Abstract
We use surveillance data to describe influenza A and B virus circulation over two consecutive seasons with excess all-cause mortality in Europe, especially in people aged 60 years and older. Influenza A(H3N2) virus dominated in 2016/17 and B/Yamagata in 2017/18. The latter season was prolonged with positivity rates above 50% among sentinel detections for at least 12 weeks. With a current west–east geographical spread, high influenza activity might still be expected in eastern Europe.
Keywords: Europe, influenza, surveillance, epidemiology, severity, mortality, intensive care
The yearly influenza epidemics during each winter season vary in burden and severity. During the 2016/17 and 2017/18 seasons, all-cause excess mortality was observed during periods of high influenza virus circulation [1,2]. Our aim is to describe and compare the pattern of influenza virus circulation and related disease severity by number of patients and fatal cases in intensive care units (ICUs) across European Union/European Economic Area (EU/EEA) countries for the seasons 2016/17 and 2017/18. As influenza circulation progressed from a west to east direction across Europe in 2017/18, a better understanding of the current epidemiological situation might help to prepare countries in the eastern part of the World Health Organization (WHO) European Region for high influenza activity and severity [3].
Influenza surveillance in Europe
The European Influenza Surveillance Network (EISN) performs influenza surveillance from week 40 to week 20 of the following year [4,5]. Weekly epidemiological and virological influenza data are collected from 30 EU/EAA countries and 11 countries report data on severe and fatal cases with laboratory-confirmed influenza in ICUs. Collected data in selected primary care settings include the percentage of these sentinel specimens testing positive for influenza [6].
Influenza virus circulation in the 2016/17 and 2017/18 seasons
The influenza virus positivity rates among sentinel specimens in EU/EEA countries over the 2016/17 and 2017/18 seasons are shown in Figure 1.
Figure 1.
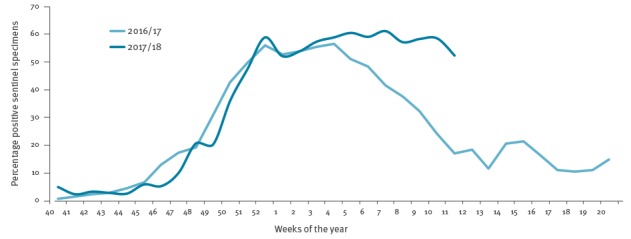
Percentage positivity for influenza viruses among sentinel specimens, by week and season, European Union/European Economic Area, 2016/17 and 2017/18 (up to week 11)
2016/17 seasonal influenza epidemic
Sentinel surveillance outcome
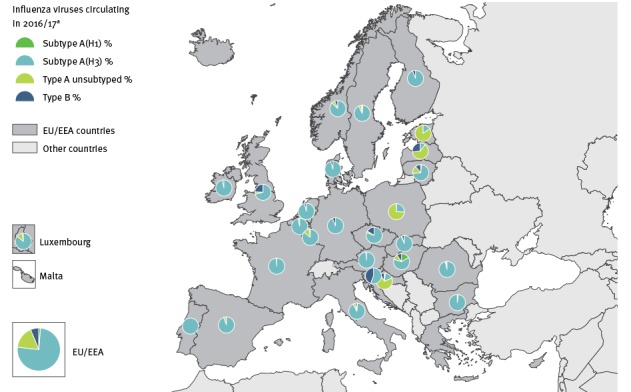
The 2016/17 epidemic was characterised by an early start, with overall sentinel detections crossing the 10% positivity threshold in week 46/2016 (Figure 1) and with a dominance (75%; 10,242/13,584) of influenza A(H3N2) viruses among all positive sentinel specimens, 17% (n = 2,318) influenza A unsubtyped, 1% (n = 172) A(H1N1)pdm09, 2% (n = 281) B no lineage, 1% (n = 117) B/Victoria and 3% (n = 454) B/Yamagata lineage) [7]. Only Slovenia reported a substantial proportion (44%; 113/259) of B/Yamagata viruses in sentinel specimens (Figure 2). The positivity rate in the EU/EEA remained above 10% for 27 consecutive weeks with a dominance of B/Yamagata viruses in the final weeks of the season. The peak phase with positivity levels above 50% (maximum positivity: 57%) lasted for 6 consecutive weeks.
