Abstract
Objective
The purpose of this study was to assess the diagnostic accuracy of a modified Bragard test compared with the straight leg raise (SLR) test in patients presenting with electrodiagnostic evidence of L5 and S1 nerve root compression.
Methods
This was a cross-sectional study conducted on 506 consecutive patients with signs and symptoms consistent with lumbosacral radiculopathy confirmed by electrodiagnostic study. Patients were evaluated from September 2013 to September 2015 in the physical medicine and rehabilitation outpatient clinic of Shahid Faghihi Teaching Hospital, Shiraz, Iran. The SLR test was investigated concomitantly to determine the sensitivity and specificity.
Results
Electrodiagnostic study findings indicated lumbosacral radiculopathy in 312 patients. Of these participants, 198 were positive on SLR testing, and of 114 SLR-negative patients, 79 were positive on Modified Bragard testing. Sensitivity of the Modified Bragard test was 69.3%, and specificity was 67.42%. Positive and negative predictive values were 73.15% and 63.16%, respectively. Positive likelihood ratio was 2.13, and negative likelihood ratio was 0.46. Diagnostic odds ratio was 4.63. In patients with symptom duration of less than 3 weeks, SLR sensitivity and specificity decreased as the Modified Bragard test diagnostic accuracy increased.
Conclusions
The Modified Bragard test is easy to perform and has an acceptable test performance, which can help to increase the discriminative power of clinical examination in patients with L5 or S1 nerve root compression who exhibit a negative SLR test result, especially in the acute phase of disease.
Key Indexing Terms: Intervertebral Disc Displacement, Physical Examination, Radiculopathy, Sensitivity and Specificity, Low Back Pain, Sciatica
Introduction
Low back pain is one of the most common health problems and results in personal, community, and financial burden globally. A recent global review of the prevalence of low back pain in the adult general population reported a point prevalence of 12% to 33% and a 1-year prevalence of 22% to 65%.1 Of all 291 conditions studied in the Global Burden of Disease 2010 Study, low back pain ranked highest in terms of disability (years lived with disability), and sixth in terms of overall burden (disability-adjusted life years).2 In Iran, low back pain is the third leading cause of disease burden as measured by disability-adjusted life years in the Iranian population aged 15 to 69 years, regardless of the causes of intentional and unintentional injuries.3
There are different medical conditions that cause low back and lower extremity pain, and patients may have more than 1 disorder. The question of whether a lumbosacral radiculopathy—or sciatica—is present is one of the most common cause of referrals to the electrodiagnostic laboratory.4 Although precise epidemiologic data are difficult to establish, the prevalence of lumbosacral radiculopathy is approximately 3% to 5%, distributed equally in men and women.5 Most radiculopathies are caused by root compression, most commonly from the intervertebral disk disease or other degenerative changes of the spinal column, such as ligamentous hypertrophy or the bony changes that accompany osteoarthritis. Other compressive lesions can less commonly cause radiculopathy, such as tumors and cysts.4 Lumbosacral radiculopathy is characterized by pain, paresthesia, weakness, reflex change, and sensory loss. Pain and paresthesia are uniquely distributed within the areas innervated by the affected nerve root.6
Patients with sciatica are commonly treated in primary care, but a small proportion is referred to secondary care and may eventually have surgery.7 Primary care clinicians use patient history and physical examination to evaluate the likelihood of radiculopathy and select the patients for further imaging and possible surgery. Clinical provocative tests, which place the lower extremity in a position to aggravate or relieve radicular compression symptoms, are commonly used in clinical practice in patients with a suspected lumbosacral radiculopathy. The straight leg raise test (SLR) and the crossed straight leg raising test (CSLR) are physical maneuvers that provoke the lumbosacral nerve roots. These tests are often used in making decisions about diagnostic imaging or hospital referral.8 Another complementary physical maneuver is the Bragard test. It is used when the SLR test is positive at a given point: the leg is lowered below the angle of radicular pain and dorsiflexion of the foot is induced. If there is an increase in radicular pain, the test is considered positive.
Because the current evidence indicates poor diagnostic performance of most physical tests used to identify lumbar radiculopathy,9 it is worthwhile to present a variation of a test that appears to have better diagnostic accuracy. The purpose of this study was to compare the diagnostic accuracy of the Modified Bragard test and the SLR test in a selected group of patients who had a clinical presentation of lumbosacral radiculopathy and correlated electrodiagnostic evidence of L5 or S1 nerve root compression.
