Abstract
Objective
The purpose of this study was to investigate correlative factors affecting chronic low back pain (CLBP), with special emphasis on the radiographic postural findings in the sagittal lumbosacral spine.
Methods
A cross-sectional study alongside a randomized trial was conducted. Standing lateral lumbar spine radiographs from 352 patients with CLBP enrolled in a randomized trial were analyzed and radiographic mensuration of lumbar lordosis, lumbosacral disc angle, and sacral inclination performed. These angles were correlated with baseline variables, including CLBP intensity, age, and sex. Multiple polynomial regressions were performed in which CLBP intensity was regressed on linear and quadratic terms of lumbar lordosis to investigate the possibility of greater pain with hypo- and/or hyperlordosis.
Results
There was no significant correlation of the angles with pain and age (r ≤ 0.09, P > .05). Weak but statistically significant correlation was identified between all 3 measurements and sex (r = –0.12 to 0.21, P < .05). Greater pain was not noted for hypo- and hyperlordosis; regression coefficients for the linear and quadratic effects were approximately 0 (P > .05).
Conclusion
This study determined that there was no correlation between lumbar lordosis and pain levels for people with CLBP; thus, use of lumbar spine radiographic mensuration in the management of pain for people with CLBP is not recommended.
Key Indexing Terms: Low Back Pain, Posture, Lordosis, Radiography
Introduction
Low back pain (LBP) is considered the single leading cause of professional and social disability worldwide.1 At least 70% of the population experiences low back pain at least once during their lifetime.2 Despite its socioeconomic impact and high prevalence,3 the etiology and understanding of the disease remain relatively enigmatic. Changes in the lumbar lordosis have been debated as a correlating factor in the production of LBP, with previous studies finding varying results.4, 5, 6, 7 Despite the differing conclusions regarding sagittal alignment of the lumbar spine and its association with LBP, clinicians continue to assess the lordosis and consider their findings when creating a treatment plan.
Historically, clinicians have noted a relationship between aberrations of lumbar spine posture and the development of low back pain.8 Abnormal posture causes straining of the highly innervated soft tissues, with tightening of the static postural muscles and weakening of dynamic musculature, thus indirectly altering the lumbar lordosis.9 Additionally, these habitual postural abnormalities lead to excessive shearing of the joints and eventually degeneration of the articular surfaces.8 Based on these findings, it has been speculated that deviation away from the “normal” lumbar lordosis plays a role in the production of low back pain.4 Consequently, the significance of radiographic mensuration of the lumbosacral spine used in practice requires further evaluation to see if it warrants a place in clinical practice.
In addition to aberrant posture, many factors have been suggested to play a role in the sagittal alignment of the lumbar spine. It has been proposed by previous authors that differences of the lordotic curve, as well as other sagittal lumbosacral measurements, including sacral inclination and the lumbosacral disc angle, may correlate with sex and age.5, 10, 11, 12 It is important to examine the effects of these particular factors as they partake in the patient-specific treatment.
Currently there is no general consensus on whether or not there is a relationship between low back pain and the sagittal lordosis of the lumbar spine.4, 5, 6, 7 The inconsistency of the findings could be due to error introduced by radiographic technique and mensuration as well as the sample participants. In addition, studies use a variety of methods to measure lordosis (eg, radiographs and flexible rulers), which may contribute to inconsistency. If radiographs are used, different techniques are used to measure lordosis. Furthermore, participants vary from study to study in sample size, sex, and age, all of which leave room for differences of findings. Studies with small sample sizes have been conducted with varied results.4, 6, 7, 12, 13 Hence, there has been a need to reevaluate the relationship between pain and posture using a larger sample size. The failure to agree suggests the need for further studies to investigate the relationship between low back pain and lordosis. Because clinicians continue to evaluate lumbar lordosis and other associated angles when forming a treatment plan for their patients, it is essential that their clinical significance, if any, be examined. The presence or absence of a correlation with pain will give preliminary evidence on the viability of the use of radiographic mensuration for the care of chronic LBP (CLBP).
The purpose of this study was to evaluate correlation between radiographic postural findings in the sagittal lumbosacral spine, including lumbar lordosis, lumbosacral disc angle, and sacral inclination posture and pain intensity for people with CLBP. The primary hypothesis was that the 3 angles are correlated with CLBP intensity, age, and sex, with emphasis on the relationship between lumbar lordosis and CLBP. A secondary hypothesis was a quadratic association between LBP and lumbar lordosis, such that greater pain would be noted at the higher and lower ends of the lordosis range.
