Abstract
This study examined racial/ethnic disparities in three core postpartum depression (PPD) symptoms, and identified specific predictors of PPD including sociodemographic variables, life stressors and maternal employment. White, African American, Hispanic, and Asian/Pacific Islander women from the New York City area (n=3,010) completed the 2009–2011 Pregnancy Risk Assessment Monitoring System. African American women were less likely to have PPD than White women. Maternal employment during the postpartum was associated with an increased likelihood of PPD for White women relative to women who were not employed. Life stressors and maternal employment should be considered as culturally contextualized factors related to postpartum depression.
Keywords: postpartum depression, racial disparities, employment, stressful life events
Introduction
Approximately 19.2% of all women experience postpartum depression (PPD) (Gavin et al., 2005), however, little is known about racial/ethnic differences in prevalence, the risks, and the experience of the depression symptomatology (Chentsova-Dutton & Tsai, 2007; O’ Hara, 2009; Kleinman, 2004). To date, the data on prevalence is mixed (Howell, Mora, Horowitz, & Leventhal, 2005; Wei, Greaver, Marson, Herndon, & Rogers, 2008; Yonkers, Ramin, Rush, & Navarrete, 2001). For instance, Howell et al., (2005) found that African American and Hispanic women reported more PPD symptoms than White women. This is in contrast to Yonkers and colleagues’ (2001) study, which observed that rates of PPD among Hispanic and African American women were comparable to rates of PPD reported by White women. These mixed findings suggest the possibility that sociodemographic risk variables (Beeghly et al., 2003; Hobfoll, Ritter, Lavin, Hulsizer, & Cameron, 1995; Rich-Edwards et al., 2006) or factors that vary by culture such as social support or language (Huang, Wong, Ronzio, & Yu, 2007; Yonkers et al., 2001), or stigma of having PPD (Kleinman, 2004), (Georg Hsu et al., 2008) may account for these observed race/ethnic differences.
If prenatal life stressors predicts PPD, and certain racial/ethnic groups are faced with greater social and economic adversity, then the life experiences of different groups ought to be considered in predicting PPD (Da Costa, Larouche, Dritsa, & Brender, 2000; Lancaster et al., 2010; O’hara & Swain, 1996; Robertson, Grace, Wallington, & Stewart, 2004; Zayas, Cunningham, Mckee, & Jankowski, 2002). Indeed, the level (e.g., number of total stressors) and the type of exposures (moving, a family death, poverty) of prenatal stress and the type of depression symptomatology (e.g., sadness, loss of interest) vary by race/ethnicity (Liu, Giallo, Doan, Seidman, & Tronick, 2016; Liu & Tronick, 2012). Although this may not be surprising given that such experiences are contextualized by cultural beliefs and practices, (Hobfoll, 1998) the factors associated with PPD are not well understood among diverse postpartum women.
There is also limited research on the role of maternal employment during the postpartum and its association with PPD. The limited research on maternal employment and mental health is a surprising omission given the relationship between stressful life events and increased risk for PPD (Liu, Giallo, Doan, Seidman, & Tronick, 2016; Pfost, Stevens, & Lum, 1990), as maternal employment following birth poses a significant life experience for many families. Studies that have examined stress including the demands of maternal employment prior to and during pregnancy have focused on negative health outcomes including the risk for preterm birth and low infant birth weight (Lobel et al., 2008; Schetter & Tanner, 2012; Wadhwa, Sandman, Porto, Dunkel-Schetter, & Garite, 1993). There is a small literature on the association of postpartum employment on mental health (Mayberry, Horowitz, & Declercq, 2007; McGovern et al., 2007). For instance, one study found positive work-related variables such as low job stress and coworker support to be associated with decreased endorsement of PPD symptoms (McGovern et al., 2007). In another study, full time employed mothers relative to mothers who were not employed full time were at decreased risk for depression symptoms and symptom severity (Mayberry et al., 2007). The authors noted that full time mothers were more likely to report mild symptoms of depression, while mothers who were not employed full time had higher rates of moderate to severe depression symptoms. The findings on race/ethnic differences are mixed, with either no racial differences (Mayberry et al., 2007) or racial/ethnic minorities showing fewer PPD symptoms in relation to employment (McGovern et al., 2007). In sum, there is little known about the role of maternal employment and its association with postpartum depression symptoms and whether this might vary based by racial/ethnic groups. Investigating racial differences in the relationship between employment and PPD would help employers and service providers better understand the potential impact that employment has on maternal mental health and how this may vary by race/ethnicity.
Finally, studies that have examined race/ethnic disparities have relied on provider diagnoses and screeners such as the Edinburgh Postnatal Depression scale (Cox, Holden, & Sagovsky, 1987). The PRAMS-3D is an ultra-brief measure of depression that examines sadness, hopelessness, and feeling slowed down. As a 3-item screener, it is an efficient method for collecting data on core symptoms of PPD. Its implementation in a large and diverse population dataset produces a sample size that allows for the stratification of race/ethnicity, and thus a comparison across groups, which is often a limitation in understanding race/ethnic differences in the risks and outcomes of postpartum depression.
To address the missing gaps in the literature, the goal of this present study was to examine racial/ethnic disparities when considering three core PPD symptoms as a measure for PPD and to identify specific predictors for PPD, including maternal employment. The PRAMS data collected from 2009–2011 in New York City provides sufficient sample sizes of Whites, Blacks, Hispanics, and Asian/Pacific Islanders (A/PI) so that prevalence can be compared across groups, and where specific predictors for PPD could be examined within group. Furthermore, it relies on three core depression symptoms as an ultra brief screener for PPD. Therefore, our analyses also provide an opportunity to compare PPD prevalence across race/ethnicity and also with previous PPD outcome measures in the PRAMS from 2004–2007, specifically, when the diagnosis is by a provider as reported by the participant (Liu & Tronick, 2012). Finally, we also focused on maternal employment during the postpartum given that is an important life experience that affects the mother and her family and is often overlooked in the literature on PPD.
