Abstract
Objective
The purpose of this case report is to describe a patient with a fracture of the Stieda process.
Clinical Features
A 39-year-old woman presented with pain and swelling of her left ankle immediately following a boogie boarding accident a few days earlier. Her clinical presentation was similar to that of an ankle sprain.
Intervention and Outcome
Radiographs were ordered, and a fracture of a normal variant, the Stieda process, was identified. Non-displacement of the fracture fragment was managed with conservative treatment consisting of a short-leg cast for 6 weeks. The fracture healed without complications.
Conclusion
The importance of early recognition of this fracture helped with proper management and a favorable outcome.
Key Indexing Terms: Diagnostic Imaging, Ankle Fractures, Differential Diagnosis, Chiropractic
Introduction
The incidence of ankle fractures is 9% and, along with fractures of the distal radius, metacarpals, proximal femur, and finger phalanges, constitutes 60% of the fractures seen by orthopedic surgeons.1 Recognition of ankle fractures is paramount to good patient management. Radiologists and clinicians need to be mindful of uncommon and easily missed fractures that necessitate a modified search pattern to improve accuracy of radiographic interpretation. The purpose of this case report is to describe a rare fracture of the Stieda process that can be easily misdiagnosed as a sprain or mistaken for a normal variant and, if not recognized as a fracture, will negatively affect patient management.
The Stieda process is an elongation of the lateral tubercle of the posterior process of the talus (Fig 1). It is larger than the medial tubercle and is considered the most variable aspect of hindfoot anatomy.2, 3, 4, 5 This process is the insertion point of the posterior talofibular ligament.2, 4, 6 Fractures of the posterior process usually occur in 1 of 2 ways: forced plantar flexion of the ankle causing a nutcracker-like compression between the calcaneus and the posterior malleolus of the tibia,2, 3, 5, 6, 7, 8 or ankle inversion resulting in avulsion by the posterior talofibular ligament, known as a Shepherd fracture.5, 8
Fig 1.

Normal Stieda process (elongated lateral process of talar tubercle).
Physical examination of a patient with a Stieda process fracture will reveal pain with plantar flexion that may be aggravated with flexion of the hallux.3, 6, 8 Tenderness on palpation is usually found in the posterolateral ankle, medial to the peroneal tendons and anterior to the lateral Achilles tendon.3, 6, 8 Patients will frequently present with swelling in the posterolateral ankle as well.3, 8 The purpose of this case report is to describe a patient with a fracture of the Stieda process.
Case Report
A 39-year-old woman presented to a chiropractic office with pain and swelling of her left ankle immediately following a boogie boarding accident a few days earlier. She reported that while boogie boarding at the beach, her foot caught in the sand and was forced by a wave into plantar flexion. She felt immediate pain in the posterior portion of her ankle. She noted swelling of the left ankle that began almost immediately and persisted for the next few days. Her pain was made worse with plantar flexion and any weight bearing on the left foot.
Radiographic examination revealed an acute vertical fracture line through the Stieda process of the left talus (Fig 2). The fracture fragment was non-displaced with good apposition and alignment. No other fractures were present. The ankle mortise joint was intact with no radiographic evidence of syndesmotic injury. Incidentally noted was a small enthesophyte at the insertion of the Achilles tendon into the calcaneus.
Fig 2.
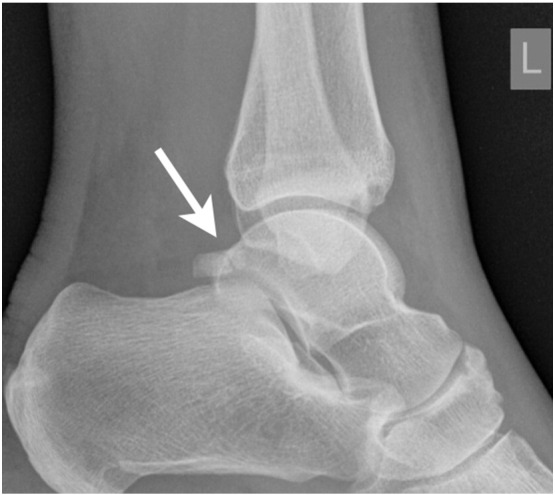
Initial image obtained following trauma. Note the subtle non-displaced fracture involving the Stieda process (arrow).
The patient was diagnosed with an acute fracture of the Stieda process of the talus and instructed to be in protected non-weight bearing for 6 weeks, followed by 2 weeks of limited weight bearing. The patient was closely monitored with serial follow-up radiographs at 2, 4, and 8 weeks to observe healing. The first radiographic series revealed no displacement of fracture fragment and there was good evidence of healing, so conservative management of immobilization continued. After 8 weeks, the patient reported painless weight bearing and plantar flexion. Radiographs at 8 weeks postinjury revealed excellent fracture healing (Figs 3 and 4). If the patient had failure of conservative care, a referral to an orthopedic surgeon would have been initiated. The fracture healed without complications. The patient gave consent for the publication of this study.
Fig 3.

Two-week follow-up image, when compared with initial radiographs, reveals no displacement of fracture fragment. Subtle haziness of the fracture line is observed (arrow).
Fig 4.