Methods
Design
This was a secondary analysis utilizing baseline data and lumbar spine radiographs from a National Institutes of Health–funded randomized controlled trial by Haas et al14 using a cross-sectional design. The correlation of sagittal plane lumbosacral angles with participant characteristics was explored.
Participants
The study included 352 of the 400 original participants. They were required to have a current history of at least 3 consecutive months of nonspecific CLBP of mechanical origin. Participants were required to be at least 18 years old and required to have had some LBP on 30 days in the prior 6 weeks and a minimum LBP index of 25 on a 100-point scale to prevent floor effects. Participants were excluded if they received manual therapy within the previous 90 days, or for contraindications to study interventions and complicating conditions such as active cancer, spinal pathologic conditions, inflammatory arthropathies, autoimmune disorders, anticoagulant conditions, neurodegenerative diseases, pain radiating below the knee, organic referred pain, pregnancy, and disability compensation.14 Additionally, any participants who had congenital bony anomalies or spondylolisthesis on the radiographs were not included in the study. Furthermore, survey data were unavailable for 15 participants and they were therefore not included in the study. All participants signed a participant information and consent form authorizing later use of the collected data and radiographs. This project was approved by the University of Western States Institutional Review Board.
Outcomes and Baseline Variables
A baseline questionnaire, validated by Jensen et al,15 was completed by the participants during the original study; it included age, sex, and average LBP in the last 4 weeks on a numeric pain rating scale from 0 to 10. The data were collected from the baseline surveys and recorded.
Radiographic Mensuration
Measurements were taken on standing lateral lumbar plain film radiographs, including lumbar lordosis, lumbosacral disc angle, and sacral inclination. Each measurement was made with the use of a Cobb ruler and a radiographic pencil by the author of this study to reduce room for error. Each participant was assigned a study identification number, and at no point was the participant’s legal name included within the data.
To find the lumbar lordosis angle, the 4-line Cobb method was used. This method has high reliability and precision (intraclass correlation = 0.98).16 The lumbar lordosis angle was found by drawing 2 straight lines tangentially to the superior endplate of the first lumbar vertebrae and the inferior endplate of fifth lumbar spine vertebrae. Perpendicular lines were then drawn, and the angle formed by the 2 intersecting lines was measured and documented (Fig 1). The lumbosacral disc angle was measured by drawing 2 lines. The first line was drawn parallel to the inferior endplate of the fifth lumbar spine vertebrae, and the second line was drawn parallel to the superior endplate of the first sacral segment. The anterior angle formed by the intersecting 2 lines was measured and documented (Fig 2).17 Lastly, sacral inclination was measured by drawing 2 lines. First, a tangential line was drawn parallel to and through the posterior margin of the first sacral segment. Then a vertical line was drawn intersecting the tangential sacral line, and the angle formed was measured and reported (Fig 3).17
Fig 1.
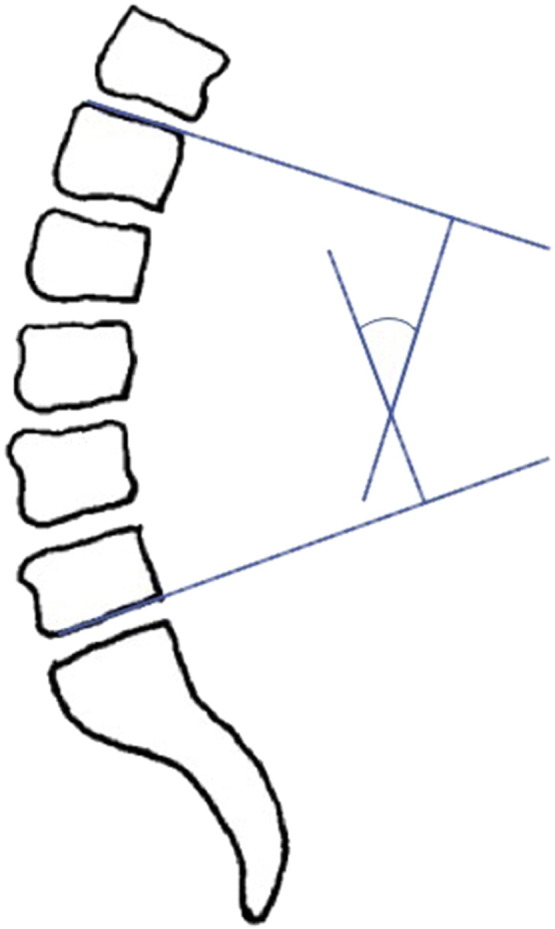
Lumbar lordosis.