Materials and Methods
Sample
This study used the NYC PRAMS from 2009–2011, a population-based survey administered to postpartum women from NYC. Coordinated by the Centers for Disease Control and Prevention and state health departments, PRAMS’ goal is to monitor maternal behaviors and experiences of women before, during, and after live birth pregnancies. The NYC Department of Health and Mental Hygiene (DOHMH) provided the dataset.
The participants were part of an ongoing population-based random sampling of NYC live births. NYC mothers of approximately 180 infants with registered birth certificates that gave birth during the previous 2–4 months were contacted for participation monthly. 82.6% percent responded by mail and 17.4% by phone. The sample was randomized without replacement and stratified by birth weight. The final dataset was weighted for stratification, non-selection, and non-response. According to the DOHMH, a total of 4,257 responses were received with a response rate of 65%. Responses represented 117,929, 115,091, and 113,661 live births for 2009, 2010, and 2011, respectively.
Measures
The birth certificate provided information on maternal race/ethnicity and nativity (i.e., U.S. or non-U.S. born mothers). Women were classified as Hispanic or non-Hispanic based on self-report. Non-Hispanic women were categorized in one of the following groups: White, African American, and Asian/Pacific Islander (A/PI) to obtain Maternal Race. Maternal Age, Nativity (U.S. Born versus Foreign Born) and Maternal Education (categorized as: 0–8, 9–11, 12, 13–15, and >16 years) were based at the time of infant birth from information in the birth certificate. Mean infant age at the time of survey completion was 3.9 months; there was no significant difference in infant age across race/ethnic groups.
The PRAMS survey itself provided information for remaining variables. To obtain Household Income, women were asked to indicate “total household income before taxes in the 12 months before the new baby was born” by checking off one of the following options: <$10,000, $10,000–$14,999, $15,000–$19,999, $20,000–$24,999, $25,000–$34,999, $35,000–$49,999, $50,000–$74,999, and >$75,000. Stressful events during pregnancy were obtained by “yes” or “no” responses to events that may have occurred during the last 12 months before the new baby was born. Examples include “I moved to a new address,” “I had a lot of bills to pay,” “I got separated or divorced from my husband or partner,” and “Someone very close to me died.” These events were counted and categorized into the following: 0, 1–2, 3–5, and 6–13 events to comprise a number of Total Stressors. A “yes” or “no” response was also used to obtain information on Intention for Pregnancy, assessed through the item, “When you got pregnant with your new baby, were you trying to get pregnant?” Maternal Employment was assessed through the item “Are you currently working outside the home?” We selected only respondents with infants who were alive at the time of the survey response.
The NYC PRAMS included additional questions that produced three factors on experiences related to depression. Mothers were asked to indicate how often they endorsed feeling or experiencing each factor on a 5-point Likert scale from 1 (Never) to 5 (Always) regarding Sad Mood (“I felt down, depressed, or sad”), Hopelessness (“I felt hopeless”) and Slowed Down (“I felt slowed down”). This three-item PRAMS-3D screener produces an overall score for depression through the sum of the subscales, with values ranging from 3 to 15. The recommended cutoff score for PRAMS-3D was used to determine depression (≥9) versus non-depression (<9) (Davis, Pearlstein, Stuart, O’Hara, & Zlotnick, 2013). The use of these items are determined to be effective as a brief screening tool for PPD, with the three items having moderate accuracy for predicting PPD as determined by structured clinical interviews (Davis et al., 2013). All subsequent results here within assume PPD based on a score equal or greater to 9.
Variables
The independent variables (predictors) were selected based on the previous literature and the availability of variables from the survey. These included socio-demographic variables (race/ethnicity, income, education), the number of prenatal stressful events and unintended pregnancy.
Responses with missing variables of interest for this study were eliminated. Variables with less than a 100% response rate included Sad Mood (91.4%), Hopelessness (89.5%), Slowed Down (89.9%), Maternal Race (96.9%), Maternal Education (99.8%), Nativity (96.8%), Household Income (86.0%), Total Stressors (98.8%), Maternal Employment (97.0%), Intention for Pregnancy (97.3%), and Infant Currently Alive (95.5%), resulting in an un-weighted study sample of 3,010.
The Institutional Review Board of the New York City Department of Health and Mental Hygiene approved the use of this dataset.
Statistical Analyses
To account for the stratified and weighted sample, the data was analyzed using the Complex Samples module of SPSS version 23.0 (SPSS Inc., Chicago, IL). Prevalence estimates within each group were generated according to predictors based on variables of interest (Race/Ethnicity, Sociodemographic, Stressors, and Maternal Employment during the postpartum period). A non-race stratified model was conducted to determine the likelihood of receiving a PPD diagnosis. To understand associated predictors by race, race-stratified logistic regressions incorporated all predictors. Note that our models failed to converge with the inclusion of infant age because of low cell sizes; thus, this variable was dropped from our analyses. Unless otherwise noted, all reported proportions represent weighted averages.
Results
Our measure of PPD, which relied on cutoffs from the PRAMS-3D showed no differences in PPD rate based on race/ethnicity, with rates ranging from 15.1% to 17.8% representing those that exceeded the cutoff (Table 1). In general, more White and A/PI women were older, more educated, and were at a higher level of income relative to Hispanic and African American women. Compared to other race/ethnic groups, A/PI had the highest rate of non-U.S. born women at 84.3%, followed by Hispanics at 57.2%, African American at 43.4%, and Whites at 29.7%. With respect to pregnancy intention, White and A/PI women were also more likely than Hispanic and African American women to have a pregnancy at the time they had intended. There was a lower rate among Hispanic women to be employed during the postpartum period compared to the other three groups at 36.5%.
Table 1.
