Abstract
This study presents the results of four Ligamentum Teres (LT) reconstruction procedures for hip instability with an average of 21.4 months follow-up (range 16.4–27.8). The indication for reconstruction was patients who complained of hip instability (hip giving way on gait or activities of daily living) on a background of a connective tissue disorder and generalized ligamentous laxity. The following data were recorded: age, sex, body mass index, hip range of motion, impingement signs, acetabular coverage (lateral center edge angle and acetabular inclination), acetabular retroversion (ischial spine sign and a crossover sign), femoral alpha angles and femoral neck shaft angles. Four patient recorded outcomes (PROs) were collected at 3 months, 12 months and 24 months. Three patients were female. Three out of four procedures had an improvement in PROs. One patient with bilateral procedures had an improvement in PROs on one side at 1 year but a failure of the graft on the contralateral side. There were no complications reported with the technique. LT reconstruction and concomitant capsular plication in this case series is associated with an improvement in outcomes in three out of four of the patients with hip instability associated with a full thickness tear of the LT and who presented with hip instability on a background of generalized ligamentous laxity and a connective tissue disorder. However, the physical examination, radiographic and intra-operative findings which may help predict who would benefit from LT reconstruction require further investigation.
INTRODUCTION
Bony and soft tissue structures contribute to the stability of the hip joint. The soft tissue components of stability consist of the labrum, capsuloligamentous complex and ligamentum teres (LT) [1]. About 60% less force is required to distract the hip in the presence of a labral tear, supporting the concept of the importance of the labrum in hip stability [2, 3]. The importance of the capsuloligametous complex to hip instability is most noted after reports in the literature of hip instability or dislocation following hip arthroscopy in which a capsulotomy/capsulectomy was performed without closure [4–7]. In the adult, the LT was theorized to have limited biomechanical or vascular importance and hence was routinely sacrificed during procedures involving open surgical hip dislocation [8–10]. However, a recent review on the LT's increasing importance by O’Donnell et al. has highlighted that the LT has an important role in hip proprioception and mechanics [11]. Martin et al. used a string model to assess the excursion of the LT during hip movements. They reported that the LT may contribute to hip stability particularly in external rotation in flexion and internal rotation in extension [12]. In addition, they reported that in patients with inferior acetabular insufficiency or generalized ligamentous laxity, complete LT ruptures may result in instability during squatting and crossing one leg behind the other [12]. Similarly, Kivlan et al. [13] used human cadavers to demonstrate that when the human hip moves into flexion-abduction, the LT moves into a position that provides anterior and inferior stabilization of the hip. Furthermore, the prevalence of LT tears at arthroscopy ranges from 5 to 51%, raising the possibility that it may be a potential pain generator in these patients [14–16].
The optimal management of LT tears is not been clearly defined [17]. Debridement of selected fibers in patients with pain rather than instability has had favorable outcomes [18, 19]. Others have advocated LT reconstruction may help address pain in patients who present with instability [20]. Patients with predominantly instability symptoms are more likely to be female, ligamentous lax and have an increased range of motion of the hip [21]. Hip instability may manifest as groin pain and/or painful clunking or clicking of the hip that may be exacerbated by extension and external rotation activities of the hip [22]. Osseous anatomy may be normal or abnormal in these patients and treatment relies on stabilizing the secondary soft tissue restraints such as the labrum and capsule in addition to osseous corrections [23]. Van Arkel et al. conducted a biomechanical study which showed that the LT as a secondary restraint to hip stability in high flexion, adduction and external rotation with the primary restraints being the lateral arm of the iliofemoral ligament and the ischiofemoral ligament [24]. Therefore, in patients with instability symptoms on a background of connective tissue disorders or generalized ligamentous laxity reconstruction of a torn LT may be an important adjunct to restoration of capsular stability once bony morphology was determined as normal without any gross femur or acetabulum dysplastic characteristics [25]. Simpson et al. [20] were the first to report on the technique of LT reconstruction and Philippon et al. [26] have the largest series of four patients in whom the majority reported improved outcomes with reconstruction. Amenabar et al. [27] also reported improved patient outcomes with LT reconstruction. The purpose of this study is to report on the outcomes in three patients in whom four reconstruction procedures were performed and report indications and early clinical experience. These patients presented with hip instability on a background of ligamentous laxity with a known or probable connective tissue disorder.
METHODS
Patient inclusion and data collection
Data were prospectively collected on all patients undergoing hip arthroscopy between April 2009 and August 2014 and retrospectively reviewed. The inclusion criteria for this study were all patients who underwent arthroscopic LT reconstruction. The institutional review board approved this study. The exclusion criteria were patients with less than one year follow up.
Indications for LT reconstruction
The indications for LT reconstruction were patients who presented with pain and instability of the hip with an associated tear of the LT in the setting of generalized ligamentous laxity on a background of diagnosis of a known connective tissue disorder or a probable connective tissue disorder. LT tears were diagnosed with the aid of magnetic resonance imaging. Patients had persistent symptoms despite a minimum of 3 months of physical therapy. In this patient population, restoration of LT integrity was considered to an important adjunct to restoration of hip stability in addition to labral treatment and capsular plication, once bony morphology was determined as normal without any gross femur or acetabulum dysplastic characteristics.
