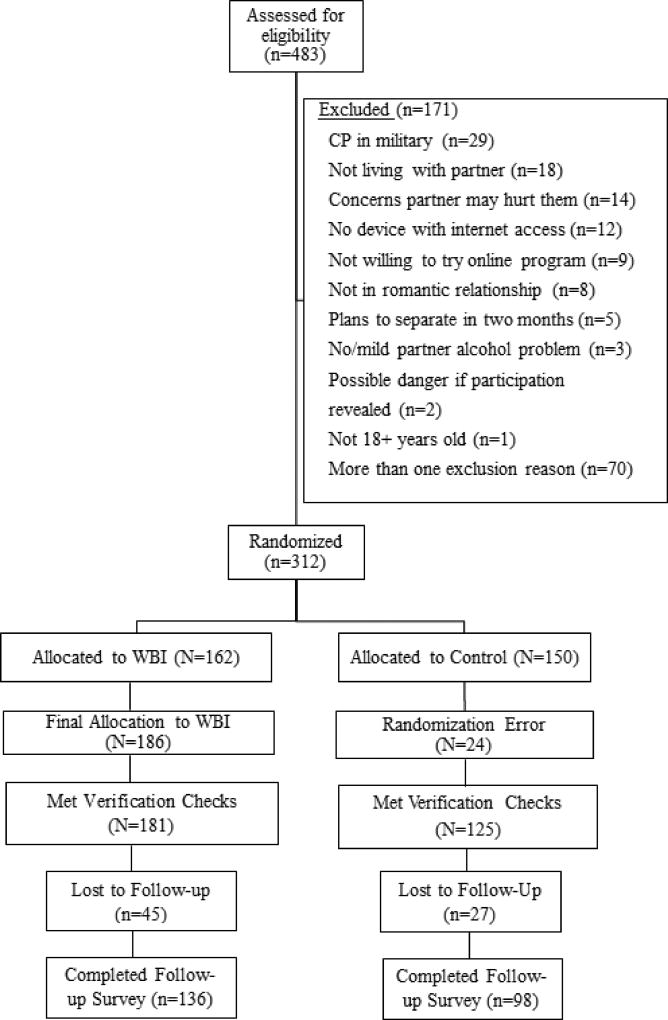
Participants were 312 CPs recruited from Facebook (see Figure 1). We adapted eligibility criteria from previous CRAFT trials (Meyers et al., 2002; Miller et al., 1999; Roozen et al., 2010). CPs needed to (1) be at least 18 years old; (2) be in a romantic relationship with their partner; (3) be living with their partner; (4) not be in the military currently themselves; (5) have a computer, mobile, phone, or tablet with Internet access; (6) have no plans to separate from their partner in the next 60 days; (7) indicate at least a value of “3” on scale from “1 not at all” to “7 very much” for the degree to which they felt their partner had an alcohol problem; (8) indicate they believed they would be in no danger if their partner found out about their participation in the study; (9) indicate no general concerns they would be physically hurt by their partner; and, (10) be willing to try an online program focused on communicating with their partner about his/her drinking. The purpose of these criteria was to ensure that we recruited participants that have frequent contact with their partner so they could practice new skills, those who would feel safe participating in this study, and those not in the military themselves, who would be subject to military reporting policies.
Figure 1.
CONSORT diagram (Consort, 2010)
Procedure
Participants were recruited online through Facebook. Facebook is one social media platform capable of reaching difficult to reach populations (Pedersen & Kurz, 2016), including military samples for alcohol intervention studies (Brief et al., 2013; Pedersen et al., 2015; Pedersen, Naranjo, & Marshall, 2017). A detailed description of the recruitment procedures are described in our prior work (Pedersen, Osilla, Helmuth, Tolpadi, & Gore, 2017). In brief, targeted ads were displayed on Facebook to individuals who were interested in military and veteran spouse/partner content (“Military Spouse Central”, “National Military Family Association”) and members of Facebook group pages for specific military bases in the United States. Interested CPs who clicked on ads were directed to a study website where they could read about the study, complete the eligibility assessment, and if eligible, complete the online informed consent and baseline survey. If randomized to the intervention, they could complete their first WBI session immediately. This process was entirely online and no research staff were involved until we phoned participants to verify baseline completion and reminded them about upcoming sessions or surveys. CPs received $50 for completion of the baseline assessment and $50 for a 5-month follow-up assessment. Toward the end of the study, we increased this incentive to $75 for their 5-month follow-up if they were hard-to-reach or about to go past the 60-day follow-up window (n=50). We also incentivized WBI CPs $10 for every post-session satisfaction survey they completed and an additional $20 when completing three of the four post-session surveys. Data from the post-session surveys were not analyzed for this paper.
CPs (N=312) were randomly assigned by computer to the Partners Connect WBI or a waitlist control group that received no intervention before their baseline survey, using permuted block randomization with random size blocks, thereby ensuring the number of people allocated to each group was approximately equal throughout recruitment (Pocock, 1984). With this approach, we assigned 162 participants to the WBI group and 150 participants to the control group. However, we erroneously sent 24 CPs randomly assigned to the control group an email with a link to access the WBI in the beginning of the study and they began the WBI. We analyzed our outcomes with and without these 24 participants and found no differences on our main effects between them and the truly randomized WBI participants. We therefore included them as WBI participants, which left us with 186 CPs assigned to the WBI and 126 to control. We then removed six CPs (one control, 5 WBI) through a series of data verification checks (e.g. partner’s pay grade and reported rank did not match), which gave us a baseline sample of 306 (181 WBI and 125 control) participants. Of the 306, 234 completed the 5-month follow-up (76.5%), resulting in 136 WBI (75.2%) CPs, and 98 (78.4%) control CPs in our final sample. Participants in the waitlist control group were eligible to complete the WBI after their follow-up, but additional data were not collected after their initial follow-up.
