Abstract
Minimally invasive plate osteosynthesis (MIPO) techniques have been developed to protect the blood flow to tissues surrounding fractures and reduce the risk of non-union. Typically, MIPO involves the insertion of a plate through a small incision and fixation with percutaneously applied screws targeted fluoroscopically. Here we present a case of a transected anterior tibial artery during routine minimally invasive plate osteosynthesis of a tibial plateau fracture to highlight a rare complication of this type of surgery and discuss relevant anatomical considerations.
Level of evidence
According to the OCEBM Levels of Evidence Working Group, this study is graded as a Level of Evidence IV.
Keywords: Anterior tibial artery, Tibial plateau fracture, Minimally invasive plate osteosynthesis
Introduction
Relative to other long-bone fractures, the tibia is distinctive for non-unions secondary to its limited soft tissue envelope [1]. Consequently, minimally invasive plate osteosynthesis (MIPO) techniques have been developed to safeguard extraosseous blood flow and improve union rates [2]. Despite preservation of microvascular blood supply, injury to larger neurovascular bundles is a known risk of less-invasive exposures, as they do not afford direct visualization of these critical structures. Nonetheless, injury to the anterior tibial artery in the proximal tibia is exceedingly rare, with only one other example reported in the literature [3]. Here we describe a case of injury to the proximal anterior tibial artery during routine percutaneous plating of the proximal tibia.
Case report
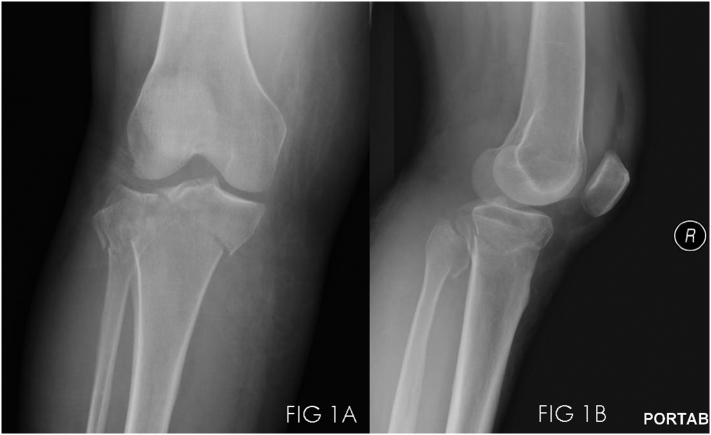
A 55-year-old pedestrian was transferred to our institution after being struck by a motor vehicle, having sustained a Schatzker VI tibial plateau fracture (AO/OTA 41.C1, Fig. 1A/B). On examination she was neurovascularly intact with palpable dorsalis pedis and posterior tibial pulses. While there were no signs of compartment syndrome, she had sufficient swelling to preclude immediate definitive osteosynthesis.
Fig. 1.
AP injury film showing AO/OTA41.C1 proximal tibia fracture (1A). Lateral (1B).
Accordingly, initial management consisted of closed reduction and placement of a length-stable spanning knee external fixator. She remained neurovascularly intact with intact pedal pulses and returned to the floor for ice and traction elevation.