Clinical evaluation
Symptoms of instability reported included the hip joint feeling unstable on either gait or range of movement, particularly extension and external rotation activities [28]. A history of instability of other joints was actively sought, as was a diagnosis of a connective tissue disorder [28]. Maximum flexion and maximum internal and external rotation at 90° of flexion were recorded. The specific test used to evaluate hip stability involved placing the patient in the supine position and the examiner placing the patient's hip in extension and external rotation. Discomfort or apprehension represented a positive finding. This implies abnormal physiologic motion resulting from soft-tissue deficiencies (e.g. anterior capsular laxity) [29]. Anterior, lateral and posterior impingement test signs were performed as described by Byrd et al. [30] and recorded as either present or absent. Ligamentous laxity was diagnosed according to Beighton's criteria [31].
Imaging
Radiographic measurements
Radiographic views included an AP pelvic view, a 45° Dunn view and a false profile view. Measurements were made including the acetabular inclination (AI) angle using the method described by Jessel et al. [32], the lateral (LCEA) and anterior (ACEA) center edge angle of Wiberg [33], the presence of an ischial spine sign [34], crossover sign [34], alpha angle (Dunn view) [35] and femoral neck shaft angle. The crossover sign size was quantified according to its percent from the acetabulum diameter. All measurements were taken by the same orthopedic surgeon (X.X.) using a picture archiving and communication system computer program.
Preoperatively all patients underwent magnetic resonance imaging (MRI) using a 3T magnet of the affected hip to evaluate for intra-articular and extra-articular pathological abnormalities. The status of the LT was also documented.
Surgical technique
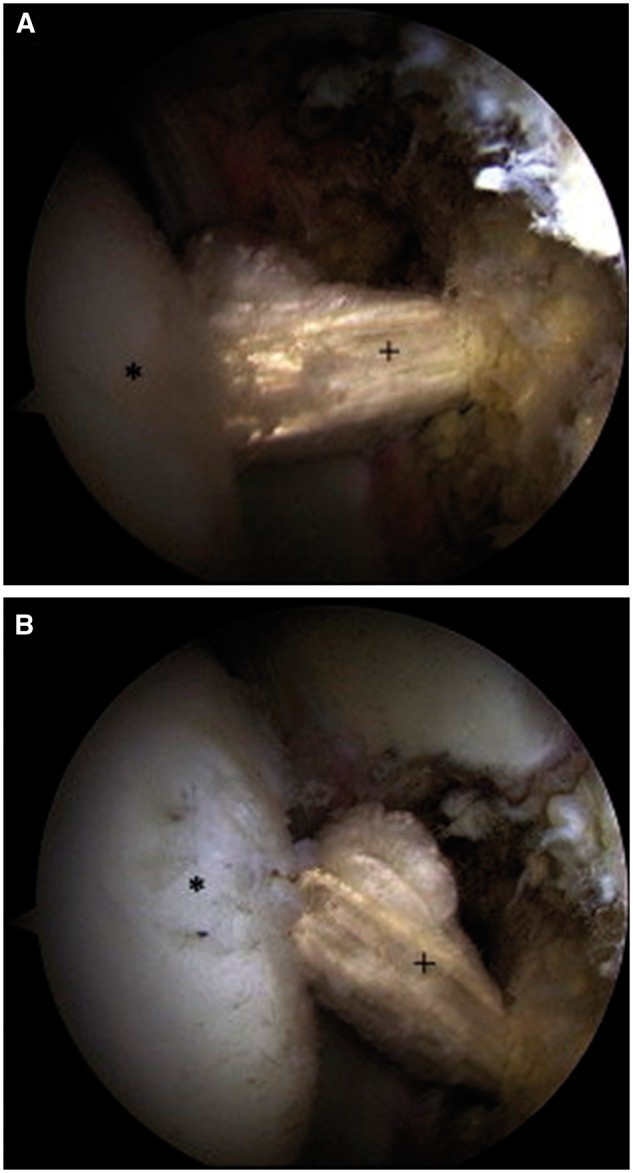
All hip arthroscopies were performed under general anesthesia in the supine position using a traction table and well-padded perineal post. All patients had muscle relaxant administered at the induction of anesthesia. Intra-operative diagnoses and procedures performed in the central, peripheral and peritrochanteric compartments were recorded. Labral tears were classified according to the Seldes classification [36]. A Seldes type 1 tear was disruption at the labral chondral junction and a Seldes type 2 tear was an intra-substance tear. The clock-face method was used to document the size and the location of the labral tear [37]. This method measures labral tearing using the 12-o’clock position as the most superolateral portion of the acetabulum and the 6-o’clock position as the transverse ligament. Disruption at the acetabular labral–chondral junction was described according to the acetabular labral articular disruption grading (ALAD) [14]. Chondral defects of the acetabulum and femur were graded according to the Outerbridge classification [38]. Any additional pathology in the joint was addressed before LT reconstruction. Bony pathology was corrected under fluoroscopic guidance. Acetabuloplasty was performed for pincer impingement, and a femoral osteoplasty was performed for cam impingement [39]. Full thickness articular cartilage damage was treated with debridement to create stable borders. Labral tears were treated with debridement or refixation. The decision on whether to debride or refixate the labrum in the setting of a labral tear depended on the stability of the labrum. Stable tears were debrided, whereas detached tears underwent repair. An iliopsoas fractional lengthening was performed by extending the medial capsulotomy and dividing the tendon at the level of the pelvic brim. The capsule was plicated using three or more stitches to create an inferior shift and imbrication in patients with generalized ligamentous laxity. The LT was examined and probed upon identification of a complete tear (Fig. 1) and classified as in Table I; the stump in the acetabular fossa was cleared with the Nav X ablation device (Arthrex, Naples, FL) and a shaver (Fig. 2).
