Abstract
Objective
The optimal treatment for isolated fractures of ulnar shaft is debatable. The purpose of this study was to compare functional outcomes and radiological union in patients treated for isolated fractures of the ulnar shaft by open reduction and internal fixation and a long arm cast.
Methods
This prospective study was conducted at level I trauma center from November 2014 to March 2016. 30 patients with isolated fractures of ulnar shaft were randomized to two groups to receive treatment by open reduction and internal fixation by plates and screws and a long arm cast. Outcome assessment was done by Disabilities of Arm Shoulder and Hand (DASH) score, range of motion at wrist and elbow, grip strength and radiological union. Quantitative variables were summarized Mean or Median. Normality was assessed using Kolmogorov-Smirnov test. Independent samples t-test and Mann-Whitney test were used for normally distributed variables and non-normally distributed variables respectively. Categorical variables were summarized as proportions. Effect of the intervention for categorical variables was assessed using Chi-square test
Results
There was no difference between the groups for pain on Visual Analogue Scale (VAS), grip strength, DASH score, and union at the end of 12 months. There was no difference between the groups for range of motion at the elbow and wrist. 12 (85.7%) patients in the ORIF group and 15 (93.7%) in the cast group united at the end of 12 months. The mean time to union was 13 weeks in the ORIF group and 18 weeks in the cast group.
Conclusion
Open reduction and internal fixation results in anatomical restoration of ulna, but this does not translates to better functional outcomes in short term (12 months).
Keywords: Ulna fracture, Plaster cast, Malunited fracture, Internal fracture fixation
1. Introduction
The optimal management of isolated fractures of the ulnar shaft is debatable. Both operative and non-operative methods of management have been advocated for treatment of these fractures.1, 2, 3, 4 The options for non-operative treatment are a plaster of Paris cast (long arm or short arm), functional brace, ace wrap (elastic bandage) and a sling. The options for operative treatment available are plates and intra-medullary nails. Non-operative management is associated with complications of nonunion, malunion, pain, deformity and decrease in range of motion of the wrist and the elbow. Operative fixation is associated with risk of infection, non-union, hardware prominence and may require a second operation for removal of hardware. To the best of our knowledge no prospective study has compared outcomes after operative and non-operative treatment of isolated fractures of the ulnar shaft.
1.1. Aims and Objectives
This study was conducted to investigate functional and radiological outcomes in isolated fractures of ulnar shaft after operative treatment by plates and non-operative treatment by above elbow plaster of Paris cast.
2. Subjects and methods
Skeletally mature patients who sustained isolated fractures of the ulnar shaft (AO type 22A1.1, 22A1.2, 23A1.2, 22B1.1, 22B1.2) presenting within 14 days of injury were randomized to two groups for treatment. The two groups were Open reduction and internal fixation (ORIF) group and Long arm cast (Cast group) group. The exclusion criteria were:
-
1.
Patients with injury to opposite upper extremity.
-
2.
Ipsilateral upper limb injury other than isolated ulna fracture.
-
3.
Ipsilateral wrist injury, elbow arthritis and congenital anomaly.
-
4.
Fractures within two centimeters of the distal radio-ulnar joint.
-
5.
Isolated fractures of the proximal one-third of the ulna and segmental fractures.
-
6.
Fractures with less than 15 ° of angulation of the ulnar shaft.
-
7.
Fractures with less than one cortical thickness displacement.
-
8.
Pathologic fractures.
The study was approved by institutional review board. Patients were informed of the treatment options available to them. Those patients consented to be part of the study were recruited to any of the two groups; the ORIF group and the Cast group by block randomization. Patients were free to withdraw from the study at any time during the study period.
2.1. Cast group
Patients in this group were treated by an above elbow plaster of Paris cast after closed reduction of the fracture. The acceptable reduction was defined as less than 50% of displacement and less than ten degrees of angulation on anteroposterior (AP) and lateral radiographs. The cast was kept for six weeks. Elbow and wrist mobilization of the extremity was started after six weeks.