Partners Connect WBI
The WBI contained four 30–45 minute sessions (see Table 1) that were structured with (1) a video introducing the session topic; (2) interactive questions and personalized feedback based on the CP’s baseline survey responses (in Session 1), or in between session practice activities (Sessions 2–4); (3) skills building (e.g., positive communication strategies); and, (4) next steps. Each session was spaced one week apart to give CPs a chance to practice the skills learned in a prior session. If CPs did not finish a session, they could continue from where they left off using a unique log-in code. Readers are encouraged to read a paper we published previously that describe the intervention in detail (Osilla et al., 2014).
Table 1.
WBI Description by Session
| Session | Goals |
|---|---|
| Session 1: Self-Care |
|
| Session 2: Let’s Talk |
|
| Session 3: Exiting the Roadmap |
|
| Session 4: Forming a New Roadmap |
|
The WBI was designed to help the CP address their own mental health concerns and improve their relationship quality (satisfaction and positive communication). Session 1 addresses CPs’ mental health issues. CPs receive personalized feedback about their drinking and mental health issues, are encouraged to engage in pleasant activities for self-care and to identify a support person to talk with about their concerns. CPs are encouraged to practice skills with their social support person in between sessions. Session 2 focuses on improving their relationship through positive communication exercises. Session 3 focuses on functional analysis of their partner’s drinking, and how to positively reinforce their partner’s sobriety and negatively reinforce their drinking. Session 4 focuses on continuing self-care and talking with their partner about their concerns while interacting with them in healthy ways.
CP outcome measures
Descriptive measures
We assessed demographics of the CP (gender, race/ethnicity, education, relationship status, age of children [if present]). We also asked how many times CPs drank heavily in the past month (defined as 4 or more drinks on one occasion), and if CPs received mental health counseling, therapy, or self-help for their own personal or emotional issues in the past year.
Depression
CPs’ depression were measured using the Patient Health Questionnaire (PHQ-8, α = .84 at baseline) (Kroenke et al., 2009). The PHQ-9 has been well validated in primary care settings and in the general population for detecting depression [(sensitivity/specificity > .80), test-retest reliability (ICC=.84)(Kroenke, Spitzer, Williams, & Lowe, 2010)]. Each of the eight items of the PHQ-8 is scored from 0 (not at all) to 3 (nearly every day). PHQ-8 scores of 10 or more indicate moderate depression with high sensitivity (100%) and specificity (95%) (Kroenke, Spitzer, & Williams, 2001; Kroenke et al., 2009).
Anxiety
CPs’ anxiety was measured using the Generalized Anxiety scale (GAD-7; α = .90) (Kroenke, Spitzer, Williams, Monahan, & Löwe, 2007). Each of the seven items ranged from 0 (not at all) to 3 (nearly every day). Scores of 10 or more indicate moderate anxiety and the scale has high test-retest reliability (ICC=.83), sensitivity and specificity (>80%), and convergent validity with other anxiety scales (r > .07).(Spitzer, Kroenke, Williams, & Lowe, 2006)
Anger expression
We measured CPs’ anger expression on the State-Trait Anger Expression Inventory (STAXI-2) (Spielberger, 1999). The anger expression index comprised of four subscales (i.e., anger expression in, anger expression out, anger control in, anger control out) and was calculated such that higher index scores indicated more intense anger that is suppressed or expressed aggressively or both (α = .76 at baseline).
Social support
The CP’s level of social support was assessed using three subscales taken from the MOS Social Support Survey, which has high convergent validity (r > .72), and internal consistency reliability and test-retest reliability among adults (Sherbourne & Stewart, 1991). The subscales were: emotional/informational support (e.g., someone to give you good advice about a crisis; α = .96), tangible support (e.g., someone to help with daily chores if you were sick; α = .95), and positive social interaction (e.g., someone to do something enjoyable with; α = .97). Items were rated on a five-point scale from 1 (none of the time) to 5 (all of the time), and then averaged across each subscale representing how frequently they received each type of support. Participants were asked to think of someone other than their partner when answering these questions.
Relationship quality
The CPs’ perceptions of the quality of their relationship with their partners was measured using the 6-item Quality of Marriage Index (QMI; α = .96 at baseline) (Norton, 1983). Items were rated on a ten-point scale from 1 (strongly disagree) to 10 (strongly agree) and we scored it by summing the six items (max = 60, highest quality). The QMI has been used in previous studies of military couples (Doss et al., 2012; Skopp et al., 2011).
Family conflict
The quality of the family environment was measured using the conflict subscale from the Family Environment Scale (FES) (Moos & Moos, 1986). The 9-item subscale measured anger and conflict among family members. Prior research using Confirmatory Factor Analysis shows that the conflict subscale of the FES demonstrates good convergent validity with scales measuring similar constructs and is able to reliably distinguish families with an antisocial alcohol abusing parent from control families (Sanford, Bingham, & Zucker, 1999). Items were rated on a five-point scale from 1 (strongly disagree) to 5 (strongly agree). We reverse-scored four of the items and then summed the nine items so that higher scores reflected more conflict (max = 45; α = .80 at baseline).
WBI number of sessions
We calculated the number of sessions completed (max=4).