Fig 2.
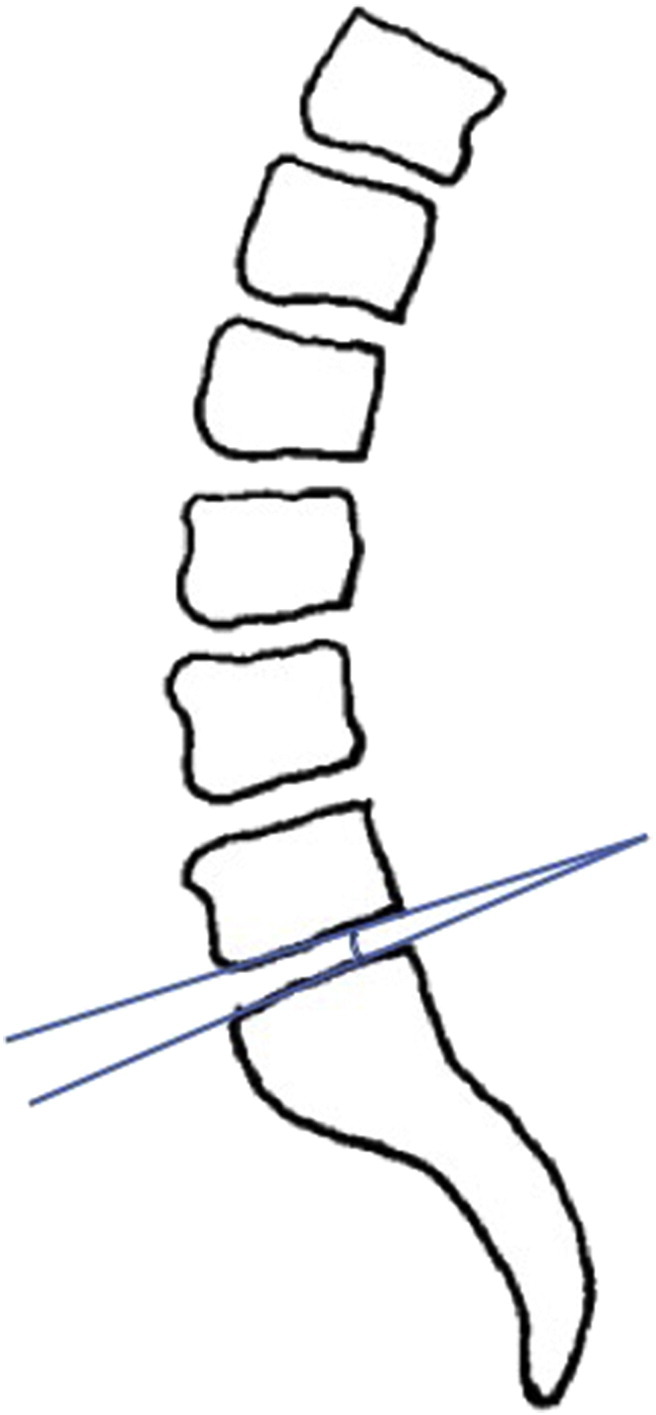
Lumbosacral disc angle.
Fig 3.
