Abstract
Background
We describe the prevalence of invasive carbapenem-resistant Acinetobacter spp. isolated from 2005 to 2016 in different regions of Switzerland.
Methods
Using the Swiss Antibiotic Resistance Centre (anresis) database that includes data from 70% of all hospitalized patients and one third of all ambulatory practitioners in Switzerland, we analysed the number of carbapenem-susceptible and resistant Acinetobacter spp. isolated from blood or cerebrospinal fluid, and further described their temporal and regional fluctuations.
Results
From 2005 to 2016, 58 cases of resistant or intermediate strains to carbapenem were observed among 632 cases of invasive Acinetobacter. Multivariable analyses indicated that the number of carbapenem-resistant isolates (mean 4.8 ± sd 2.12) and carbapenem resistance rates per region per annum (8.4% ± 13.9%) were low and stable over the studied period. Large fluctuations were observed at the regional level, with e.g. the North East region displaying resistance rates twice as high as that found in other regions.
Conclusion
Despite a relatively stable number of carbapenem-resistant Acinetobacter isolates in Switzerland, our results suggest the existence of a diverse pool of A. baumannii species in hospital settings, and confirm the implication of carbapenem-resistant Acinetobacter calcoaceticus-Acinetobacter baumannii (ACB) complex in the vast majority of clinical infections and nosocomial outbreaks with notable regional fluctuations.
Electronic supplementary material
The online version of this article (10.1186/s12879-018-3061-5) contains supplementary material, which is available to authorized users.
Keywords: Carbapenem resistance, Acinetobacter baumannii complex, Surveillance, Epidemiology, Temporal trends, Regional trends
Background
In the Gram-negative, strictly aerobic Acinetobacter genus, the species that mostly present a risk as opportunistic human pathogens are A. baumannii, A. nosocomialis, A. pittii, A. calcoaceticus, A. seifertii and A. dijkshoorniae, which belong to the so-called Acinetobacter calcoaceticus-Acinetobacter baumannii (ACB) complex. Generally, these four species are not well differentiated at the phenotypic level [1]. They represent the most relevant species clinically, as they may cause serious, difficult-to-treat infections in patients in healthcare settings [1, 2], and are prevalent in the European Union / European Economic Area countries. In contrast, “non-ACB” Acinetobacter species generally present lower pathogenicity and are often found in the environment. Yet, uncommon and opportunistic non-ACB Acinetobacter species, such as A. ursingii, may also cause bloodstream infections [3, 4]. Over the last years, the epidemiological situation has worsened in Europe and worldwide with reports of inter-regional spread and endemic establishment of A. baumannii resistant to carbapenems, a last-line group of β-lactam antibiotics used to treat patients infected with multidrug-resistant Gram-negative bacteria [5–8]. Here we report on the temporal and regional analysis of invasive carbapenem-resistant Acinetobacter isolated in Switzerland from 2005 to 2016.
Methods
Antibiotic susceptibility results (AST) were extracted from the database of the Swiss Antibiotic Resistance Centre (anresis.ch) on 8 June 2017. This database includes all AST results from 20 participating laboratories, representing about 70% of all hospitalized patients and one third of all ambulatory practitioners. The laboratories are geographically spread over all Swiss regions and include private, university and general hospital laboratories. These laboratories send all results from routine testing of clinical bacteriology cultures to the anresis database on a regular basis (weekly or monthly). In contrast to other surveillance systems, all antimicrobial resistance results are sent to the anresis database, not restricting the data either to invasive isolates or to specific microorganisms. To allow for higher comparability with international reports, we therefore used the same approach as in the antibiotic surveillance systems of the ECDC (EARS) and of the WHO-Europe (CASEAR), which restrict their analyses to invasive isolates from blood cultures or cerebrospinal fluid. Duplicate entries were removed and only the first date of occurrence of Acinetobacter isolation in case of re-infected patients was kept for a given year. Isolates from foreign countries were excluded.
