Abstract
Background
Chronic obstructive pulmonary disease (COPD) is a serious disease frequently accompanied by anxiety and depression. Few studies have focused on anxiety and depression for mild COPD patients in China. This study aimed to assess the prevalence and associated factors for anxiety and depression among patients with mild COPD in urban communities.
Methods
A cross-sectional survey of 275 mild COPD patients was conducted in 6 communities randomly sampled from Pudong New Area of Shanghai, China, in 2016. Data on socioeconomic factors and health conditions were acquired through a face-to-face interview as well as a physical examination. The Hospital Anxiety and Depression Scale (HAD) and EQ-5D visual analogue (EQ-5Dvas) were applied to evaluate their mental health and quality of life, respectively. Logistic regression model was used to estimate adjusted odds ratios (aORs) and their 95% confidential intervals (CI) for risk factors associated with anxiety or depression.
Results
Among 275 subjects, 8.1% had anxiety and 13.4% had depression. Logistic regression analysis indicated that female patients were more likely to suffer from anxiety than male patients (aOR = 6.41, 95% CI:1.73-23.80). Poor health status (EQ-5Dvas score < 70) was significantly associated with increased risks of anxiety (aOR = 5.99, 95% CI: 2.13-16.82) and depression (aOR = 2.67, 95% CI: 1.29-5.52).
Conclusions
There were increased risks of anxiety and depression in mild COPD patients living in urban communities. Female sex and poor health status were significantly correlated to anxiety or depression. More interventions should be developed to reduce the risks of anxiety and depression at the early stage of COPD.
Electronic supplementary material
The online version of this article (10.1186/s12888-018-1671-5) contains supplementary material, which is available to authorized users.
Keywords: Depression, Anxiety, Quality of life, COPD, Mild
Background
Chronic obstructive pulmonary disease (COPD) was the fifth leading cause of mortality globally in 2011, and was expected to be the third leading cause by 2030 [1]. In 2010, the total cost of COPD was 50 billion US dollars and the average cost per patient was over 4000 US dollars in the US, while they were respectively 36.9 billion and 2259 US dollars in China [2–6].
Patients of COPD are at a considerable risk of suffering from symptoms of depression and anxiety [7]. The prevalence of anxiety symptoms varied from 30 to 90%, and that of depressive symptoms ranged from 13 to 70% among COPD patients (mostly inpatients) [8–13]. Previous studies indicated that anxiety and depressive symptoms in COPD patients were correlated with various factors including age, gender, severity of COPD, general health status, smoking, physical endurance and social performance [14–18]. These studies were mainly conducted among inpatients who had severe COPD, and few of them focused on the prevalences of depression and anxiety and their influencing factors among mild COPD patients in community settings [8–19]. The aim of this study was to estimate the prevalences of anxiety and depression among mild COPD patients living in urban Chinese communities and their associated factors.
Methods
Study site and population
A cross-sectional study was carried out in Pudong New Area of Shanghai, China, from June to August in 2016. A register system including data of diagnosed COPD patients from all secondary and tertiary hospitals was created in 2014. Six out of 46 communities were selected randomly to recruit patient with mild COPD. At the enrollment, spirometry function test was implemented on each patient to verify their COPD severity. Inclusion criteria were as follows: 1) a person was previously diagnosed as mild COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) (forced expiratory volume in one second of percent predicted (FEV1% predicted) ≥80%, the ratio of FEV1 to forced vital capacity (FVC) < 0.7) [20]; 2) a person provided informed consent and medical records were available; and 3) a person was a local resident aged 40 to 70 years and was capable of participating in the study by themselves. Patients with serious or unstable disease(s) (such as cardiovascular, neurological and musculoskeletal diseases) or inpatients were excluded. Patients with cognitive impairment and mobility limitation were excluded as well. Among 300 patients who participated in the study, 275 (91.7%) met all the criteria and were included in this analysis.