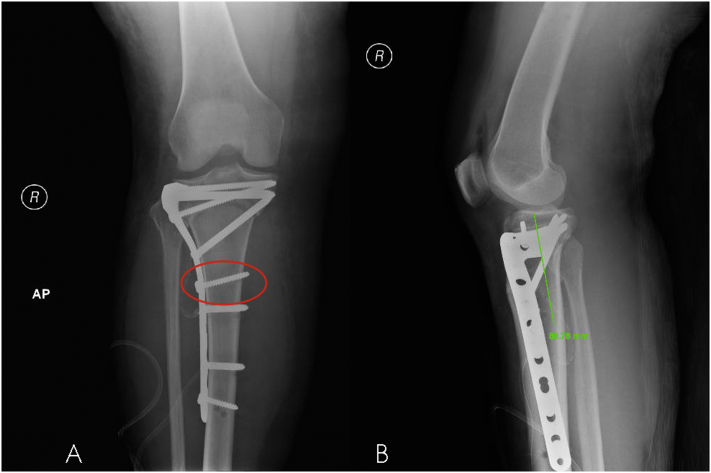
Once the soft-tissue swelling had adequately resolved (hospital day #5), the patient was returned to the operating room for osteosynthesis. A sterile tourniquet was available but not used. The authors performed an anterolateral approach to the tibial plateau through a 10 cm curvilinear incision centered over Gerdy's tubercle. The proximal anterior compartment was laterally elevated to expose the fracture. A minimal submeniscal arthrotomy was then performed to expose the joint surface. After the medial and lateral articular surfaces had been reduced and fixed with lag screws, the authors elected to plate the lateral tibia using a 4.5 mm large-fragment lateral tibial plateau locking plate (Synthes, West Chester, PA) measuring 154 mm in length(Fig. 2A/B). The plate was applied through the surgical incision in submuscular, extraperiosteal fashion to the anterolateral face of the tibia. The plate was secured in a distal to proximal fashion using percutaneous 4.5 mm cortical screws, by first making a small 1 cm stab incision, dilating the incision with a hemostat, then drilling under fluoroscopic guidance through a soft-tissue protector.
Fig. 2.
AP (2A) and lateral (2B) postoperative films.
During insertion of the solid soft-tissue protection sleeve and drill-bit 73 mm from the proximal aspect of the plate and 80 mm from the tibial plateau, brisk bleeding was encountered. Pressure was held over the incision, but bleeding continued despite this. At this point the authors expanded the distal incision another 5 cm and explored the anterior compartment of the leg. Multiple arborizing vessels of the anterior tibial artery were discovered as well as a transection injury to the main vessel, which coursed through the muscular belly of the tibialis anterior muscle.
The artery was isolated proximal and distal to the transection point, but primary repair was not felt to be obtainable. Collateral flow through the posterior tibial artery was confirmed by palpation. Subsequently, the authors proceeded to ligate the anterior tibial artery at the level of injury using 2–0 silk ties. The foot remained well-perfused with intact posterior tibial arterial flow and the remainder of the screw fixation was applied. Estimated blood loss from this portion of the procedure was 150 ml.
Postoperatively the patient had full motor and sensory function to her lower extremity. She continued to have intact pedal pulses although her dorsalis pedis pulse was moderately diminished on palpation (1 +). On Doppler exam her dorsalis pedis continued to have biphasic retrograde flow with a weaker signal compared to the contralateral extremity.
On 4 month follow up the patient was doing well with excellent clinical and radiographic evidence of healing. Distally she remained neurovascularly intact. This case has undergone institutional ethical board review prior to submission.