Partner outcome measures
Alcohol consumption
Collateral reports of alcohol data have been validated (Meyers et al., 1998; Meyers et al., 2002; Miller et al., 1999; Roozen et al., 2010). CPs reported their perceptions about how many days their partner consumed five drinks or more on one occasion and the quantity of drinks they had on an average occasion. CPs also filled out the Drinking Norms Rating Form (DNRF) to assess perceptions of their partners’ total drinks per week in the past 30 days (Baer, Stacy, & Larimer, 1991).
Analytic plan
Missing data management
For all scales except anger expression, we replaced the values for missing items in the scale with the participant’s mean rating of the remaining non-items. This was done so that summed scales would be correctly calibrated for all participants, and high Cronbach’s alpha values indicated that this substitution was appropriate for the data. If a participant had missing data for more than half of the items on a scale, then the scale was coded as missing for that participant and no substitution was performed. Missing scale items were replaced for an average of 6.0% of participants across baseline measures and for an average of 5.5% of participants across follow-up measures. For anger expression, scores were substituted as per the STAXI-2 manual (e.g., if ten or more items from the 57 items or two items from a scale were missing, the participant’s score was set to missing) (Spielberger, 1999).
Covariates
We controlled for CP education, partner years of service, presence of children, and partner military status (i.e., enlisted, officer, veteran). We found the control CPs reported receiving more education (51% reported with a bachelor’s degree or more compared to 35% of WBI CPs) and that their partners had more years of military service than control CPs. We controlled for these variables in all analyses. There were no significant differences between the groups on other demographic characteristics and outcome variables at baseline. In addition, we controlled for baseline levels of the outcome and partner military status (veteran or active duty/reserve/guard) because veterans and active duty/reserve/guard may experience different barriers to care (e.g., fewer barriers due to confidentiality for veterans) and have different base rates of heavy drinking (Schell & Marshall, 2008). We also controlled for partner military rank (enlisted or officer) as alcohol misuse is significantly associated with paygrade especially after returning from combat deployment (Mustillo et al., 2015).
We used multiple regression analyses in SAS 9.4 to evaluate the impact of the WBI on CP mental health (i.e., depression, anxiety, anger expression), relationship quality, social support, and family conflict at follow-up, controlling for baseline scores and covariates. We then assessed whether the number of sessions CPs completed influenced outcomes. Finally, as an exploratory analysis, we analyzed the simple within-subjects’ change from baseline to follow-up for each outcome within the WBI and control groups via paired t-tests to explore our hypotheses that CPs in the WBI condition would have improved outcomes.
RESULTS
Participant characteristics
Our final analytic sample comprised 136 CPs who were allocated to WBI and 98 to control (Table 2). There were no differences in attrition at follow-up by intervention group. Overall, 95% of CPs were female, 71% White, 9% multi-racial, 6% African American, 4% Hispanic/Latino, and a mean age of 32 (SD = 6.5, Range = [22, 68]). About 89% of CPs reported being married to their partner; those that were married reported being married for 7.5 years (SD = 4.9) on average. Approximately 77% of CPs reported having children.
Table 2.
Baseline Participant Characteristics (N=234)
| Variable | Control (n=98) Number (%)/Mean (SD) |
WBI (n=136) Number (%)/Mean (SD) |
|---|---|---|
| Characteristics: | ||
|
| ||
| Mean age (SD) | 32.3 (5.8) | 31.9 (7.0) |
| Gender [N (%)] | ||
| Male | 1 (1.0%) | 4 (2.9%) |
| Female | 94 (95.9%) | 128 (94.1%) |
| Prefer Not to Answer | 2 (2.0%) | 4 (2.9%) |
| (Missing) | 1 (1.0%) | 0 (0.0%) |
| Race [N (%)] | ||
| American Indian | 2 (2.0%) | 0 (0.0%) |
| Asian | 4 (4.1%) | 3 (2.2%) |
| Black or African American | 5 (5.1%) | 9 (6.6%) |
| Hispanic/Latino(a) or of Spanish Origin | 2 (2.0%) | 8 (5.9%) |
| Native Hawaiian or other Pacific Islander | 0 (0.0%) | 1 (0.7%) |
| White | 68 (69.4%) | 98 (72.1%) |
| Multiracial (Checked More Than One Race) | 12 (12.2%) | 10 (7.4%) |
| Other | 1 (1.0%) | 3 (2.2%) |
| (Missing) | 4 (4.1%) | 4 (2.9%) |
| Education [N (%)] | ||
| Less than 4-year college | 47 (48.0%) | 86 (63.2%) |
| College graduate or more educated | 48 (49.0%) | 47 (34.6%) |
| (Missing) | 3 (3.1%) | 3 (2.2%) |
| Relationship Status [N (%)] | ||
| Married | 88 (89.8%) | 119 (87.5%) |
| Living with Partner | 8 (8.2%) | 7 (5.1%) |
| Never married/single | 0 (0.0%) | 6 (4.4%) |
| (Missing) | 2 (2.1%) | 4 (2.9%) |
| Average Years if Married (SD) | 7.6 (5.3) | 7.5 (4.7) |
| Have Children [N (%)] | ||
| No | 15 (15.3%) | 34 (25.0%) |
| Yes | 80 (81.6%) | 100 (73.5%) |
| (Missing) | 3 (3.1%) | 2 (1.5%) |
| Anxiety | 6.4 (4.5) | 6.8 (5.2) |
| Depression | 6.8 (4.2) | 7.2 (4.7) |
| Anger Expression | 33.4 (13.3) | 37.0 (13.5) |
| Relationship Quality | 36.9 (13.6) | 34.2 (13.4) |
| Social Support (informational) | 3.1 (1.1) | 3.2 (1.1) |
| Social Support (tangible) | 3.0 (1.4) | 3.1 (1.4) |
| Social Support (positive social interaction) | 3.2 (1.3) | 3.0 (1.3) |
| Family Conflict | 22.2 (6.3) | 24.0 (6.4) |
| Total Drinks Per Week | 3.7 (8.3) | 4.3 (7.1) |
| Experienced At Least 1 Heavy Drinking Episode in the Past 30 Days | ||
| No | 66 (67.3%) | 89 (65.4%) |
| Yes | 25 (25.5%) | 43 (31.6%) |
| (Missing) | 7 (7.1%) | 4 (2.9%) |
| Drinking Days (at least one drink) in the Past Month | 4.7 (7.2) | 5.0 (6.9) |
At baseline, 28% screened positive for major depression on the PHQ-8, 23% screened positive for generalized anxiety disorder on the GAD-7, and 30.5% reported at least one heavy drinking episode in the past month. About half (54.7%; n=128) reported experiencing at least one of these behavioral health problems of major depression, generalized anxiety, or a heavy drinking episode. At baseline, of those who met criteria for depression, anxiety, or reported a heavy drinking episode, 63% reported not receiving any therapy, counseling, or self-help in the past year. At baseline, 206 CPs (88%) perceived that their partners drank heavily (five drinks or more on one occasion) at least once in the past month and drank a mean of 10 (SD = 6) drinks on their heaviest occasion in the past month. Average relationship quality reported by CPs in our sample was just under the midpoint of the scale (M = 35.30, SD = 13.49).
