Abstract
The purpose of this study is to demonstrate the assessment of intra-capsular femoral head and neck tumors, and to describe the arthroscopic surgical technique used to resect and fill the bone defects. Three cases of benign femoral head and neck lesions are presented. Two benign enchondromas and one benign osteochondroma were resected arthroscopically. Traction was used in one case. Modified Harris Hip Score improved in all three cases to scores of 95 or greater with an average improvement of 16 points with a minimum follow up of 15 months. Arthroscopic surgical resection of intra-capsular femoral hip lesions offers an effective alternative to open resection. This technique offered good outcomes in the limited cohort. We suggest that arthroscopic resection of intra-capsular femoral hip lesions be considered in relevant cases as an alternative to open resection.
INTRODUCTION
Benign bone tumors are relatively rare. These tumors can be classified as latent, active or aggressive [1]. Latent lesions are usually asymptomatic and are frequently encountered incidentally during evaluation of other complaints [2]. Active and aggressive lesions are most often symptomatic. Active lesions are often associated with isolated pain, and aggressive lesions may cause progressive bone destruction [3]. Surgical treatment of these active or aggressive lesions may be warranted based on the extent of bone involved and the clinical symptoms associated with the pathology. Treatment options for these lesions are based on the lesion’s location, the aggressiveness of the tumor/lesion and the expected morbidity of the procedure.
Most benign bone lesions can be diagnosed by assessing the age of the patient, tumor location and the tumors appearance on imaging studies [2]. Chondroblastoma and infection are good examples of well-defined benign ‘end of bone’ lesions in the skeletally immature. In the adult population under the age of 40, giant cell tumors are the most common epiphyseal lesions. In addition to these true end-of-bone lesions a variety of lesions can occur in the meta-epiphyseal region of long bones. These meta-epiphyseal lesions include enchondromas, aneurysmal bone cysts and chondromyxoid fibromas amongst others.
Due to the location and complex anatomy of the hip joint, surgical treatment of benign active or aggressive bone tumors of the femoral head and neck pose a challenge for orthopedic surgeons. Surgical intra-lesional resection remains the mainstay of treatment in benign active and aggressive bone lesions. This technique involves fenestration of the involved bone and curettage of the tumor. The anterior, lateral, anterolateral or combined anterior and lateral approach has been used to resect femoral head and neck bone tumors [4]. However, surgical treatment of bone tumors proximal to the hip joint is often associated with injury to the peri-articular muscles, the joint capsule, articulating chondral surface and bone [4–6]. The sequela of these procedures may include infection, limited mobility, decreased hip stability, diminished range of motion, increased pain, secondary osteoarthritis, avascular necrosis and local recurrence depending on the specimen's pathology [4–6]. Furthermore, in some cases hip dislocation is necessary to access the lesion during open resection, and hip dislocation is associated with various sequelae in and of itself [7].
Arthroscopy has become an established technique to treat hip joint pathologies. In light of the afore-mentioned risks associated with open surgical intervention for benign bone lesions of the proximal femur (head and neck) arthroscopic tumor resection is a valid treatment option in selected cases of benign bone lesions of the femoral head and neck [8]. The purpose of this study is to demonstrate the assessment of intra-capsular femoral head and neck tumors, and to describe the arthroscopic surgical technique used to resect and fill the bone defects.
CASES
Case 1
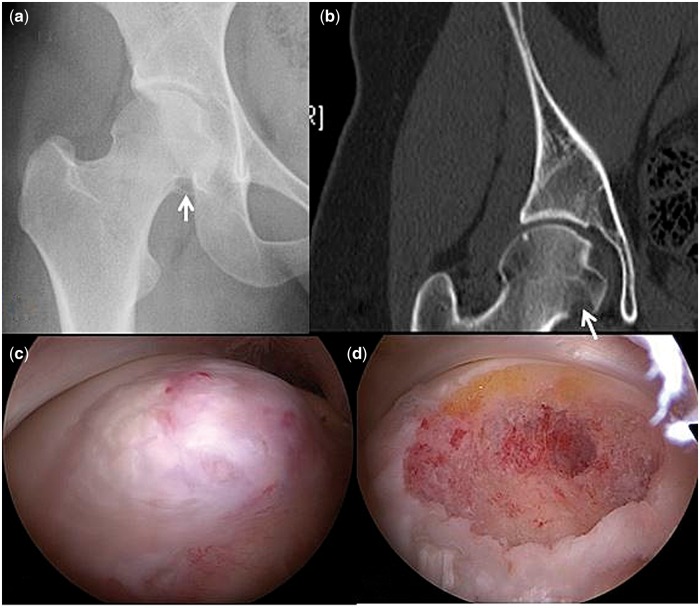
A 29-year-old healthy female presented to the musculoskeletal oncology department with increasing right-hip pain for the past 8 years. The patient was working as a bar manager and described increasing pain that was interfering with activities of daily living and sports. Physical examination showed a normal gait pattern. The patient exhibited full range of hip motion with pain on flexion adduction internal rotation (FADDIR), and tenderness on palpation of the anterior aspect of the groin. AP pelvis radiographs demonstrated a radiolucent lesion at the inferior margin of the right femoral head confirmed by computed tomography (Fig. 1A and B). Magnetic Resonance Imaging (MRI) showed a subcortical lesion within the inferior margins of the right femoral head, sized at 14 × 20 × 14 mm with a lobular appearance without cortical breaching or edema.