Methods
This cross-sectional study included 506 consecutive patients referred for electrodiagnosis of the lower extremities as a result of unilateral radicular low back pain who were evaluated from September 2013 to September 2015 in the physical medicine and rehabilitation outpatient clinic of Shahid Faghihi Teaching Hospital, Shiraz, Iran. The study was performed in accordance with the Declaration of Helsinki. Its protocol was reviewed by medical ethics committee of Shiraz University of Medical Sciences. The rationale of the study was explained to all participants and they all signed a consent form before enrollment. This article was written according to the Standards for Reporting of Diagnostic Accuracy statement (except for items 13, 18, 22, and 24).10
Inclusion and Exclusion Criteria
Inclusion criteria were: age range of 20 to 80 years with a history and physical examination suggesting unilateral L5 or S1 radiculopathy (which includes symptoms of low back pain with pain or paresthesia radiating into the right or left lower extremity below the level of the knee, in the nerve root territory, dermatomal sensory loss for at least 2 weeks; or any sign of muscle atrophy or weakness as well as decreased Achilles stretch reflexes). Exclusion criteria were: current pregnancy or a history of major trauma to the vertebral column or spinal or lower limb surgery, history of spinal congenital abnormalities and diagnosis of infection or malignancies, and underlying rheumatologic disease or diabetes.
Clinical Examination
All participants were referred by physicians other than those who performed the study. One physical medicine and rehabilitation specialist blinded to all outcome data visited all eligible participants and performed the physical examinations. Standardized clinical examination consisted of L5, S1 dermatomal sensory testing through softly striking the skin bilaterally and simultaneously. The patient, with eyes closed, was asked if the feeling clearly differed between the left and right sides, L5, S1 myotomal muscle strength (by testing muscle strength during big toe extension and ankle plantar flexion in supine position against resistance compared with nonsymptomatic side), and determination of Achilles stretch reflexes (noticing reflex diminution or abolishment) and muscle wasting (by measuring calf circumference and providing 1 cm difference with nonsymptomatic side for a positive test result). There were intervals of 5 minutes’ rest between diagnostic tests to allow the patients recover from any pain or discomfort induced during examination. The order of test performance (SLR or Modified Bragard test) was also randomly alternated to prevent testing bias.
Assessment Procedures
The SLR test was performed by having the patient lie down on a flat examination table in a supine position. Both hips and knees of the involved leg were maintained in a neutral position neither abducted nor adducted. The patient’s head was not supported by a pillow. The examiner grasped the patient’s heel in the cup of his hand. The examiner’s other hand maintained the patient’s knee in an extended position. The examiner slowly raised the tested leg up to 90° by flexing the hip while maintaining the knee in extension and keeping the limb neutral, neither externally nor internally rotated. The maneuver was positive if the patient complained of reproduction of symptoms distal to the knee joint, between 30° and 70° of hip flexion.5 An angular goniometer with a degree of error equal to ±1° was applied at the level of the greater trochanter to measure the value of hip flexion.
When a structural abnormality such as a herniated disk compresses the nerve root proximal to or at the neural foramen, pain may occur. This may lead to pain radiating down the leg in the appropriate nerve root distribution (generally L5, or S1). The exact cause of the pain is unknown, but the symptoms may be related to decreased blood flow in the nerve root, increased tension of the nerve, compression of the nerve root, nerve root irritation, or other causes.6 The reproduction of back pain only or thigh pain (not extending distal to the knee) was considered a negative test.
The Modified Bragard test was performed in the following manner. The patient was positioned supine on the examination table with both legs straight. The examiner began with the SLR test. If the patient sensed no radicular pain or symptoms despite 70° hip flexion (negative SLR test), the foot was dorsiflexed firmly, and if radiating pain below the knee was produced, the Modified Bragard test result would be recorded as positive. The test is based on the hypothesis that combining hip flexion and knee extension with ankle dorsiflexion will increase the examiner’s capacity to provoke nerve root/sciatic signs and symptoms in SLR-negative patients.