Intervention efficacy
Estimates and related tests of significance for main effect models on CP outcomes are provided in Table 3. Controlling for baseline levels of the outcome and the other covariates, WBI CPs reported significantly lower levels of anxiety and higher levels of emotional/informational and tangible social support at follow-up compared to CPs in the control condition. WBI CPs in reported an average symptom score reduction of 1.32 (SD = 4.94) on the GAD-7 at follow-up, while control CPs reported a symptom increase of 0.4 (SD = 5.22) at follow-up. WBI CPs also reported more frequent emotionally supportive interactions at follow-up, while control CPs reported less frequency in these types of interactions. WBI and control CPs both reported more frequent tangible support at follow-up, but WBI CPs reported more frequent interactions over time. Of note, CPs in the WBI condition had marginally lower levels of depressive symptoms at follow-up compared to CPs in the control condition. WBI CPs reported an average reduction in depressive symptoms was 1.29 (SD = 4.89) on the PHQ-8 at follow-up, while control CPs reported an average reduction of 0.22 (SD = 4.46) at follow-up.
Table 3.
Partners Connect Intervention Effects on Changes in CP Outcomes
| Criterion | Predictor | b | t | p |
|---|---|---|---|---|
| Anxiety | Baseline anxiety | .412 | 6.70 | <.001 |
| Children | 1.827 | 2.54 | .012 | |
| Partner years of service | −.043 | −.81 | .417 | |
| CP education | .200 | .32 | .747 | |
| Partner enlisted status | .790 | .74 | .463 | |
| Partner veteran status | .361 | .53 | .596 | |
| Intervention | −1.60 | −2.64 | .009 | |
|
| ||||
| Depression | Baseline depression | .485 | 7.48 | <.001 |
| Children | 1.821 | 2.63 | .009 | |
| Partner years of service | −.001 | −.02 | .983 | |
| CP education | .346 | .59 | .559 | |
| Partner enlisted status | 1.119 | 1.08 | .281 | |
| Partner veteran status | −.532 | −.81 | .418 | |
| Intervention | −.792 | −1.35 | .177 | |
|
| ||||
| Anger Expression | Baseline anger expression | .758 | 13.89 | <.001 |
| Children | 3.264 | 1.74 | .083 | |
| Partner years of service | −.012 | −.09 | .926 | |
| CP education | −.286 | −.18 | .858 | |
| Partner enlisted status | 2.317 | .86 | .392 | |
| Partner veteran status | −.046 | −.03 | .978 | |
| Intervention | −2.171 | −1.37 | .172 | |
|
| ||||
| Relationship Quality | Baseline relationship quality | .603 | 9.35 | <.001 |
| Children | −.634 | −.30 | .764 | |
| Partner years of service | −.327 | −2.11 | .036 | |
| CP education | −3.343 | −1.85 | .066 | |
| Partner enlisted status | 1.764 | .58 | .565 | |
| Partner veteran status | −.066 | −.03 | .972 | |
| Intervention | .058 | .03 | .974 | |
|
| ||||
| Social Support (informational) | Baseline social support | .510 | 8.26 | <.001 |
| Children | .119 | .69 | .488 | |
| Partner years of service | −.001 | −.009 | .930 | |
| CP education | −.129 | −.89 | .373 | |
| Partner enlisted status | −.435 | −1.76 | .080 | |
| Partner veteran status | .091 | .59 | .556 | |
| Intervention | .325 | 2.30 | .022 | |
|
| ||||
| Social Support (tangible) | Baseline social support | .410 | 6.77 | <.001 |
| Children | .057 | .27 | .788 | |
| Partner years of service | −.001 | −.02 | .986 | |
| CP education | −.094 | −.53 | .598 | |
| Partner enlisted status | −.473 | −1.56 | .119 | |
| Partner veteran status | −.014 | −.07 | .941 | |
| Intervention | .410 | 2.36 | .019 | |
|
| ||||
| Social Support (positive social interaction) | Baseline social support | .413 | 7.03 | <.001 |
| Children | .128 | .67 | .501 | |
| Partner years of service | −.016 | −1.17 | .144 | |
| CP education | −.117 | −.72 | .470 | |
| Partner enlisted status | −.372 | −1.34 | .182 | |
| Partner veteran status | −.063 | −.37 | .711 | |
| Intervention | .224 | 1.41 | .159 | |
|
| ||||
| Family Conflict | Baseline family conflict | .600 | 10.39 | <.001 |
| Children | 1.480 | 1.63 | .105 | |
| Partner years of service | .063 | .96 | .336 | |
| CP education | 1.779 | 2.34 | .020 | |
| Partner enlisted status | .068 | .05 | .958 | |
| Partner veteran status | 1.253 | 1.56 | .120 | |
| Intervention | −.779 | −1.03 | .305 | |
Partner: Service member/veteran
There were no significant intervention effects on CP anger expression, relationship quality, family conflict, or positive social interaction support. There were no main effects of the WBI on perceived service member or veteran partner drinking over time. However, since we hypothesized that the WBI would improve relationship quality and positive social interaction support and decrease family conflict and partner drinking, we explored the simple within-subjects’ change from baseline to follow-up within each group via paired t-tests. Of note, WBI CPs reported significant improvements in relationship quality, t(132) = 3.10, p = .002, and family conflict, t(133) = 3.46, p < .001, but control CPs did not (t(95) = 0.99, p = .324, and t(96) = 0.26, p = .792, respectively). No other tests revealed different patterns of results between groups. In addition, both the CPs in the WBI and control groups reported perceptions that their partners had significant decreases in the past month in the number of drinks per week (~1.2 fewer drinks per week) and in heavy drinking days (~4 fewer drinks per day) (all ps < .001).