Proportion of women according to sociodemographic factors, number of prenatal life stressors, maternal employment during the postpartum, and PPD based on PPD threshold by race/ethnicity
| White | Asian/Pacific Islander | Hispanic | African American | |
|---|---|---|---|---|
| (n=838) | (n=463) | (n=985) | (n=724) | |
| Maternal Age | ||||
| <20 | 1.0a | 2.0a | 10.9b | 7.7c |
| 20–34 | 70.1a | 74.4a,b | 74.6b | 76.1b |
| ≥35 | 28.9a | 23.5b | 14.5c | 16.2c |
| Maternal Education | ||||
| 0–8 | 0.2a | 4.0b | 11.4c | 2.4b |
| 9–11 | 1.9a | 13.6b | 21.1c | 15.3b |
| 12 | 16.4a | 17.4a | 24.6b | 26.1b |
| 13–15 | 17.5a | 14.7a | 28.0b | 37.2c |
| ≥16 | 63.9a | 50.3b | 14.8c | 19.0d |
| Income | ||||
| <10,000 | 8.0a | 16.6b | 34.4c | 27.3d |
| 10,000–14,999 | 6.6a | 17.7b | 17.6b | 10.3c |
| 15,000, 19,999 | 3.9a | 7.6b | 9.0b | 8.5b |
| 20,000–24,999 | 3.2a | 7.5b | 8.0c | 12.4d |
| 25,000–34,999 | 6.7a | 6.4a | 9.5b | 15.0c |
| 35,000–49,999 | 6.9a | 4.8a | 7.3a | 10.0b |
| 50,000–74,999 | 10.7a | 7.4a | 5.6b | 9.2a |
| ≥75,000 | 53.9a | 32.0b | 8.6c | 7.3c |
| Maternal Nativity | ||||
| U.S. Born | 70.3a | 15.7b | 42.8c | 56.6c |
| Non-U.S. Born | 29.7a | 84.3b | 57.2c | 43.4c |
| Stresses | ||||
| 0 | 42.8a | 46.0a | 26.7b | 22.6b |
| 1–2 | 42.5a | 43.6a | 44.4a | 42.2a |
| 3–5 | 14.5a | 8.8b | 24.0c | 29.7d |
| 6–13 | 0.2a | 1.5b | 4.9c | 5.5c |
| Intention for Pregnancy | ||||
| Sooner | 26.3a | 26.9b | 12.2c | 16.6d |
| Later | 16.0a | 23.8b | 39.1c | 38.0c |
| Then | 55.2a | 42.6b | 39.5b | 31.7c |
| Did not want | 2.5a | 6.7b | 9.2b | 13.7c |
| Maternal Employment | ||||
| No | 52.6a | 56.3a,c | 63.5b | 58.4c |
| Yes | 47.4a | 43.7a,c | 36.5b | 41.6c |
| Postpartum Depression Diagnosis | ||||
| No | 82.2a | 83.2a | 82.7a | 84.9a |
| Yes | 17.8a | 16.8a | 17.3a | 15.1a |
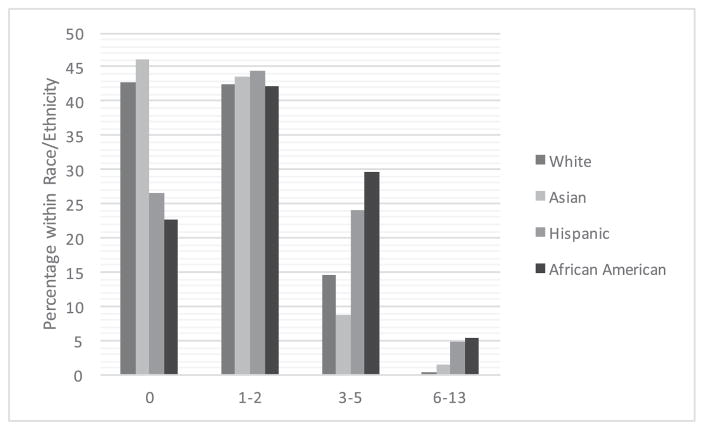
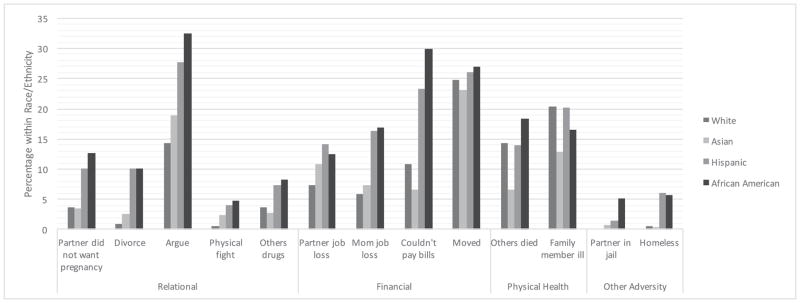
We examined the percentage of women based on the number of stressors endorsed according to race/ethnicity (Table 1, Figure 1). More Whites and A/PI endorsed having experienced no stressors relative to Hispanics and African Americans. No racial/ethnic differences were observed among those who endorsed 1–2 stressors, whereas more Hispanics and Blacks compared to Whites and A/PI endorsed 3–5 or 6 or more stressors. We also examined percentage of women who endorsed specific stressors according to race/ethnicity (Figure 2). The most common stressors for each group, as defined by a rate of over 20%, included moving and family members who were ill among Whites, moving and arguments among A/PI, moving, arguments, couldn’t pay bills, and family members who were ill among Hispanics, and moving, couldn’t pay bills, and arguments in African Americans.
Figure 1.
Percentage of women endorsing 0, 1–2, 3–5, and 6–13 stressors by race/ethnicity
Figure 2.
Percentage of women endorsing specific types of stressors by race/ethnicity
In reporting these more common stressors, we found no significant difference in the race/ethnic groups in reported moving. However, 32.5% of African American women and 27.7% of Hispanic women reported having frequent arguments during the prenatal period, which was significantly higher than White and A/PI women. Moreover, there was a significant difference in the report of being unable to pay bills, with African Americans at 29.9% and Hispanics at 23.3% reporting this to be a stressor relative to Whites and A/PI.