Electrodiagnosis (EDx) served as the reference criterion for lumbosacral radiculopathy. All the eligible participants underwent the same standardized electrophysiologic examination by a board-certified physiatrist with 10 years of postgraduate experience by the same instrument (Medelec Synergy VIASIS, Surrey, England) in the same session as physical examination was performed without any time interval. She was unaware of the patients’ physical examination at the time of enrollment.
The EDx was considered positive according to standardized diagnostic criteria: (A) positive sharp waves or fibrillation potentials (in 1-limb muscle plus lumbar paraspinal muscles at the corresponding level, or in 2-limb muscles innervated by the same nerve root), (B) remodeled motor unit action potentials (high-amplitude, long-duration or polyphasic motor unit action potentials increased more than 30% in at least 2 muscles of 1 myotome innervated by the same myotome but by separate peripheral nerves), or (C) prolonged soleus H reflexes.11, 12
All nerve conduction study procedures were performed in accordance with the guidelines for measurement, temperature, safety precautions, and electrode placement.13 Motor and sensory nerve conduction studies were carried out first, and after that, H-reflex testing of the soleus and electromyography were conducted. The H reflex was used to evaluate the status of the peripheral nervous system with respect to proximal peripheral nerve conduction and potential entrapment of the nerve roots, such as radiculopathies. To perform soleus muscle H-reflex testing, the patient was positioned comfortably in prone position with the feet off the edge of a plinth. A pillow was placed beneath the legs to cause slight knee flexion. The active electrode was located in the bisected line between the mid-popliteal fossa and the Achilles tendon, and the reference electrode was located over the Achilles tendon when the ground electrode was placed between the stimulus and recording electrode. Sweep speed of 10 ms/div, amplifier sensitivity of 500 μV/div and pulse duration of 1.0 ms were used. The cathode of the stimulator was placed in the mid-popliteal fossa with the anode distal. The stimulus was delivered at a rate of 1 stimulation every 2 to 3 seconds. The current intensity was slowly increased until the H-reflex magnitude was maximized without concomitant activation of the motor fibers. Several responses were noted at this stimulus level to ensure a reproducible and stable response. The latency was then recorded to the initial departure of the H reflex from the baseline. Side-to-side difference of 1.5 ms was used as a prediction of an S1 radiculopathy.14 H-reflex latency prolongation or side-to-side differences probably indicate neural demyelination with significant damage of the large diameter nerve axons.15
Statistics
Descriptive statistics were used to analyze the sample's demographic data and clinical findings. Positive and negative results from EDx were cross tabulated (2 × 2 contingency table) with positive and negative results from each index test and sensitivity, specificity, and positive and negative predictive values. The diagnostic odds ratio (DOR) and likelihood ratio (LR) with 95% confidence intervals (CIs) were calculated.
Furthermore, patients were divided according to the duration of symptoms into acute (<3 weeks) and chronic (>3 months) to compare them statistically.16, 17 For each group, sensitivity, specificity, positive and negative LRs, and positive and negative predictive values were analyzed. Statistical analyses were done using Statistical Package for the Social Sciences, Version 14.0 (SPSS Inc, Chicago, Illinois).
Results
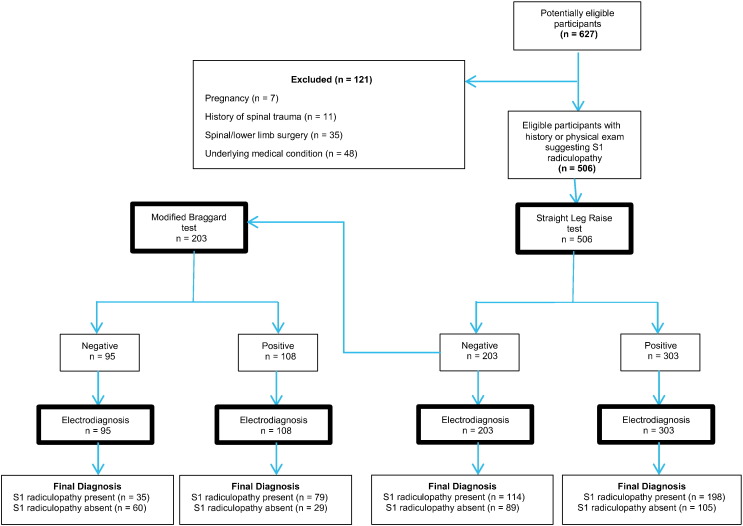
A total of 627 potentially eligible participants were enrolled in the study. Of these, 121 participants were excluded from further analysis because of pregnancy, history of surgery or trauma, and confounding underlying medical condition (Fig 1).