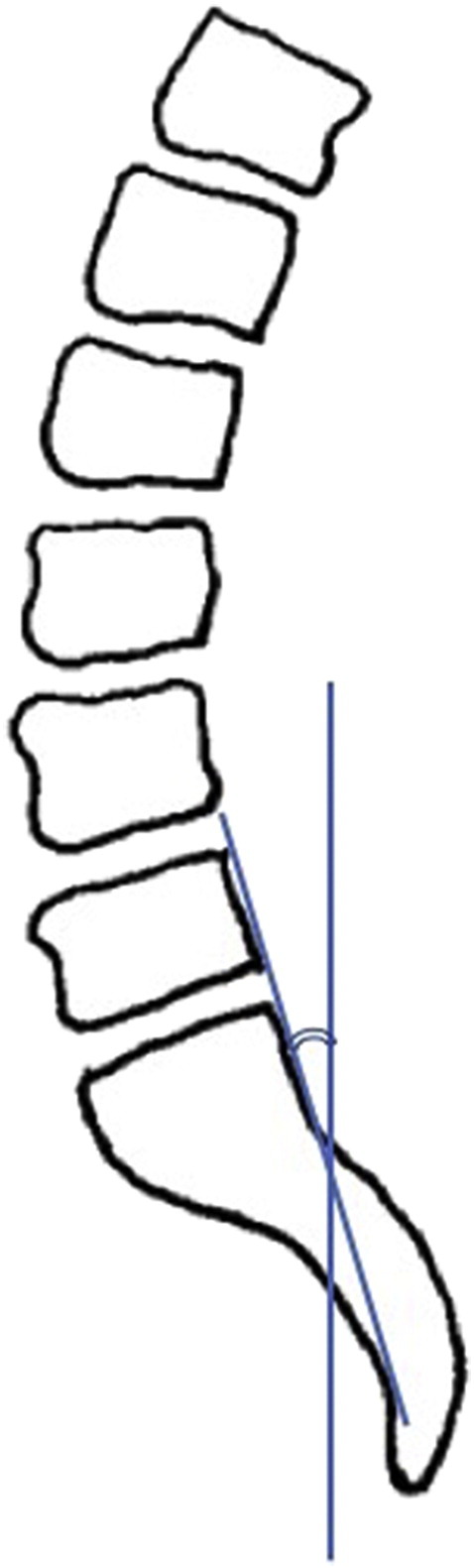
Sacral inclination.
Statistical Analysis
Using Pearson correlation coefficients, the correlation between each of the 3 radiographic angles (lumbar lordosis, lumbosacral disc angle, and sacral inclination) and each of the baseline variables (average CLBP, age, and sex) was calculated. Additionally, a linear regression analysis was conducted to evaluate the relationship of hypolordosis and hyperlordosis with chronic LBP. Low back pain was regressed on linear and quadratic terms for lumbar lordosis in a single model. A significant quadratic term would indicate increased pain with hypolordosis and hyperlordosis. Statistical significance was set at α = .05. All analysis was conducted using Microsoft Excel 2010 (Microsoft, Redmond, Washington).
Results
Participant Characteristics
In a sample of 352 participants with at least 3 months of CLBP, there were 166 women (47%) and 186 men (53%). Their ages ranged from 18 to 81 with a mean age of 41.5 years (Table 1). The mean LBP intensity was 4.7 out of 10 (standard deviation = 1.7).
Table 1.
Values Are Mean (Standard Deviation) or Number (Percentage) of Age, Women, Average CLBP, Lumbar Lordosis Angle, Sacral Inclination Angle, and Lumbosacral Disc Angle
| Variable | Mean | Standard Deviation |
|---|---|---|
| Age | 41.5 | 14.1 |
| Women | 166 (47%) | |
| Average numeric pain score (out of 10) | 4.1 | 1.7 |
| Lumbar lordosis angle (degrees) | 43.3 | 11.0 |
| Sacral inclination angle (degrees) | 52.7 | 7.8 |
| Lumbosacral disc angle (degrees) | 14.5 | 5.0 |
CLBP, chronic low back pain.
Lumbar Lordosis Angle
The range of lordosis was between 5° and 78° with a mean of 43.3 ± 11.0° (Table 1). The lordosis correlated poorly with average CLBP (r = 0.09) and was determined to not be statistically significant (P = .175) (Table 2). No notable linear or quadratic trends in chronic LBP were identified for the lordosis angle (regression coefficients equaled approximately zero). Furthermore, there was no significant correlation identified between lordosis angle and age (r = –0.01, P = .652). However, a weak but statistically significant correlation between the lumbar lordosis angle and sex (r = –0.12, P = .026) was revealed. The mean lumbar lordosis identified in men was 2.6° less than that of women.
Table 2.