A major objective was whether sociodemographic variables, stressor variables, and maternal employment in the postpartum accounted for PPD. In the unadjusted model, we observed no race/ethnic differences in the likelihood for PPD. After adjusting for sociodemographic variables, stressor variables, and maternal employment, African American women were significantly less likely than White women to have PPD (Table 2). Other factors that were associated with PPD for all women included having 16 or more years of education, having at least 1 stressor, with a 1.8 times increase with 1–2 stressors endorsed, 3.4 times increase with 3–5 stressors, and 10.6 times increase with 6+ stressors. Finally, maternal employment in the postpartum period increased the likelihood of postpartum depression by 1.5 times in the overall sample.
Table 2.
Logistic regression models of race/ethnicity, other sociodemographic factors, number of prenatal life stressors, maternal employment during the postpartum with unadjusted and adjusted odds of having PPD based on PPD threshold (n=3,010)
| Unadjusted Model | Adjusted Model | |||
|---|---|---|---|---|
| Race | OR | CI | OR | CI |
| White | 1.0 | -- | 1.0 | -- |
| Asian/Pacific Islander | 0.9 | 0.6–1.3 | 0.9 | 0.6–1.3 |
| Hispanic | 1.0 | 0.7–1.3 | 0.8 | 0.6–1.1 |
| African American | 0.8 | 0.6–1.1 | 0.5* | 0.4–0.8 |
| Maternal Age | ||||
| <20 | 1.0 | -- | ||
| 20–34 | 0.9 | 0.5–1.7 | ||
| ≥35 | 1.0 | 0.5–1.9 | ||
| Maternal Education | ||||
| 0–8 | 1.0 | -- | ||
| 9–11 | 1.5 | 0.7–3.0 | ||
| 12 | 1.0 | 0.5–2.2 | ||
| 13–15 | 1.9 | 0.9–3.7 | ||
| ≥16 | 2.0† | 1.0–4.2 | ||
| Income | ||||
| <10,000 | 1.0 | -- | ||
| 10,000–14,999 | 1.0 | 0.7–1.6 | ||
| 15,000, 19,999 | 1.2 | 0.7–2.0 | ||
| 20,000–24,999 | 1.1 | 0.7–1.8 | ||
| 25,000–34,999 | 1.2 | 0.8–2.0 | ||
| 35,000–49,999 | 0.7 | 0.4–1.3 | ||
| 50,000–74,999 | 1.2 | 0.7–1.9 | ||
| ≥75,000 | 0.8 | 0.5–1.3 | ||
| Maternal Nativity | ||||
| U.S. Born | 1.0 | -- | ||
| Non-U.S. Born | 1.1 | 0.9–1.5 | ||
| Stresses | ||||
| 0 | 1.0 | -- | ||
| 1–2 | 1.8*** | 1.3–2.4 | ||
| 3–5 | 3.4*** | 2.4–4.9 | ||
| 6+ | 10.6*** | 5.9–19.0 | ||
| Intention for Pregnancy | ||||
| Do not want | 1.0 | -- | ||
| Sooner | 0.7 | 0.5–1.1 | ||
| Later | 0.6* | 0.4–0.9 | ||
| Then | 0.5* | 0.3–0.7 | ||
| Maternal Employment | ||||
| No | 1.0 | -- | ||
| Yes | 1.5** | 1.2–2.0 | ||
p<0.1,
p<.05,
p<.01,
p<.001
When stratifying our analyses by race/ethnicity, we found that associations varied greatly by ethnicity (Table 3). First, White and African American women with a maternal education beyond 8th grade were less likely to have PPD, although Hispanics with 9–11 years, 13–15 years, and 16 years of education were more likely to have PPD. No conclusions were drawn from the A/PI sample likely due to small cell sizes resulting in wide confidence intervals. Only certain levels of income were associated with PPD, including $20,000–$24,999 for Whites and $25,000–$34,999 for Hispanics. In contrast, $35,000–$49,000 predicted a lower likelihood for PPD in African Americans. Relative to no stressors, having 3–5 stressors was associated with PPD for Whites, Hispanics, and African Americans, and 6+ stressors were associated with PPD only for Hispanics and African Americans. Again, no conclusions were drawn for A/PI likely due to small cell sizes, which resulted in wide confidence intervals. Maternal employment during the postpartum was associated with PPD for only Whites and A/PI but not for Hispanics or African Americans. Finally, neither maternal nativity nor pregnancy intention was associated with PPD.
Table 3.
