Abstract
The objective of this study is to retrospectively examine the effects of pre-operative fascia iliaca (FI) and lumbar plexus (LPB) nerve blocks on post-operative pain and secondary post-operative variables following arthroscopic surgery of the hip. Subjects undergoing arthroscopic surgery of the hip received one of three pre-operative anesthetic techniques; general anesthesia only, general anesthesia with FI or general anesthesia with LPB. Patient reported pain scores (0–10) were recorded at 0, 30, 60, 90 and 120 min after admission to the post-anesthesia care unit (PACU). Secondary variables examined include time spent in the PACU, morphine equivalent administered, presence of nausea, persistent numbness, parasthesia, weakness, increased narcotic usage for rebound pain, ED visits and hospital admissions. The mean pain scores over all time points were significantly lower in the LPB group (2.38) than the FI group (4.08, P < 0.001) and the Gen group (3.55, P < 0.001). Patients receiving a lumbar plexus block exhibited significantly decreased pain at t = 0 (P = 0.019), t = 30 (P = 0.038), t = 60 (P = 0.013), t = 90 (P = 0.017) and t = 120 (P = 0.001) after admission to PACU. The FI group showed no improvement in any post-operative variable when compared with general anesthesia alone. There was no difference in the time to discharge or in morphine equivalent administered between groups. One patient receiving a lumbar plexus block experienced a seizure lasting about 10 s. However, there were no medium or long-term complications. Lumbar plexus block administered in concert with general anesthesia provides clinically important and statistically significant post-operative pain relief when compared with general anesthesia alone or general anesthesia plus fascia iliaca block.
INTRODUCTION
Despite the significant rise in the numbers of hip arthroscopies performed annually [1, 2], there is a relative paucity of reports regarding optimal anesthesia for these procedures. Considerations specific to hip arthroscopy include control of intra-operative pain, adequate muscle relaxation to allow for distraction for work in the central compartment and post-operative pain management. General anesthesia and spinal anesthesia with or without epidural are commonly employed to achieve these goals.
The hip is innervated predominately by branches of the lumbar plexus: the femoral nerve, obturator nerve and the lateral femoral cutaneous nerve; as well as the sacral plexus via the nerve to the quadratus femoris, and at times, directly via the sciatic nerve [3]. Cutaneous innervation of the lateral thigh where the most commonly employed portals for hip arthroscopy are located is provided by the lateral femoral cutaneous nerve [4].
The fascia iliaca block anesthetizes both the femoral and the lateral femoral cutaneous nerves and can be performed under ultrasound guidance [5]. Krych et al. reported that pre-operative fascia iliaca block was safe and effective when combined with multimodal anesthesia for hip arthroscopy in a series of 30 patients [6]. Administration of a fascia iliaca compartment block has been reported to reduce pain in patients undergoing surgery for fractures of the femoral shaft [7] and hip fracture patients in the Emergency Department [8].
The lumbar plexus block has also demonstrated efficacy in pain management and decreasing post-operative opioid use and associated side effects in hip arthroplasties [9–11]. While the fascia iliaca block relies on diffusion of anesthetic under the iliacus fascia to anesthetize the femoral and lateral femoral cutaneous nerves, the lumbar plexus block targets these nerves and the obturator nerve at their origins [11, 12]. Local anesthesia at the origin of the lumbar plexus has been shown to be effective not only in enhancing intra-operative and post-operative analgesia but also in improving relaxation and immobility of the lower extremity in hip arthroplasties, fracture repair and other hip and knee surgeries [9–11, 13].
We sought to identify the safety and the utility of pre-operative nerve blockade in conjunction with general anesthesia. We hypothesized that patients receiving a pre-operative fascia iliaca or lumbar plexus blockade in addition to general anesthesia would exhibit decreased post-operative pain scores, decreased opiate and anti-emetic consumption, and shorter time spent in the post-anesthesia care unit (PACU).