Data collection and quality control
All information was collected by using a structured questionnaire and a physical examination. Demographic information included age, alcohol drinking history (Yes/No), smoking history (Yes/No), years of education (< 9 years/≥9 years), monthly household income (< 3000 RMB/≥3000 RMB), and regular exercise (Yes/No). Clinical information collected included disease duration, regular use of COPD medications in the past 12 months (Yes/No), exacerbation in the past 12 months (Yes/No) and comorbid conditions (hypertension, diabetes, kidney disease, stroke, cardiovascular diseases or others).
All field investigators received specific trainings in questionnaire interviewing, data recording and specific medical testing (scale assessment and spirometry function test) before the study was conducted. Questionnaire data were double-checked for its accuracy and completeness.
Measurements of anxiety and depression symptoms as outcome variables
The Hospital Anxiety and Depression Score (HAD) is a concise and commonly used questionnaire to assess the existence of depression and anxiety symptoms for COPD patients [21–25] (Additional file 1). The HAD is a self-administered questionnaire with two subscales (HAD-A for anxiety symptom and HAD-D for depression symptom) and each subscale contains seven items. Each item score ranges from 0 to 3, and the total score for each subscale ranges from 0 to 21 (0 manifests rare symptom, and 3 indicates apparent symptom) [21, 22]. Studies showed that HADs with ≥8 points as cut-off points for anxiety and depression symptoms performed great sensitivity and specificity in Chinese patients [19, 26]. Participants with a HAD score greater than 8 points were more likely to suffer from anxiety or depression, and a higher score implies more advanced severity of clinically anxious or depressed symptom [15, 18, 21, 27].
In the current study, we defined a patient with “anxiety” or “depression” as having a HAD-A or HAD-D score of 8 points or higher.
Spirometry function test, physical examination and health status assessment
Spirometry function test was performed at enrollment to acquire FEV1 and FVC values as well as FEV1% predicted to determine COPD severity or stage according to the guideline for COPD [20]. Each patient inhaled 20 ml salbutamol before pulmonary function testing was conducted and then complied with steps required for a spirometry function test. Final pulmonary function testing values were the average values of two satisfactory tests. Height and weight were measured to calculate body mass index (BMI, weight (kg)/height2 (m2)). In addition, health status was assessed with EQ-5D visual analogue (EQ-5Dvas), which was considered to be a reliable and efficient tool for previous COPD studies [28–30]. Two previous studies used the visual analogue as a measure of quality of life in the association with depressive and anxious symptoms [31, 32]. For the EQ-5Dvas test, each patient drew a horizontal line on a scale to represent their health status, ranging from 0 (worst imaginable health status) at the bottom to 100 (best imaginable health status) at the top.
Statistical analysis
Data analysis was performed by using SAS 9.2 for Windows (SAS Institute, Inc., Cary, NC). Pearson Chi square test or Fisher exact test was used for comparisons of categorical variables. Student t-test or Wilcoxon test was applied for two-group comparisons of continuous variables with or without a normal distribution. Logistic regression analysis was used to estimate crude odds ratios (cORs) and adjusted OR (aOR) as well as their 95% confidential intervals (CI) for risk factors associated with anxiety or depression. The p value of < 0.05 was considered statistically significant.
Results
Basic characteristics of subjects
Among 275 patients, 134 (48.7%) were male. The average age and BMI were 61.5 ± 6.0 years and 25.1 ± 4.0 (Kg/m2), respectively. Nearly 40% of participants had a history of smoking, with a higher proportion of ever smoking in male patients than in female patients. Women had a longer average duration of COPD (13.2 years) and were more likely to have a comorbid condition (59.6%), compared to men. There were no significant differences in EQ-5Dvas scores, regular use of COPD medications, as well as exacerbation in the past 12 months between male and female patients (Table 1).
Table 1.