Logistic regression models of race/ethnicity, other sociodemographic factors, number of prenatal life stressors, maternal employment during the postpartum with adjusted odds of having PPD based on PPD threshold (n=3,010)
| Maternal Age | OR | CI | OR | CI | OR | CI | OR | CI |
|---|---|---|---|---|---|---|---|---|
| <20 | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- |
| 20–34 | 0.1 | 0.0–0.9 | 0.8 | 0.2–4.8 | 0.9 | 0.4–2.1 | 1.5 | 0.4–5.4 |
| ≥35 | 0.1 | 0.0–1.0 | 1.3 | 0.2–8.4 | 0.9 | 0.4–2.4 | 1.1 | 0.3–4.3 |
| Maternal Education | ||||||||
| 0–8 | 1.0 | -- | 1.0 | 1.0 | -- | 1.0 | -- | |
| 9–11 | 0.0* | 0.0–0.4 | 10.3a | 1.2–93.0 | 3.4* | 1.1–10.2 | 0.1* | 0.3–0.5 |
| 12 | 0.0* | 0.0–0.1 | 15.0a | 1.9–119.8 | 2.3 | 0.8–6.9 | 0.1* | 0.0–0.4 |
| 13–15 | 0.0* | 0.0–0.3 | 21.2a | 2.5–180.1 | 3.8* | 1.3–10.9 | 0.2* | 0.0–0.7 |
| ≥16 | 0.0* | 0.0–0.3 | 24.0a | 3.0–193.9.0 | 3.3* | 1.1–10.2 | 0.4 | 0.1–1.7 |
| Income | ||||||||
| <10,000 | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- |
| 10,000–14,999 | 2.8 | 0.5–14.2 | 0.8 | 0.3–2.4 | 0.5 | 0.3–1.0 | 1.9 | 0.8–4.6 |
| 15,000, 19,999 | 1.1 | 0.1–9.0 | 2.0 | 0.5–8.1 | 1.2 | 0.6–2.4 | 0.9 | 0.4–2.4 |
| 20,000–24,999 | 5.8* | 1.2–29.0 | 1.3 | 0.3–5.0 | 1.1 | 0.5–2.5 | 0.4 | 0.2–1.0 |
| 25,000–34,999 | 1.4 | 0.3–6.3 | 1.4 | 0.3–5.5 | 2.2* | 1.0–4.8 | 0.5 | 0.2–1.1 |
| 35,000–49,999 | 1.0 | 0.2–5.2 | 1.9 | 0.5–6.8 | 1.2 | 0.5–2.6 | 0.2* | 0.1–0.5 |
| 50,000–74,999 | 2.8 | 0.7–11.5 | 0.8 | 0.2–3.1 | 1.7 | 0.7–4.2 | 0.4 | 0.1–1.4 |
| ≥75,000 | 1.9 | 0.5–7.5 | 0.5 | 0.2–1.6 | 1.0 | 0.4–2.4 | 0.5 | 0.1–1.7 |
| Maternal Nativity | ||||||||
| U.S. Born | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- |
| Non-U.S. Born | 0.8 | 0.5–1.2 | 1.2 | 0.5–3.0 | 1.4 | 0.9–2.2 | 1.4 | 0.8–2.4 |
| Stresses | ||||||||
| 0 | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- |
| 1–2 | 1.7† | 1.0–2.8 | 2.2 | 1.1–4.5 | 1.6 | 0.9–2.9 | 1.9 | 0.8–4.4 |
| 3–5 | 2.9*** | 1.6–5.5 | 7.8a | 2.9–20.8 | 3.4*** | 1.9–6.3 | 3.2** | 1.3–7.5 |
| 6–18 | 0.4 | 0.0–8.4 | 7.7a | 0.9–67.9 | 11.5*** | 4.5–29.0 | 10.5*** | 3.4–32.2 |
| Intention for Pregnancy | ||||||||
| Do not want | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- |
| Sooner | 1.2 | 0.3–4.6 | 0.5 | 0.2–1.5 | 0.6 | 0.3–1.3 | 0.9 | 0.4–2.3 |
| Later | 1.4 | 0.4–5.2 | 0.4 | 0.1–1.3 | 0.6 | 0.3–1.2 | 0.5 | 0.2–1.1 |
| Then | 0.8 | 0.2–2.8 | 0.3 | 0.1–1.0 | 0.5 | 0.2–1.0 | 0.5 | 0.2–1.2 |
| Maternal Employment | ||||||||
| No | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- |
| Yes | 2.0*** | 1.2–3.0 | 2.1*** | 1.1–4.0 | 1.4 | 0.9–2.2 | 1.4 | 0.8–2.4 |
p<0.1,
p<.05,
p<.01,
p<.001,
Confidence intervals too wide and must be interpreted with caution
Discussion
The goal of this present study was to examine racial/ethnic disparities in three core PPD symptoms and to identify specific predictors for PPD, including maternal employment. The prevalence of PPD across groups in this 2009–2011 dataset (range of 15.1% to 17.8%), based on the PRAMS-3D which produced a cut off score, was consistent with prevalence based from other PPD screeners (e.g., Gavin et al., 2005). However, in comparison to the previous literature relying on reported diagnosis among PRAMS participants from New York City in 2004–2007, (Liu & Tronick, 2013) these rates in the current analysis from 2009–2011 data are higher and show no racial/ethnic differences. New York City 2009–2011 and 2004–2009 PRAMS participants were similar socio-demographically, with a greater proportion of White and A/PI women that were older (≥35 years), more educated (≥16 years), and had a higher income level (≥$75,000) compared to Hispanic and African American women. In both datasets, there was a greater proportion of A/PI who were non-U.S. born and White and A/PI women were more likely to have an intended pregnancy relative to Hispanics and African Americans.
Together, one interpretation is that prevalence and race/ethnic differences of PPD between these two data collections may be due to the specific outcome measure used for PPD. First, the observation of higher overall prevalence rates when using the three-item screener than a reported diagnosis is not surprising, as screeners are intended to detect possible depression, that requires a follow-up assessment and diagnosis by a provider. Thus, prevalence rates determined by screeners will be greater than prevalence determined by diagnosis. Second, the greater race/ethnic differences when relying on a diagnosis as compared to a three-item screener may be attributed to providers and the information they gather when meeting with a patient that may encompass both provider knowledge of culturally specific manifestation of depression, but also provider biases regarding behavior (Liu & Tronick, 2012). For instance, A/PI may be less likely to endorse the items, as depression is often more likely to be somatized and described in physical terms or bodily complaints such as headaches, shortness of breath, or sleep disturbances (Parker, Cheah, & Roy, 2001). As well, it is certainly possible that racial/ethnic variations in the symptoms of PPD (Liu & Tronick, 2013) could be masked by the summation of a score across three items. However, to the extent that PPD reflects moderate-to-high levels of at least two depression symptoms for all groups, we conclude that the use of a cut off score as showed through previous analysis of the PRAMS-3D (Davis et al., 2013) indicates that the groups in this study do not significantly differ in total severity.
Our analyses revealed that greater numbers of endorsed stressors was associated with PPD, consistent with the overall literature indicate life stress as a risk for PPD (Boyce & Hickey, 2005; Liu & Tronick, 2013; Rubertsson, Wickberg, Gustavsson, & Rådestad, 2005). With regards to race/ethnicity our data revealed a greater number of exposures to stressful life events among African American and Hispanic women, compared to White and A/PI women. Moreover, the type of stressors experienced differ across the ethnic groups; we found that arguments and difficulty with paying bills were more common stressors for African and Hispanic women than for White and A/PI women, while moving was a more prevalent stressor for both A/PI and Whites.