METHODS
Following institutional review board approval, a retrospective chart analysis was conducted on 145 consecutive hip arthroscopy patients. All surgeries were performed at a single outpatient facility between 27 September 2013 and 14 January 2015 by a board-certified orthopaedic surgeon and fellowship-trained hip arthroscopy specialist who has performed over 2000 arthroscopic surgeries of the hip. These procedures represent approximately one-third of the surgeon’s arthroscopic hip surgeries performed during this time period (and all of them consecutively at the facility where the study was performed). Nerve blocks were administered by one of three anesthesiologists on staff at the facility. The surgeon used anterolateral and mid-anterior portals. An additional distal anterolateral portal was utilized for labral reconstruction and gluteus medius/minimus repair procedures. The sole inclusion criterion was that each respective patient underwent an arthroscopic hip procedure under general anesthesia with or without a pre-operative fascia iliaca or lumbar plexus nerve block at the facility. Exclusion criteria included osteoarthritis of the hip and self or family-reported history of narcotics abuse. Consent was waived due to the retrospective, de-identified nature of this chart review.
Patients were asked to identify their pain level at various points in time using a 0–10 scale, with 10 being the worst pain imaginable. Pain scores were recorded prior to administration of anesthetic, then post-operatively at admission to the PACU (t = 0, t = 30, t = 60, t = 90 and t = 120 min), or until the patient was discharged. Total time spent in PACU was monitored and recorded for each patient, along with the identity and strength of any post-operative medication administered during the time spent in recovery. Nausea and the need for antiemetic medication were noted. The amount of opioid given to each patient in PACU was converted to a standard morphine equivalent using an equianalgesic conversion [14]. Patients were questioned at initial follow-up (3–5 d post-operatively) with regard to potential short-term complications of regional anesthesia, including numbness, paresthesia, weakness, rebound pain and incidence of falls. Medium and long-term complication screening was conducted at standard follow-up appointments at 2 weeks, 6 weeks, 3 months, 6 months and 12 months post-operatively.
The three groups were compared with respect to categorical data (sex, presence of nausea and procedure type) using the χ2 analysis. Continuous variable demographic data (age, height, weight and BMI) were compared using Independent-sample Student’s t-tests and single factor analysis of variance (ANOVA). Pain scores, morphine equivalent and time to discharge were assessed using Independent-sample Student’s t-tests and single-factor analysis of covariance (ANCOVA) to eliminate confounding effects of the covariate pre-operative pain. A P values < 0.05 was determined to be statistically significant.
Fascia iliaca block
All fascia iliaca nerve blocks were performed pre-operatively in the PACU under close monitoring using ultrasound guidance with the patient in the supine position. The ultrasound transducer was oriented in the transverse plane, close to the femoral crease and lateral to the femoral artery. Needle entry was performed at the lateral third of the distance from the anterior superior iliac spine and pubic tubercle. Local anesthetic was injected slowly under ultrasound guidance with repeated aspirations, allowing it to spread medial to lateral under the fascia iliaca but superficial to the iliacus muscle in order to anesthetize the femoral and lateral femoral cutaneous nerves. The local anesthetic used was 40 ml 0.375% ropivacaine with 4 mg of preservative-free dexamethasone.
Lumbar plexus block
All lumbar plexus blocks were performed pre-operatively in the PACU under close monitoring using anatomic landmarks, ultrasound guidance and a nerve stimulator. The patient was placed in the lateral decubitus position, operative hip up with a slight forward tilt. The iliac crest, spinous processes at the midline and posterior superior iliac spine were used as landmarks. The needle was inserted perpendicular to the skin at a point at the lateral one-third of a line that intersects the horizontal line passing through the spinous process and iliac crest, as well as the two perpendicular lines of the spinous process and posterior superior iliac spine. A nerve stimulator was then used to incite visible or palpable quadriceps muscle stimulation at 0.5–1.0 mA. Subsequently, 40 ml of 0.375% Ropivacaine with 4 mg of preservative-free dexamethasone was injected slowly with repeated aspirations. To prevent falls, patients undergoing lumbar plexus or fascia iliaca blocks were discharged with a knee immobilizer that they were instructed to wear until the block had completely worn off.
RESULTS
A total of 145 consecutive patients that underwent a hip arthroscopy procedure between 27 September 2013 and 14 January 2015 at the ambulatory surgical center were included in the study. No exclusions were made from the 145 consecutive eligible patients. The sample size requisite for determining significance was calculated via power analysis using data from a study by Xing et al. examining similar anesthetic manipulations on comparable populations [15]. The first 55 patients received general anesthesia alone (Gen), the subsequent 30 patients received an ultrasound-guided fascia iliaca regional block prior to general anesthesia (FI) and the following 60 patients received an ultrasound-guided lumbar plexus block prior to general anesthesia (LPB). Statistical analysis revealed similar demographics between the three cohorts (Table I, Supplementary data are available at Journal of Hip Preservation Surgery online). There was no significant disparity in pre-operative pain between groups [ANOVA: F(2,142)=0.276, P = 0.759] (Table II, Supplementary data are available at Journal of Hip Preservation Surgery online).
