Abstract
Background
Early presentation is desirable in all cases of acute prolonged chest pain. Causes of delayed presentation vary widely across geographic regions because of different patients' profile and different healthcare capabilities.
Objectives
To detect causes of delay of Non-ST elevation acute coronary syndrome (NSTE-ACS) patients in our country.
Methods
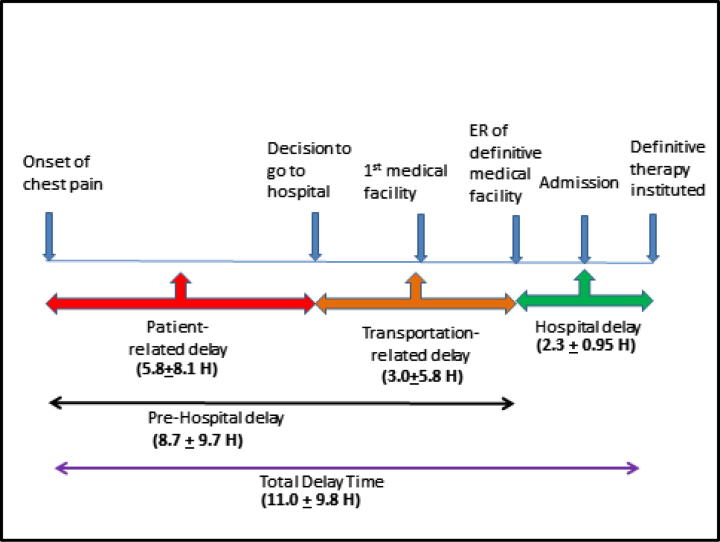
Patients admitted with NSTE-ACS were included. We recorded the time delay between the onsets of acute severe symptoms till their arrival to the hospital (Pre-hospital delay). We also recorded the time delay between the arrival to hospital and the institution of definitive therapy (hospital delay). Causes of pre-hospital delay are either patient- or transportation-related, while hospital delay causes are either staff- or system-related.
Results
We recruited 315 patients, 200 (63.5%) were males, 194 (61.6%) hypertensives, 180 (57.1%) diabetics, 106 (33.7%) current smokers and 196 (62.2%) patients had prior history of cardiac diseases. The mean pre-hospital delay time was 8.7 ± 9.7 h. Sixty-six percent of this time was due to patient-related causes and 34% of pre-hospital delay time was spent in transportation. The mean hospital delay time was 2.3 ± 0.95 h. In 89.8% of cases, the hospital delay was system-related while in 10.2% the reason was staff-related. The mean total delay time to definitive therapy was 11.0 ± 9.8 h.
Conclusion
Pre-hospital delay was mainly patient-related. Hospital delay was mainly related to healthcare resources. Governmental measures to promote ambulance emergency services may reduce the pre-hospital delay, while improving the utilization of healthcare resources may reduce hospital delay.
Keywords: Pre-hospital delay, Hospital delay, NSTE-ACS
1. Introduction
Cardiovascular disease (CVD) is still the leading cause of death among Europeans and worldwide. The Global Burden of Disease study estimated that 29.6% of all deaths worldwide were caused by CVD in 2010, double the number of deaths caused by cancers.1
Non-ST elevation ACS myocardial infarction (NSTE-ACS) and unstable angina (UA) account for about 2.5 million hospital admissions annually worldwide.2
There are variations in the standard of care and quality of practice in different countries secondary to economic and social differences across the world. Indian patients with ACS have a higher rate of STEMI (61%) than do patients in high income countries (15–25%). The median time from symptoms to hospital was 360 min (several times higher than in the US and other high income countries).3 Time is a crucial issue in the management of high-risk acute coronary syndromes. During the last few decades, we have learned that, in the setting of an ACS, time means saved myocardium.4 Recent ESC guidelines indicate that very high-risk patients should be treated within two hours while high-risk patients should be treated within 12 h of hospital presentation.5
There is a paucity of data on the delay in NSTE-ACS treatment in developing countries.
A number of factors are involved in the delay between the onset of ACS and the start of various treatments: patient beliefs, preferences, access to care, family and social support, trust in medical services, transportation, availability of qualified physicians or nurses, availability of medications, catheter lab and consumables.
Pre-Hospital delay is the time from onset of symptoms till arrival to the point of definitive care. In some European countries such as Britain and Sweden, pre-hospital delay times are notably longer than those reported in the United States.1
Hospital delay is defined as the time from arrival to the point of definitive care till the start of guideline determined medical therapy.