Basic information among male and female patients with mild COPD
| Characteristics | Total | Male | Female | P value |
|---|---|---|---|---|
| Number [n(%)] | 275 | 134(48.7) | 141(51.3) | . |
| Age, years [mean(SD)] | 61.5(6.0) | 62.1(5.4) | 60.9(6.5) | 0.113 |
| BMI (kg/m2) [mean(SD)] | 25.1(4.0) | 24.7(3.9) | 25.5(4.2) | 0.074 |
| Ever alcohol drinking [n(%)] | 54(19.6) | 49(36.6) | 5(3.5) | < 0.0001 |
| Ever smoking [n(%)] | 115(41.8) | 113(84.3) | 2(1.4) | < 0.0001 |
| Regular exercise [n(%)] | 98(35.6) | 48(35.8) | 50(35.5) | 0.95 |
| Years of education [n(%)] | ||||
| < 9 | 229(83.3) | 109(81.3) | 120(85.1) | 0.403 |
| ≥ 9 | 46(16.7) | 25(18.7) | 21(14.9) | |
| Monthly household income per capita/Yuan [n(%)] | ||||
| < 3000/per month | 141(51.3) | 57(42.5) | 84(59.6) | 0.005 |
| ≥ 3000/per month | 134(48.7) | 77(57.5) | 57(40.4) | |
| Duration of COPD, year [mean(SD)] | 11.3(14.1) | 9.4(13.9) | 13.2(14.1) | 0.004 |
| EQ-5Dvas score [mean(IQR)] | 70.6(14.3) | 70.1(14.6) | 71.0(14.1) | 0.322 |
| Regular COPD medication use, in recent 12 months [n(%)] | 97(35.3) | 48(35.8) | 49(34.8) | 0.853 |
| Exacerbation, in recent 12 months [n(%)] | 77(28.0) | 35(26.1) | 42(29.8) | 0.498 |
| Comorbidity [n(%)] | 145(52.7) | 61(45.5) | 84(59.6) | 0.020 |
Abbreviations: BMI body mass index
For comparison, χ2 test used for binary variables, and Student’s t test or Wilcoxon non-parametric test employed for continuous variables; the bold P values indicated the statistical significance
Prevalences of anxiety and depression
The overall prevalences of anxiety and depression were 7.6 and 13.1%, respectively. Figure 1 shows the prevalences according to sex, smoking history and health status. An increased risk of anxiety was observed in female patients (12.8%, P < 0.001), smokers (11.3%, P = 0.008) and those with poor health status (EQ-5Dvas score < 70) (15.6%, P = 0.0003). Patients with poor health status (EQ-5Dvas score < 70) (20.8%) were more likely to suffer from depression than those with better health status (8.9%) (P = 0.005) (Fig. 2).
Fig. 1.
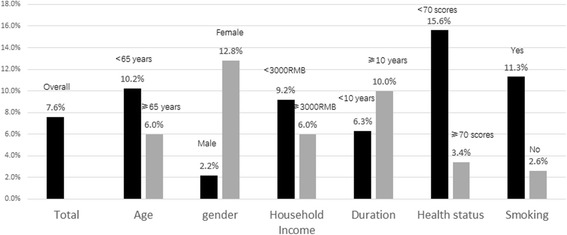
Prevalence of anxiety symptoms among patients of mild COPD
Fig. 2.

Prevalence of depression symptoms among patients of mild COPD
Factors associated with anxiety and depression
After adjustment for covariates, female patients were more likely to suffer from anxiety (aOR = 6.41, 95% CI: 1.73-23.80), and patients with poor health status (EQ-5Dvas score < 70) had a higher risk of anxiety (aOR = 5.99, 95% CI: 2.13-16.82) (Table 2). Similarly, poor health status was significantly associated with an increased risk of depression (aOR = 2.67, 95% CI: 1.29-5.52) after important covariates were taken into account (Table 3).
Table 2.