Eight-week follow-up image reveals osseous union of the fracture fragment with the host bone.
Discussion
Fracture of the Stieda process of the talus is a rare injury and must be differentiated from an os trigonum and simple ankle sprains. The os trigonum, an accessory bone from a secondary ossification center, is located directly posterior to the lateral tubercle (Fig 5). The os trigonum may persist as a separate ossicle attached to the lateral process by a cartilaginous synchondrosis and can be a source of pain.3, 4, 6 Because of its similar appearance and location, many Stieda process fractures are misdiagnosed as an os trigonum.6 To differentiate the two, it is important to thoroughly inspect the appearance of the bone. An os trigonum will be rounded with corticated edges. In contrast, a Stieda process fracture will have a rough and irregular surface with no cortical edge at the fracture site.9
Fig 5.
Note the os trigonum posterior to the talus, with the characteristic smooth, rounded, corticated edge separating the ossicle from the remainder of the talus.
Ankle sprains are most commonly caused by inversion and plantar flexion of the ankle, similar to the mechanisms for fracture of the Stieda process. This has resulted in frequent misdiagnosis of these fractures as sprains.3, 8, 10 In 1 case series, 17 of 20 patients with fractures were misdiagnosed with ankle sprains.3, 8 Because ankle sprains are frequently encountered, the Ottawa ankle rules can assist clinicians in avoiding unnecessary radiographs and determining whether radiographs should be obtained to exclude a fracture. The ankle assessment covers the ability to walk 4 steps (immediately after the injury or at the emergency department) and notes localized tenderness of the posterior edge or tip of either malleolus.11
Once the fracture is identified, proper management is essential for good prognosis. Minimal or non-displacement of fracture fragments is amenable to conservative management with a short-leg cast and non-weight bearing for 4 to 6 weeks. Weight bearing as tolerated is allowed after the period of immobilization.3, 6, 8 Complications of misdiagnosis or poor management of these fractures include chronic pain, late arthrosis, and limitation of ankle range of motion.2, 4, 5, 6, 10
Limitations
This case report is for 1 patient. The findings in this study may not necessarily relate to findings in other patients.
Conclusion
A rare injury of a common normal variant was described. Because of its similar appearance and location, a Stieda process fracture could be misdiagnosed as an accessory ossicle, the os trigonum. It is important to recognize and identify the fracture early to ensure proper management resulting in a favorable outcome by preventing complications.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): W.L.M., B.L.H.
Design (planned the methods to generate the results): W.L.M., B.L.H.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): B.L.H.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): W.L.M.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): W.L.M., B.L.H.
Literature search (performed the literature search): W.L.M.
Writing (responsible for writing a substantive part of the manuscript): W.L.M., B.L.H.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): B.L.H.
Practical Applications
-
•
This study emphasizes that an overlooked injury may potentially be mismanaged.
-
•
This study emphasizes the importance of differentiating a normal variant from a fracture.
Alt-text: Image 1
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Berkowitz M, Kim D. Process and tubercle fractures of the hindfoot. J Am Acad Orthop Surg. 2005;13(8):492–502. doi: 10.5435/00124635-200512000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Judd D, Kim D. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002;66(5):785–794. [PubMed] [Google Scholar]
- 4.Nyska M, Howard C, Matan Y. Fracture of the posterior body of the talus: The hidden fracture. Arch Orthop Trauma Surg. 1998;117(1-2):114–117. doi: 10.1007/BF00703458. [DOI] [PubMed] [Google Scholar]
- 5.Prasad F, Mittal D, Harlekar V, Raut V. Fracture of the posterior process of the talus: A case report. Eur J Orthop Surg Traumatol. 2007;17(4):417–419. [Google Scholar]
- 6.Kou J, Fortin P. Commonly missed peritalar injuries. J Am Acad Orthop Surg. 2009;17(12):775–786. doi: 10.5435/00124635-200912000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Bhanot A, Kaushal R, Bhan R, Gupta P, Gupta R, Bahadur R. Fracture of the posterior process of talus. Injury. 2004;35(12):1341–1344. doi: 10.1016/j.injury.2003.10.025. [DOI] [PubMed] [Google Scholar]
- 8.Paulos L, Johnson C, Noyes F. Posterior compartment fractures of the ankle: A commonly missed athletic injury. Am J Sports Med. 1983;11(6):439–443. doi: 10.1177/036354658301100611. [DOI] [PubMed] [Google Scholar]
- 9.Mansour R, Jibri Z, Kamath S, Mukherjee K, Ostlere S. Persistent ankle pain following a sprain: A review of imaging. Emerg Radiol. 2011;18(3):211–225. doi: 10.1007/s10140-011-0945-8. [DOI] [PubMed] [Google Scholar]
- 10.Warren NP, Knottenbelt JD. The Ottawa ankle rules and missed fractures of the talus. Emerg Med J. 2001;18(6):521. doi: 10.1136/emj.18.6.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stiell IG, McKnight RD, Greenberg GH. Implementation of the Ottawa ankle rules. JAMA. 1994;271(11):827–832. [PubMed] [Google Scholar]