We used the interpreted, qualitative data (SIR) delivered by the participating laboratories, as most microbiological laboratories send only qualitative, interpreted resistance data (SIR). SIR data are not validated by anresis.ch but by the laboratories sending the data. All laboratories participating in anresis.ch are approved and participate in at least one external quality program from NEQAS (https://ukneqas.org.uk/) or from the Quality Control Center Switzerland (http://www.cscq.ch). Isolates are classified as susceptible, non-susceptible or intermediate to at least one of imipenem or meropenem following clinical breakpoints of the given years published in the European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines (www.eucast.org) or, according to the Clinical and Laboratory Standards Institute document M31-A3 (CLSI). Most of the participating laboratories switched from CLSI to EUCAST breakpoints between 2011 and 2013.
In addition to SIR data, local laboratories provide accompanying epidemiological information, such as sample location, provider of the sample, patient sex and age-group, but no clinical data about diagnosis, therapy or outcome. Isolate prevalence was modelled via Generalized Poisson regression and resistance rates via logistic regression, with year and regions as explanatory variables. We calculated 95% confidence intervals using robust standard errors for the parameter estimates of the Generalized Poisson regression [9]. Analyses and visualization were done with the R statistical environment (version 3.3.2).
Results
From 2005 to 2016, a total of 800 invasive Acinetobacter isolates were identified in the anresis.ch database, consisting of 707 carbapenem-susceptible and 93 carbapenem-resistant isolates, respectively. After removal of duplicates, 58 resistant or intermediate isolates were identified out of 632 cases (resistance rate 9.2%) over the study period (Table 1). Four out of 58 carbapenem-resistant isolates were isolated from cerebrospinal fluid, the rest from blood cultures. Co-resistance to other antibiotics, such as aminoglycosides (47/55, 86%), trimethoprim-sulfamethoxazole (42/54, 78%) and fluoroquinolones (47/55, 86%), was high, whereas no colistin-resistance was reported for 23 isolates tested. There was a significant increase in the total number of Acinetobacter isolations over time (linear regression, F = 21.56, P < 0.001, R2 = 0.65) with 32.1 isolates per year on average (t = 6.39, P < 0.001), increasing at a yearly rate of 3.2 new isolates (t = 4.64, P < 0.001). When ACB complex species were only considered, there was 18.6 isolates per year on average (t = 5.62, P < 0.001), increasing at 0.98 (t = 2.17, P = 0.055) new isolates per year. The largest number of resistant isolates belonged to the ACB complex (55/299, 18.4%), while resistance rates were much lower in species not belonging to the ACB complex (1/184, 0.5%). For Acinetobacter isolates not typified at species level, 2 out of 149 (1.3%) were carbapenem resistant (Table 1).
Table 1.
Number and taxonomic affiliation of invasive Acinetobacter isolates from 2005 to 2016 in Switzerland
| Taxonomic affiliationa | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Susceptibility rates | ACB complex | Non-ACB complex | Isolates not typified | ||||||||||
| n | S (%) | R (%) |
A. baumannii
A. calcoaceticus A. nosocomialis A. pittii |
A. ursingii | A. lwoffii | A. junii | A. johnsonii | A. haemolyticus | A. radioresistens | A. baylyi | A. parvus | ||