Dose response
Among the 134 WBI participants, 13% completed no sessions, 11% completed one session, 4% completed two sessions, 7% completed three sessions, and 65% completed all four sessions. There was a significant linear association between number of WBI sessions completed and CP outcomes: those CPs who completed more WBI sessions had greater reductions in their anxiety [b = −.536, SE = .238, t(121) = −2.26, p = .026], depression [b = −.598, SE = .232, t(121) = −2.58, p = .011], and anger expression (indicating more adaptive management of angry feelings) [b = −1.747, SE = .688, t(115) = −2.54, p = .013] than those who completed fewer WBI sessions. Completing more sessions was also associated with increases in tangible social support [b = .155, SE = .071, t(120) = 2.18, p = .031] and positive social interaction support [b = .145, SE = .065, t(120) = 2.22, p = .028]. No other effects of WBI dose on CP and service member/veteran partner outcomes were significant.
DISCUSSION
Partners Connect is a readily accessible web-based intervention that fills a need for military families who face significant help-seeking barriers. This study is the first to evaluate the efficacy of a military CP-focused intervention that can be accessed at any time outside the traditional military health system. First, we demonstrated our ability to successfully recruit and retain a challenging population (Tanielian et al., in press) through Facebook (see also Pedersen et al., 2017). CPs were mostly young, married, and White, which matches data from the larger military spouse population (Office of the Deputy Under Secretary of Defense, 2015). As is the case in the military population, CPs were primarily women with male partners. Despite 55% experiencing depression, anxiety, or a heavy drinking episode, about 63% of participants in the sample with these symptoms reported not seeking help in the past year. Thus, the Facebook recruitment and web-based nature of the approach appeared to reach CPs who were distressed but not receiving help otherwise.
We found Partners Connect reduced CP anxiety and increased their emotional and tangible social support, factors that have a strong research base in affecting quality of life and health outcomes (Olatunji, Cisler, & Tolin, 2007; Uchino, 2006). Although the WBI effect was not significant in the regression models (i.e., the two groups were not different from each other), exploratory within-group analyses revealed that relationship quality and family conflict significantly improved over time for WBI CPs, but not for control CPs. These results provide preliminary support that the WBI impacted CP anxiety and social support, which makes sense because of the intervention’s focus on CP self-care through pleasant activities and identification of a support person to practice session activities with that person. It is possible that by equipping CPs with practical tools such as positive communication, CPs were more confident and effective in helping to address their partner’s drinking directly, but this relationship needs to be tested in future research. In a population that experiences high stress related to their partner’s drinking, demonstrating CP improvements from a stand-alone WBI has large clinical implications for helping the CP population who might not otherwise seek care. These findings warrant further study in a larger clinical trial that evaluates the WBI in a larger sample and over a longer follow-up period to assess whether WBI participants report more sustained improvements over time.
The majority of WBI participants (64%) completed all four sessions of Partners Connect and thus received the full intervention as it was designed, which is higher than expected from similar WBI studies that show completion rates of less than half (Brief et al., 2013). This is important because intervention dose was associated with improved CP mental health symptoms: CPs who completed more WBI sessions had greater reductions in depression, anxiety, and anger expression compared to WBI CPs who completed fewer sessions. While CPs who completed all four sessions may be a self-selected and more motivated group, future versions of this intervention should incorporate strategies to encourage sustained adherence to the intervention.
Both groups reported significant improvements in their perceptions of their partner’s drinking rates. We surmise that the overall improvements in drinking outcomes occurred for three reasons: First, CPs responded to an ad for people concerned about their partner’s drinking and wanting tools to help. Their participation was intentional and they took steps to address their problem by consenting to participate and completing surveys; that alone may have been helpful. Second, the CPs were likely in distress at the time of enrollment and experienced regression to the mean as is common in assessment-only groups. Finally, it is conceivable that after the CPs’ baseline survey, CPs may have been more aware of their partner’s drinking behavior, and reductions may reflect a more accurate perception of their partner’s drinking.