Fig. 1.
(A) AP pelvis radiograph. The radiolucent lesion is denoted with an arrow in the inferior margin of the right femoral head. (B) Computed tomography. The lesion is denoted with an arrow. (C) A large lesion in the medial aspect of the femoral head was demonstrated with arthroscopic visualization. (D) Resection of the lesion.
Due to continued pain and limitations of activity, it was recommended that the patient proceed with arthroscopic resection. Surgery was performed without traction. The proximal anterolateral portal was first established for the visualization of the peripheral compartment. A large lesion in the medial aspect of the femoral head was demonstrated (Fig. 1C). A distal anterolateral portal was then established under direct visualization penetrating the capsule medial to the viewing portal. Capsulotomy between the two entry points was performed with a hooked radiofrequency probe (VAPR; DePuy Mitek, Raynham, MA, USA) to facilitate instrument maneuverability. Curette, shaver and burr were used to facilitate complete tumor resection (Fig. 1D). The capsule was repaired using absorbable sutures. The pathology report confirmed benign enchondroma. At 15 months post-operatively the patients Modified Harris Hip Score (MHHS) and VAS scores had improved from 84 and 5 pre-operatively to 100 and 0 post-operatively. The patient was also able to return to jogging and Pilates post-operatively without pain.
Case 2
A 39-year-old female presented with 3 years of progressive left hip and groin pain with limitations to her activities of daily living. The pain was exacerbated by positional changes (standing from a seated position), walking and accompanied by a clicking sensation around the hip joint. On physical examination, the patient walked with a mild-antalgic gate. Tenderness was elicited upon palpation of the left groin. The patient exhibited full range of motion both passively and actively. AP pelvis radiographs and a CT scan revealed a triangular bony protuberance emanating from the medial aspect of the femoral neck proximal to the left lesser trochanter (Fig. 2A).
Fig. 2.
(A) AP pelvis radiograph. The triangular bony protuberance emanating from the medial aspect of the femoral neck proximal to the left lesser trochanter is denoted with an arrow. (B) Figure-of-4-position was utilized intra-operatively to bring the medially located lesion into an anterior position and to relive tension of the iliopsoas tendon. (C) Intra-operative arthroscopic view of the lesion demonstrating the proximity of the bony protuberance and the iliopsoas tendon (IPT). (D) Post-excision arthroscopic visualization of the lesion and the IPT. (E) AP pelvis radiograph. Confirmation of removal of the bony protuberance ensured with radiography.
The patient underwent arthroscopic excision of the lesion. Due to the peripheral location of the tumor traction was not applied and no distal fixation of the limb was used during the procedure. The entire limb was prepped and draped to allow unrestrained motion of the hip during the surgery. A proximal anterolateral portal was established for the direct visualization of the lesion. The leg was then mobilized into the figure-of-4-position, in order to bring the medially located lesion into an anterior position and to relieve tension of the Iliopsoas tendon (Fig. 2B). The distal anterolateral working portal was established under direct visualization. The acetabular labrum and the femoral head–neck junction appeared to be intact. A bony prominence proximal to the lesser trochanter was detected with associated signs of irritation and impingement on the iliopsoas tendon. The tumor was excised using curved osteotome, burr and shaver (Fig. 2C–E postop radiograph). The pathology report confirmed benign osteochondroma. Post-operatively, the patient complained of anterolateral numbness in the distribution of the lateral femoral cutaneous nerve, which resolved completely by 3 months. The patient was able to return to full activity without limitation in motion or pain on activity. The pre-operative MHHS improved from 85 to 96 at 24 months post-operatively.
Case 3
A healthy 20-year-old male presented to the musculoskeletal oncology department after incidental diagnosis of a cystic lesion located in the left femoral head (Fig. 3A). The lesion was found incidentally after the patient underwent an MRI of the lower abdomen for suspected appendicitis. Six months after the incidental finding the patient began to complain of left groin pain.