Fig 1.
Flow diagram showing the sensitivity of the modified Bragard test versus straight leg raise test.
Mean (standard deviation [SD]) age of the participants was 46.51 (14.63) years old. Among them, 204 patients (40.3%) were male and 302 (59.6%) were female. Frequency of positive clinical findings, provocative tests, and electrodiagnostic findings on the symptomatic side of the participants with EDx evidence of sciatica are shown in Table 1.
Table 1.
Findings on the Symptomatic Side of Participants With EDx Evidence of Sciatica
| Measure | No. of Participants With Lumbosacral Radiculopathy (%), n = 312 |
|---|---|
| Clinical finding | |
| Ankle plantar flexion weakness | 28 (9) |
| Big toe extension weakness | 46 (14.7) |
| Dermatomal sensory loss in heel/lateral of foot | 62 (19.8) |
| Dermatomal sensory loss on the dorsum of foot | 30 (9.61) |
| Impaired Achilles deep tendon reflexes | 91 (29.1) |
| Muscle wasting | 32 (10.2) |
| Provocative test | |
| Positive SLR | 198 (63.4) |
| Positive modified Bragard test | 79 (69.2)a |
| Electrodiagnostic finding | |
| Prolonged H reflex | 250 (80.1) |
| PSW/fibrillation potentials | 67 (21.4) |
| Remodeled MUAPs | 188 (60.2) |
EDx, electrodiagnosis; MUAP, motor unit action potential; SLR, straight leg raise; PSW, positive sharp wave.
Positive modified Bragard test in total number of 114 patients with sciatica who are SLR negative.
Of the 506 patients, 312 (172 were female and 140 were male) were diagnosed with lumbosacral radiculopathy on the basis of EDx findings; the mean (SD) age of the patients was 47.80 (13.7) years. Duration of symptoms ranged from 14 days to 72 months, with a mean (SD) duration of 24.2 (22.3) weeks.
Of these 312 sciatica patients, 198 had positive a SLR test on the ipsilateral side of complaint, whereas of the 194 patients for whom the electrodiagnostic evaluation was thought to indicate no evidence for L5 or S1 radiculopathy, the SLR test yielded negative results for 89 patients (Table 2). There was no significant difference in the age between the SLR-positive and SLR-negative patients.
Table 2.
2 × 2 Contingency Table for SLR Test
| Result | Positive EDx for Lumbosacral Radiculopathy | Negative EDx for Lumbosacral Radiculopathy | Total |
|---|---|---|---|
| Positive straight leg raising | 198 | 105 | 303 |
| Negative straight leg raising | 114 | 89 | 203 |
| Total | 312 | 194 | 506 |
EDx, electrodiagnosis; SLR, straight leg raise.
Of the 114 SLR-negative patients for whom the sciatica was documented by EDx, 79 participants had a positive Modified Bragard test, whereas of the 89 SLR-negative patients for whom electrodiagnostic evaluation was thought to indicate no evidence for L5 or S1 radiculopathy, the test yielded negative results for 60 patients (Table 3).
Table 3.
2 × 2 Contingency Table for Modified Bragard Test
| Result | Positive EDx for Lumbosacral Radiculopathy | Negative EDx for Lumbosacral Radiculopathy | Total |
|---|---|---|---|
| Positive modified Bragard test | 79 | 29 | 108 |
| Negative modified Bragard test | 35 | 60 | 95 |
| Total | 114 | 89 | 203 |
EDx, electrodiagnosis.
The sensitivity value of the SLR test for sciatica was 63.46% (95% CI: 57.85-68.81), and specificity was 45.88% (95% CI: 38.72-53.16). The positive and negative predictive values were 65.35% and 43.84%. The positive LR was 1.17 (95% CI: 1.00-1.37), and the negative LR was 0.80 (95% CI: 0.64-0.98). The DOR was 1.46 (Table 4).
Table 4.