Correlation Coefficients and P Values Among Lumbar Lordosis Angle, Sacral Inclination Angle, Lumbosacral Disc Angle and Average CLBP, Age, and Sex
| Angle | Average CLBP, r (P Value) | Age, r (P Value) | Sex, r (P Value) |
|---|---|---|---|
| Lumbar lordosis angle | 0.09 (.175) | –0.01 (.652) | –0.12 (.026) |
| Sacral inclination angle | 0.09 (.204) | –0.05 (.110) | –0.15 (.005) |
| Lumbosacral disc angle | –0.04 (.378) | 0.01 (.941) | 0.21 (<.001) |
CLBP, chronic low back pain.
Sacral Inclination Angle
Sacral inclination angles had a wide range from 18.5° to 77° with an average of 52.7 ± 7.8° (Table 1). Statistical analysis with Pearson correlation coefficients identified no statistically significant correlation between sacral inclination and average CLBP (r = 0.09, P = .204) (Table 2). Additionally, there was no significant correlation noted between sacral inclination and age (r = –0.05, P = .110). A weak (r = –0.15) but statistically significant correlation (P = .005) was identified between sacral inclination and sex. Men had a mean sacral inclination 2.3° less than women did.
Lumbosacral Disc Angle
The measurements of lumbosacral disc angle ranged from 3° to 28° with an average of 14.5 ± 5.0° (Table 1). No statistically significant correlation was identified between lumbosacral disc angle and average CLBP (r = –0.04, P = .378) (Table 2). Furthermore, statistical analysis revealed no significant correlation between lumbosacral disc angle and age (r = 0.01, P = .941). However, a weak but statistically significant correlation was identified between lumbosacral disc angle and sex (r = 0.21, P < .001). Men had a mean lumbosacral disc angle 2° higher than women did.
Discussion
With respect to lumbar lordosis and CLBP, prior studies have varied greatly in their results.4, 5, 6, 7 In the present study, no statistically significant correlation was identified between the degree of lumbar lordosis and pain in a CLBP population. Our results agree with Hansson et al,6 who reported no relationship between lumbar lordosis and acute or CLBP. Additionally, in a 2001 study by Nourbakhsh et al,5 no difference was identified between normal participants and symptomatic patients in a study on CLBP. In contrast, Jackson et al7 reported a significantly decreased lumbar lordosis in the CLBP patients. The inconsistency of the findings could be due to a multitude of factors, including variations in sample size, demographic features of the sample population (age, race, and sex), and radiographic measurement technique.
Our statistical analysis identified no significant correlation between the degree of lumbar lordosis and age, which is not consistent with prior research. With respect to increasing age, it has been accepted that a total loss of lordosis occurs. Dreischarf et al10 reported an average 20% loss of lumbar lordosis with aging in their 2014 study on asymptomatic participants. Nourbakhsh et al5 reported a significant loss of lordosis in the group aged 50 to 65 compared with the younger participant groups. However, they also identified no relationship between age and lumbar lordosis in the younger participant groups. Researchers who have reported loss of lordosis with age hypothesize that this is due to a variety of factors, such as osteoporosis, degenerative disc disease, weakening of the abdominal musculature, and overall increased lumbar stiffness.10, 11, 18, 19 The differing results between our study and prior research could be due to the fact that our participants are from a CLBP population lacking a control group, which may be obscuring the results.
The study findings agreed with prior studies that reported a statistically significant correlation between lumbar lordosis and sex. Lang-Tapia et al20 reported, in their study on healthy participants, that the lumbar lordosis in women was 12° more than in men. Janssen et al21 reported that the female sagittal spinopelvic alignment was greatly different from male alignment, with higher dorsally directed shear loads than in the male spine. In 2001, Nourbakhsh et al5 reported that the degree of lumbar lordosis in women is 10° greater than that in men in an LBP study. Although the magnitude of degree difference between men and women was determined to be less in our study, we noted similar results, with women having 2.6° greater lumbar lordosis measurement.
Our results both agree and disagree with prior studies with respect to sacral inclination and lumbosacral disc angle and how they correlate with pain, age, and sex. Evcik et al12 reported that sacral inclination angles increased in patients with CLBP. However, using a line fit plot, our data indicated no such trend, showing no signs of correlation between sacral inclination and pain; however, with respect to sex, Evcik et al12 had similar findings in that women tended to have higher sacral inclination angles. Yet when lumbosacral disc angles were analyzed, our results disagreed with theirs, as we determined that men had higher lumbosacral disc angles. Based on prior research on the trends of sagittal spinopelvic radiographic measurements, similar findings as Evcik et al12 were anticipated. With an increase in lordosis, it should be expected to find an increase in lumbosacral disc angle, as well as sacral inclination.12, 22 Further studies should be considered to examine sex differences and include an asymptomatic control group for comparison between asymptomatic, acute, and CLBP patients.