2.2. ORIF Group
Patients recruited in this group were operated under a supraclavicular block in tourniquet control. The interval between extensor carpi ulnaris muscle and flexor carpi ulnaris muscle was utilized to expose the fracture site. A low contact dynamic compression plate (LC-DCP) was used in all cases to fix the fracture. The surgical incision was closed over a suction drain. Patients were mobilized when the pain decreased in the post-operative period.
Outcome assessment was done on following parameters:
-
1.
Range of motion: Range of motion of elbow joint (flexion/extension), wrist joint (palmar flexion/dorsal flexion) and forearm(supination/pronation) was measured by the goniometer at 2 weeks, 6 weeks, 12 weeks, 6, 9 and 12 months after operation in the ORIF group and 6 weeks, 12 weeks, 6,9 and 12 months in the cast group.
-
2.
The pain was measured on the visual analog scale (VAS). 0–4 mm was recorded as no pain, 5–44 mm as mild pain, 45–74 mm as moderate pain, 75–100 mm as severe pain.
-
3.
Grip strength was measured by a handheld Dynamometer. Grip strength was measured with the patient seated on an armless chair with the elbow by their sides and flexed to 90°.
-
4.
Functional outcome: The functional outcome assessment was done by the Disabilities of Arm, shoulder, and hand (DASH) score.
-
5.
Radiological outcomes: Radiological union was defined by the disappearance of the fracture line on three cortices of four on AP and lateral radiographs. Radiographs of the forearm with wrist and elbow joint were taken for both the ORIF and the cast groups at 2 weeks, 6 weeks, 6, 9 and 12 months after the fracture.
Data was entered using Microsoft Excel and analyzed using IBM SPSS Version 20. Quantitative variables were summarized as either Mean (SD) or Median (Interquartile range IQR). Normality was assessed using Kolmogorov-Smirnov test. Difference in quantitative variables for the two groups was assessed using Independent samples t-test for normally distributed variables and for non-normally distributed variables, the Mann-Whitney test was used. Categorical variables were summarized as proportions. Effect of the intervention for categorical variables was assessed using Chi-square test.
3. Results
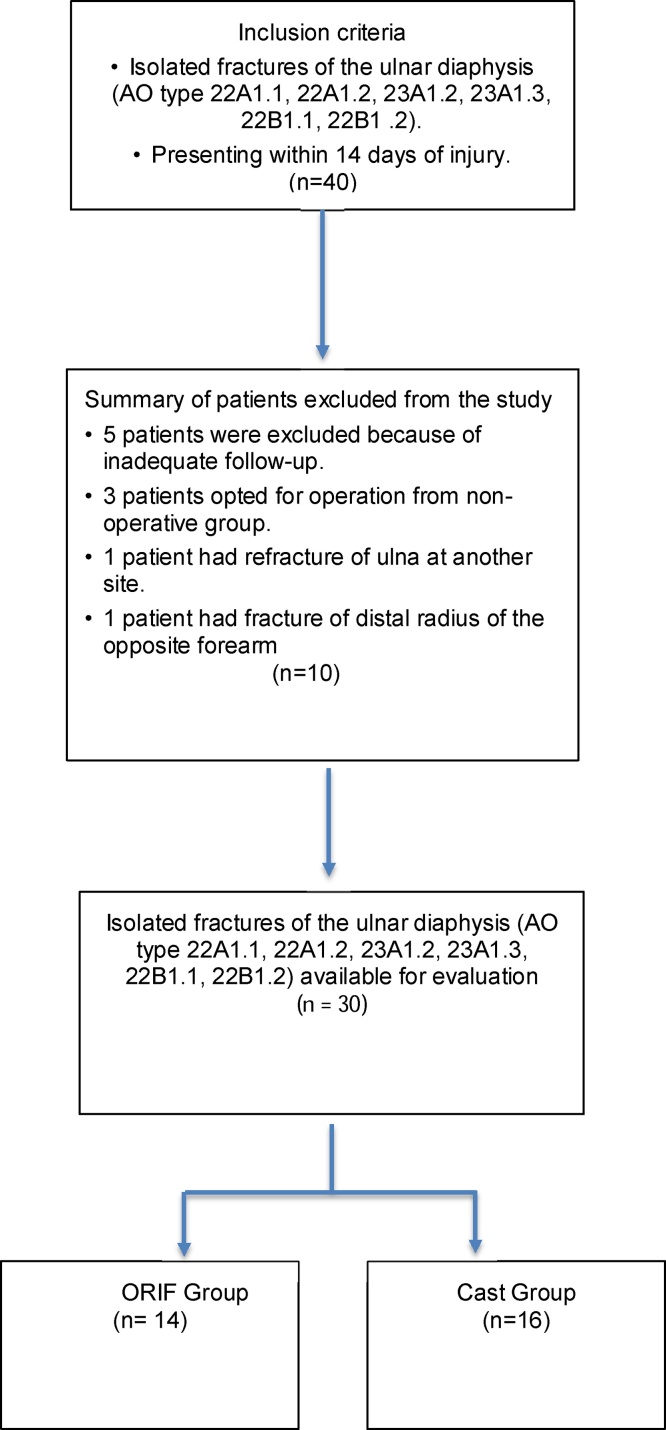
40 patients were recruited into the study. 30 patients were available at the end of 12 months for evaluation (Fig. 1). The excluded patients were not different from the study groups, except for the fractured side which was more on left. The demographic data and the fracture data in each group are summarized in (Table 1). There was no difference between the cast and the ORIF groups for age, sex distribution, fracture pattern, mechanism of injury and fracture location. The most common mechanism of injury was road traffic accidents, which was more than 50% in both the groups. 