Sensitivity, Specificity, Positive and Negative LRs, and Positive and Negative Predictive Values in 2 Provocative Tests
| Test | Sensitivity (95% CI) | Specificity (95% CI) | PLR (95% CI) | NLR (95% CI) | PPV (95% CI) | NPV (95% CI) |
|---|---|---|---|---|---|---|
| Modified Bragard Test | 69.30% (59.97-77.60) | 67.42% (56.66-76.98) | 2.13 (1.54-2.94) | 0.46 (0.33-0.62) | 73.15% (66.36-79.00) | 63.16% (55.67-70.06) |
| Straight Leg Raising | 63.46% (57.85-68.81) | 45.88% (38.72-53.16) | 1.17 (1.00-1.37) | 0.80 (0.64-0.98) | 65.35% (61.77-68.76) | 43.84% (38.72-49.10) |
CI, confidence interval; NLR, negative likelihood ratio; NPV, negative predictive value; PLR, positive likelihood ratio; PPV, positive predictive value.
The sensitivity value of the Modified Bragard test for sciatica was 69.30% (95% CI: 59.97-77.60), and specificity was 67.42% (95% CI: 56.66-76.98). The positive and negative predictive values were 73.15% and 63.16%. The positive LR was 2.13 (95% CI: 1.54-2.94) and the negative LR was 0.46 (95% CI: 0.33-0.62). The DOR was 4.63 (Table 4).
Subgroup analysis was carried out on chronicity of the complaint comparing only acute (symptoms <3 weeks) and chronic (symptoms >12 weeks) patients. Of the 506 patients, 98 had the symptoms for less than 3 weeks and were labeled as acute, whereas 267 had the symptoms for 3 months or longer and were labeled as chronic. Subacute patients (n = 141) were not included in the subgroup analysis. There was no significant age difference between the acute and chronic patients. Statistical analysis was also performed using 2 × 2 contingency tables for each of the 2 groups. Results are shown in Table 5.
Table 5.
Sensitivity, Specificity, and Positive and Negative LRs in Acute and Chronic Patients
| Measure | Acute Patients |
Chronic Patients |
||
|---|---|---|---|---|
| Straight Leg Raising | Modified Bragard Test | Straight Leg Raising | Modified Bragard Test | |
| Sensitivity (95% CI) | 58.47% (54.03-62.91) | 76.62% (67.01-86.22) | 62.24% (56.75-67.72) | 66.50% (57.92-75.11) |
| Specificity (95% CI) | 42.85% (33.3-52.4) | 66.25% (58.76-73.73) | 45.91% (38.66-53.20) | 64.38% (57.66-71.11) |
| Positive LR (95% CI) | 1.09 (1-1.18) | 4.23 (2.78-5.69) | 1.17 (1.02-1.34) | 2.20 (1.50-2.91) |
| Negative LR (95% CI) | 0.53 (0.32-0.77) | 0.35 (0.21-0.49) | 0.77 (0.61-0.93) | 0.5 (0.33-0.67) |
CI, confidence interval; LR, likelihood ratio.
Evaluating false-positive SLR results indicated that the SLR test yielded positive results for 39.8% of the patients whose EDx identified no electrophysiological abnormality, 66.6% of the patients with radiculopathy other than L5 and S1 roots, and 55% of the patients with EDx evidence of a nerve problem other than a radiculopathy (Table 6).
Table 6.
Positive Test Results in Patients for Whom the EDx Indicated No Evidence for L5, S1 Radiculopathy
| EDx Final Impression | n Positive (n total) |
|
|---|---|---|
| Straight Leg Raising | Modified Bragard Test | |
| No evidence of any electrophysiological abnormality | 18 (43) | 6 (20) |
| Radiculopathy other than L5 and S1 roots | 22 (33) | 7 (15) |
| Nerve problems other than a radiculopathy | 65 (118) | 16 (54) |
| Total | 105 (194) | 29 (89) |
EDx, electrodiagnosis.
The Modified Bragard test yielded positive results for 30% of the patients whose EDx indicated no electrophysiological abnormality, 46.6% of the patients with radiculopathy other than L5 and S1 roots, and 29.6% of the patients with EDx evidence of a nerve problem other than radiculopathy (Table 6).
Discussion
Provocative lumbosacral tests with high diagnostic value can help clinicians such as family physicians, doctors of chiropractic, or manual or physical therapists to confirm their diagnosis, especially in those participants lacking well-defined neurologic deficits, without having to resort to advanced diagnostic testing.