In regard to clinical application, our results do not support the use of lumbar spine radiograph roentgenometrics for the management of pain for patients with CLBP. These results agree with the current diagnostic imaging practice guidelines of the spine. Bussières et al23 state that in the absence of red flags, radiographs are not initially indicated in patients with subacute (4-12 weeks’ duration) and persistent LBP (>12 weeks’ duration). They concur with the present study stating that generally studies have not identified a significant correlation between lumbar spine posture and LBP. Furthermore, the majority of changes that were noted on the radiographs that may contribute to the pain, such as degenerative changes, do not affect or change the clinical management of the patient.23
Limitations
Errors made in constructing the radiographic measurements may have affected the correlations, thus obscuring potential correlations. Additionally, the radiographs and data were pulled from a randomized trial; thus, no normal “control” group was included in the study for comparison. Without an asymptomatic control group to compare radiographic mensuration values to, it is difficult to truly evaluate if a correlation exists. Furthermore, differences between studies in demographic characteristics such as race, age, and sex, may contribute to variations in results. This study focused on the outcome measures of pain, sex, and age and did not include other measures such as disability or function.
Despite the inconsistencies in the literature, as well as the present study’s collected data, lumbar lordosis continues to be considered when managing patients with low back pain. With this in mind, it is essential that further studies are performed on larger populations that vary in demographic characteristics such as age, sex, race, and economic status to help reveal any potential relationships that the secondary variables may have in a population with low back pain. Additionally, it would be interesting to further investigate to see if a correlation between low back pain and obesity exists. Unfortunately, study participant weight was not available during the present study.
Conclusions
This study determined that there was no correlation between lumbar lordosis and pain levels for people with CLBP. All of the sagittal lumbosacral radiographic measurements correlated poorly with pain and age. However, a weak, but statistically significant trend was identified between all 3 radiographic measurements and sex. Therefore, use of lumbar spine radiographic mensuration in the management of pain for people with CLBP is not recommended.
Funding Sources and Conflicts of Interest
Data were collected as part of a study funded by the National Center for Complementary and Integrative Health, National Institutes of Health (U01 AT001908). The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the official views of the National Center for Complementary and Integrative Health. No conflicts of interests were reported for this study.
Contributorship Information
Concept development (provided idea for the research): S.K.S.
Design (planned the methods to generate the results): S.K.S., M.H.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): M.H.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): S.K.S.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): M.H.
Literature search (performed the literature search): S.K.S.
Writing (responsible for writing a substantive part of the manuscript): S.K.S., M.H.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): S.K.S., M.H.
Practical Applications
-
•
This study adds to prior studies and practice guidelines, which state that the use of radiographs to assess posture in patients with CLBP is not supported.
-
•
In patients with CLBP, the use of radiographs to assess posture will likely not affect patient management or care.