| 2005 | 37 | 34 (91.9) | 3 (8.1) | 2/20 a | 0/0 | 0/9 | 0/0 | 0/0 | 0/1 | 0/0 | 0/0 | 0/0 | 1/4 |
| 2006 | 48 | 44 (91.7) | 4 (8.3) | 4/27 | 0/0 | 0/7 | 0/1 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/9 |
| 2007 | 32 | 32 (100.0) | 0 (0.0) | 0/16 | 0/0 | 0/8 | 0/1 | 0/1 | 0/0 | 0/0 | 0/0 | 0/0 | 0/6 |
| 2008 | 48 | 43 (89.6) | 5 (10.4) | 5/13 | 0/0 | 0/12 | 0/1 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/17 |
| 2009 | 35 | 31 (88.6) | 4 (11.4) | 4/11 | 0/1 | 0/6 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/13 |
| 2010 | 61 | 56 (91.8) | 5 (8.2) | 5/22 | 0/1 | 0/14 | 0/3 | 0/0 | 0/0 | 0/1 | 0/0 | 0/0 | 0/15 |
| 2011 | 53 | 49 (92.5) | 4 (7.5) | 4/23 | 0/4 | 0/5 | 0/1 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/16 |
| 2012 | 53 | 45 (84.9) | 8 (15.1) | 8/17 | 0/2 | 0/10 | 0/3 | 0/0 | 0/1 | 0/0 | 0/0 | 0/1 | 0/11 |
| 2013 | 54 | 47 (87.0) | 7 (13.0) | 7/16 | 0/4 | 0/9 | 0/1 | 0/1 | 0/1 | 0/2 | 0/0 | 0/0 | 0/13 |
| 2014 | 75 | 69 (92.0) | 6 (8.0) | 6/26 | 0/7 | 0/10 | 0/0 | 0/3 | 0/1 | 0/3 | 0/0 | 0/0 | 0/19 |
| 2015 | 64 | 57 (89.1) | 7 (10.9) | 5/25 | 1/4 | 0/12 | 0/2 | 0/0 | 0/2 | 0/0 | 0/0 | 0/0 | 1/12 |
| 2016 | 72 | 61 (93.8) | 5 ( 6.9) | 5/28 | 0/10 | 0/6 | 0/8 | 0/2 | 0/0 | 0/0 | 0/1 | 0/0 | 0/12 |
| Total | 632 | 574 (90.8) | 58 (9.2) | 55/244 | 1/33 | 0/108 | 0/21 | 0/7 | 0/6 | 0/6 | 0/1 | 0/1 | 2/147 |
aThe first and second numbers correspond to the number of resistant and number of susceptible isolates, respectively. Overall, 485 of 632 (76.7%) of the isolates were characterized at the species level
Generalized Poisson regression of the number of carbapenem-resistant isolates on year (from 2005 to 2016) and across 8 Swiss regions indicated that year has no significant effect on the average of 4.83 (sd 2.13) total Acinetobacter isolates per year or on the number of ACB isolates (average 4.58 sd 2.11), with incident rate ratios [IRR] of 1.00 (95% CI 0.96–1.04, P > 0.050) for both ACB and non-ACB isolates (Additional file 1: Table S1). The North East region, with a total of 24 resistant Acinetobacter (22 of which were ACB) isolations from 2005 to 2016, was significantly above all other regions in terms of number of resistant isolates, e.g. the comparison with Centre East (2 isolates, both ACB) taken as the reference region yielded IRR = 2.00 (1.35–2.98), P < 0.001 (for ACB only, values were IRR = 2.19 (1.46–3.28), P < 0.001). Other regions with 4.9 (sd 2.5) carbapenem-resistant Acinetobacter isolates on average were not significantly different from Centre East (P > 0.05).
Those trends were confirmed when examining resistance rates per year per region (Fig. 1a, b), which reached 8.4% (sd 13.9%) on average, and for ACB isolates 15.4% (sd 26.1%). There was no significant temporal trend in resistance rates (for all Acinetobacter isolates, OR 1.06 (0.98–1.16), P = 0.155; for ACB isolates only, OR 1.08 (0.99–1.19), P = 0.096). Only the North East region (resistance rates for all Acinetobacter isolates of 23.4% sd 22%; for ACB isolates, 32.9% sd 30.7%) had higher rates on average (OR 6.75 (1.88–43.32), P = 0.012; for ACB isolates, 4.95 (1.24–33.3) P = 0.045) than region Center East (resistance rate 4.4% sd 10.8%; for ACB isolates, 11.1% sd 29.6%). Other regions had resistance rates ranging from 1.3 to 13.0% (2.1 to 19.8% for ACB isolates), which were not significantly different from that of Center East (P > 0.05).
Fig. 1.