Some magnetic resonance imaging– or EDx-confirmed patients with lumbosacral radiculopathy were SLR negative in clinical evaluation. In other words, “SLR sensitivity may have been overestimated over the years.”18, 19 This observation is parallel to our findings, indicating sensitivity of 63.46% (95% CI: 57.85-68.81) for SLR test (Table 4). The moderate sensitivity value reported indicates that administration of this test might produce considerable negative responses in patients with sciatica.
The SLR test alone cannot provide sufficient guidance to the examiner for a correct interpretation of the clinical picture of the patient, and only rarely does the positive or negative test result change the clinical diagnosis (as can be inferred from positive and negative LRs).20 The DOR noted in our study implies a slightly greater likelihood for the test to be positive in the group of patients with radiculopathy compared with nonradiculopathy patients. Therefore, a modified Bragard test may be a way to enhance the SLR test to discriminate the patients with lumbosacral radiculopathy from nonradiculopathy participants.
Ankle dorsiflexion in conjunction with knee extension increases the nerve root/sciatic tension.21 Three orthopedic and neurologic tests are associated with dorsiflexion of the foot: the Bragard, Fajersztajn, and Homan tests. The Homan test uses foot dorsiflexion to detect deep vein thrombosis and the Bragard and Fajersztajn tests are confirmatory tests for SLR and CSLR tests, respectively. Thus, there is no independent test using dorsiflexion to increase the nerve root/sciatic tension in SLR-negative or CSLR-negative patients. The modified Bragard test combines hip flexion and knee extension with ankle dorsiflexion to increase the examiner’s capacity to provoke the nerve root/sciatic signs and symptoms in SLR-negative patients. As shown in Table 4, the modified Bragard test is a provocative test with acceptable diagnostic odd ratio that augments the SLR test and helps to increase the sensitivity of physical examination.
As shown in Table 5, in patients with acute phase of lumbosacral radiculopathy, the sensitivity and specificity of SLR decrease slightly, which can be concomitantly compensated by the increased diagnostic accuracy of the modified Bragard test. A possible explanation for this difference in acute and chronic phase SLR could be the initial minimum inflammation of the nerve roots at the level of compression in the acute phase of disease. Dorsiflexion of the foot maximizes the tension on the nerve roots, emphasizing the importance of the modified Bragard test in SLR-negative patients in the acute phase of the disease. Lower accuracy of provocative tests in patients with chronic disease may contribute to the relatively higher age in this group because the discriminative power of the SLR seems to decrease when age increases.20, 22
In our study, a positive SLR test provided a sensitivity of 63.46 and specificity of 45.88 for diagnosing a lumbosacral radiculopathy. van der Windt et al9 in their review article reported heterogeneity with sensitivities of SLR ranging between 35% and 97% and specificities between 10% and 100%. Vroomen et al23 reported the sensitivity of SLR to be 64%, and specificity was reported to be 57%. These findings are parallel to ours.
The modified Bragard test provided a sensitivity of 69.3% and specificity of 67.4% for diagnosing a lumbosacral radiculopathy. Thus, more sensitive tests, like the modified Bragard, might be used in radiculopathy in which the SLR is negative. It is another variation of neurodynamic tests designed to place the sciatic nerve roots under increased tension and would warn the examiner of the presence of nerve root compression when there is a negative SLR test.
There are some important considerations to keep in mind to perform the Modified Bragard test correctly. It is a provocative test for patients who have a positive result on SLR testing. The ankle should be dorsiflexed at the maximal point of the leg raising (70°) after the radicular pain for SLR has diminished, not from the beginning of raising, because ankle dorsiflexion may limit the angle of SLR.24 The test result is considered positive only if the pain radiates below the level of the knee.
