Abstract
The disadvantages of the one-third-tubular plate construct to stabilize lateral malleolar fractures include; difficulty achieving adequate cancellous screw thread purchase in the bone of the distal fragment, with subsequent risk of the screws backing out. This can cause irritation and pain, and may require further surgery to remove the screw. We describe a variation of the standard technique that eliminates the risk of the distal lateral malleolar screws backing out and provides a lower profile construct. This has the potential advantages of reduced wound related problems and less postoperative pain and irritation.
Introduction
An inter-fragmentary lag screw protected by a lateral one-third tubular plate is the most commonly used fixation method for treating displaced lateral malleolar fractures. Difficulty achieving adequate screw thread purchase in the cancellous bone of the distal fragment can lead to the screws backing out. This can cause construct failure and prominent metalwork, resulting in pain and irritation.
We describe a simple variation on the standard one-third-tubular plate construct method of protecting the lag screw fixation during lateral malleolar fracture surgery. The proposed advantages are of a more stable construct, reduced risk of the distal screws backing out, and a lower profile construct resulting in potentially fewer wound healing problems and less postoperative pain and irritation.
Technique
The fracture is reduced and inter-fragmentary compression achieved using a lag screw according to standard AO techniques.
Step 1: A one-third-tubular LCP 3.5 mm locking plate of appropriate length is selected.
Step 2: 3.5 mm LCP drill guides are secured into the reciprocal distal screw holes of the plate (Fig. 1A and Fig. 1B).
Fig. 1.
A – 3.5 mm LCP one-third-tubular plate hole with pre-milled thread to receive 3.5 mm LCP drill guide.
B – 3.5 mm LCP drill guides secured into distal holes of the LCP one-third-tubular plate.
C – LCP one-third-tubular plate contoured to distal fibula with 3.5 mm LCP drill guides in most distal holes.
D – Deformation of pre-milled thread in LCP one-third-tubular plate where LCP drill guide was not in place during plate contouring.
E – LCP one-third-tubular titanium plate secured to a saw bone with two distal 3.5 mm locking head screws and two proximal 3.5 mm cortical screws.
Step 3: The plate is contoured according to the shape of the distal fibula, taking care not to lever on the threaded drill guides (Fig. 1C).
Note: Securing the threaded drill guides into the reciprocal threaded holes on the plate prior to plate contouring prevents deformation of the pre-milled thread in the plate (Fig. 1D).
Step 4: The plate is accurately applied onto the lateral malleolar bone by applying pressure to the attached drill guides.
Note: this is important, as the locking screw will not compress the plate onto the bone.
Step 5: The distal plate is secured using 3.5 mm locking uni-cortical screws in the distal fragment (where uni-cortical cancellous non locking head screws would usually be placed). We normally use standard non-locking bi-cortical screws proximally in the plate (Fig. 1E).
Results
During a 12-month period a single consultant performed the above technique on 6 patients with displaced lateral malleolar fractures. No complications were encountered during the surgical procedures. The patients were followed up routinely at six weeks, 12 weeks, six months, and 12 months post-operatively. There were no wound related problems nor metalwork related irritation or pain. At 12 month follow up there was no radiographic evidence of the distal screws backing out in any of the patients in our series.
Clinical case
A 46-year-old female presented with a displaced Webber B fracture of the right lateral malleolus. The fracture was reduced and compressed using a standard lag screw technique. A one-third-tubular plate was secured as described above (Fig. 2).
Fig. 2.