Fig. 1.
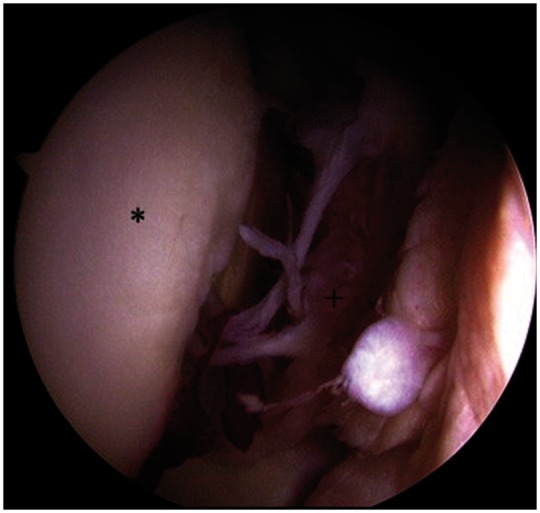
Intra-operative complete tear of the LT.
Table I.
LT classification
| Type | Domb (%) | Villar |
|---|---|---|
| 0 | 0 | No tear |
| 1 | 0–50 | Complete rupture |
| 2 | 50–100 | Partial tear |
| 3 | 100 | Degenerative tear |
Fig. 2.
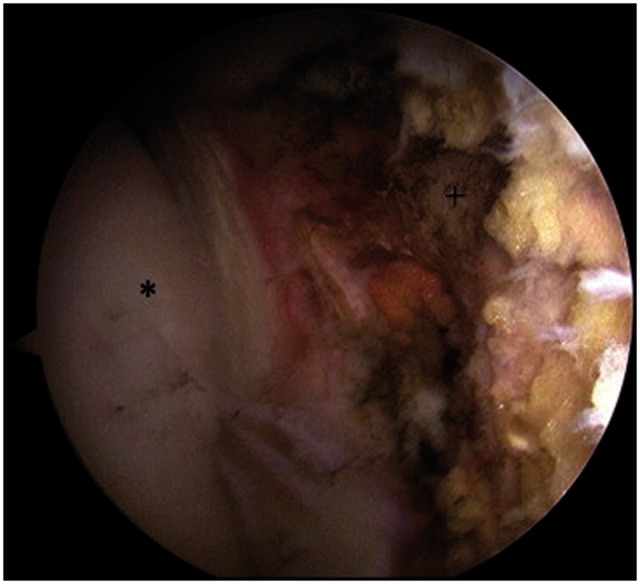
Appearance following debridement of the LT.
Graft preparation
The graft choice may include a semitendinosus autograft or allograft or a tibialis anterior allograft. All grafts were double-stranded and secured at each end with a whip stitch using No. 2 fiberwire (Arthrex). The graft was then secured to a 12 mm RetroButton (Arthrex) with a 3 mm loop. The graft is prepared before tunnel preparation. The choice of autograft or allograft was dependent upon whether patients had undergone a previous procedure in which ipsilateral autograft was used or patient personal preference. The graft was sized to determine acetabular and femoral tunnel and reamer sizes. Typically the graft sizes were 7 or 8 mm.
Femoral and acetabular tunnels
A lateral 2 cm incision is made to approach the femoral transtrochanteric tunnel; the location is determined by fluoroscopy (Fig. 3). A 3.2 mm guidewire (Arthrex, cannulated reaming instruments) is passed through the lateral cortex of the greater trochanter, exiting through the center of the fovea in the footprint of the LT. This is performed using a “free-hand” technique with fluoroscopic assistance and direct visualization of the guide's exit point in the fovea. Over the guidewire, a cannulated reamer (Arthrex) is used to create the femoral tunnel. Drilling of the acetabular tunnel is performed through the femoral tunnel, with the hip internally rotated and abducted to achieve correct tunnel positioning in the cotyloid fossa. The anatomic insertion of the LT in the cotyloid fossa is made in the inferior portion of the fossa. To maintain a safe distance from the obturator vessels, the tunnel is placed slightly posterior to the center of the base of the fossa. preoperatively, potential vascular complications specific to this procedure are discussed in detail with the patient. Fluoroscopic assistance is used to ensure that the guidewire is not penetrating into the pelvis, and the drilling is performed cautiously to avoid plunging through the medial cortex of the acetabular fossa [20]. The tunnel passes through the medial wall with the same diameter.
Fig. 3.

Fluroscopic guidance to determine tunnel placement for LT reconstruction.
Graft placement
Graft placement is performed by direct visualization and fluoroscopic assistance. Two knot-pushers are used to lead the graft–button complex through the tunnels; one knot-pusher is used to lead the button through the tunnel, and the second knot-pusher is used to flip the button over the medial cortex. Tunnel size did not have to be increased to accommodate passage of the knot pushers. Once the button has been flipped, tension is placed on the graft and fluoroscopy is used to ensure that the button has flipped and is secure.