Limitations
One of the inherent problems in determining the accuracy of provocative tests is the lack of a gold standard for the diagnosis of lumbosacral radiculopathy. Electrodiagnostic studies for radiculopathy are rarely falsely positive; if an electromyogram indicates evidence of a radiculopathy, the patient almost certainly has one. When the criteria used for diagnosis are the presence of positive sharp waves and fibrillation in 1 limb muscle plus the lumbar paraspinal muscles at the corresponding level or in 2 limb muscles innervated by the same nerve root, it is 100% specific for lumbosacral radiculopathy.4 If evidence of either acute changes or chronic denervation (as indicated by the fact that more than 30% of motor units are polyphasic, have large amplitude, and have increased duration) is used as the electrodiagnostic criterion, then specificity decreases, but it still remains in the range of 81 (nearly 100%), depending on the level tested.4
The diagnostic sensitivity and specificity of H-reflex testing vary widely, depending on the criteria and methods used to define the abnormality. One study noted 100% sensitivity and specificity, whereas others reported sensitivity of 51%, specificity of 91%, positive predictive value of 64%, and negative predictive value of 84% in the S1 radiculopathy group.11
A further limitation is that neither index tests (SLR and modified Bragard tests) nor the reference standard (EDx) was administered by 2 examiners, so reproducibility (interobserver variation of the tests) was not assessed. Intraexaminer and interexaminer reliability of the modified Bragard test need to be investigated and reported before it can be recommended for use in clinical practice or future research studies.
Other important methodological limitations include spectrum bias. Because the suspicion of a radiculopathy was the reason for referral in this study and also the reason for inclusion in the study, the participants were more likely to have a worse clinical presentation than those presenting in primary care. Patients most likely would have been referred for EDX testing because of a strong clinical suspicion of a radiculopathy or the lack of response to conservative care, so they are more likely than participants recruited with pseudoradicular pain or pain from the brachial plexus or a peripheral nerve to be accurately classified according to these tests.
Another limitation of the present study was that the participants were exclusively representative of radicular low back pain because of L5 and S1 root compression. Although the intervertebral disks affected most commonly are L4-5 and L5-S1, leading to L5 or S1 radiculopathies,5 the diagnostic property of the test in this study may be different when L4 or S2 root level is involved, so the results should be interpreted with caution.
Conclusions
The modified Bragard test is easy to perform and has an acceptable test performance, which can help to increase discriminative power of clinical examination in patients with L5 or S1 nerve root compression who exhibit a negative SLR test result, especially in the acute phase of the disease.
Acknowledgments
The authors thank Shiraz University of Medical Sciences, Shiraz, Iran, and also the Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Funding Sources and Conflicts of Interest
The present article was from the thesis study by author Seyedeh Halimeh Jafari and was financially supported by Shiraz University of Medical Sciences grant No. 91-01-01-545. No conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): K.H.
Design (planned the methods to generate the results): K.H.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): K.H.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): S.H.J.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): S.H.J., H.Y.
Literature search (performed the literature search): H.Y.
Writing (responsible for writing a substantive part of the manuscript): H.Y.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): H.Y., K.H.
Practical Applications
-
•
This study suggests a modification of the Bragard test with acceptable diagnostic accuracy.
-
•
This test may increase the discriminative power of clinical examination in patients with lumbosacral radiculopathy but negative SLR, especially in the acute phase of the disease.
Alt-text: Image 1
References
- 1.Hoy D, Bain C, Williams G. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 2.Hoy D, March L, Brooks P. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):968–974. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- 3.Mousavi SJ, Akbari ME, Mehdian H. Low back pain in Iran: a growing need to adapt and implement evidence-based practice in developing countries. Spine. 2011;36(10):E638–E646. doi: 10.1097/BRS.0b013e3181fa1da2. [DOI] [PubMed] [Google Scholar]