Discussion
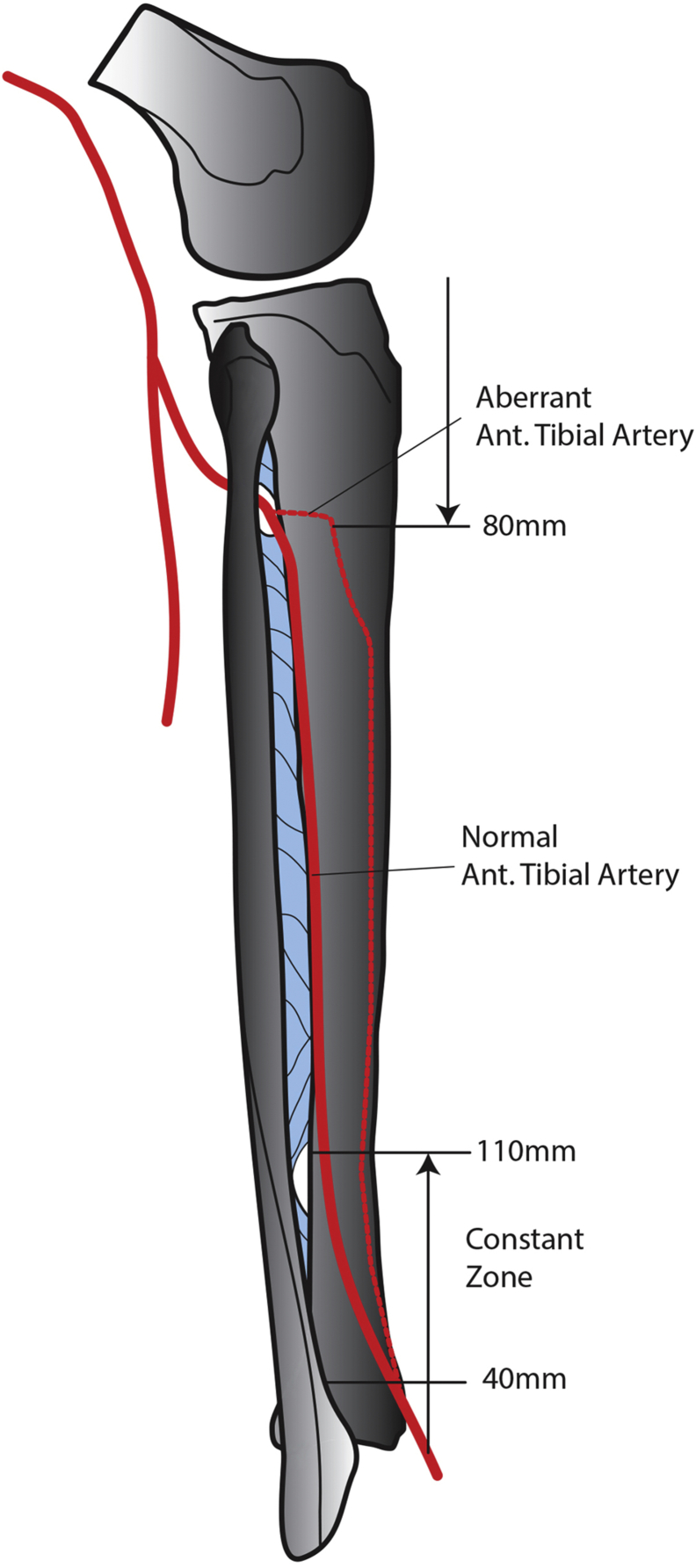
The anterior tibial artery passes through the oval foramen of the interosseous membrane at the proximal tibia where it is anchored by genicular arteries (Fig. 3). It then runs along the interosseous membrane against the posterior aspect of the lateral tibia face. Distally it is described as gradually moving toward the anterior cortical surface, and thus is typically not at risk with proximal lateral procedures [4].
Fig. 3.
Schematic of anatomic and aberrant tibial artery course.
Percutaneous injury to the proximal anterior tibial artery is rare, with only one other case reported in the literature [3]. While minimally invasive plate osteosynthesis (MIPO) techniques are commonly utilized for distal tibia fractures [2], [5], [6], they are also useful with treating proximal articular fractures with metaphyseal involvement [7]. MIPO techniques are advantageous as they limit exposure and disruption of periosteal blood supply [8], [9]. However, one distinct disadvantage is the inability to directly observe structures at risk.
As visualization is limited with MIPO techniques, detailed understanding of regional anatomy is critical for safety. Typically, the anterior tibial artery is not at risk in the proximal lateral portion of the tibia. In their cadaver study, Wolinsky et al. describe a constant region 40–110 mm from the tibial plafond where the anterior tibial artery courses from proximal posterior to distal anterior and recommend direct open exposure for MIPO procedures in this area [10]. In a similar cadaver study, Lidder et al. describe the neurovascular bundle (anterior tibial artery and deep peroneal nerve) as crossing through a danger zone on average 76 mm from the plafond with a range of 21–138 [11].
In their case report, Gary et al. describe percutaneous injury to the anterior tibial artery 189 mm below the tibia plateau [3]. This patient had sustained an AO/OTA 41.C3 injury and had probable alteration of his anatomy through extensive metaphyseal extension of the fracture, multiple debridements, fasciotomies, and skin grafting. Other case reports have documented pseudoaneurysm of the anterior tibial artery resulting from other types of minimally invasive surgery, specifically external fixator and Ilizarov frame application [12], [13], [14].
Here we describe a case of injury to the anterior tibial artery adjacent to the proximal tibia in a patient with likely unaltered anatomy to highlight its rarity. Similar to the case described by Gary et al., the authors also did not inflate the tourniquet which could have made the vessels a larger target secondary to engorgement. However, our vascular injury occurred much more proximal in the tibia (80 mm vs 189 mm) than in the case described by Gary, consistent with an even greater anomalous course.