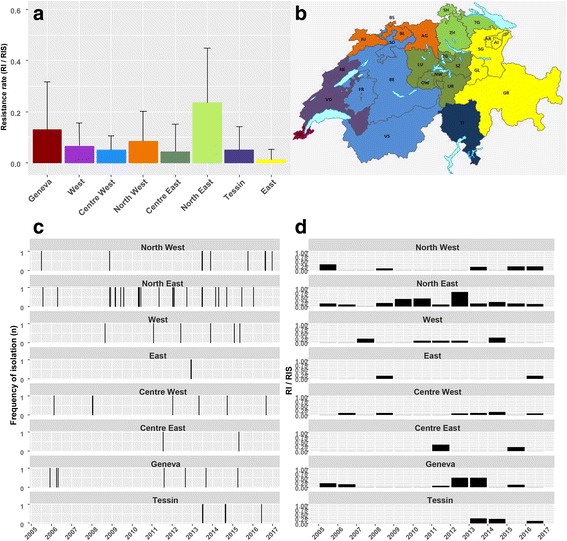
a Acinetobacter resistance rates (number of resistant isolates compared to total number of isolates) per region from 2005 to 2016 in Switzerland. Standard deviation bars represent annual fluctuations per region. b Map of the Swiss regions defined in this study. The original map template, which was made freely available by the Federal Statistical Office (https://www.bfs.admin.ch/bfs/en/home/statistics/regional-statistics/maps.html), was modified by the authors. c Frequency of isolation of resistant Acinetobacter across Swiss regions from 2005 to 2016 (daily resolution). d Acinetobacter resistance rates per year and per region in Switzerland
At a more detailed level of analyses (daily resolution, Fig. 1c; and resistance rate per region per year, Fig. 1d), number of cases and carbapenem-resistance rates associated with Acinetobacter isolates displayed large temporal and regional disparities, both displaying patterns reminiscent of outbreaks: the detailed analysis of the increase in 2010 observed in the North East region was highly suggestive of an outbreak because 5 resistant Acinetobacter isolations, all belonging to ACB, occurred for the whole region within six weeks in the same intensive care unit of burn patients.
We tested the effect of the variation in laboratories contributing to the anresis database on our conclusions by using the data provided by the 14 laboratories that always sent data from 2005 onwards. This sensitivity analyses showed that the number of resistant isolates and resistance rates over year and region did not change qualitatively as compared to the results obtained with the complete dataset (Additional file 1: Table S1): The number of total resistant isolates in the sensitivity analyses did not significantly increase over time and the North East region displayed higher number of isolates than any other region, considering all Acinetobacter isolates or only ACB isolates (Additional file 1: Table S1). Similarly, the sensitivity analysis of the factors affecting resistance rates also confirmed that there was no significant temporal changes for all Acinetobacter isolates and when considering ACB isolates only (the temporal trend was marginally significant for ACB with P = 0.042; Additional file 1: Table S1), and that the North East region had higher rates on average than other regions (resistance rates in the sensitivity analyses ranging from 1.0 to 11.1 and 0 to 24.0% for ACB isolates).
Discussion
A publication by the ECDC of an article entitled “Carbapenem-resistant Acinetobacter baumannii in healthcare settings” [8], concluded that “there has been an overall increase in carbapenem-resistant Acinetobacter baumannii in Europe, especially in countries of lower prevalence.” Using the database of the Swiss Antibiotic Resistance Centre (anresis.ch), which includes all AST results representing about 70% of all hospitalized patients and one third of all ambulatory practitioners in Switzerland, we report on the first nationwide surveillance study on invasive carbapenem-resistant Acinetobacter isolated from 2005 to 2016 in Switzerland. Importantly, we observed that the resistance rate has stabilized yearly at 8.4%, with large temporal and regional disparities, but without increase over time.
Our results indicate the existence of a diverse pool of A. baumannii and related species in hospital settings in Switzerland, as also observed in France [10]. We confirmed the implication of carbapenem-resistant ACB complex isolates in the vast majority of clinical infections and nosocomial outbreaks that involved Acinetobacter isolates, as observed previously in Germany over a 5-year period [11]. Our findings were also in agreement with the known higher risk of infection by A. baumannii in burn patients in hospital settings, as already reported in Switzerland [12] and in other countries [13, 14].