Moreover, our data also suggests different associations between the number of stressors and PPD symptoms, such that African American and Hispanics endorsed a higher number of stressors as compared to Whites and A/PI. Furthermore, in the overall sample we observed that maternal employment in the postpartum was associated with an increased likelihood of PPD. This is in contrast to previous literature that points to the protective capacity of postpartum employment on maternal mental health (Mayberry et al., 2007; McGovern et al., 2007). Second, race-stratified analyses revealed a relation between maternal employment and postpartum depression only in White and A/PI women.
The lack of association between employment and postpartum depression for Hispanics and African Americans may be explained by social support and attitudes about work. Specifically, while White mothers report the largest support network, Hispanic and African American mothers tend to receive a higher proportion of their social support from family members, and tend to perceive these interactions as higher in quality than those of White mothers (Koniak-Griffin, Lominska, & Brecht, 1993). Indeed, racial differences in social support is further exemplified through qualitative accounts that Hispanic and African American mothers are more proactive than White mothers in mobilizing support in the postpartum period, using of direct instruction and education about housework and infant caretaking (Negron, Martin, Almog, Balbierz, & Howell, 2013). It is important to consider that size, quality, and composition of social support networks in the postpartum differ among racial groups, (Koniak-Griffin et al., 1993; Sagrestano, Feldman, Rini, Woo, & Dunkel-Schetter, 1999) and that for groups such as African American and Hispanics, this social support might buffer the quantity and type of stressors that would otherwise be a risk for PPD.
In addition to the provisions of social support, racial/ethnic differences beliefs about work may also be a buffer to the postpartum risks conferred by stressful life events. Indeed, qualitative and quantitative accounts note African American women’s preference and orientation to work over that of their white counterparts (Bridges & Etaugh, 1994; Gjerdingen, Mcgovern, Attanasio, Johnson, & Kozhimannil, 2014; Spitze & Waite, 1980). Possible explanations for the source of this orientation have suggested that maternal role modeling, financial obligations, and social/community expectations impact African Americans women’s decisions to work, (Beauboeuf-Lafontant, 2007; Macke & Morgan, 1979; Spitze & Waite, 1980) and such ideals could extend and operate into the postpartum period. For example, one study examining racial differences between college students’ perceptions of a mother working with a 1-year-old infant revealed that African American female students, as compared to White female students, tended to expect fewer costs and more rewards in employment (Bridges & Etaugh, 1994). This preference among African Americans to evaluate the financial benefits of work is further supported by another study on racial differences in work preferences, which revealed that Black workers tended to prefer higher incomes, as compared to White workers who tend to prefer feeling accomplished in a job (Weaver, 1975). Thus, while protective capacity of increased stressors against PPD may appear counterintuitive, other factors such as social support or preferences to work for particular groups serve as a buffer to postpartum mental health, even in light of increased stress risks for PPD. Given the dearth of literature on this topic, further investigation is warranted in order to better understand racial/ethnic differences in the relationship between employment (specifically in the postpartum) and PPD.
Limitations and Future Directions
Our study contains limitations to be considered in the interpretation of findings. With self-reported data, retrospective response bias may be possible, although likely reduced because the events presented to our participants were highly salient and largely within the context of their recent pregnancy. The use of a single item for maternal employment is a limitation, as it does not provide information on the quantity, quality, and timing of the maternal experience with work. The survey also did not include additional items that provided information about social support and other postpartum experiences that could moderate the association between maternal employment and PPD. Despite the population level data, we could not examine subgroups within race/ethnic categories due to low statistical power. Individual experiences based on the heterogeneity of the race/ethnicity may have been overlooked. Finally, our analyses identify significant associations in the data but do not demonstrate causality. Thus, we do not know to what extent maternal employment experiences in the postpartum accounts for the experience of PPD. Moreover, we were unable to test whether qualitative differences in social support and attitudes towards work explain some of our racial/ethnic differences. Future work should test these meditational models. In contrast to past work (Mayberry et al., 2007; McGovern et al., 2007; Miyake, Tanaka, Sasaki, & Hirota, 2011), our study found that work did not buffer against PPD. Past studies have focused specifically on the positive relationship between work-related variables and maternal wellbeing such as full-time employment status, coworker support, supervisor support, and a sense of control over the work environment (McGovern et al., 2007). Since our findings suggest that work-related variables may impact maternal well-being negatively, further study is needed to clarify this relationship. Understanding implicit and/or explicit factors related to working in the postpartum, such as labor demands, balancing responsibilities, or stress, have implications for mothers, service providers and employers about factors that impact maternal mental health. Additional studies on different time periods may clarify the association over time. For instance, it may be possible that the negative association between employment status and PPD changes over time.
Conclusions
Our findings indicate racial/ethnic variations in the pregnancy and postpartum experiences of New York City women. While PPD prevalence rates did not differ by race/ethnicity based on the PRAM-3D as a screener, our race-stratified analyses allowed us to uncover racial/ethnic differences at the level of risk for PPD. African American and Hispanics relative to Whites and A/PI endorsed a greater number of stressors overall during the pregnancy, with frequent arguments and difficulty with paying bills being common stressors. Yet, maternal employment was predictive of PPD for Whites and A/PI and not African American and Hispanics. There are host of reasons for why women would experience PPD. To better understand the risks, we must consider the specific life stressors that women experience due to their race/ethnicity, and culture. Race/ethnic differences in the quantity, quality, and personal and cultural expectations of work, and social and community responses to women in the postpartum period may explain these differential associations. Clinicians and policy makers can improve work-life experiences by identifying what may be a risk and what may be protective based on the unique backgrounds of mothers.
Acknowledgments
The authors would like to acknowledge the NYC Department of Health and Mental Hygiene Bureau of Maternal, Infant and Reproductive Health PRAMS Team, Bureau of Vital Statistics, and the CDC PRAMS Team, Program Services and Development Branch, Division of Reproductive Health. Support for preparing this manuscript was provided through the Commonwealth Research Center (SCDMH82101008006). The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Medical School and its affiliated academic health care centers.
Footnotes
Conflicts of Interest
None of the authors have any conflicts of interests to report.