The motion and the tension of the graft are examined in internal and external rotation while the hip is in traction (Fig. 4). The traction of the leg is then removed while traction is maintained on the graft. The leg is positioned in 10° of hyperextension and 60° of external rotation, and a polyetheretherketone interference screw (Arthrex) is used for femoral fixation. The excess graft is cut flush with the lateral cortex of the femur followed by standard wound closure. The patient undergoes placement of an X-Act ROM hip brace (DJO Global, Vista, CA) and abduction pillow.
Fig. 4.
Reconstructed LT with a semitendinosis graft.
Rehabilitation and recovery
For the first 6 weeks, the patient is kept in a hip brace locked at 0°–90° of flexion at all times and is restricted to 20 lbs of foot-flat weight bearing. In addition, an abduction pillow is used at night for the same period. The patient starts physical therapy on the first post-operative day and is instructed to refrain from adduction and external rotation. Six weeks post-operatively, the use of the brace and crutches at six weeks discontinued and the patient continues physical therapy with an emphasis on strengthening the gluteus medius and core muscles, as well as gradual progression of range of motion.
Outcome measures
Four hip specific outcome questionnaires were administered to patients pre- and post-operatively. These were the modified Harris Hip Score (mHHS), the non-arthritic hip score (NAHS) and the Hip Outcome Score—Sport-Specific Subscale (HOS—SSS). Patients were asked to estimate their pain on a visual analog scale (VAS) from 0 to 10, where 0 indicated no pain at all and 10 indicated the worse possible pain. These scores were recorded at the preoperative visit, at 3 months post-operatively and yearly thereafter. Patients rated their level of satisfaction after surgery on a scale of 0–10 with 10 being extremely satisfied and 0 being not satisfied at all. A satisfaction of 7 or more was considered a good/excellent result [40].
Statistical analysis
The patients’ pre and post-operative results were compared using a 2-tailed Student's t-test for comparison of continuous variables and Chi-square test to compare categorical variable. p-values of <0.05 were considered statistically significant. Statistical analysis was performed with Microsoft Office Excel 2007 (Microsoft, Redmond, WA). Intra-rater reliability of radiographic measurements was determined using Bartko’s method for measuring a rater’s self-consistency [41] and was found to be greater than 0.79 for all measurements.
RESULTS
Demographics
During the study period, 2,463 hip arthroscopies were performed, of which 167 had complete tears of the LT. There were 487 partial tears treated, of which 97 were treated with debridement. Six reconstruction procedures were performed in five patients. Four reconstruction procedures in three patients had minimum one year follow up. The demographic findings are shown in Table II. The mean age of the cohort was 32.7 years. There were two females and one male. The mean body mass index (BMI) was 22.2 kg/m2. Mean follow-up was 21.4 (range 16.4–24.3) months. The decision to reconstruct the LT in these patients was based on all patients reporting symptoms that the hip felt unstable on gait and activities of daily living with a concomitant diagnosis of Ehlers-Danlos syndrome and a prior history of operative stabilization of another joint.
Table II.
Demographics
| Patient | Age (years) | Sex | BMI (kg/m2) | Follow-up (months) |
|---|---|---|---|---|
| 1 | 22.6 | M | 25.9 | 24.3 |
| 2 | 21.3 | F | 22.2 | 27.8 |
| 3 | 43.5 | F | 20.4 | 17.3 |
| 4 | 43.7 | F | 20.4 | 16.4 |
| Average | 32.7 | — | 22.2 | 21.4 |
Physical examination
The mean range of motion was flexion of 115° and, at 90° of hip flexion, internal rotation of 22.5° and external rotation of 50° (Table III). Three out of four, 0/4 and 4/4 of procedures had a positive anterior, posterior and lateral impingement tests respectively. All procedures developed apprehension with extension and external rotation of the hip. All patients had Beighton's scores of greater than 6.
Table III.
Pre-operative clinical data
| Patient | Flexion | IR (at 90° of flexion) | ER (at 90° of flexion) | Anterior Impingement | Posterior Impingement | Lateral Impingement | Apprehension with extension and external rotation |
|---|---|---|---|---|---|---|---|
| 1 | 120 | 30 | 60 | Y | N | Y | Y |
| 2 | 120 | 40 | 50 | N | N | Y | Y |
| 3 | 100 | 10 | 45 | Y | N | Y | Y |
| 4 | 110 | 10 | 45 | Y | N | Y | Y |
| Average | 115 | 22.5 | 50 | — | — | — | — |
Imaging
Plain imaging findings
With respect to indices for dysplasia, the mean LCEA was 30°, ACEA was 38° and AI was 1.5°. In one procedure, the acetabular floor was medial to the ilioischial line (i.e. profunda). One procedure had a prominent ischial spine and two procedures had positive cross-over signs. The neck shaft angle in two procedures was above 137° and less than 116° in one patient with bilateral reconstructions who had previous varus osteotomies (Table IV).
Table IV.