The strengths of our study are that analyses were based on data collected regularly and systematically over 10 years, covering a large proportion of hospitalized patients in Switzerland. Limitations of our study include the fact that there are no mandatory Swiss guidelines for antibiotic resistance testing. Yet the Swiss Society of Microbiology encourages the use of EUCAST breakpoints and provides recommendations on their website (http://www.swissmicrobiology.ch). Nevertheless individual laboratories are free to use other guidelines and methods than EUCAST. Although most laboratories initially based their testing on CLSI guidelines, they changed to EUCAST guidelines between 2011 and 2013, with in general an increased use of automated systems over the years. Therefore identification methods may differ between different laboratories. Another limitation is the fact that clinical isolates were classified as “susceptible”, “intermediate”, or “resistant” based on clinical breakpoints. As such, quantitative resistance data are not available for most isolates. This classification indicates the likelihood of a therapeutic success (e.g. dosing, method and route of administration, pharmacokinetic and pharmacodynamics) with a certain antibiotic and thus helps the attending physician to select the best possible treatment. The use of different clinical breakpoints (e.g. EUCAST vs. CLSI) or changing breakpoints over time may therefore influence the results. However with the change from CLSI breakpoints to EUCAST breakpoints (as performed by most of the anresis-laboratories between 2011 and 2013) we would expect a methodology-related increase in resistance rates during this time period, as breakpoints for susceptibility by disc diffusion in EUCAST are higher than in CLSI 2009–2011 (imipenem ≥23 vs. ≥16, meropenem ≥21 vs. ≥16, respectively; [15]). This consideration strengthens further our conclusion that carbapenem resistance in Acinetobacter did not increase over time in Switzerland.
Conclusions
Our analyses which cover both multiple years and multiple regions conjointly highlight the usefulness of surveillance approaches that integrate different temporal and spatial resolution levels. Therefore, further surveillance efforts are needed to detect and control Acinetobacter outbreaks, and to limit the endemic establishment of resistant isolates in additional health facilities and across EU regions.
Additional file
Table S1. Sensitivity analyses of temporal and regional trends in Acinetobacter and in ACB (number of isolates, resistance rates). We compared the effects of year and region on the number of resistant isolates and on resistant rates by considering data sent either by all laboratories or by laboratories that regularly sent data since 2005. (DOCX 22 kb)
Acknowledgements
We thank all microbiology laboratories participating in the anresis.ch network: Institute for Laboratory Medicine, Cantonal Hospital Aarau; Central Laboratory, Microbiology Section, Cantonal Hospital Baden; Clinical Microbiology, University Hospital, Basel; Viollier AG, Basel; Laboratory Medicine EOLAB, Department of Microbiology, Bellinzona; Institute for Infectious Diseases, University Bern; Microbiology Laboratory, Unilabs, Coppet; Central Laboratory, Cantonal Hospital Graubünden; Microbiology Laboratory, Hospital Thurgau; Microbiology Laboratory Hôpital Fribourgeois, Fribourg; Bacteriology Laboratory, Geneva University Hospitals, Geneva; ADMED Microbiology, La Chaux-de-Fonds; Institute for Microbiology, Université de Lausanne; Centre for Laboratory Medicine, Cantonal Hospital Luzern; Centre for Laboratory Medicine, Cantonal Hospital Schaffhausen;Centre for Laboratory Medicine Dr. Risch, Schaan; Central Institute, Hôpitaux Valaisans (ICHV), Sitten; Centre for Laboratory Medicine St. Gallen; Institute for Medical Microbiology, University Hospital Zürich; Laboratory for Infectious Diseases, University Children’s Hospital Zürich.
The Swiss Centre for Antibiotic Resistance (ANRESIS):
A. Burnens, Synlab Suisse, Switzerland; A. Cherkaoui, Bacteriology Laboratory, Geneva University Hospitals, Switzerland; O. Dubuis, Viollier AG, Basel, Switzerland; A. Egli, Clinical Microbiology, University Hospital Basel, Switzerland; V. Gaia, Department of microbiology, EOLAB, Bellinzona, Switzerland; D. Koch, Federal Office of Public Health, Bern, Switzerland; A. Kronenberg, Institute for Infectious Diseases, University of Bern, Switzerland; S. L. Leib, Institute for Infectious Diseases, University of Bern, Switzerland; P. Nordmann, Molecular and Medical Microbioloy, Department of Medicine, University Fribourg, Switzerland; V. Perreten, Institute of Veterinary Bacteriology, University of Bern, Switzerland; J.-C. Piffaretti, Interlifescience, Massagno, Switzerland; G. Prod’hom, Institute of Microbiology, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland; J. Schrenzel, Bacteriology Laboratory, Geneva University Hospitals, Geneva, Switzerland; A. F. Widmer, Division of Infectious Diseases & Hospital Epidemiology, University of Basel, Switzerland; G. Zanetti, Service of Hospital Preventive Medicine, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland; R. Zbinden, Institute of Medical Microbiology, University of Zürich, Switzerland.