Possible factors associated with anxiety symptoms among mild COPD patients
| Characteristics | cOR(95%CI)a | aOR(95%CI)b |
|---|---|---|
| Gender | ||
| Male | 1.00 | 1.00 |
| Female | 6.39(1.84~ 22.23) | 6.41(1.73~ 23.79) |
| Age, years | ||
| < 65 | 1.00 | 1.00 |
| ≥ 65 | 0.56(0.23~ 1.37) | 0.58(0.21~ 1.55) |
| Household income per capita/Yuan | ||
| < 3000/per month | 1.00 | 1.00 |
| ≥ 3000/per month | 0.86(0.63~ 1.16) | 1.04(0.74~ 1.46) |
| Duration, years | ||
| < 10 | 1.00 | 1.00 |
| ≥ 10 | 1.66(0.68~ 4.05) | 1.21(0.45~ 3.19) |
| EQ-5Dvas score | ||
| ≥ 70 | 1.00 | 1.00 |
| < 70 | 5.34(1.20~ 14.27) | 5.99(2.13~ 16.82) |
| Comorbidities | ||
| No | 1.00 | 1.00 |
| Yes | 0.98(0.40~ 2.40) | 0.90(0.33~ 2.43) |
Abbreviations: cOR crude odds ratio, aOR adjusted odds ratio
a Data represents univariate association as determined by logistic regression model
b Variable included in the multivariate logistic regression model: gender, age, monthly household per capita, disease duration, EQ-5Dvas score and comorbidity; the bold OR (95% CI) indicated the statistical relationship
Table 3.
Possible factors associated with depression symptoms among COPD patients
| Characteristics | cOR(95%CI)a | aOR(95%CI)b |
|---|---|---|
| Gender | ||
| Male | 1.00 | 1.00 |
| Female | 1.58(0.77~ 3.24) | 1.48(0.69~ 3.19) |
| Age, years | ||
| < 65 | 1.00 | 1.00 |
| ≥ 65 | 0.69(0.34~ 1.39) | 0.68(0.32~ 1.41) |
| Household income per capita/Yuan | ||
| < 3000/per month | 1.00 | 1.00 |
| ≥ 3000/per month | 0.86(0.68~ 1.09) | 0.91(0.71~ 1.17) |
| Duration, year | ||
| < 10 | 1.00 | 1.00 |
| ≥ 10 | 1.13(0.55~ 2.33) | 0.95(0.44~ 2.02) |
| EQ-5Dvas score | ||
| ≥ 70 | 1.00 | 1.00 |
| < 70 | 2.68(1.32~ 5.46) | 2.67(1.29~ 5.52) |
| Comorbidities | ||
| No | 1.00 | 1.00 |
| Yes | 0.88(0.44~ 1.78) | 0.89(0.43~ 1.86) |
Abbreviations: cOR crude odds ratio, aOR adjusted odds ratio
a Data represents univariate association as determined by logistic regression model
b Variable included in the multivariate logistic regression model: gender, age, monthly household per capita, disease duration, EQ-5Dvas score and comorbidity; the bold OR (95% CI) indicated the statistical relationship
Discussion
In this cross-sectional study, the prevalence was 7.6% for anxiety and 13.1% for depression (13.1%) among mild COPD patients living in urban community. The prevalences for COPD patients were higher as compared with those for general populations [19, 33–35]. Among the general adult population in China, the prevalences of anxiety and depression were 5.3 and 7.2%, respectively, when assessed by the HADs scale, and were 5.6 and 6.1% when assessed by the Diagnostic and Statistical Manual of Mental Disorders fourth edition (DSM-IV) scale [19, 29]. Another Chinese cohort study of 0.5 million adults found that the prevalence of depressive symptoms was as low as 2.4%, which was similar to the finding from a meta-analysis of 21 studies covering 11 provinces [30, 33]. The prevalence of anxiety varied from 10 to 100%, while that of depression varied from 7 to 79% depending on the stage of COPD [34]. Most previous studies, which recruited COPD patients with moderate to extremely severe stages from hospitals, found inconsistent relationships between severity of COPD and mental health [19, 35–38]. Different instruments measuring anxiety and depression symptoms were used in different studies, which is one reason for study discrepancies [39, 40]. In this study, only mild COPD patients from community settings were included. Our prevalence estimates were lower than those using the same scale of HAD (9.6 to 49% for anxiety and 22.8 to 52% for depression) [11, 38] except for one that included patients with mild COPD only [19].