Figure 2.
Distribution of viral types/subtypes in sentinel specimens by country, European Union/European Economic Area, influenza season 2016/17
EU/EEA: European Union/European Economic Area.
a Only sentinel specimens are included.
Results from surveillance in intensive care units
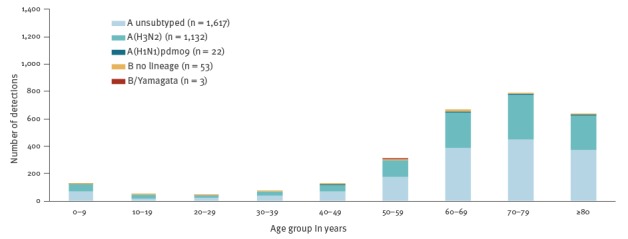
During 2016/17, 10 countries (Czech Republic, Denmark, Finland, France, Ireland, Romania, Slovakia, Spain, Sweden, and the United Kingdom (UK)) reported a total of 3,959 patients admitted to ICUs with laboratory-confirmed influenza (Figure 3). Of these patients, 96% (n = 3,813) were infected with influenza A virus, with 92% (1,465/1,592) of the subtyped A viruses being A(H3N2). The majority of cases (81%; 3,194/3,959) were reported from three countries, namely France (n = 1,469 cases), the UK (n = 1,109) and Spain (n = 616). Most cases in the 2016/17 season occurred up to week 11, by which 97% (3,837/3,959) of all the season’s cases in ICU and 99% (593/599) of all fatal cases had been reported.
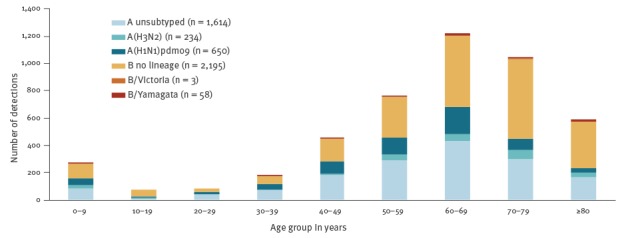
Figure 3.
Distribution of laboratory-confirmed influenza cases admitted to ICU, by age group and type/subtype, in the reporting European Union/European Economic Area countries, 2016/17 season (n = 2,827 patients)a
ICU: intensive care unit.
a Of the total reported 3,959 patients, 2,827 where age information was available are included in the figure.
2017/18 seasonal influenza epidemic
Sentinel surveillance outcome
During the 2017/18 season, the influenza positivity of tested sentinel specimens passed the 10% threshold in week 47 2017, and the 50% threshold in week 52 2017. Positivity rates exceeded 52% for over 12 weeks indicating an unusually protracted peak period of influenza activity across the countries (maximum positivity: 61%; Figure 1). In the previous seven seasons, the number of weeks with a positivity of 50% and higher ranged between 0 (2009/10; 2013/14) and 8 (2012/13; 2015/16) weeks.
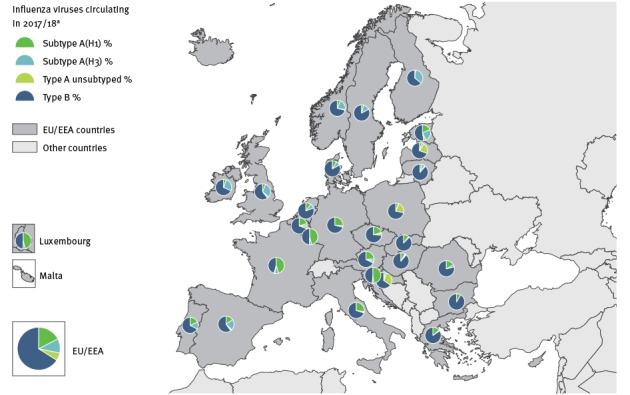
During the initial weeks of the 2017/18 season, similar numbers of influenza A and B viruses were detected in sentinel specimens, but between weeks 48 2017 and 11 2018, influenza B viruses were dominant (66%; 12,455/18,888). Among B viruses with lineage determination, 97% (5,687/5,860) were of the Yamagata lineage. Overall during this period, 6% (n = 1,102) unsubtyped influenza A, 17% (n = 3,283) A(H1N1)pdm09, 11% (n = 2,048) A(H3N2), 35% (n = 6,595) B without lineage determination, 1% (n = 173) B/Victoria and 30% (n = 5,687) B/Yamagata lineage were detected. All countries had a proportion of sentinel B viruses of 46% or higher. Both influenza A(H1N1)pdm09 and A(H3N2) viruses co-circulated with B viruses, but the pattern and magnitude varied across countries. These different patterns are more visible at country-level (Figure 4).