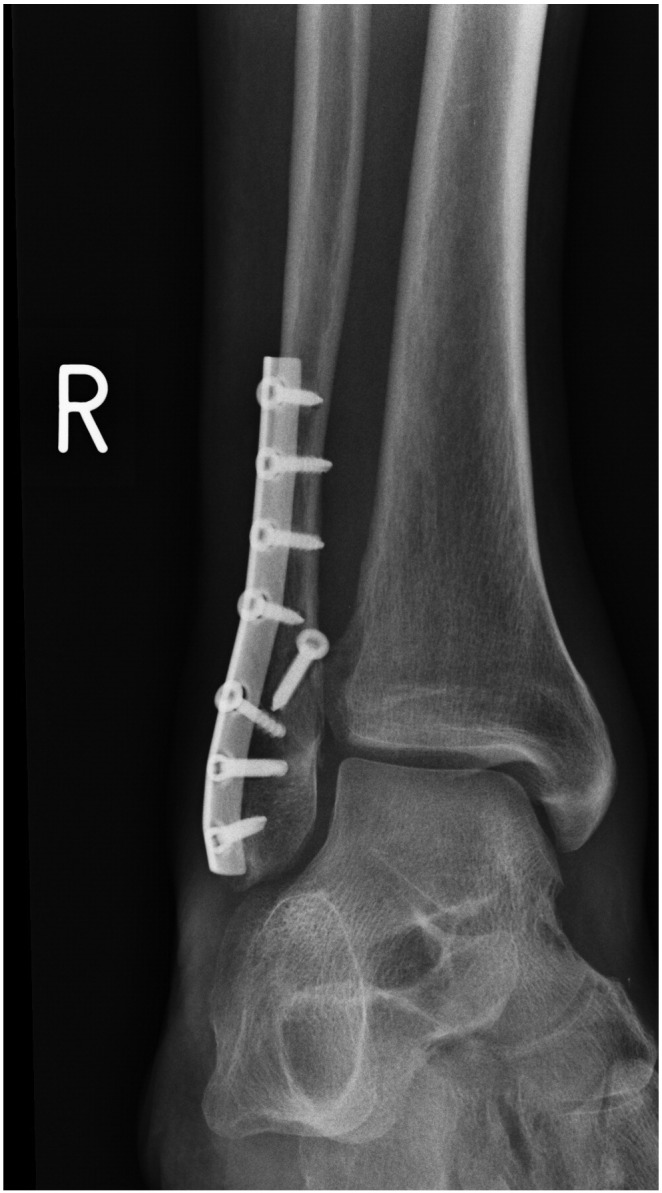
Post-operative anterior-posterior radiograph following open reduction and internal fixation with a standard lag screw technique and a one-third-tubular locking plate, secured with distal 3.5 mm locking head screws and proximal cortical screws.
Discussion
We suspect that knowledge of the capability of the Stainless Steel and Titanium one-third-tubular plate to accept a 3.5 mm locking head screw head is limited (Fig. 1A).
Indications
This technique can be used for any lateral malleolar fracture that the surgeon would usually reduce and fix with a standard lag screw and one-third-tubular plate construct.
Limitations
We advocate the use of a one-third-tubular plate with distal locking screws to act as a neutralizing construct and not to act as a bridging plate. Therefore we are not advocating our technique as a replacement for the pre-contoured distal fibular locking plates for use in the osteoporotic patient where poor bone quality can make it difficult to achieve fixation.
Strengths
We describe the use of a stable lower profile construct with theoretical advantages of fewer wound healing problems and less postoperative pain and irritation related to the metalwork.
The difference in screw head profile although small has the potential to reduce skin related pressure symptoms over the subcutaneous distal fibula.
The senior author has received referrals to assess patients with irritation and pain related to distal malleolar screws blacking out of cancellous bone (Fig. 3). The locking head screws eliminate the risk of screws backing out in the construct we describe. Our technique is cost neutral with a non-locking cancellous screw and locking head screw having the same cost in our trust.
Fig. 3.

Example of distal non-locking screw backing out and causing skin irritation and pain.
Conclusion
Our technique is performed easily and we believe provides a superior alternative to the one-third-tubular plate secured with non-locking head screws.
Author conflict of interests
None.
Contributions not meeting authorship criteria
None.
Funding sources
None.
Author financial support
None.
Contributor Information
Daniel S. Hill, Email: daniel.hill1@nhs.net.
A. Nadeem Baqai, Email: nadeem.baqai@mbht.nhs.uk.