For COPD patients, women were more likely to suffer from anxiety, and poor health status assessed by using EQ-5D was associated with increased risks of both anxiety and depression. A systematic review of 10 studies showed that women were significantly more likely to suffer from anxiety than men (56% vs 35%, P = 0.04), and similar sex disparity also existed in other studies [36, 40, 41]. One possibility would be that female patients with COPD had a lower income level, a longer duration and more comorbid conditions, compared to male patients. However, sex difference remained significant after taking these factors into consideration. Similar finding for the relationships between health status and anxiety/depression were observed in other studies [14, 42, 43]. In one hand, those who have positive symptoms of anxiety or depression in general tend to report worse health status. In another hand, those with worse health status worry more about their conditions, which could worsen their anxiety or depression symptoms. A cross-sectional study provided no information on the direction of the associations. Therefore, cohort study design is required to further explore the nature of these associations.
There are strengths and limitations in this study. This study was conducted in urban communities and all invited subjects participated in the study. All subjects included in the study were confirmed to be at the mild stage of COPD based on a free post-bronchodilator pulmonary function test. However, a cross-sectional study design provided no evidence for causal associations between risk factors and presence of psychological symptoms. Since severe COPD cases were not included in this study and we could not assess the overall occurrences of anxiety and depression for COPD. In addition, the exclusion of any inpatients might result in an underestimation of the prevalences of anxiety and depression in mild COPD patients.
Conclusions
In conclusion, anxiety and depression were common in patients with mild COPD living in urban communities and mental health care services should be provided to these patients. Female sex and poor health status were significantly correlated to anxiety and depression symptoms. More interventions should be developed to reduce the risks of anxiety and/or depression at the early stage of COPD in community settings.
Additional file
The questionnaire for COPD patients in communities of Pudong District, Shanghai. The questionnaire covered on data of geographic, socioeconomic, lifestyle and occupational exposure factors, and COPD and comorbidities. (PDF 288 kb)
Acknowledgements
All authors would like to give their thanks for the health professionals in community health centers and the individuals who participated in this study.
Funding
This work was founded by the Health Science Foundation of Shanghai (201540415), Shanghai 3-Year Public Health Action Plan (GWTD2015S04) and Shanghai Leading Academic Discipline Project of Public Health (15GWZK80101). The sponsors have no role in the study design, survey process, data analysis and manuscript preparation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable requests.
Abbreviations
- CI
Confidence interval
- DSM-IV
Diagnostic and statistical manual fourth edition
- HAD
The Hospital Anxiety and Depression Score
- IQR
Interquartile range
- OR
Odds ratio
- SD
Standard deviation
Authors’ contributions
CY, RX, QH, WN, and FC contributed in study protocol and creation of questionnaire. XT, QH, ZX, WK, and RX investigated and acquired information. XT, QH, CY, WN, and FC analyzed and interpreted the data and drafted and revised different sections of the manuscript. FC and WN are accountable for all aspects of the work in ensuring that questions related to the accuracy of any part of the manuscript are appropriate investigated and resolved. All authors read and approved the final manuscript.
Authors’ information
Not applicable
Ethics approval and consent to participate
The ethic approval for this study was issued by the Institutional Review Board of the Fudan University School of Public Health. The nature and purpose of this study was illustrated and full confidentiality guaranteed. A written informed consent was obtained from all participants. They were permitted to withdraw from the study at any time without negative consequences.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12888-018-1671-5) contains supplementary material, which is available to authorized users.
Contributor Information
Tian Xiao, Email: 15211020011@fudan.edu.cn.
Hua Qiu, Email: hqiu@pdcdc.sh.cn.
Yue Chen, Email: Yue.Chen@uottawa.ca.
Xianfeng Zhou, Email: xfzhou@pdcdc.sh.cn.
Kang Wu, Email: kwu@pdcdc.sh.cn.
Xiaonan Ruan, Email: xnruan@pdcdc.sh.cn.
Na Wang, Phone: +86 215 423 7161, Email: na.wang@fudan.edu.cn.
Chaowei Fu, Phone: +86 215 423 7161, Email: fcw@fudan.edu.cn.
References
- 1.World Health Organization (WHO): Burden of COPD. Available from: http://www.who.int/respiratory/copd/burden/en. Accessed 22 Mar 2018.