Fig. 3.
(A) AP pelvis radiograph. A cystic lesion was demonstrated on radiograph in the left femoral head. (B) CT scan demonstrated a lobular lesion in the epiphyseal region of the femoral head sparing the articular surface. (C) Intra-operative arthroscopic visualization of the femoral head. The femoral head was probed and appeared to be intact. (D) Intra-operative fluoroscopic assistance was used to identify the location of the lesion. (E) Intra-operative arthroscopic visualization of the cavity after resection using a curette and shaver to the underlying bed of bleeding bone. (F) Bone substitute was used to fill the cavity left after lesion excision.
The patient had hip pain with flexion abduction and external rotation and a negative FADDIR test. CT scan demonstrated a lobular lesion in the epiphyseal region of the femoral head sparing the articular surface (Fig. 3B). The lesion measured 2.3 × 15 × 1.6 cm. Due to continued symptoms and the subchondral location at the weight bearing zone of the femoral head, hip arthroscopy including biopsy samples, debridement and curettage was suggested. Due to the size and location of the lesion bone substitute was used to fill the cavity.
Hip arthroscopy was first performed with traction for evaluation of possible articular penetration of the lesion. A lateral portal was established under fluoroscopy and then a mid-anterior portal [9] was created under arthroscopic visualization with the aid of fluoroscopic guidance. Capsulotomy between the two entry points was performed with a hooked radiofrequency probe (VAPR; DePuy Mitek, Raynham, MA, USA) to facilitate instrument maneuverability. The femoral head was probed and appeared to be intact (Fig. 3C). Traction was then released and the peripheral compartment was inspected. The location of the lesion was identified using fluoroscopy (Fig. 3D). The capsule was further divided in a T shape. A small window on the lateral cortex of the femoral head was created. The lesion was excised using a curette and a shaver to the underlying bleeding bed of bone (Fig. 3E). The cavity was than filled with an osteo-conductive (HA) Bone Paste (BoneSource BVF, Stryker, Mahwah, NJ, USA) (Fig. 3F). The capsule was closed at the end of the procedure and the pathology report confirmed benign enchondroma. Post-operative radiographs at 18 months after surgery showed marked increased density of the femoral head (Fig. 4A and B). The patients MHHS and Visual Analogue Scale score were improved from 74 and 6 pre-operatively to 95 and 0 post-operatively with 30 months follow up.
Fig. 4.
Post-operative radiographs at 18 months following surgery showed marked increased density of the femoral head.
DISCUSSION
The principal outcome of this study reports good clinical outcomes and minimal tissue morbidity in three cases of arthroscopic benign femoral head and neck tumor resection. The all-arthroscopic technique allows for adequate tumor resection using a minimally invasive technique with theoretical enhanced safety, decreased complications and reduced sequela when compared with open resection for femoral head and neck tumors [8].
The arthroscopic techniques used for the resection of intra-capsular lesions in these cases are known techniques reapplied to a novel setting. Portal establishment, instrumentation and decompression techniques are similar to those previously described in arthroscopic surgery for femoral acetabular impingement (FAI). However, in each of the described cases surgery was planned ‘a la cart’. Traction was not applied in two cases. In one case distal fixation was not used to allow free manipulation of the hip. In one hip traction was applied for inspection and palpation of the cartilage. A combination of arthroscopic shaver, curette and burr was used to resect the lesions to clear margins. Following resection of small lesions filling of the defect was not necessary. However, in the case of larger bony defects, bone substitute may be applied in the same fashion as previously described by Jamali et al. [10] in hip arthroscopy for FAI caused by bone cysts.
Arthroscopic procedures provide shortened rehabilitation time when compared with open procedures [11]. Furthermore, arthroscopic procedures may reduce complication rates and the possible sequela associated with open hip surgery [12]. A major complication of open hip procedures, especially with dislocation, is decreased hip stability and lengthened rehabilitation period [12, 13]. Joint dislocation is known to jeopardize hip stability [12, 13]; however, open resection also applies an insult to the capsule that decreases hip stability [12, 13]. Arthroscopic resection offers a minimally invasive technique to resect intra-capsular lesions, especially in the femoral head and neck, without the drawbacks of open resection.
Leal et al. [14] describes a case of arthroscopic enchondroma resection. In that case, the author uses similar techniques and quotes the ease of operation. Furthermore, in the case of a large bony defect, greater than one-third the width of the femoral neck, screws can be placed under fluoroscopy to stabilize the intra-capsular femur.