Alt-text: Image 1
References
- 1.Tüzün C, Yorulmaz I, Cindas A, Vatan S. Low back pain and posture. Clin Rheumatol. 1999;18(4):308–312. doi: 10.1007/s100670050107. [DOI] [PubMed] [Google Scholar]
- 2.Deyo R, Rainville J, Kent D. What can the history and physical examination tell us about low back pain? JAMA. 1992;268(6):760–765. [PubMed] [Google Scholar]
- 3.Andersson GBJ. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581–585. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 4.Youdas JW, Garrett TR, Egan KS, Therneau TM. Lumbar lordosis and pelvic inclination in adults with chronic low back pain. Phys Ther. 2000;80(3):261–275. [PubMed] [Google Scholar]
- 5.Nourbakhsh MR, Moussavi SJ, Salavati M. Effects of lifestyle and work-related physical activity on the degree of lumbar lordosis and chronic low back pain in a Middle East population. J Spinal Disord. 2001;14(4):283–292. doi: 10.1097/00002517-200108000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Hansson T, Bigos S, Beecher P, Wortley M. The lumbar lordosis in acute and chronic low-back pain. Spine. 1985;10(2):154–155. doi: 10.1097/00007632-198503000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976) 1994;19(14):1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 8.During J, Goudfrooij H, Keessen W, Beeker TW, Crowe A. Toward standards for posture. Postural characteristics of the lower back system in normal and pathologic conditions. Spine (Phila Pa 1976) 1985;10(1):83–87. [PubMed] [Google Scholar]
- 9.Christie HJ, Kumar S, Warren SA. Postural aberrations in low back pain. Arch Phys Med Rehabil. 1995;76(3):218–224. doi: 10.1016/s0003-9993(95)80604-0. [DOI] [PubMed] [Google Scholar]
- 10.Dreischarf M, Albiol L, Rohlmann A. Age-related loss of lumbar spinal lordosis and mobility—a study of 323 asymptomatic volunteers. PLoS ONE. 2014;9(12):e116186. doi: 10.1371/journal.pone.0116186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsuji T, Matsuyama Y, Sato K, Hasegawa Y, Yimin Y, Iwata H. Epidemiology of low back pain in the elderly: correlation with lumbar lordosis. J Orthop Sci. 2001;6(4):307–311. doi: 10.1007/s007760100023. [DOI] [PubMed] [Google Scholar]
- 12.Evcik D, Yücel A. Lumbar lordosis in acute and chronic low back pain patients. Rheumatol Int. 2003;23(4):163–165. doi: 10.1007/s00296-002-0268-x. [DOI] [PubMed] [Google Scholar]
- 13.Ashraf A, Farahangiz S, Pakniat Jahromi B, Setayeshpour N, Naseri M, Nasseri A. Correlation between radiologic sign of lumbar lordosis and functional status in patients with chronic mechanical low back pain. Asian Spine J. 2014;8(5):565–570. doi: 10.4184/asj.2014.8.5.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haas M, Vavrek D, Peterson D, Polissar N, Neradilek MB. Dose-response and efficacy of spinal manipulation for care of chronic low back pain: a randomized controlled trial. Spine J. 2014;14(7):1106–1116. doi: 10.1016/j.spinee.2013.07.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- 16.Hicks GE, George SZ, Nevitt MA, Cauley JA, Vogt MT. Measurement of lumbar lordosis: inter-rater reliability, minimum detectable change and longitudinal variation. J Spinal Disord Tech. 2006;19(7):501–506. doi: 10.1097/01.bsd.0000210116.94273.ad. [DOI] [PubMed] [Google Scholar]
- 17.Yochum TR, Rowe LJ. 3rd ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2005. Yochum and Rowe's Essentials of Skeletal Radiology. [Google Scholar]
- 18.Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20(12):1351–1358. [PubMed] [Google Scholar]
- 19.Takeda N, Kobayashi T, Atsuta Y. Changes in the sagittal spinal alignment of the elderly without vertebral fractures: a minimum 10-year longitudinal study. J Orthop Sci. 2009;14(6):748–753. doi: 10.1007/s00776-009-1394-z. [DOI] [PubMed] [Google Scholar]
- 20.Lang-Tapia M, Espana-Romero V, Anelo J, Castillo MJ. Differences on spinal curvature in standing position by gender, age and weight status using a noninvasive method. J Appl Biomech. 2011;27(2):143–150. doi: 10.1123/jab.27.2.143. [DOI] [PubMed] [Google Scholar]
- 21.Janssen MMA, Drevelle X, Humbert L, Skalli W, Castelein RM. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine (Phila Pa 1976) 2009;34(23):E826–E832. doi: 10.1097/BRS.0b013e3181a9fd85. [DOI] [PubMed] [Google Scholar]
- 22.Korovessis PG, Stamatakis MV, Baikousis AG. Reciprocal angulation of vertebral bodies in the sagittal plane in an asymptomatic Greek population. Spine. 1998;23(6):700–704. doi: 10.1097/00007632-199803150-00010. discussion 704-705. [DOI] [PubMed] [Google Scholar]
- 23.Bussières AE, Taylor JA, Peterson C. Diagnostic imaging practice guidelines for musculoskeletal complaints in adults—an evidence-based approach—part 3: spinal disorders. J Manip Physiol Ther. 2008;31(1):33–88. doi: 10.1016/j.jmpt.2007.11.003. [DOI] [PubMed] [Google Scholar]