Imaging findings
| Patient | LCEA | ACEA | AI | Profunda | IS | Crossover | Neck shaft angle | Alpha angle | MRI LT tear |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 27 | 36 | 5 | N | N | 30 | 138 | 92 | Full thickness |
| 2 | 30 | 39 | 0 | Y | Y | 10 | 137 | 66 | Full thickness |
| 3 | 32 | 39 | 0 | N | N | 0 | 116 | 56 | Full thickness |
| 4 | 31 | 38 | 0 | N | N | 0 | 114 | 62 | Partially torn/frayed |
| Average | 30 | 38 | 1.25 | 10 | 126.5 | 69 |
MRI findings
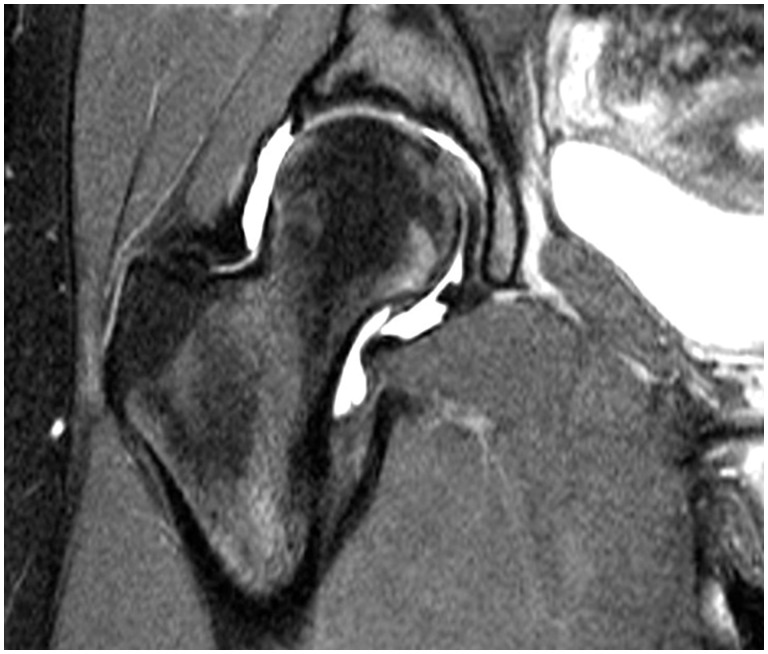
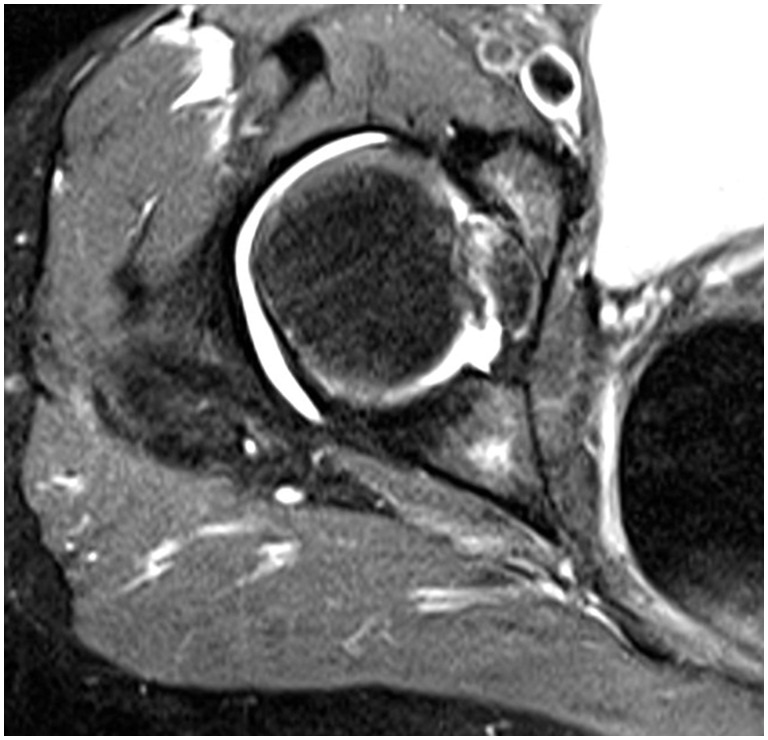
Three procedures had full thickness tears of the LT on MRI and one procedure was considered to have partial. Fig. 5 shows the MRI findings of an intact LT with ligamentous connection between the fovea capitis and acetabular floor. Fig. 6 shows the findings of a partial or possible tear of the LT with increase signal within the ligament on T2 weighted imaging and bony edema within the region of the fovea capitis.
Fig. 5.
Appearance of an intact LT on MRI.
Fig. 6.
Appearance of a tear of LT on MRI.
Intra-operative findings and concomitant procedures
Intraoperative findings and concomitant procedures are shown in Tables V and VI. Three out of four and 1/4 of procedures had an ALAD defect of grade 1 and 3, respectively. The size of the ALAD defects ranged from 1 to 1.5 cm2. LT tears were graded as a Domb 3 and Villar 1 in 3/4 of procedures and as a Domb 2 and Villar 2 in 1/4 of procedures. Two procedures had a LT reconstruction using semitendinosis autograft and two procedures’ patients had tibialis anterior allografts.
Table V.
Intra-operative findings
| Patient | Seldes tear | Location of tear | Size of tear | ALAD type | ALAD size (cm2) | Femoral outerbridge | Outerbridge size (cm2) | LT tear domb | LT tear villar |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 13.5–14.5 | 1 h | 1-Softening | 1 | 0 | — | 3 | 1 |
| 2 | — | — | — | 1-Softening | 1.5 | 0 | — | 3 | 1 |
| 3 | — | — | — | 3-Fissuring | 1 | 0 | — | 3 | 1 |
| 4 | 1&2 | 12.0–15.0 | 3 h | 1-Softening | 1 | 0 | — | 2 | 2 |
Table VI.