Future research is needed to better understand the effects of the WBI on both CP and their partners beyond the five-month assessment period in the current study. Research on civilian couples show that men and women are significantly more likely to make a health behavior change when their partner does as well, such as when one quits smoking or increases physical activity (Jackson, Steptoe, & Wardle, 2015). Thus, changes in either partner are highly likely to benefit the other partner. Future research should also examine the mechanism for which partner drinking is affected including whether improvements in CP outcomes mediate reductions in partner drinking. If CPs can serve as a gateway to changing partner drinking and help-seeking, this intervention would significantly advance work to help service members who misuse alcohol.
The current study has limitations worth noting. Although similar to the demographics of military spouses (Office of the Deputy Under Secretary of Defense, 2015) where over 90% of military spouses are female, our sample targeted female CPs and consisted of mostly young White women who were married to male service members and veterans. Due to the pilot nature of our work, our WBI was limited to female vignettes of CPs and did not account for male CP perspectives or same-sex relationships. Future research could extend the WBI to other populations including other concerned family members. Also, although collateral reports of alcohol data have been validated (Meyers et al., 1998; Meyers et al., 2002; Miller et al., 1999; Roozen et al., 2010), CP perceptions of their partner’s drinking and help-seeking may be biased in some way since they are based solely on observations of their partner. Finally, our study uses a waitlist control, which may lead to overestimations of intervention effects (e.g. Miller, 2015), and future research could explore comparing the WBI to another active comparison intervention.
Military partners are disproportionately affected by their partner’s alcohol misuse, but no preventive interventions exist that help alleviate the mental health symptoms that these CPs experience due to their partner’s drinking. This WBI is a unique intervention because it targets the CP, it is web-based, and it exists outside the traditional health system as a stand-alone intervention. In general, web-based interventions that are widely accessible to this population fill a substantial need. Future research is needed to better understand the implications of using the CP to facilitate change for themselves and their partner, and doing so with WBIs present dissemination opportunities for reaching large numbers of people with effective intervention.
Acknowledgments
The current study was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA; 1R34AA023123, Principal Investigator: Karen Chan Osilla). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIAAA or the National Institutes of Health. The authors would like to thank Dr. Robert J. Meyers for his consultation and guidance adapting CRAFT for this study. The authors also express appreciation to Helen Chin, Marylou Gilbert, Eric Helmuth, Stefanie Howard, Lisa Jonsson, PhuongGiang Nguyen, and Rosalyn Velasquez without whom this research would not be possible.
Footnotes
Portions of this paper were presented at annual conferences of the Addiction Health Services Research (2016) and Research Society on Alcoholism (2016, 2017).
Contributor Information
Karen Chan Osilla, RAND Corporation, 1776 Main Street, PO Box 2138, Santa Monica, CA 90407-2138, USA.
Thomas E. Trail, RAND Corporation, 1200 South Hayes Street, Arlington, VA 22202-5050, USA.
Eric R. Pedersen, RAND Corporation, 1776 Main Street, PO Box 2138, Santa Monica, CA 90407-2138, USA.
Kristie L. Gore, RAND Corporation, 1200 South Hayes Street, Arlington, VA 22202-5050, USA.
Anagha Tolpadi, RAND Corporation, 1776 Main Street, PO Box 2138, Santa Monica, CA 90407-2138, USA.
Lindsey M. Rodriguez, University of South Florida St. Petersburg, 140 7th Ave. S., St., Petersburg, FL 33701, USA.
References
- Baer JS, Stacy A, Larimer M. Biases in the Perception of Drinking Norms among College-Students. Journal of Studies on Alcohol. 1991;52(6):580–586. doi: 10.15288/jsa.1991.52.580. [DOI] [PubMed] [Google Scholar]
- Booth B, Segal MW, Bell DB, Martin JA, Ender MG, Rohall DE, Nelson J. What we know about Army families: 2007 update. Family and Morale, Welfare and Recreation Command; Arlington, VA: 2007. [Google Scholar]
- Brief DJ, Rubin A, Keane TM, Enggasser JL, Roy M, Helmuth E, Hermos J, Lachowicz M, Rybin D, Rosenbloom D. Web intervention for OEF/OIF veterans with problem drinking and PTSD symptoms: A randomized clinical trial. Journal of consulting and clinical psychology. 2013;81(5):890. doi: 10.1037/a0033697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett-Zeigler I, Ilgen M, Valenstein M, Zivin K, Gorman L, Blow A, Duffy S, Chermack S. Prevalence and correlates of alcohol misuse among returning Afghanistan and Iraq veterans. Addictive behaviors. 2011;36(8):801–806. doi: 10.1016/j.addbeh.2010.12.032. [DOI] [PubMed] [Google Scholar]
- De Burgh HT, White CJ, Fear NT, Iversen AC. The impact of deployment to Iraq or Afghanistan on partners and wives of military personnel. International Review of Psychiatry. 2011;23(2):192–200. doi: 10.3109/09540261.2011.560144. [DOI] [PubMed] [Google Scholar]
- Department of Defense Instruction. Problematic Substance Use by DoD Personnel, Number 1010.04. 2014 Available at http://www.dtic.mil/whs/directives/corres/pdf/101004p.pdf.