- 2.Soriano JB, Rodriguez-Roisin R. Chronic obstructive pulmonary disease overview: epidemiology, risk factors, and clinical presentation. Proc Am Thorac Soc. 2011;8(4):363–367. doi: 10.1513/pats.201102-017RM. [DOI] [PubMed] [Google Scholar]
- 3.Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, Menezes AM, Sullivan SD, Lee TA, Weiss KB, et al. International variation in the prevalence of COPD (the BOLD study): a population-based prevalence study. Lancet. 2007;370(9589):741–750. doi: 10.1016/S0140-6736(07)61377-4. [DOI] [PubMed] [Google Scholar]
- 4.Wu M, Zhao Q, Chen Y, Fu C, Xu B. Quality of life and its association with direct medical costs for COPD in urban China. Health Qual Life Outcomes. 2015;13:57. doi: 10.1186/s12955-015-0241-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res. 2013;5:235–245. doi: 10.2147/CEOR.S34321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen X, Wang N, Chen Y, Xiao T, Fu C, Xu B. Costs of chronic obstructive pulmonary disease in urban areas of China: a cross-sectional study in four cities. Int J Chron Obstruct Pulmon Dis. 2016;11:2625–2632. doi: 10.2147/COPD.S118523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagena EJ, van Amelsvoort LG, Kant I, Wouters EF. Chronic bronchitis, cigarette smoking, and the subsequent onset of depression and anxiety: results from a prospective population-based cohort study. Psychosom Med. 2005;67(4):656–660. doi: 10.1097/01.psy.0000171197.29484.6b. [DOI] [PubMed] [Google Scholar]
- 8.Bentsen SB, Miaskowski C, Rustoen T. Demographic and clinical characteristics associated with quality of life in patients with chronic obstructive pulmonary disease. Qual Life Res. 2014;23(3):991–998. doi: 10.1007/s11136-013-0515-5. [DOI] [PubMed] [Google Scholar]
- 9.Di Marco F, Verga M, Reggente M, Maria CF, Santus P, Blasi F, Allegra L, Centanni S. Anxiety and depression in COPD patients: the roles of gender and disease severity. Respir Med. 2006;100(10):1767–1774. doi: 10.1016/j.rmed.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 10.Eckerblad J, Todt K, Jakobsson P, Unosson M, Skargren E, Kentsson M, Theander K. Symptom burden in stable COPD patients with moderate or severe airflow limitation. Heart Lung. 2014;43(4):351–357. doi: 10.1016/j.hrtlng.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Kunik ME, Roundy K, Veazey C, Souchek J, Richardson P, Wray NP, Stanley MA. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127(4):1205–1211. doi: 10.1378/chest.127.4.1205. [DOI] [PubMed] [Google Scholar]
- 12.Reinke LF, Slatore CG, Udris EM, Moss BR, Johnson EA, Au DH. The association of depression and preferences for life-sustaining treatments in veterans with chronic obstructive pulmonary disease. J Pain Symptom Manag. 2011;41(2):402–411. doi: 10.1016/j.jpainsymman.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 13.Walke LM, Byers AL, Tinetti ME, Dubin JA, McCorkle R, Fried TR. Range and severity of symptoms over time among older adults with chronic obstructive pulmonary disease and heart failure. Arch Intern Med. 2007;167(22):2503–2508. doi: 10.1001/archinte.167.22.2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cleland JA, Lee AJ, Hall S. Associations of depression and anxiety with gender, age, health-related quality of life and symptoms in primary care COPD patients. Fam Pract. 2007;24(3):217–223. doi: 10.1093/fampra/cmm009. [DOI] [PubMed] [Google Scholar]
- 15.Gudmundsson G, Gislason T, Janson C, Lindberg E, Suppli UC, Brondum E, Nieminen MM, Aine T, Hallin R, Bakke P. Depression, anxiety and health status after hospitalisation for COPD: a multicentre study in the Nordic countries. Respir Med. 2006;100(1):87–93. doi: 10.1016/j.rmed.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 16.Dowson C, Laing R, Barraclough R, Town I, Mulder R, Norris K, Drennan C. The use of the hospital anxiety and depression scale (HADS) in patients with chronic obstructive pulmonary disease: a pilot study. N Z Med J. 2001;114(1141):447–449. [PubMed] [Google Scholar]