The delay in treating ACS varies widely across different countries.6
Given the lack of current data for extent of pre-hospital and hospital delay in our patients with an ACS from different population settings, we decided to study the extent and causes of pre-hospital and hospital delay.7
2. Methods
In this prospective observational study, we recruited 315 hospitalized consecutive NSTE-ACS patients from two University Hospitals. Patients were recruited over the period of 18 months, from August 2013 to February 2015. We excluded patients in outpatient clinic not requiring hospitalization, patients with mental disability and patients unwilling to share personal, social or medical information. The protocol was approved by the institutional ethical committee, in accordance with the ethical standards laid down in the Declaration of Helsinki. All patients signed an informed consent.
2.1. Delay was divided into two major parts
∗Pre-Hospital delay: was defined as the time from onset of symptoms suggestive of ACS till arrival to the point of definitive care; namely hospital emergency department (ED).
The causes of delay were classified into:
-
1.
Patient-related (Decision delay): was defined as the time from onset of symptoms until the patient decided to seek medical help. This delay depends mainly on patient's ideas, beliefs, personality type, socioeconomic status, level of education, marital status, home companions, gender, age, prior illness, family history of ACS, and similar condition in relatives or acquaintances.
-
2.
Transportation-related: was defined as the time between decision to seek medical care and arrival to the ED. It was mainly affected by mode of transport and traffic.
Arbitrary, we further subdivided the prehospital delay into delay > 2 h and < 2 h (we chose the 2 h period as the average period for a patient to reach the first medical facility).
∗Hospital delay: was defined as the time from arrival to the hospital ED till the initiation of guideline-directed therapy namely the loading of dual anti-platelets, heparin, nitroglycerin infusion or GP IIb/IIIa blocker whichever earlier.
The expected causes of hospital delay were classified into
-
1.
Staff-related: failure to diagnose, delayed diagnosis, inertia to treat or technician/nurses-related causes.
-
2.
System-related: unavailable medical devices, lack of supplies, bureaucratic reasons or shortage of beds.
2.2. Data collection
Patients with NSTE-ACS were questioned using standardized questionnaire form.
Patients were asked fixed questions with standard sequence. Questions included social and demographic factors, clinical parameters and risk factors, contextual influences, the acute perception of symptoms, mode of transportation and time of delay from chest pain to start conclusive therapy. Clinical diagnosis was obtained and confirmed by ECG and laboratory results of troponin, CK and CKMB. Time of arrival to ER, time of Admission and time of Heparin/Nitroglycerin/GP IIb-IIIa Blocker therapy were obtained from documented files, nurses and doctors. Diagnosis of NSTE-ACS was made according to the most recent guidelines.8, 9
Data collected included personal data, level of education, working status, social condition and accommodation status, questions about cardiovascular risk factors and prior history of ischemic heart disease.
Other questions focused on description of the current attack of ACS, stressing on the timings of events and causes of delayed response to symptoms and mode of transportation.
The in-hospital delay times were derived from the patient's file.
2.3. Statistical analysis
The sample size was calculated to be 315 patients. The sample size was calculated to achieve a 95% confidence level on a population with characteristics similar to the Brazilian/Argentinian population of the GRACE registry.6 Continuous variables were presented as mean values ± standard deviation. Categorical variables were presented as absolute and relative (%) frequencies. P values of less than 0.05 were considered significant. The analysis of data was done by an SPSS 18.0 program. Comparison of means was done using the independent sample t-test. Chi-square cross tabulation test was used to compare different categorical variables.
3. Results
The characteristics of the included patients are shown in Table 1.
Table 1.
The demographic and social characteristics of patients.
| Demographic and socioeconomic status | Patients with NSTE-ACS (n = 315) |
|---|---|
| Age (yrs.) | |
| (Mean ± SD) | 57.0 ± 9.8 |
| Male gender | 200 (63.5%) |
| Residence | |
| Cairo | 217 (68.9%) |
| Beni Suef | 98 (31.1%) |
| Illiterate | 68 (21.6%) |
| Unemployed | 91 (28.9%) |
| Atherosclerotic risk factors | |
|
194 (61.6%) |
|
180 (57.1%) |
|
106 (33.7%) |
| History of cardiovascular diseases | 196 (62.2%) |
Chest pain started at home in 217 (68.9%) patients but only 14 (4.4%) patients called for an ambulance. The ambulance responded in only 9 patients (2.9%). Eventually, patients went to hospital using their private cars (n = 135, 42.9%), taxi cab (n = 131, 41.6%) or by a public bus (n = 39, 12.4%).
The mean of pre-hospital and hospital delay times is depicted in Fig. 1.
Fig. 1.
A diagram demonstrating the delay times from onset of chest pain till definite therapy. ER; Emergency Room.