- 4.Barr K. Electrodiagnosis of lumbar radiculopathy. Phys Med Rehabil Clin North Am. 2013;24(1):79–91. doi: 10.1016/j.pmr.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 5.Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin. 2007;25(2):387–405. doi: 10.1016/j.ncl.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Rabin A, Gerszten PC, Karausky P, Bunker CH, Potter DM, Welch WC. The sensitivity of the seated straight-leg raise test compared with the supine straight-leg raise test in patients presenting with magnetic resonance imaging evidence of lumbar nerve root compression. Arch Phys Med Rehabil. 2007;88(7):840–843. doi: 10.1016/j.apmr.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ. 2007;334(7607):1313–1317. doi: 10.1136/bmj.39223.428495.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deville WL, van der Windt DA, Dzaferagic A, Bezemer PD, Bouter LM. The test of Lasegue: systematic review of the accuracy in diagnosing herniated discs. Spine. 2000;25(9):1140–1147. doi: 10.1097/00007632-200005010-00016. [DOI] [PubMed] [Google Scholar]
- 9.van der Windt DA, Simons E, Riphagen II. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database Syst Rev. 2010;(2) doi: 10.1002/14651858.CD007431.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Bossuyt PM, Reitsma JB, Bruns DE. Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. Standards for Reporting of Diagnostic Accuracy. Clin Chem. 2003;49(1):1–6. doi: 10.1373/49.1.1. [DOI] [PubMed] [Google Scholar]
- 11.Dillingham TR, Lauder TD, Andary M. Identifying lumbosacral radiculopathies: an optimal electromyographic screen. Am J Phys Med Rehabil. 2000;79(6):496–503. doi: 10.1097/00002060-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Cho SC, Ferrante MA, Levin KH, Harmon RL, So YT. Utility of electrodiagnostic testing in evaluating patients with lumbosacral radiculopathy: an evidence-based review. Muscle Nerve. 2010;42(2):276–282. doi: 10.1002/mus.21759. [DOI] [PubMed] [Google Scholar]
- 13.Tsao B. The electrodiagnosis of cervical and lumbosacral radiculopathy. Neurol Clin. 2007;25(2):473–494. doi: 10.1016/j.ncl.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Braddom RI, Johnson EW. Standardization of H reflex and diagnostic use in Sl radiculopathy. Arch Phys Med Rehabil. 1974;55(4):161–166. [PubMed] [Google Scholar]
- 15.Alrowayeh HN, Sabbahi MA. H-reflex amplitude asymmetry is an earlier sign of nerve root involvement than latency in patients with S1 radiculopathy. BMC Res Notes. 2011;4:102. doi: 10.1186/1756-0500-4-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brandt HC, Spiller I, Song IH, Vahldiek JL, Rudwaleit M, Sieper J. Performance of referral recommendations in patients with chronic back pain and suspected axial spondyloarthritis. Ann Rheum Dis. 2007;66(11):1479–1484. doi: 10.1136/ard.2006.068734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grotle M, Brox JI, Veierød MB, Glomsrød B, Lønn JH, Vøllestad NK. Clinical course and prognostic factors in acute low back pain: patients consulting primary care for the first time. Spine. 2005;30(8):976–982. doi: 10.1097/01.brs.0000158972.34102.6f. [DOI] [PubMed] [Google Scholar]
- 18.Majlesi J, Togay H, Unalan H, Toprak S. The sensitivity and specificity of the slump and the straight leg raising tests in patients with lumbar disc herniation. J Clin Rheumatol. 2008;14(2):87–91. doi: 10.1097/RHU.0b013e31816b2f99. [DOI] [PubMed] [Google Scholar]
- 19.Vroomen PC, de Krom MC, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of sciatica due to disc herniation: a systematic review. J Neurol. 1999;246(10):899–906. doi: 10.1007/s004150050480. [DOI] [PubMed] [Google Scholar]
- 20.Capra F, Vanti C, Donati R, Tombetti S, O’Reilly C, Pillastrini P. Validity of the straight-leg raise test for patients with sciatic pain with or without lumbar pain using magnetic resonance imaging results as a reference standard. J Manipulative Physiol Ther. 2011;34(4):231–238. doi: 10.1016/j.jmpt.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 21.Miller KJ. Physical assessment of lower extremity radiculopathy and sciatica. J Chiropractic Med. 2007;6(2):75–82. doi: 10.1016/j.jcme.2007.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tabesh H, Tabesh A, Fakharian E, Fazel M, Abrishamkar S. The effect of age on result of straight leg raising test in patients suffering lumbar disc herniation and sciatica. J Res Med Sci. 2015;20(2):150–153. [PMC free article] [PubMed] [Google Scholar]
- 23.Vroomen PC, de Krom MC, Wilmink JT, Kester AD, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry. 2002;72(5):630–634. doi: 10.1136/jnnp.72.5.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gajdosik RL, Rieck MA, Sullivan DK, Wightman SE. Comparison of four clinical tests for assessing hamstring muscle length. J Orthop Sports Phys Ther. 1993;18(5):614–618. doi: 10.2519/jospt.1993.18.5.614. [DOI] [PubMed] [Google Scholar]