- 17.Lewis KE, Annandale JA, Sykes RN, Hurlin C, Owen C, Harrison NK. Prevalence of anxiety and depression in patients with severe COPD: similar high levels with and without LTOT. COPD. 2007;4(4):305–312. doi: 10.1080/15412550701595716. [DOI] [PubMed] [Google Scholar]
- 18.Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007;167(1):60–67. doi: 10.1001/archinte.167.1.60. [DOI] [PubMed] [Google Scholar]
- 19.Lou P, Zhu Y, Chen P, Zhang P, Yu J, Zhang N, Chen N, Zhang L, Wu H, Zhao J. Prevalence and correlations with depression, anxiety, and other features in outpatients with chronic obstructive pulmonary disease in China: a cross-sectional case control study. BMC Pulm Med. 2012;12:53. doi: 10.1186/1471-2466-12-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Global Initiative for Chronic Obstructive Lung Disease . Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2017. [Google Scholar]
- 21.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 22.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 23.McKenzie DK, Frith PA, Burdon JG, Town GI. The COPDX plan: Australian and New Zealand guidelines for the management of chronic obstructive pulmonary disease 2003. Med J Aust. 2003;178(Suppl):S7–S39. doi: 10.5694/j.1326-5377.2003.tb05213.x. [DOI] [PubMed] [Google Scholar]
- 24.Coventry PA, Bower P, Keyworth C, Kenning C, Knopp J, Garrett C, Hind D, Malpass A, Dickens C. The effect of complex interventions on depression and anxiety in chronic obstructive pulmonary disease: systematic review and meta-analysis. PLoS One. 2013;8(4):e60532. doi: 10.1371/journal.pone.0060532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maurer J, Rebbapragada V, Borson S, Goldstein R, Kunik ME, Yohannes AM, Hanania NA. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008;134(4 Suppl):43S–56S. doi: 10.1378/chest.08-0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang Q, Liao J, Liao X, Wu X, Wan M, Wang C, Ma Q. Disease knowledge level is a noteworthy risk factor of anxiety and depression in patients with chronic obstructive pulmonary disease: a cross-sectional study. BMC Pulm Med. 2014;14:92. doi: 10.1186/1471-2466-14-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Janssen DJ, Spruit MA, Leue C, Gijsen C, Hameleers H, Schols JM, Wouters EF. Symptoms of anxiety and depression in COPD patients entering pulmonary rehabilitation. Chron Respir Dis. 2010;7(3):147–157. doi: 10.1177/1479972310369285. [DOI] [PubMed] [Google Scholar]
- 28.Wacker ME, Jorres RA, Karch A, Wilke S, Heinrich J, Karrasch S, Koch A, Schulz H, Watz H, Leidl R, et al. Assessing health-related quality of life in COPD: comparing generic and disease-specific instruments with focus on comorbidities. BMC PULM MED. 2016;16(1):70. doi: 10.1186/s12890-016-0238-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phillips MR, Zhang J, Shi Q, Song Z, Ding Z, Pang S, Li X, Zhang Y, Wang Z. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey. Lancet. 2009;373(9680):2041–2053. doi: 10.1016/S0140-6736(09)60660-7. [DOI] [PubMed] [Google Scholar]