Table I.
Patient demographics
| Gen | Gen + FI | Gen + LPB | |
|---|---|---|---|
| (n=55) | (n=30) | (n=60) | |
| Sex, n | |||
| Male | 18 | 11 | 19 |
| Female | 37 | 19 | 41 |
| Age, mean ± SD | 34.51 ± 11.51 | 30.57 ± 13.51 | 35.45 ± 12.47 |
| Mean height (m) | 1.69 | 1.69 | 1.7 |
| Mean weight (kg) | 70.39 | 67.84 | 70.19 |
| Mean BMI (kg/m2) | 24.22 | 23.59 | 24.18 |
| Procedure type, n (%) | |||
| Femoral osteoplasty | 47 (85.5) | 21 (73.3) | 51 (86.7) |
| Acetabular osteoplasty | 23 (41.8) | 9 (30) | 23 (38.3) |
| No osteoplasty | 7 (12.7) | 8 (26.7) | 8 (13.3) |
| Labral repair | 33 (60) | 24 (80) | 30 (50) |
| Labral reconstruction | 18 (32.7) | 4 (13.3) | 22(36.7) |
| Labral debridement | 6 (10.9) | 2 (6.7) | 11 (18.3) |
| Glut min/med repair | 0 (0) | 1 (3.3) | 2 (3.3) |
Table II.
Pre-Operative and PACU Pain Scales
| Gen | Gen + FI | Gen + LPB | P values | F ratio | ||||
|---|---|---|---|---|---|---|---|---|
| Variable | µ ± Std Err | n | µ ± Std err | n | µ ± Std err | n | ||
| Pre-op pain | 2.36±0.35 | 55 | 2.73±0.44 | 30 | 2.63±0.3 | 60 | 0.759 | 0.276 |
| Pain in PACU | ||||||||
| t=0 | 3.25±0.45 | 55 | 4.12±0.72 | 30 | 2.03±0.39 | 60 | 0.019* | 4.081 |
| t=30 | 4.1±0.39 | 55 | 4.72±0.58 | 30 | 3.08±0.40 | 60 | 0.038* | 3.362 |
| t=60 | 3.62±0.33 | 54 | 4.08±0.48 | 30 | 2.57±0.29 | 60 | 0.013* | 4.455 |
| t=90 | 3.32±0.37 | 37 | 3.5±0.4 | 30 | 2.16±0.29 | 49 | 0.017* | 4.238 |
| t=120 | 3.08±0.49 | 18 | 3.85±0.74 | 13 | 1.57±0.38 | 28 | 0.001* | 7.498 |
*Statistically significant difference between the Gen + LPB group and both the Gen and Gen + FI group.
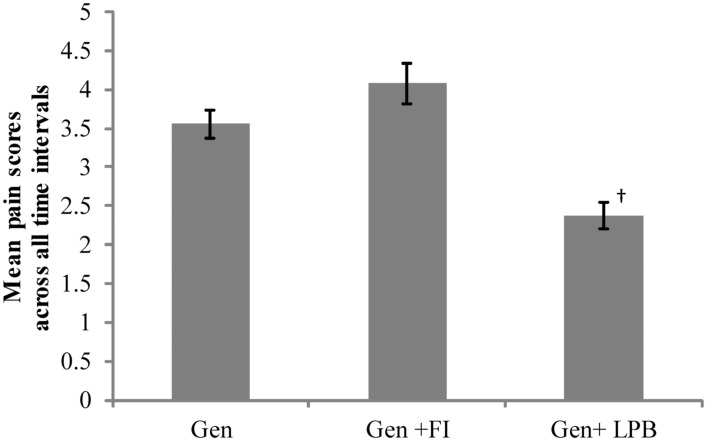
The mean post-operative pain scores across all time points were significantly lower in the LPB group (2.38) than the FI group (4.08, P < 0.001) and the Gen group (3.55, P < 0.001) (Fig. 1). The results of one-way ANCOVA controlling for pre-operative pain reveal that patients receiving a lumbar plexus block exhibited significantly decreased pain at each measured interval following arthroscopic surgery of the hip [t = 0 (P = 0.019), t = 30 (P = 0.038), t = 60 (P = 0.013), t = 90 (P = 0.017) and t = 120 (P = 0.001)] (Table II, Supplementary data are available at Journal of Hip Preservation Surgery online) (Fig. 2).