Figure 4.
Distribution of viral types/subtypes in sentinel specimens by country, European Union/European Economic Area, influenza season 2017/18 (up to week 11)
EU/EEA: European Union/European Economic Area.
a Only sentinel specimens are included.
Results from surveillance in intensive care units
Up to week 11 2018, 7,789 laboratory-confirmed influenza cases in ICUs were reported from 10 countries (Czech Republic, Denmark, Finland, France, Ireland, the Netherlands, Romania, Spain, Sweden, and the UK). Altogether, the UK (n = 2,983), France (n = 2,614) and Spain (n = 1,119) reported the vast majority of cases (86%; 6,716/7,789). Comparing data up to week 11 in 2017/18 to the complete 2016/17 season, this is an increase of ICU cases by 169%, 78% and 82% in these countries, respectively (Figure 3, Figure 5).
Figure 5.
Distribution of laboratory-confirmed influenza cases admitted to ICU, by age group and type/subtype, in the reporting European Union/European Economic Area countries, 2017/18 season (up to week 11) (n = 4,754)a
a Of the total reported 7,789 patients, 4,754 where age information was available are included in the figure.
Influenza A was detected in 52% (n = 4,036) of the 7,789 patients, and 59% (n = 872) of the 1,471 subtyped influenza A viruses were reported as A(H1N1)pdm09 with 51% (n = 449) of them reported by France.
The vast majority (81%; 190/234) of all B viruses as well as A(H3N2) viruses were detected in ICU patients aged 50 years and older. The majority (64%; 419/650) of patients infected with A(H1N1)pdm09 were 40 to 69 years-old.
Disease severity in 2016/17 and 2017/18
The severity of disease caused by B viruses during the 2017/18 season is also reflected in the high proportion of B infections among fatal outcomes reported from ICUs (49%; 420/851). This is in contrast with the previous season in which 1% (5/599) of fatal cases in ICUs died of influenza B infection. In 2016/17, 0.5% (3/599) of the fatal cases were infected with A(H1N1)pdm09, 44% (266/599) with A(H3N2) and 54% (325/599) with an unsubtyped influenza A virus. In 2017/18, 15% (124/851) of the fatal cases were infected with A(H1N1)pdm09, 5% (42/851) with A(H3N2) and 31% (265/851) with an unsubtyped influenza A virus.
Among all cases reported with influenza B infection in ICUs and known outcome, 5/52 (10%) died in 2016/17, while 420/1,983 (21%) died in 2017/18. More than 50% (333/636) of all fatal cases over 60 years of age had influenza B and among fatal cases infected with influenza B virus, 79% (333/420) were 60 years of age and older. A similar distribution between virus type and age has been also observed in the B/Yamagata virus dominated season 2012/13.
Discussion
The ongoing 2017/18 influenza season with dominant circulation of influenza B and a co-circulation of A(H1N1)pdm09 and/or A(H3N2) viruses is proving to have a severe impact, as did the 2016/17 season with its dominance of influenza A(H3N2). The dominance of A(H3N2) viruses associated with a high severity, prolonged season and all-cause excess mortality in the EU/EEA in 2016/17 [2] is comparable to the situation in the United States during the 2017/18 season [8]. The dominant B/Yamagata virus circulation with mixed A virus pattern in 2017/18 causing high severity, long duration of peak influenza activity and all-cause excess mortality in the EU/EEA is comparable to 2012/13, an influenza B/Yamagata virus dominated season with A(H1N1)pdm09 and A(H3N2) co-circulation [1,2,9,10]. Influenza A(H3N2) viruses are known to affect disproportionately those aged above 65 years, leading to outbreaks in long-term care homes, increases in hospitalisation and mortality in this age group [11,12]. B viruses are described as causing milder disease and affecting more the younger age groups [13]. In both seasons described here, however, we observed the highest number of severe cases in patients admitted to ICUs aged 60 years and older. As seen previously, patients infected with A(H1N1)pdm09 in ICU were slightly younger than patients infected with influenza A(H3N2) or B [14,15].