- 30.Chen Y, Bennett D, Clarke R, Guo Y, Yu C, Bian Z, Ma L, Huang Y, Sun Q, Zhang N, et al. Patterns and correlates of major depression in Chinese adults: a cross-sectional study of 0.5 million men and women. Psychol Med. 2017;47(5):958–970. doi: 10.1017/S0033291716002889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Racic M, Todorovic R, Ivkovic N, Masic S, Joksimovic B, Kulic M. Self- perceived stress in relation to anxiety, depression and health-related quality of life among health professions students: a cross-sectional study from Bosnia and Herzegovina. Zdr Varst. 2017;56(4):251–259. doi: 10.1515/sjph-2017-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El FA, Bentata Y, Ada N, Oneib B. Depression and anxiety disorders in chronic hemodialysis patients and their quality of life: a cross-sectional study about 106 cases in the northeast of Morocco. Saudi J Kidney Dis Transpl. 2017;28(2):341–348. doi: 10.4103/1319-2442.202785. [DOI] [PubMed] [Google Scholar]
- 33.Guo X, Meng Z, Huang G, Fan J, Zhou W, Ling W, Jiang J, Long J, Su L. Meta-analysis of the prevalence of anxiety disorders in mainland China from 2000 to 2015. Sci Rep. 2016;6:28033. doi: 10.1038/srep28033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andenaes R. Psychological characteristics of patients with chronic obstructive pulmonary disease: a review. J Psychosom Res. 2005;59(6):427–428. doi: 10.1016/j.jpsychores.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 35.Balcells E, Gea J, Ferrer J, Serra I, Orozco-Levi M, de Batlle J, Rodriguez E, Benet M, Donaire-Gonzalez D, Anto JM, et al. Factors affecting the relationship between psychological status and quality of life in COPD patients. Health Qual Life Outcomes. 2010;8:108. doi: 10.1186/1477-7525-8-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim KU, Park HK, Jung HY, Ahn JJ, Moon E, Kim YS, Lee MK, Lee H. Association of depression with disease severity in patients with chronic obstructive pulmonary disease. Lung. 2014;192(2):243–249. doi: 10.1007/s00408-013-9547-4. [DOI] [PubMed] [Google Scholar]
- 37.Iguchi A, Senjyu H, Hayashi Y, Kanada R, Iwai S, Honda S, Kitagawa C, Ozawa H, Rikitomi N. Relationship between depression in patients with COPD and the percent of predicted FEV(1), BODE index, and health-related quality of life. Respir Care. 2013;58(2):334–339. doi: 10.4187/respcare.01844. [DOI] [PubMed] [Google Scholar]
- 38.Eisner MD, Blanc PD, Yelin EH, Katz PP, Sanchez G, Iribarren C, Omachi TA. Influence of anxiety on health outcomes in COPD. Thorax. 2010;65(3):229–234. doi: 10.1136/thx.2009.126201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matte DL, Pizzichini MM, Hoepers AT, Diaz AP, Karloh M, Dias M, Pizzichini E. Prevalence of depression in COPD: a systematic review and meta-analysis of controlled studies. Respir Med. 2016;117:154–161. doi: 10.1016/j.rmed.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 40.Willgoss TG, Yohannes AM. Anxiety disorders in patients with COPD: a systematic review. Respir Care. 2013;58(5):858–866. doi: 10.4187/respcare.01862. [DOI] [PubMed] [Google Scholar]
- 41.Laurin C, Lavoie KL, Bacon SL, Dupuis G, Lacoste G, Cartier A, Labrecque M. Sex differences in the prevalence of psychiatric disorders and psychological distress in patients with COPD. Chest. 2007;132(1):148–155. doi: 10.1378/chest.07-0134. [DOI] [PubMed] [Google Scholar]
- 42.Chavannes NH, Huibers MJ, Schermer TR, Hendriks A, van Weel C, Wouters EF, van Schayck CP. Associations of depressive symptoms with gender, body mass index and dyspnea in primary care COPD patients. Fam Pract. 2005;22(6):604–607. doi: 10.1093/fampra/cmi056. [DOI] [PubMed] [Google Scholar]
- 43.Miravitlles M, Molina J, Quintano JA, Campuzano A, Perez J, Roncero C. Factors associated with depression and severe depression in patients with COPD. Respir Med. 2014;108(11):1615–1625. doi: 10.1016/j.rmed.2014.08.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The questionnaire for COPD patients in communities of Pudong District, Shanghai. The questionnaire covered on data of geographic, socioeconomic, lifestyle and occupational exposure factors, and COPD and comorbidities. (PDF 288 kb)
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable requests.