- Department of the Army. The Army Substance Abuse Program. Washington, DC: 2012. [Google Scholar]
- Dobson KS, editor. Handbook of Cognitive-Behavioral Therapies. 3. New York, NY: Guilford Press; 2010. [Google Scholar]
- Doss BD, Rowe LS, Morrison KR, Libet J, Birchler GR, Madsen JW, McQuaid JR. Couple therapy for military veterans: Overall effectiveness and predictors of response. Behavior Therapy. 2012;43(1):216–227. doi: 10.1016/j.beth.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Drummet AR, Coleman M, Cable S. Military families under stress: Implications for family life education. Family Relations. 2003;52(3):279–287. doi: 10.1111/j.1741-3729.2003.00279.x. [DOI] [Google Scholar]
- Eaton KM, Hoge CW, Messer SC, Whitt AA, Cabrera OA, McGurk D, Cox A, Castro CA. Prevalence of mental health problems, treatment need, and barriers to care among primary care-seeking spouses of military service members involved in Iraq and Afghanistan deployments. Military medicine. 2008;173(11):1051–1056. doi: 10.7205/milmed.173.11.1051. [DOI] [PubMed] [Google Scholar]
- Erbes CR, Meis LA, Polusny MA, Arbisi PA. Psychiatric distress among spouses of National Guard soldiers prior to combat deployment. Mental Health in Family Medicine. 2012;9(3):161–169. [PMC free article] [PubMed] [Google Scholar]
- Franks MM, Shields CG, Lim E, Sands LP, Mobley S, Boushey CJ. I will if you will: Similarity in married partners’ readiness to change health risk behaviors. Health Education & Behavior. 2012;39(3):324–331. doi: 10.1177/1090198111402824. [DOI] [PubMed] [Google Scholar]
- Golub A, Vazan P, Bennett AS, Liberty HJ. Unmet need for treatment of substance use disorders and serious psychological distress among veterans: a nationwide analysis using the NSDUH. Mil Med. 2013;178(1):107–114. doi: 10.7205/milmed-d-12-00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottman JM. The roles of conflict engagement, escalation, and avoidance in marital interaction: A longitudinal view of five types of couples. Journal of consulting and clinical psychology. 1993;61:6–6. doi: 10.1037//0022-006x.61.1.6. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Substance use disorders in the U.S. armed forces. Washington, DC: The National Academies Press; 2012. [Google Scholar]
- Jackson SE, Steptoe A, Wardle J. The influence of partner’s behavior on health behavior change: the English longitudinal study of ageing. JAMA internal medicine. 2015;175(3):385–392. doi: 10.1001/jamainternmed.2014.7554. [DOI] [PubMed] [Google Scholar]
- Karney BR, Crown JS. Families under stress: An assessment of data, theory, and research on marriage and divorce in the Military. Santa Monica, CA: RAND Corporation; 2007. [Google Scholar]
- Karney BR, Trail TE. Associations Between Prior Deployments and Marital Satisfaction Among Army Couples. Journal of Marriage and Family. 2017;79(1):147–160. doi: 10.1111/jomf.12329. [DOI] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Annals of internal medicine. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. Journal of affective disorders. 2009;114(1):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- LeardMann CA, Powell TM, Smith TC, Bell MR, Smith B, Boyko EJ, Hooper TI, Gackstetter GD, Ghamsary M, Hoge CW. Risk factors associated with suicide in current and former US military personnel. Jama. 2013;310(5):496–506. doi: 10.1001/jama.2013.65164. [DOI] [PubMed] [Google Scholar]
- Mattiko MJ, Olmsted KL, Brown JM, Bray RM. Alcohol use and negative consequences among active duty military personnel. Addict Behav. 2011;36(6):608–614. doi: 10.1016/j.addbeh.2011.01.023. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Mille WR, Hill DE, Tonigan JS. Community reinforcement and family training (CRAFT): Engaging unmotivated drug users in treatment. Journal of Substance Abuse. 1998;10(3):291–308. doi: 10.1016/S0899-3289(99)00003-6. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Miller WR, Smith JE, Tonigan JS. A randomized trial of two methods for engaging treatment-refusing drug users through concerned significant others. Journal of consulting and clinical psychology. 2002;70(5):1182–1185. doi: 10.1037//0022-006x.70.5.1182. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Wolfe BL. Get your loved one sober: Alternatives to nagging, pleading and threatening. Center City, MN: Hazelden; 2004. [Google Scholar]
- Miller WR, Meyers RJ, Tonigan JS. Engaging the unmotivated in treatment for alcohol problems: A comparison of three strategies for intervention through family members. Journal of consulting and clinical psychology. 1999;67(5):688–697. doi: 10.1037//0022-006x.67.5.688. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. 3. New York: Guilford Press; 2012. [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale manual. 2. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- Morral AR, Gore KL, Schell TL, Bicksler B, Farris C, Ghosh-Dastidar B, Jaycox LH, Kilpatrick D, Kistler S, Street A, Tanielian T, Williams KM. Estimates for Department of Defense Service Members from the 2014 RAND Military Workplace Study. Santa Monica, CA: RAND Corporation; 2016. Sexual Assault and Sexual Harassment in the US Military: Volume 2. [Google Scholar]
- Mustillo SA, Kysar-Moon A, Douglas SR, Hargraves R, Wadsworth SM, Fraine M, Frazer NL. Overview of depression, post-traumatic stress disorder, and alcohol misuse among active duty service members returning from Iraq and Afghanistan, self-report and diagnosis. Military medicine. 2015;180(4):419–427. doi: 10.7205/MILMED-D-14-00335. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Helping Patients Who Drink Too Much: A Clinician's Guide 2005 [Google Scholar]