17 of 30 patients had the fracture of the distal third of ulna. There were nine smokers each in the cast and the ORIF groups. Five patients in the ORIF group and one patient in the cast group had associated injuries. There was no difference in union between the patients with or without associated injuries at the end of 12 months (P- .254). One patient had posterior cruciate ligament injury, two had tibia and fibula fracture, two had the fracture of the shaft of the femur, one had isolated fracture of the fibula, and one had fracture of the 5th metatarsal. There was no difference between the groups for VAS score, grip strength, DASH score, and union at the end of 12 months (Table 2). There was no difference between the groups for range of motion at the elbow and wrist (Table 3). 12 (85.7%) patients in the ORIF group and 15 (93.7%) in the cast group united at the end of 12 months (Table 2). The mean time to union was 13 weeks in the ORIF group and 18 weeks in the cast group. A representative case one each from the ORIF group and the cast group is presented here in Fig. 2, Fig. 3 respectively. Two cases sustained nonunion in the ORIF group and one in the cast group. One patient continued screw back-out in the ORIF group. There was no infection in any of the groups (Table 3).
Fig. 1.
CONSORT flow diagram showing patient selection during the study.
Table 1.
| Parameter | ORIF group | Cast group | P-value |
|---|---|---|---|
| Number of patients (n) | 14 | 16 | |
| Injured side n (%) | 0.491* | ||
| Right | 07 (50) | 10 (62.5) | |
| Left | 07 (50) | 06 (37.5) | |
| Mean age (years) | |||
| Mean (SD) | 35.50 (13.04) | 41.88 (14.78) | 0.22** |
| Sex distribution n (%) | 0.602* | ||
| Number of Males | 13 (92.9) | 13 (81.2) | |
| Number of Females | 01 (7.1) | 03 (18.8) | |
| Mechanism of injury | |||
| Road traffic accidents (RTA) | 57.1% | 50.0% | 0.958* |
| Accidental falls | 28.6% | 31.2% | |
| Assault | 7.1% | 12.5% | |
| Others(Hit by cricket ball, hit by a cow) | 7.1% | 6.2% | |
| Fracture pattern | |||
| Transverse | 05 | 07 | 0.654* |
| Oblique | 09 | 09 | |
| Fracture location | 0.688* | ||
| Distal third | 09 | 08 | |
| Mid third | 04 | 07 | |
| Proximal third | 01 | 01 | |
| AO TYPE | 0.064* | ||
| 21A2.1 | 01 | 01 | |
| 22A2.1 | 03 | 05 | |
| 22A3.1 | 01 | 02 | |
| 23A2.1 | 01 | 04 | |
| 23A3.1 | 08 | 04 | |
| Number of patients with Associated injuries | |||
| n (%) | 05(35.7) | 01(6.2) | 0.72* |
| Smokers n (%) | 09(64.3) | 09(56.2) | 0.654* |
Open reduction and internal fixation.