Most of our patients first sought medical advice at a university hospital (n = 228, 72.4%) and rest of patients sought first medical help at public hospitals (n = 34, 10.8%), private clinics (n = 35, 11.1%), private hospitals (n = 15, 4.8%) and insurance hospitals (n = 3, 1%). The decision taken at the first medical facility in most of the patients (72.2%) was admission for treatment. Most of the patients had reached the first medical facility later than 2 h (n = 247, 78.1%).
Patients who sought help in more than one medical facility before reaching the destination hospital of definitive medical therapy, showed significantly increased prehospital delay time (p < 0.001), as demonstrated in Table 2.
Table 2.
Prehospital delay times according to the location of first medical help.
| Location of first medical help | No. of patients | Mean prehospital delay ± SD (h) |
|---|---|---|
| University Hospital | 228 | 7.5 ± 9.1 |
| Public Hospital | 34 | 11.6 ± 9.1 |
| Insurance Hospital | 3 | 8.8 ± 1.4 |
| Private Hospital | 15 | 17.3 ± 16.8 |
| Private clinic | 35 | 10.5 ± 8.1 |
Most of the prehospital delay time (66%) was due to patient's related reasons; before deciding to go to hospital. On the other hand in hospital delay, 89.8% of time delay was system-related.
The detailed causes of delay are represented in Table 3.
Table 3.
Causes of prehospital and hospital delay.
| Causes of delay | Frequency number (%) |
|---|---|
| Prehospital delay | |
| *Patient-related reasons | |
| 1. Symptoms related: | |
|
94 (29.8) |
|
50 (15.9) |
|
58 (18.4) |
| 2. Social and system related: | |
|
47 (14.9) |
|
7 (2.2) |
|
18 (5.7) |
|
3 (1) |
|
7 (2.2) |
| *Transportation-related reasons | |
| Traffic and transportation | 283 (89.8) |
| Waiting your turn in the medical facility | 32 (10.2) |
| Hospital Delay | |
| |
|
21 (6.7) |
|
11 (3.5) |
| |
|
77 (24.4) |
|
42 (13.3) |
|
40 (12.7) |
|
119 (37.8) |
|
1 (0.3) |
|
4 (1.3) |
Table 4 demonstrates the difference between patients who came early (<2 h) and those who came late (>2 h).
Table 4.
Profile of patients according to their prehospital delay times.
| Variable | Prehospital delay ⩽ 2 h (n = 68) | Prehospital delay > 2 h (n = 247) | P value |
|---|---|---|---|
| Age (Mean ± SD) | 56.0 ± 9.7 | 57.3 ± 9.8 | 0.3 |
| Sex (male) | 48 (69.6%) | 152 (61.5%) | 0.2 |
| HTN | 39 (56.5%) | 155 (62.7%) | 0.3 |
| DM | 45 (65.2%) | 135 (54.7%) | 0.1 |
| History of IHD | 37 (53.6%) | 159 (64.4%) | 0.1 |
| Current smoker | 25 (36.2%) | 81 (32.8%) | 0.7 |
| Prehospital delay time (h) | 1.6 ± 0.5 | 10.7 ± 10.1 | <0.001 |
| Hospital delay time (h) | 2.1 ± 1.0 | 2.3 ± 0.9 | 0.1 |
| Total delay time (h) | 3.7 ± 1.1 | 13.0 ± 10.2 | <0.001 |
4. Discussion
The burden of cardiovascular disease in our country is quite large and is on the rise. According to the latest WHO data published in 2012, coronary artery disease reached 20.5% of the total deaths in our country; this ranks it as number 23 in the world.10
In the present study, the incidence of NSTE-ACS presenting to our Coronary Care Unit uncovers only the tip of the iceberg.
In NSTE-ACS the myocardial cell injury can occur after 20 min of ischemia. Reducing the time to treatment and maximizing myocardial salvage in keeping with the mantra that “time is muscle” present a logistic challenge.11 So, as time is an important element, this study focuses on causes of pre-hospital and hospital delay in management of patients with NSTE-ACS.
The study showed that only about 1/5 of ACS patients arrived to hospital in less than 2 h after symptom onset. We chose the 2 h limit as it seems a suitable time for instituting medical treatment and saving the myocardium.
In a similar study in Pakistan, 36% of patients arrived before 3 h of symptom onset.12 In Iran 43.2% reached 1–6 h after symptom onset.13 Song has reported a delay of more than 2 h in 55.4% and more than 6 h in 20.3% of patients.14 The median pre-hospital delay in four hospitals in London was 2 h and in five hospitals in USA, this time was 4.25 h.15
The mean prehospital delay in this study was 8.7 h, which is longer than that represented in The GRACE study which showed a median pre-hospital delay time of 4.0 h in Argentina/Brazil, 2.5 h in Australia/New Zealand, 3 h in Europe and 2.7 h in United States/Canada.6
Several factors were associated with longer pre-hospital delay in our patients with NSTE-ACS, including middle age, male gender, unemployed, with medical history of hypertension, previous diagnosis of heart disease and current smokers. These factors have associated with prolonged delay in observational two big studies by GRACE6 and Elbarouni et al.16 who have specifically evaluated the delay times among patients with NSTE-ACS.