The reason for the prolonged and increased activity as well as the severe clinical impact of influenza B viruses during the 2017/18 season is not fully understood. Countries perform either sentinel or universal hospital surveillance and no major change in reporting has occurred which would explain the increase of cases in ICU [16].
Although the most commonly used trivalent vaccine contained the B/Victoria lineage in both 2016/17 and 2017/18 seasons, a moderate vaccine effectiveness for B/Yamagata and A(H1N1)pdm09 in 2017/18 was observed; the effectiveness for A(H3N2) viruses in both seasons, however, was low [12,17]. The moderate and low vaccine effectiveness as well as low vaccine coverage might have contributed to the lower protection in the population together with an accumulation of susceptible people since the last dominant B/Yamagata circulation five seasons ago [18]. Further in-depth analyses are needed to describe the mostly affected population and identify relevant underlying co-morbidities and other factors, e.g. cold weather, that might have contributed to the prolonged virus activity and severity. Neuraminidase inhibitors remain an option for the prophylaxis and treatment of the currently circulating influenza viruses, and their use should be considered along the national and international guidance and recommendations, especially for cases with severe and rapidly progressing disease [19]. The season in Europe has progressed in a marked west–east direction and countries in the eastern part of the WHO European Region should be prepared for possible cases of severe disease and impact on healthcare services. However, influenza activity remains high also in central and western parts of Europe with continuously observed all-cause mortality.
Acknowledgement
We thank the influenza surveillance team at World Health Organization Regional Office for Europe, Copenhagen, Demark, for their collaboration.
We thank all EISN members and ERLI-Net laboratories for their tireless commitment in collecting and providing high-quality European influenza surveillance data.
We are also grateful to the TESSy data managers for their support and ECDC staff for their critical review.
Members of the European Influenza Surveillance Network: WHO: Piers Mook, Tamara Meerhoff; Austria: Theresia Popow-Kraupp, Daniela Schmid; Belgium: Barbezange Cyril, Bossuyt Nathalie, Moreels Sarah, Thomas Isabelle, Van Casteren Viviane; Bulgaria: Korsun Neli; Croatia: Draženović Vladimir; Cyprus: Koliou Maria, Pieridou Despo; Czech Republic: Havlíčková Martina, Jiřincová Helena, Kynčl Jan, Denmark: Fischer Thea Kølsen, Krause Knudsen Lisbet, Trebbien Ramona; Estonia: Päll Kaie, Sadikova Olga; Finland: Haveri Anu, Ikonen Niina, Lyytikäinen Outi, Murtopuro Satu; France: Behillil Sylvie, Bernard-Stoecklin Sibylle, Blanchon Thierry, Campese Christine, Enouf Vincent, Lina Bruno, Turbelin Clement, Valette Martine, van der Werf Sylvie; Germany: Buda Silke, Dürrwald Ralf; Greece: Kalkouni Ourania, , Mentis Andreas, Papa Anna, Pogka Vasiliki; Hungary: Jankovics István, Molnár Zsuzsanna, Rózsa Mónika; Iceland: Löve Arthur, Sigmundsdóttir Guðrún; Ireland: Connell Jeff, Domegan Lisa, Duffy Margaret, Dunford Linda, O’Donnell Joan; Italy: Bella Antonino, Rizzo Caterina, Simona Puzelli, Maria Rita Castrucci; Latvia: Nikiforova Raina, Pakarna Gatis, Zamjatina Natalija; Liechtenstein: Jamnicki Abegg Marina; Lithuania: Griškevičius Algirdas, Lipnickienė Vilnelė, Muralytė Svajūnė; Luxembourg: Fournier Guillaume, Nguyen Trung; Malta: Barbara Christopher, Maistre Melillo Jackie, Melillo Tanya, Zahra Graziella; The