References
- Beauboeuf-Lafontant T. “You Have to Show Strength”: An Exploration of Gender, Race, and Depression. Gender and Society. 2007;21(1):28–51. http://doi.org/10.1177/0891243206294108. [Google Scholar]
- Beeghly M, Olson K, Weinberg M, Pierre S, Downey N, Tronick E. Prevalence, Stability, and Socio-Demographic Correlates of Depressive Symptoms in Black Mothers During the First 18 Months Postpartum. Maternal and Child Health Journal. 2003;7(3):157–168. doi: 10.1023/a:1025132320321. http://doi.org/10.1023/A:1025132320321. [DOI] [PubMed] [Google Scholar]
- Boyce P, Hickey A. Psychosocial risk factors to major depression after childbirth. Social Psychiatry and Psychiatric Epidemiology. 2005;40(8):605–612. doi: 10.1007/s00127-005-0931-0. http://doi.org/10.1007/s00127-005-0931-0. [DOI] [PubMed] [Google Scholar]
- Bridges JS, Etaugh C. Black and white college women’s perceptions of early maternal employment. Psychology of Women Quarterly. 1994;18(3):427–431. http://doi.org/10.1111/j.1471-6402.1994.tb00465.x. [Google Scholar]
- Chentsova-Dutton YE, Tsai JL. Cultural factors influence the expression of psychopathology. In: Lilienfeld SO, O’Donohue WT, editors. The great ideas of clinical science: 17 principles that every mental health professional should understand. New York: Routledge/Taylor & Francis Group; 2007. pp. 375–396. [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry: The Journal of Mental Science. 1987;150:782. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Da Costa D, Larouche J, Dritsa M, Brender W. Psychosocial correlates of prepartum and postpartum depressed mood. Journal of Affective Disorders. 2000;59(1):31–40. doi: 10.1016/s0165-0327(99)00128-7. http://doi.org/10.1016/S0165-0327(99)00128-7. [DOI] [PubMed] [Google Scholar]
- Davis K, Pearlstein T, Stuart S, O’Hara M, Zlotnick C. Analysis of brief screening tools for the detection of postpartum depression: comparisons of the PRAMS 6-item instrument, PHQ-9, and structured interviews. Archives of Women’s Mental Health. 2013;16(4):271. doi: 10.1007/s00737-013-0345-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavin N, Gaynes B, Lohr K, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression - A systematic review of prevalence and incidence. Obstetrics And Gynecology. 2005;106(5):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Georg Hsu LK, Wan YM, Chang H, Summergrad P, Tsang BYP, Chen H. Stigma of Depression Is More Severe in Chinese Americans than Caucasian Americans. Psychiatry. 2008;71(3):210–218. doi: 10.1521/psyc.2008.71.3.210. http://doi.org/10.1521/psyc.2008.71.3.210. [DOI] [PubMed] [Google Scholar]
- Gjerdingen D, Mcgovern P, Attanasio L, Johnson PJ, Kozhimannil KB. Maternal depressive symptoms, employment, and social support. Journal of the American Board of Family Medicine: JABFM. 2014;27(1):87–96. doi: 10.3122/jabfm.2014.01.130126. http://doi.org/10.3122/jabfm.2014.01.130126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll SE. Stress, culture, and community: The psychology and philosophy of stress. New York: Plenum Press; 1998. [Google Scholar]
- Hobfoll SE, Ritter C, Lavin J, Hulsizer MR, Cameron RP. Depression prevalence and incidence among inner-city pregnant and postpartum women. Journal of Consulting and Clinical Psychology. 1995;63(3):445–53. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]
- Howell EA, Mora PA, Horowitz CR, Leventhal H. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstetrics and Gynecology. 2005;105(6):1442–50. doi: 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman A. Culture and Depression. The New England Journal of Medicine. 2004;351(10):951–953. doi: 10.1056/NEJMp048078. http://doi.org/10.1056/NEJMp048078. [DOI] [PubMed] [Google Scholar]
- Koniak-Griffin D, Lominska S, Brecht ML. Social support during adolescent pregnancy: a comparison of three ethnic groups. Journal of Adolescence. 1993;16(1):43–56. doi: 10.1006/jado.1993.1004. http://doi.org/10.1006/jado.1993.1004. [DOI] [PubMed] [Google Scholar]
- Lancaster C, Gold K, Flynn H, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: A systematic review. American Journal Of Obstetrics And Gynecology. 2010;205(3):236–236. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CH, Giallo R, Doan SN, Seidman LJ, Tronick E. Racial and Ethnic Differences in Prenatal Life Stress and Postpartum Depression Symptoms. Archives of Psychiatric Nursing. 2016;30(1):7. doi: 10.1016/j.apnu.2015.11.002. http://doi.org/10.1016/j.apnu.2015.11.002. [DOI] [PubMed] [Google Scholar]
- Liu C, Tronick E. Do Patient Characteristics, Prenatal Care Setting, and Method of Payment Matter When it Comes to Provider-Patient Conversations on Perinatal Mood? Maternal and Child Health Journal. 2012;16(5):1102–1112. doi: 10.1007/s10995-011-0835-4. http://doi.org/10.1007/s10995-011-0835-4. [DOI] [PubMed] [Google Scholar]
- Liu C, Tronick E. Rates and Predictors of Postpartum Depression by Race and Ethnicity: Results from the 2004 to 2007 New York City PRAMS Survey (Pregnancy Risk Assessment Monitoring System) Maternal and Child Health Journal. 2013;17(9):1599–1610. doi: 10.1007/s10995-012-1171-z. http://doi.org/10.1007/s10995-012-1171-z. [DOI] [PubMed] [Google Scholar]
- Lobel M, Cannella DL, Graham JE, Devincent C, Schneider J, Meyer BA. Pregnancy-Specific Stress, Prenatal Health Behaviors, and Birth Outcomes. Health Psychology. 2008;27(5):604–615. doi: 10.1037/a0013242. http://doi.org/10.1037/a0013242. [DOI] [PubMed] [Google Scholar]