A Burnens (andre.burnens@synlab.com); AF Widmer (awidmer@uhbs.ch); A. Cherkaoui (Abdessalam.Cherkaoui@hcuge.ch); C. Corradi (Corinne.Corradi@bag.admin.ch); D. Koch (daniel.koch@bag.admin.ch); A. Egli (Adrian.Egli@usb.ch); G Zanetti (Giorgio.Zanetti@unil.ch); G Prod’hom (Guy.Prodhom@chuv.ch); J Schrenzel (Jacques.Schrenzel@hcuge.ch); J Marschall (jonas.marschall@insel.ch); O Dubuis (olivier.dubuis@viollier.ch); P Nordmann (patrice.nordmann@unifr.ch); V Perreten (vincent.perreten@vetsuisse.unibe.ch); JC Piffaretti (piffaretti@interlifescience.ch); R Zbinden (rzbinden@imm.uzh.ch); S Leib (stephen.leib@ifik.unibe.ch); V Gaia (Valeria.Gaia@eoc.ch).
Funding
The anresis.ch database is funded by the Swiss Federal Office of Public Health. The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The data that support the findings of this study are available from anresis.ch (http://www.anresis.ch/), and interactive tables presenting aggregated data are available at http://www.anresis.ch/index.php/Interactive-database.html. Access to raw data is, however, restricted and should be requested to the anresis.ch steering committee.
Abbreviations
- ACB
Acinetobacter calcoaceticus-Acinetobacter baumannii
- AST
Antibiotic susceptibility test
- CI
Confidence interval
- IRR
Incident rate ratio
- OR
Odds ratio
- sd
Standard deviation
Authors’ contributions
All authors conceived and designed the study. AR analysed and interpreted the data, and wrote the manuscript; AK coordinated anresis.ch, provided access to hospital network, interpreted the results, and reviewed the clinical content of the manuscript. All authors have read and approved the manuscript.
Ethics approval and consent to participate
Analysis and publication of the data presented in the study were done in agreement with the steering committee of the Swiss Centre for Antibiotic Resistance (ANRESIS).
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12879-018-3061-5) contains supplementary material, which is available to authorized users.
Contributor Information
A. Ramette, Phone: +41 31 632 9540, Email: alban.ramette@ifik.unibe.ch
A. Kronenberg, Email: andreas.kronenberg@ifik.unibe.ch
and the Swiss Centre for Antibiotic Resistance (ANRESIS):
A. Burnens, A. Cherkaoui, O. Dubuis, A. Egli, V. Gaia, D. Koch, A. Kronenberg, S. L. Leib, P. Nordmann, V. Perreten, J.-C. Piffaretti, G. Prod’Hom, J. Schrenzel, A. F. Widmer, G. Zanetti, and R. Zbinden
References
- 1.Nemec A, Krizova L, Maixnerova M, van der Reijden TJ, Deschaght P, Passet V, et al. Genotypic and phenotypic characterization of the Acinetobacter calcoaceticus-Acinetobacter baumannii complex with the proposal of Acinetobacter pittii sp. nov. (formerly Acinetobacter genomic species 3) and Acinetobacter nosocomialis sp. nov. (formerly Acinetobacter genomic species 13TU) Res Microbiol. 2011;162(4):393–404. doi: 10.1016/j.resmic.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Peleg AY, Seifert H, Paterson DL. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev. 2008;21(3):538–582. doi: 10.1128/CMR.00058-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yakut N, Kepenekli EK, Karaaslan A, Atici S, Akkoc G, Demir SO, et al. Bacteremia due to Acinetobacter ursingii in infants: reports of two cases. Pan Afr Med J. 2016;23:193. doi: 10.11604/pamj.2016.23.193.8545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sieswerda E, Schade RP, Bosch T, de Vries J, Chamuleau MED, Haarman EG, et al. Emergence of carbapenemase-producing Acinetobacter ursingii in the Netherlands. Clin Microbiol Infect. 2017;23(10):779–781. doi: 10.1016/j.cmi.2017.04.024. [DOI] [PubMed] [Google Scholar]