In cases of benign femoral head and neck tumors in young patients the clinical decision to resect intra-capsular lesions is often difficult. Although the patient may be experiencing significant pain the sequela of open hip surgery may outweigh the benefits of tumor resection. Arthroscopic resection allows for an alternative surgical intervention not associated with the limitations and complications of an open resection. In the cases reported in this study the tumor was focal and only two portals were necessary to facilitate the resection with minimal capsulotomy and damage to bone. Arthroscopic resections of tumors located peripherally can be performed without traction, which facilitates instrument maneuverability [13]. Additionally, a relatively small capsular window is used and stability is not a major concern during the rehabilitation process. Therefore, patients are able to bear weight immediately post-operatively and undergo an expedited rehabilitation protocol. Despite the advantages of less invasive tumor resection techniques certain disadvantages and risks must be considered. In the case of an aggressive, malignant or infectious lesion an arthroscopic approach would broach the lesion. This could possibly facilitate spread of the aggressive, malignant or infectious lesion via fluid ingress/egress used in arthroscopy. High suspicion of a benign lesion must be established via workup and imaging before arthroscopic resection is considered.
Limitation
The limitations of this study are the small number of patients and the lack of a control group. Furthermore, only benign tumors were resected and the results cannot be generalized to other lesions. Bony stability was a concern in only one patient.
CONCLUSION
Arthroscopic surgical resection of intra-capsular femoral hip lesions offers an effective alternative to open resection. This technique offered good outcomes in the limited cohort. We suggest that arthroscopic resection of intra-capsular femoral hip lesions be considered in relevant cases as an alternative to open resection.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. 1980. Clin Orthop Relat Res 2003; 4–18. [DOI] [PubMed] [Google Scholar]
- 2. Yildiz C, Erler K, Atesalp AS, Basbozkurt M. Benign bone tumors in children. Curr Opin Pediatr 2003; 15:58–67. [DOI] [PubMed] [Google Scholar]
- 3. Wyers MR. Evaluation of pediatric bone lesions. Pediatr Radiol 2010; 40:468–73. [DOI] [PubMed] [Google Scholar]
- 4. Hu YC, Lun DX, Zhao SK. Combined anterior and lateral approaches for bone tumors of the femoral neck and head. Orthopedics 2012; 35:e628–34. [DOI] [PubMed] [Google Scholar]
- 5. Strong DP, Grimer RJ, Carter SR. et al. Chondroblastoma of the femoral head: management and outcome. Int Orthop 2010; 34:413–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cho HS, Park IH, Han I. et al. Giant cell tumor of the femoral head and neck: result of intralesional curettage. Arch Orthop Trauma Surg 2010; 130:1329–33. [DOI] [PubMed] [Google Scholar]
- 7. Ganz R, Gill TJ, Gautier E. et al. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 2001; 83:1119–24. [DOI] [PubMed] [Google Scholar]
- 8. Torres-Eguia RJ, Colmenero Rolon CA, Arauz De Robles S. et al. Epiphyseal femoral tumour resection under intraosseous endoscopic control. Hip Int 2010; 20(Suppl 7):S32–5. [DOI] [PubMed] [Google Scholar]
- 9. Kelly BT, Weiland DE, Schenker ML. et al. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy 2005; 21:1496–504. [DOI] [PubMed] [Google Scholar]
- 10. Jamali AA, Fritz AT, Reddy D. et al. Minimally invasive bone grafting of cysts of the femoral head and acetabulum in femoroacetabular impingement: arthroscopic technique and case presentation. Arthroscopy 2010; 26:279–85. [DOI] [PubMed] [Google Scholar]
- 11. Villar RN. Hip arthroscopy. Br J Hosp Med 1992; 47:763–6. [PubMed] [Google Scholar]
- 12. Harris JD, Larson CM, Nho SJ. Complications with Hip Arthroscopy Hip arthroscopy complications See Complications and Open Hip Surgery In: Nho S.et al. (eds) Hip Arthroscopy and Hip Joint Preservation Surgery, 2013. : New York, NY: Springe, pp. 1–17. [Google Scholar]
- 13. Dienst M, Gödde S, Seil R. et al. Hip arthroscopy without traction: in vivo anatomy of the peripheral hip joint cavity. Arthroscopy 2001; 17:924–31. [DOI] [PubMed] [Google Scholar]
- 14. Leal F, Nellensteijn JM, Frada R. et al. Arthroscopic treatment for femoral neck enchondroma: case report. J Hip Preserv Surg 2015; 2(4):428–30. [DOI] [PMC free article] [PubMed] [Google Scholar]