Netherlands: de Lange Marit, Dijkstra Frederika, Donker Ge, Fouchier Ron, Hooiveld Mariette, Marbus Sierk, Meijer Adam, Teirlinck Anne; Norway: Bragstad Karoline, Dudman Susanne Gjeruldsen, Hauge Siri Helene, Hungnes Olav, Tønnessen Ragnhild; Poland: Brydak Lidia, Cieślak Katarzyna, Zielinski Andrzej; Portugal: Figueiredo Augusto Gonçalo, Machado Jorge, Moreira Guiomar Raquel, Nogueira Paulo, Rebelo De Andrade Helena, Rodrigues Ana Paula; Romania: Ivanciuc Alina, Odette Popovici, Popescu Rodica; Slovakia: Staronová Edita, Mikas Ján; Slovenia: Berginc Nataša, Prosenc Katarina, Sočan Maja, Grilc Eva; Spain: Casas Inmaculada, Delgado Sanz Concha, Larrauri Amparo, Marcos María Angeles, Oliva Jesus, Ortiz De Lejarazu Leonardo Raul, Pozo Francisco, Vega Tomas; Sweden: Mia Brytting, AnnaSara Carnahan; United Kingdom: Coyle Peter, Daniels Rodney Stuart, Gunson Rory, Kearns Cathriona, MacLean Alasdair, McCaughey Conall, McMenamin Jim, Moore Catherine, Nugent Christopher, Pebody Richard, Phin Nick, Potts Alison, Reynolds Arlene, Shaw Primrose Louise, Zambon Maria.
Conflict of interest: None declared.
Authors’ contributions: CA: concept, data analysis and manuscript draft; RS: data analysis, manuscript review; AM: data and manuscript review; SI: figure development, data analysis and manuscript approval; PP: data analysis and manuscript review; members of the network provided data, reviewed the analysis and approved the manuscript.
References
- 1.European monitoring of excess mortality for public health action - EuroMOMO. Copenhagen: EuroMOMO. [Accessed 23 Mar 2018]. Available from: http://www.euromomo.eu/index.html
- 2. Vestergaard LS, Nielsen J, Krause TG, Espenhain L, Tersago K, Bustos Sierra N, et al. Excess all-cause and influenza-attributable mortality in Europe, December 2016 to February 2017. Euro Surveill. 2017;22(14):30506. 10.2807/1560-7917.ES.2017.22.14.30506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.European Centre for Disease Prevention and Control (ECDC) and World Health Organization (WHO) Regional Office for Europe. Flu News Europe - Joint ECDC-WHO/Europe weekly influenza update, Archives season 2017-18. Week 11/2018 (12–18 March 2018). ECDC/WHO. Available from: http://flunewseurope.org/Archives
- 4. Paget J, Marquet R, Meijer A, van der Velden K. Influenza activity in Europe during eight seasons (1999-2007): an evaluation of the indicators used to measure activity and an assessment of the timing, length and course of peak activity (spread) across Europe. BMC Infect Dis. 2007;7(1):141. 10.1186/1471-2334-7-141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Meijer A, Valette M, Manuguerra JC, Pérez-Breña P, Paget J, Brown C, et al. Implementation of the community network of reference laboratories for human influenza in Europe. J Clin Virol. 2005;34(2):87-96. 10.1016/j.jcv.2005.02.005 [DOI] [PubMed] [Google Scholar]
- 6. Meijer A, Brown C, Hungnes O, Schweiger B, Valette M, van der Werf S, et al. Programme of the Community Network of Reference Laboratories for Human Influenza to improve Influenza Surveillance in Europe. Vaccine. 2006;24(44-46):6717-23. 10.1016/j.vaccine.2006.05.068 [DOI] [PubMed] [Google Scholar]
- 7.European Centre for Disease prevention and Control (ECDC). Risk assessment update: seasonal influenza, EU/EEA, 2016-2017. Stockholm: ECDC; 25 Jan 2017. Available from: https://ecdc.europa.eu/en/publications-data/risk-assessment-update-seasonal-influenza-eueea-2016-2017