- 5.Doi Y, Murray GL, Peleg AY. Acinetobacter baumannii: evolution of antimicrobial resistance-treatment options. Semin Respir Crit Care Med. 2015;36(1):85–98. doi: 10.1055/s-0034-1398388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Higgins PG, Dammhayn C, Hackel M, Seifert H. Global spread of carbapenem-resistant Acinetobacter baumannii. J Antimicrob Chemother. 2010;65(2):233–238. doi: 10.1093/jac/dkp428. [DOI] [PubMed] [Google Scholar]
- 7.Kim DH, Choi JY, Kim HW, Kim SH, Chung DR, Peck KR, et al. Spread of carbapenem-resistant Acinetobacter baumannii global clone 2 in Asia and AbaR-type resistance islands. Antimicrob Agents Chemother. 2013;57(11):5239–5246. doi: 10.1128/AAC.00633-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anonymous. European Centre for Disease Prevention and Control . Rapid risk assessment: Carbapenem-resistant Acinetobacter baumannii in healthcare settings. 2016. pp. 1–14. [Google Scholar]
- 9.Cameron AC, Trivedi PK. Microeconometrics using Stata. College Station: Stata Press; 2009. [Google Scholar]
- 10.Hauck Y, Soler C, Jault P, Merens A, Gerome P, Nab CM, et al. Diversity of Acinetobacter baumannii in four French military hospitals, as assessed by multiple locus variable number of tandem repeats analysis. PLoS One. 2012;7(9):e44597. doi: 10.1371/journal.pone.0044597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schleicher X, Higgins PG, Wisplinghoff H, Korber-Irrgang B, Kresken M, Seifert H. Molecular epidemiology of Acinetobacter baumannii and Acinetobacter nosocomialis in Germany over a 5-year period (2005-2009) Clin Microbiol Infect. 2013;19(8):737–742. doi: 10.1111/1469-0691.12026. [DOI] [PubMed] [Google Scholar]
- 12.Zanetti G, Blanc DS, Federli I, Raffoul W, Petignat C, Maravic P, et al. Importation of Acinetobacter baumannii into a burn unit: a recurrent outbreak of infection associated with widespread environmental contamination. Infect Control Hosp Epidemiol. 2007;28(6):723–725. doi: 10.1086/517956. [DOI] [PubMed] [Google Scholar]
- 13.Mahdian S, Sadeghifard N, Pakzad I, Ghanbari F, Soroush S, Azimi L, et al. Acinetobacter baumannii clonal lineages I and II harboring different carbapenem-hydrolyzing-beta-lactamase genes are widespread among hospitalized burn patients in Tehran. J Infect Public Health. 2015;8(6):533–542. doi: 10.1016/j.jiph.2015.04.030. [DOI] [PubMed] [Google Scholar]
- 14.Sarhaddi N, Soleimanpour S, Farsiani H, Mosavat A, Dolatabadi S, Salimizand H, et al. Elevated prevalence of multidrug-resistant Acinetobacter baumannii with extensive genetic diversity in the largest burn Centre of Northeast Iran. J Glob Antimicrob Resist. 2016;8:60–66. doi: 10.1016/j.jgar.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 15.Hombach M, Bloemberg GV, Bottger EC. Effects of clinical breakpoint changes in CLSI guidelines 2010/2011 and EUCAST guidelines 2011 on antibiotic susceptibility test reporting of gram-negative bacilli. J Antimicrob Chemother. 2012;67(3):622–632. doi: 10.1093/jac/dkr524. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Sensitivity analyses of temporal and regional trends in Acinetobacter and in ACB (number of isolates, resistance rates). We compared the effects of year and region on the number of resistant isolates and on resistant rates by considering data sent either by all laboratories or by laboratories that regularly sent data since 2005. (DOCX 22 kb)
Data Availability Statement
The data that support the findings of this study are available from anresis.ch (http://www.anresis.ch/), and interactive tables presenting aggregated data are available at http://www.anresis.ch/index.php/Interactive-database.html. Access to raw data is, however, restricted and should be requested to the anresis.ch steering committee.