Concomitant procedures
| Patient | Labral treatment | Capsular treatment | Cartilage | Iliopsoas |
|---|---|---|---|---|
| 1 | Repair | Plication | None | None |
| 2 | None | Plication | None | None |
| 3 | None | Plication | None | None |
| 4 | Repair | Plication | None | None |
Patient reported outcomes
Apart from one procedure not competing a HOS—SSS score, all procedures had pre-operative and postoperative PRO outcomes scores recorded (Table VII). The average preoperative score for mHHS, NAHS and HOS—SSS were 42.6, 44.1, and 25.8 respectively. In three out of the four procedures, there was an improvement in all PROs except VAS, which worsened by two points in one procedure. For the other procedure, there was a worsening of all PROs.
Table VII.
Outcomes
| Pre-Operative | Follow Up | Delta | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Follo-up (months) | mHHS | HOS-SSS | NAHS | VAS | mHHS | HOS-SSS | NAHS | VAS | Satisfaction | Time | mHHS | HOS-SSS | NAHS | VAS |
| 1 | 24.3 | 21 | NA | 54 | 10 | 64 | NA | 56.25 | 3 | 10 | 24.03 | 43 | NA | 2.25 | −7 |
| 2 | 27.8 | 70 | 42 | 71 | 1 | 77 | 44.44 | 80 | 3 | 8 | 24.15 | 7 | 2.44 | 9 | 2 |
| 3 | 16.4 | 36.26 | 3.125 | 27.5 | 8 | 90.1 | 34.38 | 50 | 0 | 10 | 12.64 | 53.84 | 31.255 | 22.5 | −8 |
| 4 | 17.3 | 43 | 38 | 24 | 10 | 38.46 | 25 | 25 | 10 | 0 | 13.85 | −4.54 | −13 | 1 | 0 |
| Average | 21.5 | 42.6 | 20.8 | 44.1 | 7.3 | 63.4 | 25.9 | 52.8 | 4 | 7 | 18.7 | 24.8 | 5.1 | 8.7 | −3.3 |
DISCUSSION
The purpose of this study was to report on the results of four LT reconstructions in three patients. Two of the patients were female. All patients had a positive lateral impingement sign. There was no pattern of radiological findings with respect to acetabular coverage, version and depth. Excluding the patient that had previous varus femoral osteotomies, the remaining two patients had a valgus neck shaft angle. Intra-operatively, there was no association between LT tears and labral and chondral pathology grade. Capsular plication was concomitantly performed in all patients. With respect to PROs, three out of four procedures demonstrated an improvement in all four PROs, except for one procedure that had a worsened VAS. In one patient, there was a decline in PRO scores and that patient subsequently underwent revision reconstruction.
A recent review of management of LT tears concluded that efforts needed to be concentrated on refining the physical examination and imaging criteria for better detection preoperatively [17]. In our cohort of four patients, there was a wide variation in hip range of motion and presence of impingement signs with the exception of lateral impingement. The recently reported LT test, with a sensitivity and specificity of 90% and 85%, respectively, may help in clinical assessment [42]. In 3/4 of patients, a definite tear of the LT was detected on MRI. Bryd and Jones [15] reported a low sensitivity for radiological detection of LT pathology. They reported that only two diagnoses were made among 37 patients who underwent MR arthrogram, computed tomography or bone scanning for LT pathologic conditions.
In three out of four procedures, there was a definite improvement in PROs. A patient who had bilateral reconstructions had a poor outcome on her right side. This patient was a 43-year-old female who presented with bilateral hip pain and instability for 3 months. She had been diagnosed with hyper-mobility secondary to Ehlers–Danlos Syndrome and had bilateral femoral osteotomies at the age of 15 to reduce anterior instability caused by excessive femoral anteversion. She had a reduction in her mHHS and HOS-SSS as well as maintenance of her VAS score of 10 on the right. Conversely, her left hip had an excellent outcome with a 53 point improvement in her mHHS and a 0 VAS score at 1 year follow-up. No obvious cause for the discrepancy was found but the patient subsequently underwent a right revision reconstruction and open capsular reconstruction for recurrent posterior instability for which the 3-month follow-up results are pending. The remaining patients all had an improvement in PROs with satisfaction ranging between 7 and 10.
There are three studies that have reported on the results of LT reconstruction [20, 26, 27]. Two of the studies are case reports and one study is a case series of four patients. Grafts used in these studies include a synthetic knee medial collateral ligament; a double-stranded semitendinosus autograft and an iliotibial band tendon autograft. Philippon et al. [26] had a 2-year follow-up in two out of four patients in which one did not have preoperative scores and other patient had an improvement of mHHS of 7 points at 2 years and 21 points at 3 years. Amenabar et al. [27] published a case report in which at 12 months, the patient’s mHHS and NAHS improved by 47 and 22 points, respectively. These reports are in concordance with our results.
One strength of this study was that it has the largest number of patients with minimum 1-year follow-up. Furthermore, the study incorporated three PROs as it has been reported that no single PRO provides a comprehensive assessment post hip arthroscopy [43]. The clinical relevance of the present study’s findings is that in patients with hip instability with a background of ligamentous laxity and multi-joint instability due to a connective disorder, LT reconstruction associated with other soft tissue stabilization is associated with improved outcomes.