The study demonstrates that most of the prehospital delay was related to the time taken by the patient before deciding to go to hospital, which implies the lack of proper medical awareness in the population, while most of the hospital delay was related to problems in the system, speaking of the need to improve our hospital emergency system.
The profile of patients who came early to hospital (prehospital delay <2 h) was quite similar to those who came late (>2 h). Strange enough, patients who came to hospital late, had longer hospital delay time. We don’t have a clear explanation for that; probably late presenters might have had milder symptoms. Another explanation could be physician inertia to start early treatment in patients with delayed presentation.
In summary the prolonged delay times impose risk on myocardial health and this may increase the cost of hospital stay and subsequent drug treatment. All efforts should be directed to reduce these delay times, at least to the international recorded figures. There should be planned educational programs about the alarming symptoms of ACS and the benefits of early seeking medical care. Raising public awareness may help to reduce patient-related prolonged pre-hospital delay times.
We also need Governmental efforts to promote efficient ambulance system services and to set traffic rules to reduce crowding and allow easy and fast hospital access.
4.1. Limitations
The sample size was relatively small in comparison with some other registry studies, recall bias which may distort the patient estimates of exact timing and the fact that only survivors were interviewed, thus factors that influenced delay in individuals who did not survive ACS haven’t been captured.
A larger community based study on the presence of CAD and its risk factors can demonstrate the bigger picture.
Authorship declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors all authors and all authors are in agreement with the manuscript.
Footnotes
Peer review under responsibility of Egyptian Society of Cardiology.
References
- 1.Lozano R., Naghavi M., Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andrikopoulos G., Tzeis S., Mantas I. Epidemiological characteristics and in-hospital management of acute coronary syndrome patients in Greece: results from the TARGET study. Hellenic J Cardiol. 2012;53(1):33–40. [PubMed] [Google Scholar]
- 3.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371(9622):1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 4.Herlitz J., Thuresson M., Svensson L. Factors of importance for patients' decision time in acute coronary syndrome. Int J Cardiol. 2010;141(3):236–242. doi: 10.1016/j.ijcard.2008.11.176. [DOI] [PubMed] [Google Scholar]
- 5.Roffi M., Patrono C., Collet J.P. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2016;37(3):267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg R.J., Spencer F.A., Fox K.A. Prehospital delay in patients with acute coronary syndromes (from the Global Registry of Acute Coronary Events [GRACE]) Am J Cardiol. 2009;103(5):598–603. doi: 10.1016/j.amjcard.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 7.Taha R., Oraby M., Nasr G. Prevalence and causes of failure of receiving thrombolytic therapy in patients with acute ST-segment elevation myocardial infarction. Egypt Hear J. 2013;65(2):51–55. [Google Scholar]
- 8.Steg P.G., James S.K., Atar D. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33(20):2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 9.Hamm Christian W. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 10.WHO country page: <http://www.who.int/countries/egy/en>.
- 11.Bates E.R., Jacobs A.K. Time to treatment in patients with STEMI. N Engl J Med. 2013;369(10):889–892. doi: 10.1056/NEJMp1308772. [DOI] [PubMed] [Google Scholar]
- 12.Khan M.S., Jafary F.H., Faruqui A.M. High prevalence of lack of knowledge of symptoms of acute myocardial infarction in Pakistan and its contribution to delayed presentation to the hospital. BMC Public Health. 2007;7:284. doi: 10.1186/1471-2458-7-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farshidi H., Rahimi S., Abdi A. Factors associated with pre-hospital delay in patients with acute myocardial infarction. Iran Red Crescent Med J. 2013;15(4):312–316. doi: 10.5812/ircmj.2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song L., Yan H.-B., Yang J.-G. Impact of patients’ symptom interpretation on care-seeking behaviors of patients with acute myocardial infarction. Chin Med J (Engl) 2010;123(14):1840–1845. [PubMed] [Google Scholar]
- 15.Banks A.D., Dracup K. Factors associated with prolonged prehospital delay of African Americans with acute myocardial infarction. Am J Crit Care. 2006;15(2):149–157. [PubMed] [Google Scholar]
- 16.Elbarouni B., Goodman S.G., Yan R.T. Impact of delayed presentation on management and outcome of non-ST-elevation acute coronary syndromes. Am Heart J. 2008;156(2):262–268. doi: 10.1016/j.ahj.2008.03.025. [DOI] [PubMed] [Google Scholar]