Fig. 1.
Patient-reported pain scores for each group averaged across all time intervals after admittance to PACU. Values are reported as the mean ± the standard error of the mean. Key: † denotes significance within 99% CI.
Fig. 2.
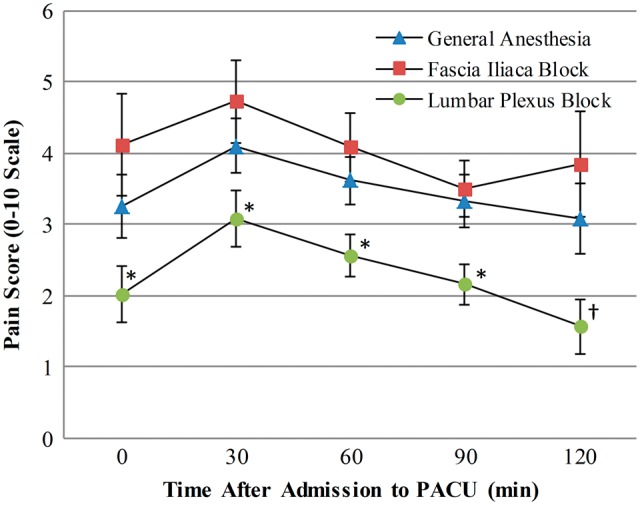
Patient-reported pain scores for each group reported at 0, 30, 60, 90 and 120 min from admittance to the post-anesthesia care unit (PACU). Values are reported as the mean ± the standard error of the mean. Key: * denotes significance within 95% CI; † denotes significance within 99% CI.
The lower pain scores among the lumbar plexus cohort did not translate into lower morphine equivalent dosing of opioids in the PACU [ANCOVA: F(2,138)=0.64, P = 0.53] (Table III). There was also no significant difference in time to discharge between groups [ANCOVA: F(2,138)=0.075, P = 0.928] (Table III). Nor did nausea requiring anti-emetics differ significantly among the groups [χ2(2)=3.67, P = 0.16] (Table III, Supplementary data are available at Journal of Hip Preservation Surgery online).
Table III.
Secondary Post-Operative Outcome Measures
| Variable | Gen | Gen + FI | Gen + LPB | P values |
|---|---|---|---|---|
| Morphine-equivalent dose in PACU, mg | 7.02 | 8.8 | 7.16 | 0.531 |
| Post-operative nausea, n (%) | 13 (24) | 4 (13) | 19 (32) | 0.16 |
| Time to discharge from PACU, min | 108.6 | 112.2 | 111.5 | 0.928 |
Complications
There were no complications in the general anesthesia or fascia iliaca block cohorts. In the lumbar plexus block cohort, there was a seizure of approximately 10 s duration in one patient. There were no other complications in any group. In none of the three groups, was there a long lasting complication from anesthesia; there was no reported incidence of persistent numbness, parasthesia, weakness or increased narcotic usage for rebound pain up to 1-year follow-up. There were no post-operative falls, Emergency Department visits or hospital admissions in any group.
DISCUSSION
Although optimal anesthesia for arthroscopic surgery of the hip has yet to be defined, recent studies examining regional anesthesia for these procedures exhibit promising preliminary results. We sought to assess the relative value of two regional blocks—the fascia iliaca block and the lumbar plexus block—compared with general anesthesia alone. The results of the current study indicate that for arthroscopic surgery of the hip a pre-operative lumbar plexus regional block performed in conjunction with general anesthesia provides significant and clinically meaningful decreases in post-operative pain reported in the PACU in an ambulatory surgical center setting. We found no benefit to pre-operative blockade of the femoral and lateral femoral cutaneous nerves alone as performed with a fascia iliaca block.
The significant decrease in pain scores in the lumbar plexus block is likely clinically meaningful; the mean difference in pain scores between the lumbar plexus block and the general and fascia iliaca block groups was 1.2 and 1.9, respectively. This exceeds the minimal clinically meaningful change of 0.9 in pain scores as proposed by Kelly and is on par or exceeds those proposed by Todd et al. [16, 17]. Importantly, these studies relate minimally significant changes for individuals, while those for group mean comparisons are generally smaller [18].