Long arm cast.
Chi-square test.
T-test.
Table 2.
Summary of Primary and secondary outcome.
| Outcome | ORIF group1 | Cast group2 | P-value |
|---|---|---|---|
| DASH score at 12 months | |||
| (Mean ± SD) | 13.36 ± 2.93 | 13.32 ± 2.39 | 0.971* |
| Mean time to union | 13 weeks | 18 weeks | |
| 3 months | 9(75%) | 8(53.33%) | |
| 6 months | 10(83.33%) | 14(93.33%) | |
| 12 months | 10(83.33%) | 14(93.33%) | 0.586** |
| Grip strength Median (IQR)4 | |||
| 12 weeks | 32.5(28–37.5) | 32.5(30–35) | 0.884*** |
| 12 months | 40.5(35.25–46.25) | 38.5(36–44) | 0.588*** |
| Visual analog scale(VAS) at 12 months | |||
| n (%) | |||
| No pain | 11 (78.6) | 15 (93.8) | 0.315**** |
| Mild Pain | 3 (21.4) | 1 (6.2) |
1. Open reduction and internal fixation.
2. Long arm cast.
3. Disabilities of Arm Shoulder and Hand score.
4. Interquartile range.
Independent Samples test.
Fisher’s exact test.
Mann-Whitney Test.
chi-square test.
Table 3.
Summary table showing range of motion and complications.
| Outcome | ORIF groupa | Cast groupb | P-value |
|---|---|---|---|
| Range of motion Median (IQR)c | |||
| Supination | 65 (38.75–70) | 55 (41.25–67.5) | 0.474* |
| Pronation | 55 (37.5–65) | 50 (35–58.75) | 0.427* |
| Wrist flexion | 65 (50–75) | 60 (50–68.75) | 0.334* |
| Wrist extension | 67.5 (52.5–70) | 57.5 (46.25–68.75) | 0.401* |
| Elbow flexion/extension | 140 (138.75–140) | 140 (140–140) | 0.929* |
| Complications | |||
| Non-union | 2 | 1 | 0.586** |
| Infection | 0 | 0 | |
| Screw Backout | 1 | 0 |
Open reduction and internal fixation.
Long arm cast.
Interquartile range.
Mann-Whitney Test.
Fisher’s exact test.
Fig. 2.
AP and lateral radiographs of a representative case managed by long arm cast, at presentation a, b; after closed reduction and cast application c, d; radiological union at 12 months e, f.
Fig. 3.
AP and lateral radiographs of a representative case managed by open reduction and internal fixation (ORIF) at presentation a, b; after ORIF c, d; radiological union at 12 months e, f.