- 8. Budd AP, Wentworth DE, Blanton L, Elal AIA, Alabi N, Barnes J, et al. Update: Influenza Activity - United States, October 1, 2017-February 3, 2018. MMWR Morb Mortal Wkly Rep. 2018;67(6):169-79. 10.15585/mmwr.mm6706a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Adlhoch C, Broberg E, Beauté J, Snacken R, Bancroft E, Zucs P, et al. Influenza season 2013/14 has started in Europe with influenza A(H1)pdm09 virus being the most prevalent subtype. Euro Surveill. 2014;19(4):20686. 10.2807/1560-7917.ES2014.19.4.20686 [DOI] [PubMed] [Google Scholar]
- 10.European monitoring of excess mortality for public health action - EuroMoMo. Pooled analyses of all-cause mortality indicates low excess mortality in Europe in the winter of 2013/14, in particular amongst the elderly. 2014. Copenhagen: EuroMOMO. [Accessed 23 Mar 2018]. Available from: http://www.euromomo.eu/methods/pdf/pooled_analyses_winter_2013_14.pdf
- 11. Beauté J, Broberg E, Plata F, Bonmarin I, O Donnell J, Delgado C, et al. Overrepresentation of influenza A(H1N1)pdm09 virus among severe influenza cases in the 2011/12 season in four European countries. Euro Surveill. 2012;17(9):20105. [PubMed] [Google Scholar]
- 12. Pebody R, Warburton F, Ellis J, Andrews N, Potts A, Cottrell S, et al. End-of-season influenza vaccine effectiveness in adults and children, United Kingdom, 2016/17. Euro Surveill. 2017;22(44):17-00306. 10.2807/1560-7917.ES.2017.22.44.17-00306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tran D, Vaudry W, Moore D, Bettinger JA, Halperin SA, Scheifele DW, et al. Hospitalization for Influenza A Versus B. Pediatrics. 2016;138(3):e20154643. 10.1542/peds.2015-4643 [DOI] [PubMed] [Google Scholar]
- 14. Snacken R, Quinten C, Devaux I, Plata F, Broberg E, Zucs P, et al. Surveillance of hospitalised severe cases of influenza A(H1N1)pdm09 and related fatalities in nine EU countries in 2010-2011. Influenza Other Respi Viruses. 2012;6(6):e93-6. 10.1111/j.1750-2659.2012.00406.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Karageorgopoulos DE, Vouloumanou EK, Korbila IP, Kapaskelis A, Falagas ME. Age distribution of cases of 2009 (H1N1) pandemic influenza in comparison with seasonal influenza. PLoS One. 2011;6(7):e21690. 10.1371/journal.pone.0021690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization (WHO) Regional Office for Europe. Influenza surveillance country profiles of WHO European Region Member States 2017. Copenhagen: WHO. [Accessed 12 Feb 2018]. Available from: http://www.euro.who.int/en/health-topics/communicable-diseases/influenza/surveillance-and-lab-network/influenza-surveillance-country-profiles/influenza-surveillance-country-profiles-of-who-european-region-member-states
- 17. Rondy M, Kissling E, Emborg H-D, Gherasim A, Pebody R, Trebbien R, et al. Interim 2017/18 influenza seasonal vaccine effectiveness: combined results from five European studies. Euro Surveill. 2018;23(9):18-00086. 10.2807/1560-7917.ES.2018.23.9.18-00086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.European Centre for Disease Prevention and Control (ECDC). Seasonal influenza vaccination in Europe; Vaccination recommendations and coverage rates in the EU Member States for eight influenza seasons, 2007–2008 to 2014–2015. Stockholm: ECDC; 2017. Available from: https://ecdc.europa.eu/en/publications-data/seasonal-influenza-vaccination-europe-vaccination-recommendations-and-coverage-2007-2015
- 19.European Centre for Disease Prevention and Control (ECDC). Expert Opinion on neuraminidase inhibitors for prevention and treatment of influenza – review of recent systematic reviews and meta-analyses. Stockholm: ECDC; 2017. Available from: https://ecdc.europa.eu/sites/portal/files/documents/Scientific-advice-neuraminidase-inhibitors-2017.pdf