This relative benefit we found in our lumbar plexus block patients is likely attributable to the more complete and proximal nervous blockade afforded by the lumbar plexus block. In addition to the femoral nerve and the lateral femoral cutaneous nerve blockade garnered by a fascia iliaca block, the lumbar plexus block provides anesthesia to other nerves originating in the lumbar plexus. The most important of these is the obturator nerve, which carries sensory information from the hip joint, adductor muscles, medial femur and the skin in the medial aspect of the thigh [11]. It is also not uncommon for an accessory femoral nerve, originating at the lumbar plexus, to innervate the anterior hip capsule [3]. Neither of these nerves would be anesthetized by a femoral or fascia iliaca nerve block, but would be blocked by a lumbar plexus block.
The efficacy of regional anesthesia has been demonstrated in other surgeries about the hip including fixation of femoral fractures, hip fractures and hip arthroplasty [7, 8, 10, 13, 19–21]. In a randomized controlled trial of post-operative total hip arthroplasty patients comparing continuous femoral versus lumbar plexus nerve blockade, Marino et al. reported that the use of continuous lumbar plexus block was associated with significantly fewer opioid-related side effects, greater distances walked and enhanced patient satisfaction [10]. Yadeau et al. reported a statistically significant decrease of 0.9 on a 0–10 scale in post-operative pain following hip arthroscopy in patients receiving a lumbar plexus blockade in concert with spinal epidural anesthesia compared with spinal epidural anesthesia alone [22]. While this was a well-designed prospective randomized trial, it was done on patients who also received neuraxial (spinal epidural) anesthesia which can be challenging in an ambulatory surgical center setting due to costs associated with post-operative length of stay.
In a retrospective cohort study of hip arthroscopy patients similar to the current study, Dold et al. compared general anesthesia alone with pre-operative femoral nerve block plus general anesthesia. While they found that patients in the femoral nerve block group received significantly lower intra- and post-operative morphine-equivalent doses, the femoral nerve block patients’ post-operative pain scores were only lower at one of the five measured time points when compared with the general anesthesia alone group [23]. Ward et al. reported that patients with pain scores over seven receiving post-operative femoral nerve blocks exhibited decreased time to discharge, decreased nausea and increased patient satisfaction compared with patients who were given morphine alone [24]. Krych et al. reported that pre-operative fascia iliaca block was safe and effective when combined with multimodal anesthesia for hip arthroscopy in a series of 30 patients [6]. Xing et al. recently reported that hip arthroscopy patients who underwent a pre-operative femoral nerve block had significantly lower pain up to 6 h post-operatively. They did report that up to six patients in the femoral nerve block group reported falls in the first 24 h post-operatively [15].
These previous studies in hip arthroscopy patients point out that regional anesthesia addressing the femoral nerve in the pre- or post-operative setting is safe and can be modestly beneficial. While our study echoes or in some cases exceeds the safety data of the previous studies, the two most salient concerns are falls and intra-vascular administration leading to seizure or arrhythmia. While our findings do support a significant benefit in post-operative pain levels with pre-operative lumbar plexus block administration, regional anesthetic blocks are not without risk. The lumbar plexus block is considered an advanced nerve block technique, due to the location of the lumbar plexus roots deep in the psoas muscle and their proximity to the epidural space [9]. Intra-vascular injection is a known complication with any local anesthetic injection as experienced by one patient in this study who had a seizure of approximately 10 s duration. This patient was a 20-year-old otherwise healthy male who despite slow administration of the ropivicaine and frequent intermittent aspiration presumably had some intravascular administration. The patient was closely monitored and had no drop in oxygen saturation or blood pressure, no arrhythmia and had an immediate and complete recovery after the seizure. As he was stable and had a functional nerve block, the decision was made to continue with surgery which proceeded without further complication. There was no adverse consequence of this both in the short-term and up to 1-year post-operatively.
Ultrasound guidance in addition to a nerve stimulator and knowledge of anatomic landmarks can minimize but not eliminate the risk of epidural or intravascular spread of anesthetic. Feedback from an alert patient and utilization of a low pressure and frequent aspiration technique are similarly important. Incidence of complications if administered with care by capable anesthesiologists is not prohibitive [9, 10]; serious neurologic injury following regional anesthesia occurs in less than three cases out of 10 000 [25]. Nonetheless, these blocks should always be performed under close monitoring with supportive care and treatment immediately available.