In conclusion, the anterior tibial artery is rarely encountered in percutaneous plating of the proximal tibia. If injured, the artery can be treated successfully with exploration and ligation after appropriate confirmation of collateral flow.
Conflict of interest
None.
References
- 1.Horne G., Iceton J., Twist J., Malony R. Disability following fractures of the tibial shaft. Orthopedics. 1990 Apr;13(4):423–426. doi: 10.3928/0147-7447-19900401-08. [DOI] [PubMed] [Google Scholar]
- 2.Collinge C., Kuper M., Larson K., Protzman R. Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J. Orthop. Trauma. 2007;21(6):355–361. doi: 10.1097/BOT.0b013e3180ca83c7. [DOI] [PubMed] [Google Scholar]
- 3.Gary J.L., Sciadini M.F. Injury to the anterior tibial system during percutaneous plating of a proximal tibial fracture. Orthopedics. 2012 Jul 1;35(7):e1125–e1128. doi: 10.3928/01477447-20120621-37. [DOI] [PubMed] [Google Scholar]
- 4.Ebraheim N.A., Lu J., Hao Y., Biyani A., Yeasting R.A. Anterior tibial artery and its actual projection on the lateral aspect of the tibia: a cadaveric study. Surg. Radiol. Anat. 1998;20(4):259–262. doi: 10.1007/BF01628486. [DOI] [PubMed] [Google Scholar]
- 5.Collinge C., Sanders R., DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin. Orthop. 2000 Jun;375:69–77. doi: 10.1097/00003086-200006000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Collinge C., Protzman R. Outcomes of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. J. Orthop. Trauma. 2010;24(1):24–29. doi: 10.1097/BOT.0b013e3181ac3426. [DOI] [PubMed] [Google Scholar]
- 7.Oh J.-K., Oh C.-W., Jeon I.-H., Kim S.-J., Kyung H.-S., Park I.-H. Percutaneous plate stabilization of proximal tibial fractures. J. Trauma Injury Infect Crit. Care. 2005 Aug;59(2):431–437. doi: 10.1097/01.ta.0000174733.67446.83. [DOI] [PubMed] [Google Scholar]
- 8.Farouk O., Krettek C., Miclau T., Schandelmaier P., Guy P., Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J. Orthop. Trauma. 1999 Aug;13(6):401–406. doi: 10.1097/00005131-199908000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Borrelli J., Jr., Prickett W., Song E., Becker D., Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J. Orthop. Trauma. 2002;16(10):691–695. doi: 10.1097/00005131-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Wolinsky P., Lee M. The distal approach for anterolateral plate fixation of the tibia: an anatomic study. J. Orthop. Trauma. 2008;22(6):404–407. doi: 10.1097/BOT.0b013e31817614b2. [DOI] [PubMed] [Google Scholar]
- 11.Lidder S., Masterson S., Grechenig C., Clement H., Gänsslen A., Grechenig S. The risk of neurovascular injury in minimally invasive plate osteosynthesis (MIPO) when using a distal tibia anterolateral plate: a cadaver study. Acta Chir. Orthop. Traumatol. Cechoslov. 2014;81(5):313–316. [PubMed] [Google Scholar]
- 12.Braito W., Montanari C., Caracciolo F., Paroni G., Domenella G. False aneurysm of the anterior tibial artery in lower leg fractures treated with the Ilizarov external fixator. Case report. Ital. J. Orthop. Traumatol. 1992;18(1):135–139. [PubMed] [Google Scholar]
- 13.Griffith J.F., Cheng J.C., Lung T.K., Chan M. Pseudoaneurysm after high tibial osteotomy and limb lengthening. Clin. Orthop. 1998 Sep;354:175–179. doi: 10.1097/00003086-199809000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Suri T., Dabas V., Sural S., Dhal A. Pseudoaneurysm of the anterior tibial artery: a rare complication of proximal tibial steinman pin insertion. Indian J. Orthop. 2011 Mar;45(2):178–180. doi: 10.4103/0019-5413.77140. [DOI] [PMC free article] [PubMed] [Google Scholar]