LIMITATIONS
The study had limitations. Despite having the largest number of cases of LT reconstructions, the number of patients in the case series was small, limiting the statistical significance of findings. Specific clinical tests for LT pathology were not included because tests had not been validated or published at the time of assessment. There was no control arm and, therefore, it is difficult to know to what extent LT reconstruction caused an improvement in PROs in the setting of other concomitant procedures. In addition, there has been no mechanical testing to determine the acetabular graft contact area with this reconstruction technique or whether the graft bonds with the tunnel wall or remains suspended from the retrobutton. Furthermore, all patients did not undergo follow-up MRI imaging to determine the integrity of the reconstruction. Finally, graft choice, particularly autologous graft, may have potentially been an issue in this patient population with a background history of abnormal collagen. However, in the patient population with hip instability due to an underlying connective tissue abnormality, this study demonstrates that LT reconstruction with concomitant labral treatments and capsular plication improved symptoms. The study adds to the body of knowledge on the evolving indications of LT reconstruction allowing future research to compare reconstruction techniques including methods of fixation.
FUNDING
This work was supported by the American Hip Institute, which receives general research support from Arthrex, Stryker, Breg, ATI, and Pacira. No funding was received directly for this work.
CONFLICT OF INTEREST STATEMENT
The senior author is a board member at the American Hip Institute and AANA Learning Center Committee; a paid consultant for Arthrex, Pacira, Stryker, and Amplitude; and receives royalties from Arthrex, Orthomerica, and DJO Global.
REFERENCES
- 1. Homma Y, Baba T, Kobayashi H, Murphy CG, Kaneko K. The importance of the soft tissue stabilizers of the hip: Three cases of rapid onset osteoarthritis following hip arthroscopy. J Orthopaed Sci: Off J Jpn Orthopaed Assoc 2015Dec 20. pii: S0949-2658(15)00105-0. [DOI] [PubMed] [Google Scholar]
- 2. Crawford MJ, Dy CJ, Alexander JW. et al. The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthopaed Relat Res 2007; 465:16–22. [DOI] [PubMed] [Google Scholar]
- 3. Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech 2003; 36:171–8. [DOI] [PubMed] [Google Scholar]
- 4. Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2009; 25:400–4. [DOI] [PubMed] [Google Scholar]
- 5. Mei-Dan O, McConkey MO, Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2012; 28:440–5. [DOI] [PubMed] [Google Scholar]
- 6. Ranawat AS, McClincy M, Sekiya JK. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. A case report. J Bone Joint Surg Am Vol 2009; 91:192–7. [DOI] [PubMed] [Google Scholar]
- 7. Sansone M, Ahlden M, Jonasson P. et al. Total dislocation of the hip joint after arthroscopy and ileopsoas tenotomy. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA 2013; 21:420–3. [DOI] [PubMed] [Google Scholar]
- 8. Bardakos NV, Villar RN. The ligamentum teres of the adult hip. J Bone Joint Surg Br Vol 2009; 91:8–15. [DOI] [PubMed] [Google Scholar]
- 9. Cerezal L, Kassarjian A, Canga A. et al. Anatomy, biomechanics, imaging, and management of ligamentum teres injuries. Radiograph: Rev Publ Radiol Soc N Amc 2010; 30:1637–51. [DOI] [PubMed] [Google Scholar]
- 10. Wenger D, Miyanji F, Mahar A, Oka R. The mechanical properties of the ligamentum teres: a pilot study to assess its potential for improving stability in children's hip surgery. J Pediatr Orthoped 2007; 27:408–10. [DOI] [PubMed] [Google Scholar]
- 11. O’Donnell JM, Pritchard M, Porthos Salas A. et al. The ligamentum teres—its increasing importance. J Hip Preserv Surg 2014; 0:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Martin RL, Palmer I, Martin HD. Ligamentum teres: a functional description and potential clinical relevance. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA 201220:1209–14. [DOI] [PubMed] [Google Scholar]
- 13. Kivlan BR, Richard Clemente F, Martin RL. et al. Function of the ligamentum teres during multi-planar movement of the hip joint. Knee Surgery, Sports Traumatol Arthrosc: Off J ESSKA 2013; 21:1664–8. [DOI] [PubMed] [Google Scholar]
- 14. Botser IB, Martin DE, Stout CE, Domb BG. Tears of the ligamentum teres: prevalence in hip arthroscopy using 2 classification systems. Am J Sports Med 2011; 39 (Suppl) :117S–25S. [DOI] [PubMed] [Google Scholar]
- 15. Byrd JW, Jones KS. Traumatic rupture of the ligamentum teres as a source of hip pain. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2004; 20:385–91. [DOI] [PubMed] [Google Scholar]
- 16. Haviv B, O'Donnell J. Arthroscopic debridement of the isolated Ligamentum Teres rupture. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA 2011; 19:1510–3. [DOI] [PubMed] [Google Scholar]