Post-operatively, we had no falls among our patients. This is likely attributable to pre-operative and post-operative counseling that included strict use of crutches and a knee immobilizer for weight-bearing until the effects of the regional anesthesia dissipated.
In the current study, there were three different anesthesiologists performing both the LPB and FI blocks. Each of the anesthesiologists was experienced and facile with various regional nerve blocks around the body performed in an outpatient setting. Therefore, it is likely that our experience is generalizable to other centers with similar competent anesthesiologists. In light of the lack of benefit observed (contrary to previous reports of beneficial results of pre- and post-operative fascia iliaca block [6–8, 26]) and despite each of the anesthesiologists having performed well over 100 fascia iliaca blocks, it is possible that centers with more experienced anesthesiologists may experience different results with these blocks. Alternatively, it is possible that while a post-operative fascia iliaca block provides sufficient analgesia, the efficacy of this block deteriorates compared with that of a femoral nerve or lumbar plexus block when administered pre-operatively.
Interestingly, the secondary data points including the use of post-operative morphine-equivalents, post-operative nausea and time to discharge did not correlate with the decrease in patient-reported pain scores in the lumbar plexus cohort. Prior to initiation of this study, there were no clear protocols set up at this facility for post-operative pain and nausea medication administration triggers or for discharge triggers for hip arthroscopy patients. For instance, most patients were given 10 mg of oxycodone by mouth as soon as they were able to tolerate oral intake regardless of their pain level. This led to a skewing of the data towards minimal change in terms of morphine equivalents used. Similarly, most patients were monitored in the PACU for similar amounts of time (90–120 min) even if their level of discomfort was low. While this may represent a weakness of this study, it is also representative of the way many arthroscopic surgeries of the hip are performed—as outpatients in a surgical center setting with a variety of nurses and under the guidance of various anesthesiologists.
There were several additional limitations to our study. This was a retrospective study with one surgeon at one facility but several different PACU nurses and three different anesthesiologists. Pain scores were patient reported to PACU nurses who were not blinded to the type of anesthesia administered. Pain scores after discharge were not tracked, and long-term complications were not assessed beyond 1-year post-operatively. Cohorts were not precisely matched with regard to surgery performed on the labrum, with more reconstructions performed in the LPB and the Gen groups than in the FI group. Given the surgeon’s technique of an additional portal and reconstruction of 9 cm of circumferential labral tissue for reconstructions compared with a typical refixation of 2–3 cm for labral repairs, more post-operative pain would be expected in the reconstruction patients of whom there were more in the LPB and Gen groups (our data reflect the opposite).
Further study, preferably prospective and randomized design, with clear triggers for pain and nausea medication administration and criteria for time of discharge, would provide additional clarity as to the relative value of these regional nerve blocks.
FUNDING
This work was entirely self-funded by the senior author.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to acknowledge the PACU nursing staff at Harborside Surgery Center for their contributions with data collection.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Colvin AC, Harrast J, Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am 2012; 94:e23.. [DOI] [PubMed] [Google Scholar]
- 2. Montgomery SR, Ngo S, Hobson T. et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy 2013; 29:661–5. [DOI] [PubMed] [Google Scholar]
- 3. Birnbaum K, Prescher A, Hessler S. et al. The sensory innervation of the hip joint—an anatomical study. Surg Rad Anat 1997; 19:371–5. [DOI] [PubMed] [Google Scholar]
- 4. Robertson WJ, Kelly BT. The safe zone for hip arthroscopy: a cadaveric assessment of central, peripheral, and lateral compartment portal placement. Arthroscopy 2008; 24:1019–26. [DOI] [PubMed] [Google Scholar]