4. Discussion
The purpose of this study was to compare the outcomes of ORIF and long arm plaster of Paris cast in isolated fractures of the ulnar shaft. We found no difference between the two methods of treatment. Age, Gender, mechanism of injury, fracture pattern, fracture location and associated injuries did not influence outcomes in either of the groups. Handoll et al. reviewed interventions for the treatment of ulnar shaft fractures and could not find sufficient evidence from randomized trials to determine which method of treatment is the most appropriate for isolated fractures of the ulnar shaft in adults.1 Non-operative management is prone to complications of malunion, secondary fracture displacement and non-union in various studies,2,3,5 but we did not find it translating to poor functional outcome scores in our study. There are no specific indications for operative treatment of isolated fractures of ulnar shaft. Studies have recommended operative fixation for the fracture of proximal third of ulna, fractures with displacement as low as 25% to > 50% or angulation of the fracture in any plane as low as 8 ° to >15 °.5, 6, 7 A fracture is considered unstable when the interosseous membrane joining the radius and ulna is torn, and operative management is recommended, but the data on fracture displacement at the time of injury being a contributing factor for the development of non-union is conflicting.7, 8, 9 We recruited patients with more than one cortex displacement and/or > 15° angulation in both the groups. The mean time to union was 13 weeks for ORIF group and 18 weeks for cast group in our study which is similar to other published studies.2, 3, 4, 5, 6, 7,9 The VAS score, the range of motion at the elbow and the wrist and grip strength were marginally better in the ORIF group than the cast group at the end of 12 months in our study, but this difference failed to reach statistical significance. Studies show that the mode of treatment has little or no influence on clinical and functional outcomes in isolated ulna fractures.5 Both the operative and non-operative methods of management have shown good to excellent results.4, 5, 6,13, 14, 15, 16, 17 One of the advantages of operative treatment over the non-operative treatment is the early restoration of function and range of motion of elbow and wrist in published studies.4,5,10,11 Patients in ORIF group in our study did marginally better than the cast group for the range of motion of elbow, but the difference did not reach statistical significance. The disadvantage of the operative management is implant removal at a later date. We did not study patients opting for implant removal in our study. Pain can be attributed to the implant in ORIF group and healing disturbances in the long arm cast group. We had more patients with mild pain in the ORIF group compared to the cast group, but the difference between groups did not reach statistical significance. Coulibaly et al. reported 20% incidence of associated injuries with isolated fractures of the ulnar shaft.5 They showed decreased incidence of nonunion and better outcomes with ipsilateral associated injuries and forearm fractures. They recommended operative fixation in the presence of associated injuries to facilitate rehabilitation and acute care.5 Ekkernkamp et al. have shown that the associated injuries have increased morbidity and hospital stay.12 There were five cases of associated injuries in the ORIF group and one case in the cast group. We did not find an association between the union rates and associated injuries in any of the groups. Complications associated with management of isolated fractures of the ulnar shaft are non-union, malunion, secondary displacement, compartment syndrome, synostosis and limitation of range of motion.5, 6, 7, 8, 9 The complication rate in both the groups in our study was comparable to other studies.5, 6, 7, 8, 9 Incidence of malunion ranges from 1% to 15% and non-union 0%–30% in published studies.5 We did not study malunion in our study. However, there was no difference in DASH score in between the groups at the end of nine months, reflecting no difference in the functional outcomes. The cause for nonunion in the treatment of isolated fractures of the ulnar shaft is conflicting and multifactorial. The factors implicated in the development of nonunion are fracture type (comminuted fractures), location, initial displacement, injury mechanism, operative treatment, age and gender.4,6,7 By contrast, studies have shown no relation between initial fracture displacement, fracture type, pattern, location, age, gender and development of nonunion.6,9,10 Nonoperative management of the isolated fractures of the ulnar shaft has been implicated in the development of delayed union.8 We had two patients of nonunion in the ORIF group and one in the cast group.
4.1. Strength and limitations of the study
The strength of the study is its prospective nature, intention to treat analysis, and less loss of follow-up. Limitations of the study were a small sample size, short follow-up, and single center of patient recruitment and assessment.
5. Conclusion
Open reduction and internal fixation results in anatomical restoration of ulna, but this does not translates to better functional outcomes in short term (12 months). Multicenter studies with large sample size and long term follow-up need to be designed to find out superiority of one treatment over another.
Conflict of interest
None to declare.
Declaration
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Specific national laws have been observed, too.