- 17. de SD, Phillips M, Philippon MJ, et al. Ligamentum teres injuries of the hip: a systematic review examining surgical indications, treatment options, and outcomes. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2014; 30:1634–41. [DOI] [PubMed] [Google Scholar]
- 18. Yamamoto Y, Usui I. Arthroscopic surgery for degenerative rupture of the ligamentum teres femoris. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2006; 22:689 e1–3. [DOI] [PubMed] [Google Scholar]
- 19. Amenabar T, O'Donnell J. Successful treatment of isolated, partial thickness ligamentum teres (LT) tears with debridement and capsulorrhaphy. Hip Int: J Clin Exp Res Hip Pathol Therapy 2013; 23:576–82. [DOI] [PubMed] [Google Scholar]
- 20. Simpson JM, Field RE, Villar RN. Arthroscopic reconstruction of the ligamentum teres. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2011; 27:436–41. [DOI] [PubMed] [Google Scholar]
- 21. Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2013; 29:162–73. [DOI] [PubMed] [Google Scholar]
- 22. Cerezal L, Arnaiz J, Canga A. et al. Emerging topics on the hip: ligamentum teres and hip microinstability. Eur J Radiol 2012; 81:3745–54. [DOI] [PubMed] [Google Scholar]
- 23. Domb BG, Martin DE, Botser IB. Risk factors for ligamentum teres tears. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2013; 29:64–73. [DOI] [PubMed] [Google Scholar]
- 24. van Arkel RJ, Amis AA, Cobb JP. et al. The capsular ligaments provide more hip rotational restraint than the acetabular labrum and the ligamentum teres: an experimental study. Bone Joint J 2015; 97-B:484–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hammarstedt JE, Redmond JM, Gupta A. et al. Arthroscopic ligamentum teres reconstruction of the hip in Ehlers–Danlos syndrome: a case study. Hip Int: J Clin Exp Res Hip Pathol Therapy 2015; 25:286–91. [DOI] [PubMed] [Google Scholar]
- 26. Philippon MJ, Pennock A, Gaskill TR. Arthroscopic reconstruction of the ligamentum teres: technique and early outcomes. J Bone Joint Surg Br Vol 2012; 94:1494–8. [DOI] [PubMed] [Google Scholar]
- 27. Amenabar T, O'Donnell J. Arthroscopic ligamentum teres reconstruction using semitendinosus tendon: surgical technique and an unusual outcome. Arthrosc Techn 2012; 1:e169–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Boykin RE, Anz AW, Bushnell BD. et al. Hip instability. J Am Acad Orthopaed Surg 2011; 19:340–9. [DOI] [PubMed] [Google Scholar]
- 29. Philippon MJ, Zehms CT, Briggs KK. et al. Hip instability in the athlete. Oper Techn Sports Med 2007; 15:189–94. [Google Scholar]
- 30. Byrd JW. Evaluation of the hip: history and physical examination. N Am J Sports Phys Therapy: NAJSPT 2007; 2:231–40. [PMC free article] [PubMed] [Google Scholar]
- 31. Smits-Engelsman B, Klerks M, Kirby A. Beighton score: a valid measure for generalized hypermobility in children. J Pediatr 2011; 158:119–23. 23 e1-4. [DOI] [PubMed] [Google Scholar]
- 32. Jessel RH, Zurakowski D, Zilkens C. et al. Radiographic and patient factors associated with pre-radiographic osteoarthritis in hip dysplasia. J Bone Joint Surg Am Vol 2009; 91:1120–9. [DOI] [PubMed] [Google Scholar]
- 33. Wiberg G. Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip. J Bone Joint Surg Am Vol 1953; 35-A:65–80. [PubMed] [Google Scholar]
- 34. Werner CM, Copeland CE, Ruckstuhl T. et al. Radiographic markers of acetabular retroversion: correlation of the cross-over sign, ischial spine sign and posterior wall sign. Acta Orthopaed Belg 2010; 76:166–73. [PubMed] [Google Scholar]
- 35. Barton C, Salineros MJ, Rakhra KS, Beaule PE. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthopaed Relat Res 2011; 469:464–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Seldes RM, Tan V, Hunt J., Jr. et al. Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthopaed Relat Res 2001; 382:232–40. [DOI] [PubMed] [Google Scholar]
- 37. Blankenbaker DG, De Smet AA, Keene JS. et al. Classification and localization of acetabular labral tears. Skelet Radiol 2007; 36:391–7. [DOI] [PubMed] [Google Scholar]
- 38. Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br Vol 1961; 43-B:752–7. [DOI] [PubMed] [Google Scholar]
- 39. Philippon MJ, Schenker ML. A new method for acetabular rim trimming and labral repair. Clin Sports Med 2006; 25:293–7. ix. [DOI] [PubMed] [Google Scholar]
- 40. Aprato A, Jayasekera N, Villar RN. Does the modified Harris hip score reflect patient satisfaction after hip arthroscopy? Am J Sports Med 2012; 40:2557–60. [DOI] [PubMed] [Google Scholar]
- 41. Bartko JJ. The intraclass correlation coefficient as a measure of reliability. Psychol Rep 1966; 19:3–11. [DOI] [PubMed] [Google Scholar]
- 42. O'Donnell J, Economopoulos K, Singh P. et al. The ligamentum teres test: a novel and effective test in diagnosing tears of the ligamentum teres. Am J Sports Med 2014; 42:138–43. [DOI] [PubMed] [Google Scholar]
- 43. Lodhia P, Slobogean GP, Noonan VK. et al. Patient-reported outcome instruments for femoroacetabular impingement and hip labral pathology: a systematic review of the clinimetric evidence. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2011; 27:279–86. [DOI] [PubMed] [Google Scholar]