- 5. Dolan J, Williams A, Murney E. et al. Ultrasound guided fascia iliaca block: a comparison with the loss of resistance technique. Reg Anesth Pain Med 2008; 33:526–31. [DOI] [PubMed] [Google Scholar]
- 6. Krych AJ, Baran S, Kuzma SA. et al. Utility of multimodal analgesia with fascia iliaca blockade for acute pain management following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc 2014; 22:838–47. [DOI] [PubMed] [Google Scholar]
- 7. Anaraki AN, Mirzaei K. The effect of fascia iliaca compartment block versus gabapentin on postoperative pain and morphine consumption in femoral surgery, a prospective, randomized, double-blind study. Indian J Pain 2014; 28:111–6. [Google Scholar]
- 8. Monzon DG, Iserson KV, Vazquez JA. Single fascia iliaca compartment block for post-hip fracture pain relief. J Emerg Med 2007; 32:257–62. [DOI] [PubMed] [Google Scholar]
- 9. Amiri HR, Zamani MM, Safari S. Lumbar plexus block for management of hip surgeries. Anesth Pain Med 2014; 4:e19407.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marino J, Russo J, Kenny M. et al. Continuous lumbar plexus block for postoperative pain control after total hip arthroplasty. A randomized controlled Trial. J Bone Joint Surg Am 2009; 91:29–37. [DOI] [PubMed] [Google Scholar]
- 11. Winnie AP, Ramamurthy S, Durrani Z. The inguinal paravascular technic of lumbar plexus anesthesia. Anesth Analg 1973; 52:989–96. [PubMed] [Google Scholar]
- 12. Heller AR, Fuchs A, Rössel T. et al. Precision of traditional approaches for lumbar plexus block: impact and management of interindividual anatomic variability. Anesthesiology 2009; 111:525–32. [DOI] [PubMed] [Google Scholar]
- 13. Touray ST, de Leeuw MA, Zuurmond WW. et al. Psoas compartment block for lower extremity surgery: a meta-analysis. Br J Anaesth 2008; 101:750–60. [DOI] [PubMed] [Google Scholar]
- 14.PL Detail-Document, Equianalgesic Dosing of Opioids for Pain Management. Pharmacist’s Letter/Prescriber’s Letter. August 2012.
- 15. Xing JG, Abdallah FW, Brull R. et al. Preoperative femoral nerve block for hip arthroscopy: a randomized, triple-masked controlled trial. Am J Sports Med 2015; 43:2680–7. [DOI] [PubMed] [Google Scholar]
- 16. Kelly AM. Does the clinically significant difference in visual analog pain scores vary with gender, age, or cause of pain? Acad Emerg Med 1998; 5:1086–90. [DOI] [PubMed] [Google Scholar]
- 17. Todd KH, Funk KG, Funk JP. et al. Clinical significance of reported changes in pain severity. Ann Emerg Med 1996; 27:485–9. [DOI] [PubMed] [Google Scholar]
- 18. Dworkin RH, Turk DC, McDermott MP. et al. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain 2009; 146:238–44. [DOI] [PubMed] [Google Scholar]
- 19. De Leeuw MA, Zuurmond WW, Perez RS. The psoas compartment block for hip surgery: the past, present and future. Anesth Res Pract 2011; 2011:159541. doi: 10.1155/2011/159541. Epub 2011 May 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fournier R, Van Gessel E, Gaggero G. et al. Postoperative analgesia with “3-in-1” femoral nerve block after prosthetic hip surgery. Can J Anaesth 1998; 45:34–8. [DOI] [PubMed] [Google Scholar]
- 21. Reavley P, Montgomery AA, Smith JE. et al. Randomised trial of the fascia iliaca block versus the ‘3-in-1’ block for femoral neck fractures in the emergency department. Emerg Med J 2015; 32:685–9. [DOI] [PubMed] [Google Scholar]
- 22. Yadeau JT, Tedore T, Goytizolo EA. et al. Lumbar plexus blockade reduces pain after hip arthroscopy: a prospective randomized controlled trial. Anesth Analg 2012; 115:968–72. [DOI] [PubMed] [Google Scholar]
- 23. Dold AP, Murnaghan L, Xing J. et al. Preoperative femoral nerve block in hip arthroscopic surgery: a retrospective review of 108 consecutive cases. Am J Sports Med 2014; 42:144–9. [DOI] [PubMed] [Google Scholar]
- 24. Ward JP, Albert DB, Altman R. et al. Are femoral nerve blocks effective for early postoperative pain management after hip arthroscopy? Arthroscopy 2012; 28:1064–9. [DOI] [PubMed] [Google Scholar]
- 25. Auroy Y, Benhamou D, Bargues L. et al. Major complications of regional anesthesia in France. The SOS regional anesthesia hotline service. Anesthesiology 2002; 97:1274–80. [DOI] [PubMed] [Google Scholar]
- 26. Potter MQ, Sun GS, Fraser JA. et al. Psychological distress in hip arthroscopy patients affects postoperative pain control. Arthroscopy 2014; 30:195–201. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.