Abstract
Synchronous penile and multiple cutaneous metastases over the pubic region from a rectal adenocarcinoma are rare, and they usually indicate widespread disease. The most frequent localization of cutaneous metastases is the postoperative scar. Simultaneous penile and pubic region metastases are extremely uncommon. Although a penile metastasis from a rectal adenocarcinoma has been reported, synchronous metastases over the penile and pubic area have not been reported previously. We present a case of penile and multiple cutaneous metastases over the pubic region from a rectal adenocarcinoma along with a brief review of the literature. To the best of our knowledge, this is the first such case reported to present with simultaneous penile and multiple cutaneous metastases.
KEYWORDS: Cutaneous metastases, Penile metastases, Radiotherapy, Rectal adenocarcinoma
INTRODUCTION
Synchronous penile and multiple cutaneous metastases over the pubic region from a rectal adenocarcinoma are rare, and they usually indicate widespread disease. The most frequent localization of cutaneous metastases is the postoperative scar. Simultaneous penile and pubic region metastases are extremely uncommon. The prognosis is poor, and the median survival after the appearance of skin metastases is 18–20 months. Although a penile metastasis from a rectal adenocarcinoma has been reported, synchronous metastases over the penile and pubic area have not been reported previously. A comprehensive review of reported cases and key features is also presented.
CASE REPORT
A 38-year-old man presented with multiple nodular lesions over the pubic region with ulceration and excoriation over the penile skin for the previous 2 months [Figure 1]. The lesions had been increasing in size and number over a period of time. The patient first consulted a dermatologist who referred him to a surgeon, given the history of malignancy in this patient with suspicion of cutaneous metastases. He had complaints of severe and intractable pain over the lesions. He had a 2-year history of carcinoma of the rectum with liver metastases. According to the American Joint Committee on Cancer Tumor-Node-Metastasis Staging System, the disease was Stage 4, so surgery was not feasible. A colonoscopy performed 9 months previously had revealed an ulceroproliferative lesion in the rectum 8 cm from the anal verge. Since a biopsy proved it to be an adenocarcinoma, a repeat biopsy was not performed. He underwent a colostomy 9 months previously because of obstructive symptoms. He received chemotherapy with three series of combinations of irinotecan, oxaliplatin, 5-fluorouracil (5 FU), and leucovorin (LV) (FOLFOX). A positron emission tomography-computed tomography scan revealed liver metastases, and he was encouraged to receive further chemotherapy, which he refused. Two months later, the patient returned to the surgery department and was found to have extensive new skin lesions involving the pubic region and external genital area. The cutaneous lesions were not close to the colostomy wound. His vital signs and laboratory investigations were normal. A hard, ulcerated lesion was felt on rectal examination. Histopathological examination of a biopsy from the skin nodules and the penile region revealed metastatic adenocarcinoma [Figure 2]. The tumor was assessed to identify histological features suggestive of high-frequency microsatellite instability which was negative in the index case. Palliative radiation therapy was advised, but the patient refused any further treatment. He also did not receive any traditional treatment such as Indian herbal medications. The patient was followed up for 2 months for symptomatic treatment and died.
Figure 1.

Multiple skin nodules over the pubic area with excoriation of the penile skin
Figure 2.
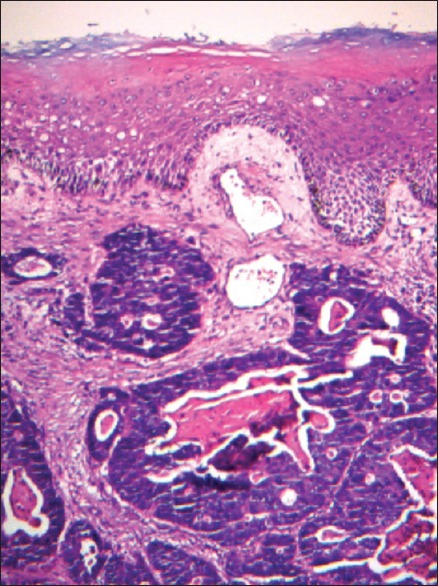
Metastatic cutaneous adenocarcinoma is revealed (H and E, ×10)
DISCUSSION
Synchronous penile and multiple cutaneous metastases over the pubic area from rectal cancer are uncommon and typically signify widespread disease associated with a poor prognosis. They indicate a failure of ongoing management or a recurrence of a malignancy which was thought to have been eradicated. Reingold found cutaneous metastases in 32 cases in autopsy studies of 2300 internal malignancies [1]. The incidence of cutaneous metastases was 5% for 7316 tumor registry patients, and among these, 1.3% had cutaneous metastases at the time of diagnosis [2]. According to a meta-analysis done by Krathen et al.[3], breast cancer is the most common primary cancer with cutaneous metastasis (24%). Colorectal, renal, lung, and urinary bladder cancers, and ovarian tumors, all have similar rates of incidence of cutaneous metastasis ranging between 3.4% and 4.0%[3]. Dehal et al.