- Macke AS, Morgan WR. Maternal Employment, Race, and Work Orientation of High School Girls. Social Forces 1979 [Google Scholar]
- Mayberry LJ, Horowitz JA, Declercq E. Depression Symptom Prevalence and Demographic Risk Factors Among U.S. Women During the First 2 Years Postpartum. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2007;36(6):542–549. doi: 10.1111/j.1552-6909.2007.00191.x. http://doi.org/10.1111/j.1552-6909.2007.00191.x. [DOI] [PubMed] [Google Scholar]
- McGovern P, Dowd B, Gjerdingen D, Dagher R, Ukestad L, McCaffrey D, Lundberg U. Mothers’ Health and Work-Related Factors at 11 Weeks Postpartum. Annals of Family Medicine. 2007;5(6):519–527. doi: 10.1370/afm.751. http://doi.org/10.1370/afm.751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyake Y, Tanaka K, Sasaki S, Hirota Y. Employment, income, and education and risk of postpartum depression: The Osaka Maternal and Child Health Study. Journal of Affective Disorders. 2011;130(1–2):133–137. doi: 10.1016/j.jad.2010.10.024. http://doi.org/10.1016/j.jad.2010.10.024. [DOI] [PubMed] [Google Scholar]
- Negron R, Martin A, Almog M, Balbierz A, Howell E. Social Support During the Postpartum Period: Mothers’ Views on Needs, Expectations, and Mobilization of Support. Maternal and Child Health Journal. 2013;17(4):616–623. doi: 10.1007/s10995-012-1037-4. http://doi.org/10.1007/s10995-012-1037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’ Hara MW. Postpartum depression: What we know. Journal of Clinical Psychology. 2009;65(12):1258–1269. doi: 10.1002/jclp.20644. http://doi.org/10.1002/jclp.20644. [DOI] [PubMed] [Google Scholar]
- O’hara MW, Swain AM. Rates and risk of postpartum depression—a meta-analysis. International Review of Psychiatry. 1996;8(1):37–54. [Google Scholar]
- Parker G, Cheah YC, Roy K. Do the Chinese somatize depression? A cross-cultural study. Social Psychiatry and Psychiatric Epidemiology. 2001;36(6):287–293. doi: 10.1007/s001270170046. http://doi.org/10.1007/s001270170046. [DOI] [PubMed] [Google Scholar]
- Pfost KS, Stevens MJ, Lum CU. The relationship of demographic variables, antepartum depression, and stress to postpartum depression. Journal of Clinical Psychology. 1990;46(5):588–592. doi: 10.1002/1097-4679(199009)46:5<588::aid-jclp2270460507>3.0.co;2-k. http://doi.org/10.1002/1097-4679(199009)46:5<588::AID-JCLP2270460507>3.0.CO. [DOI] [PubMed] [Google Scholar]
- Rich-Edwards JW, Kleinman K, Abrams A, Harlow BL, Mclaughlin TJ, Joffe H, Gillman MW. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. Journal of Epidemiology and Community Health. 2006;60(3):221. doi: 10.1136/jech.2005.039370. http://doi.org/10.1136/jech.2005.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. General Hospital Psychiatry. 2004;26(4):289–295. doi: 10.1016/j.genhosppsych.2004.02.006. http://doi.org/10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Rubertsson C, Wickberg B, Gustavsson P, Rådestad I. Depressive symptoms in early pregnancy, two months and one year postpartum-prevalence and psychosocial risk factors in a national Swedish sample. Archives of Women’s Mental Health. 2005;8(2):97–104. doi: 10.1007/s00737-005-0078-8. http://doi.org/10.1007/s00737-005-0078-8. [DOI] [PubMed] [Google Scholar]
- Sagrestano L, Feldman P, Rini C, Woo G, Dunkel-Schetter C. Ethnicity and Social Support During Pregnancy. American Journal of Community Psychology. 1999;27(6):869–898. doi: 10.1023/a:1022266726892. http://doi.org/10.1023/A:1022266726892. [DOI] [PubMed] [Google Scholar]
- Schetter CD, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Current Opinion In Psychiatry. 2012;25(2):141–148. doi: 10.1097/YCO.0b013e3283503680. http://doi.org/10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitze G, Waite L. Labor Force and Work Attitudes: “Young Women’s Early Experiences. Sociology of Work and Occupations. 1980;7(1):3. [Google Scholar]
- Wadhwa PD, Sandman CA, Porto M, Dunkel-Schetter C, Garite TJ. The association between prenatal stress and infant birth weight and gestational age at birth: A prospective investigation. American Journal of Obstetrics and Gynecology. 1993;169(4):858–865. doi: 10.1016/0002-9378(93)90016-c. http://doi.org/10.1016/0002-9378(93)90016-C. [DOI] [PubMed] [Google Scholar]
- Weaver CN. Black-white differences in attitudes toward job characteristics. Journal of Applied Psychology. 1975;60(4):438–441. http://doi.org/10.1037/h0076907. [Google Scholar]
- Wei G, Greaver L, Marson S, Herndon C, Rogers J. Postpartum Depression: Racial Differences and Ethnic Disparities in a Tri-racial and Bi-ethnic Population. Maternal and Child Health Journal. 2008;12(6):699–707. doi: 10.1007/s10995-007-0287-z. http://doi.org/10.1007/s10995-007-0287-z. [DOI] [PubMed] [Google Scholar]
- Yonkers K, Ramin S, Rush A, Navarrete C. Onset and persistence of postpartum depression in an inner-city maternal health clinic system. The American Journal of Psychiatry. 2001;158(11):1856–63. doi: 10.1176/appi.ajp.158.11.1856. [DOI] [PubMed] [Google Scholar]
- Zayas LH, Cunningham M, Mckee MD, Jankowski KRB. Depression and negative life events among pregnant African-American and Hispanic women. Women’s Health Issues. 2002;12(1):16–22. doi: 10.1016/s1049-3867(01)00138-4. http://doi.org/10.1016/S1049-3867(01)00138-4. [DOI] [PubMed] [Google Scholar]