References
- 1.Handoll H.H., Pearce P. Interventions for treating isolated diaphyseal fractures of the ulna in adults. Cochrane Database Syst Rev. 2012;13:6. doi: 10.1002/14651858.CD000523.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atkin D.M., Bohay D.R., Slabaugh P., Smith B.W. Treatment of ulnar shaft fractures: a prospective, randomized study. Orthopedics. 1995;18:543–547. doi: 10.3928/0147-7447-19950601-06. [DOI] [PubMed] [Google Scholar]
- 3.Gebuhr P., Hölmich P., Orsnes T., Soelberg M., Krasheninnikoff M., Kjersgaard A.G. Isolated ulnar shaft fractures: comparison of treatment by a functional brace and long-arm cast. J Bone Joint Surg Br. 1992;74:757–759. doi: 10.1302/0301-620X.74B5.1527129. [DOI] [PubMed] [Google Scholar]
- 4.Leung F., Chow S.P. A prospective, randomized trial comparing the limited contact dynamic compression plate with the point contact fixator for forearm fractures. J Bone Joint Surg Am. 2003;8:5–A. doi: 10.2106/00004623-200312000-00011. [2343-8] [DOI] [PubMed] [Google Scholar]
- 5.Coulibaly M.O., Jones C.B., Sietsema D.L., Schildhauer T.A. Results of 70 consecutive ulnar nightstick fractures. Injury. 2015;46:1359–1366. doi: 10.1016/j.injury.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 6.Szabo R.M., Skinner M. Isolated ulnar shaft fractures: retrospective study of 46cases. Acta Orthop Scand. 1990;61:350–352. doi: 10.3109/17453679008993534. [DOI] [PubMed] [Google Scholar]
- 7.Corea J.R., Brakenbury P.H., Blakemore M.E. The treatment of isolated fractures of the ulnar shaft in adults. Injury. 1981;12:365–370. doi: 10.1016/0020-1383(81)90004-8. [DOI] [PubMed] [Google Scholar]
- 8.Sarmiento A., Ebramzadeh E., Brys D., Tarr R. Angular deformities and forearm function. J Orthop Res. 1992;10:121–133. doi: 10.1002/jor.1100100115. [DOI] [PubMed] [Google Scholar]
- 9.Brakenbury P.H., Corea J.R., Blakemore M.E. Non-union of the isolated fracture of the ulnar shaft in adults. Injury. 1981;12:371–375. doi: 10.1016/0020-1383(81)90005-x. [DOI] [PubMed] [Google Scholar]
- 10.Anderson L.D., Sisk D., Tooms R.E., Park W.I., 3rd Compression-plate fixation in acute diaphyseal fractures of the radius and ulna. J Bone Joint Surg Am. 1975;57:287–297. [PubMed] [Google Scholar]
- 11.Hooper G. Isolated fractures of the shaft of the ulna. Injury. 1974;6:180–184. doi: 10.1016/0020-1383(74)90011-4. [DOI] [PubMed] [Google Scholar]
- 12.Ekkernkamp A., Muhr G. Stable fracture of the ulna shaft: biomechanics and therapeutic consequences. Unfallchirurg. 1988;91:551–556. [PubMed] [Google Scholar]
- 13.Ostermann P.A., Ekkernkamp A., Henry S.L., Muhr G. Bracing of stable shaft fractures of the ulna. J Orthop Trauma. 1994;8:245–248. doi: 10.1097/00005131-199406000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Boussouga M., Bousselmame N., Lazrek K., Taobane H. Surgical management of isolated fractures of the ulnar shaft. Acta Orthop Belg. 2002;68:343–347. [PubMed] [Google Scholar]
- 15.Williams E.A., Friedrich J.B. Retrospective analysis demonstrates no advantage to operative management of distal ulna fractures. Hand (N Y) 2011;6:378–383. doi: 10.1007/s11552-011-9363-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kang H.J., Shim D.J., Yong S.W., Yang G.H., Hahn S.B., Kang E.S. Operative treatment for isolated distal ulnar shaft fracture. Yonsei Med J. 2002;43:631–636. doi: 10.3349/ymj.2002.43.5.631. [DOI] [PubMed] [Google Scholar]
- 17.Saka G., Sağlam N., Kurtulmuş T., Özer C., Uğurlar M., Akpınar F. Interlocking intramedullary ulna nails in isolated ulna diaphyseal fractures: a retrospective study. Acta Orthop Traumatol Turc. 2013;47:236–243. doi: 10.3944/aott.2013.3021. [DOI] [PubMed] [Google Scholar]