[4] found 28 cases of cutaneous metastases from rectal cancer, in patients with a mean age of 55.5 years with a slight male preponderance. A total of 54% of these patients had high-risk histological features [4]. The majority of the patients presented with Stage 3 or 4 disease. Cutaneous metastases were present as a recurrence in 20 patients and were the first sign of underlying malignancy in the remaining eight patients [4]. The perineum was the site of the skin metastases in 11 patients [4]. Data regarding the macroscopic appearance of cutaneous metastatic lesions from colorectal carcinoma are scarce in the literature. Skin nodules were the most common morphological finding [4]. The nodules were small, about 1–2 cm in diameter. Cutaneous metastases can be broadly classified as adenocarcinoma, squamous carcinoma, undifferentiated carcinoma, and other types [3]. Most cutaneous metastases from colorectal carcinoma are well-differentiated, often mucin-secreting adenocarcinomas. Isolated cutaneous metastases from rectal cancer have been reported, and they indicate widespread disease and are associated with a poor prognosis [5,6]. Possible mechanisms for cutaneous metastases are lymphatics, direct extension, and implantation at the time of the operative procedure, hematogenous spread, and spread along the ligaments of an embryonic origin [7]. Metastases usually develop within the first 3 years of follow-up; the median survival of patients with cutaneous metastases is 18–20 months [8]. An established chemotherapy regimen includes irinotecan, oxaliplatin, cisplatin, 5-FU, and capecitabine. Combinations of infusional 5FU/LV with irinotecan (FOLFIRI) or FOLFOX have increased the survival to over 20 months. In one study, FOLFIRI followed by FOLFOX and FOLFOX followed by FOLFIRI increased the median survival times to 21.5 months and 20.6 months, respectively [9]. Although a penile metastasis from a rectal adenocarcinoma has been reported [10], synchronous metastases over the pubic area and penile region have not been reported previously.
CONCLUSION
Simultaneous penile and multiple cutaneous metastases over the pubic region from rectal adenocarcinoma are rare and an unusual occurrence that presents mainly in the form of skin nodules. Penile and pubic region metastases are extremely uncommon. An early diagnosis in these patients is important because it can alter the treatment.
Declaration of patient consent
The author certifies that the patient has obtained appropriate patient consent form. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Reingold IM. Cutaneous metastases from internal carcinoma. Cancer. 1966;19:162–8. doi: 10.1002/1097-0142(196602)19:2<162::aid-cncr2820190204>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 2.Lookingbill DP, Spangler N, Sexton FM. Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients. J Am Acad Dermatol. 1990;22:19–26. doi: 10.1016/0190-9622(90)70002-y. [DOI] [PubMed] [Google Scholar]
- 3.Krathen RA, Orengo IF, Rosen T. Cutaneous metastasis: A meta-analysis of data. South Med J. 2003;96:164–7. doi: 10.1097/01.SMJ.0000053676.73249.E5. [DOI] [PubMed] [Google Scholar]
- 4.Dehal A, Patel S, Kim S, Shapera E, Hussain F. Cutaneous metastasis of rectal cancer: A case report and literature review. Perm J. 2016;20:74–8. doi: 10.7812/TPP/15-078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akpak YK, Dandin Ö, Gün İ, Atay V, Haholu A. A rare case of vulvar skin metastasis of rectal cancer after surgery. Int J Dermatol. 2014;53:e337–8. doi: 10.1111/ijd.12230. [DOI] [PubMed] [Google Scholar]
- 6.Ozgen A, Karakaya E, Bozdoǧan N. Scrotal skin metastasis from rectum adenocarcinoma. Rare Tumors. 2013;5:e60. doi: 10.4081/rt.2013.e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wright PK, Jha MK, Barrett PD, Bain IM. Colonic adenocarcinoma presenting as a cutaneous metastasis in an old operative scar. J Postgrad Med. 2003;49:157–8. [PubMed] [Google Scholar]
- 8.Sarid D, Wigler N, Gutkin Z, Merimsky O, Leider-Trejo L, Ron IG, et al. Cutaneous and subcutaneous metastases of rectal cancer. Int J Clin Oncol. 2004;9:202–5. doi: 10.1007/s10147-004-0389-1. [DOI] [PubMed] [Google Scholar]
- 9.Tournigand C, André T, Achille E, Lledo G, Flesh M, Mery-Mignard D, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: A randomized GERCOR study. J Clin Oncol. 2004;22:229–37. doi: 10.1200/JCO.2004.05.113. [DOI] [PubMed] [Google Scholar]
- 10.Lee JI, Kang WK, Kim HJ, Kim SH, Oh ST. Unusual metastasis from a rectal adenocarcinoma: Penile metastasis. ANZ J Surg. 2011;81:102. doi: 10.1111/j.1445-2197.2010.05623.x. [DOI] [PubMed] [Google Scholar]