- Norton R. Measuring marital quality: A critical look at the dependent variable. Journal of Marriage and the Family. 1983;45(1):141–151. [Google Scholar]
- O'Farrell TJ, Fals-Stewart W. Alcohol abuse. Journal of Marital and Family Therapy. 2003;29(1):121–146. doi: 10.1111/j.1752-0606.2003.tb00387.x. [DOI] [PubMed] [Google Scholar]
- Office of the Deputy Under Secretary of Defense. 2014 Demographics: Profile of the Military Community." Office of the Deputy Assistant Secretary of Defense (Military Community and Family Policy 2015 [Google Scholar]
- Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: A meta-analytic review. Clinical Psychology Review. 2007;27(5):572–581. doi: 10.1016/j.cpr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Osilla KC, Pedersen ER, Gore K, Trail T, Howard SS. Study design to develop and pilot-test a web intervention for partners of military service members with alcohol misuse. Addiction Science & Clinical Practice. 2014;9(1):18. doi: 10.1186/1940-0640-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osilla KC, Pedersen ER, Tolpadi A, Howard SS, Phillips JL, Gore KL. The feasibility of a web-intervention for military veteran spouses concerned about their partner's alcohol misuse. Journal of Behavioral Health Services and Research. 2016:1–17. doi: 10.1007/s11414-016-9546-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, Hops H. Coercion, a game for two: Intervention techniques for marital conflict. In: Ulrich RE, Mountjoy P, editors. The experimental analysis of social behavior. New York: Appleton-Century-Cofts; 1972. pp. 133–177. [Google Scholar]
- Pedersen ER, Helmuth ED, Marshall GN, Schell TL, PunKay M, Kurz J. Using Facebook to Recruit Young Adult Veterans: Online Mental Health Research. Jmir Research Protocols. 2015;4(2) doi: 10.2196/resprot.3996. doi: ARTN e6310.2196/resprot.3996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Kurz J. Using Facebook for health-related research study recruitment and program delivery. Current opinion in psychology. 2016;9:38–43. doi: 10.1016/j.copsyc.2015.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Naranjo D, Marshall GN. Recruitment and retention of young adult veteran drinkers using Facebook. PLOS One. 2017;12(3):e0172972. doi: 10.1371/journal.pone.0172972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Osilla KC, Helmuth ED, Tolpadi A, Gore KL. Reaching concerned partners of heavy drinking service members and veterans through Facebook. Military Behavioral Health. 2017;5(3):265–273. [Google Scholar]
- Pocock SJ. Clinical trials: A practical approach. Chichester, UK: Wiley; 1984. [Google Scholar]
- Ramchand R, Miles J, Schell T, Jaycox L, Marshall GN, Tanielian T. Prevalence and correlates of drinking behaviors among previously deployed military and matched civilian populations. Military Psychology. 2011;23(1):6. doi: 10.1080/08995605.2011.534407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez LM, DiBello AM, Neighbors C. Perceptions of partner drinking problems, regulation strategies and relationship outcomes. Addictive behaviors. 2013;38(12):2949–2957. doi: 10.1016/j.addbeh.2013.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez LM, Osilla KC, Trail T, Gore K, Pedersen E. Alcohol use among concerned partners of heavy drinking service members and veterans. Journal of Marital and Family Therapy. doi: 10.1111/jmft.12261. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roozen HG, de Waart R, van der Kroft P. Community reinforcement and family training: an effective option to engage treatment-resistant substance-abusing individuals in treatment. Addiction. 2010;105(10):1729–1738. doi: 10.1111/j.1360-0443.2010.03016.x. [DOI] [PubMed] [Google Scholar]
- Sanford K, Bingham CR, Zucker RA. Validity issues with the family environment scale: Psychometric resolution and research application with alcoholic families. Psychological Assessment. 1999;11(3):315–325. [Google Scholar]
- Schell TL, Marshall GN. Survey of individuals previously deployed for OEF/OIF. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. 2008:87–115. [Google Scholar]
- Skopp NA, Reger MA, Reger GM, Mishkind MC, Raskind M, Gahm GA. The role of intimate relationships, appraisals of military service, and gender on the development of posttraumatic stress symptoms following Iraq deployment. Journal of Traumatic Stress. 2011;24(3):277–286. doi: 10.1002/jts.20632. [DOI] [PubMed] [Google Scholar]
- Smith JE, Meyers RJ. Motivating Substance Abusers to Enter Treatment: Working with Family Members. 1. The Guilford Press; 2007. [Google Scholar]
- Spielberger CD. State-Trait Anger Expression Inventory-2 (STAXI-2) Odessa, FL: PAR/Psychological Assessment Resources; 1999. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stuart RB. Operant-interpersonal treatment for marital discord. Journal of consulting and clinical psychology. 1969;33(6):675. doi: 10.1037/h0028475. [DOI] [PubMed] [Google Scholar]
- Tanielian T, Trail TE, Cory N. Designing and implementing strategic research studies to support military families. In: Wadsworth SM, editor. Stress in U.S. military families. New York: Springer; (in press) [Google Scholar]
- Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Verdeli H, Baily C, Vousoura E, Belser A, Singla D, Manos G. The case for treating depression in military spouses. J Fam Psychol. 2011;25(4):488–496. doi: 10.1037/a0024525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RL, Hops H, Patterson GR. A framework for conceptualizing marital conflict: A technology for altering it, some data for evaluating it. In: Handy LD, Mash EL, editors. Behavior change: Methodology, concepts, and practice. Champaign, IL: Research Press; 1973. pp. 309–342. [Google Scholar]