Abstract
Background
Hypertension is a major cause of cardiovascular disease and associated mortality, and postmenopausal women are at a high risk of hypertension. We aim to investigate the hypotensive effect and safety of acupuncture, focusing on postmenopausal women with prehypertension and stage 1 hypertension. In addition, we aim to investigate whether the effect of acupuncture treatment differed, depending on Sasang Constitution and cold–heat pattern.
Methods
This study is designed as an intervention cohort study. Two hundred postmenopausal women aged <65 years with prehypertension or stage 1 hypertension living in Daejeon city in Korea will be recruited, and randomly assigned to either an acupuncture or no-treatment control group. The intervention will consist of four sessions; one session will include acupuncture performed 10 times for 4 weeks. There will be a 20-week observation period after each session, and the total study duration will be 96 weeks. Acupuncture will be applied at the bilateral Fengchi (GB20), Quchi (LI11), Zusanli (ST36), and Sameumgyo (SP6) acupoints. The effect of acupuncture will be evaluated by comparing the change in systolic and diastolic blood pressure between the acupuncture and control groups every 4 weeks until the end of the study.
Discussion
To evaluate the success of blood pressure management, long-term observation is required, but no long-term studies have been conducted to evaluate the effect of acupuncture on blood pressure in postmenopausal women. To our knowledge, this study will be the first long-term study to investigate this issue for more than 6–8 weeks.
Keywords: Acupuncture, Hypertension, Intervention cohort study, Postmenopausal women, Prehypertension
1. Introduction
Hypertension is the major risk factor for cerebrovascular disease and cardiovascular disease. Hypertension guidelines (The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; JNC7) recommend the management of blood pressure (BP) and the risk factors of hypertension from the prehypertension stage.1, 2 Individuals with prehypertension are twice more likely to progress to hypertension than individuals with normal BP.3 Moreover, BP increases sharply in postmenopausal women due to imbalances in the cardiovascular system, such as decreased estrogen levels and the activation of the renin–angiotensin system.4, 5 Postmenopausal women are more likely to develop hypertension, obesity, diabetes, and other cardiovascular diseases (CVD) than men.6 Therefore, in postmenopausal women, BP must be monitored and managed more carefully.
Pharmacotherapy, which is a common method of controlling blood pressure, cannot be used in the prehypertension stage. A recent Cochrane review found that antihypertensive pharmacotherapy does not provide any benefit for mild hypertension.7 In another study, 9% of the patients discontinued treatment because of the side effects of antihypertensive drugs.8 To complement or replace pharmacotherapy to manage BP in postmenopausal women, continuous research and development of non-pharmacological interventions, such as lifestyle modification, are required.9 Long-term use of antihypertensive medication may result in side effects and increase the cost of medical care, thereby lowering the quality of life.10
Acupuncture treatment, which is widely used in East Asia, can be used as a non-pharmacological intervention to control hypertension in postmenopausal women. In several studies, acupuncture showed a BP-lowering effect in men and women in the prehypertension and hypertension stages.9, 10, 11, 12 Acupuncture has also been shown to be effective in controlling vasomotor symptoms, such as hot flushes in menopausal women.13 Recent studies have shown that the use of acupuncture is increasing and it is effective for lowering blood pressure.12, 14 Another study reported that the use of acupuncture in combination with pharmacological therapy is effective in decreasing arterial BP in patients with prehypertension or hypertension.15 Although several studies have shown that acupuncture is effective in lowering blood pressure,10, 11, 12, 13, 14, 15, 16 the evidence from well-designed studies that is needed to introduce acupuncture treatment for hypertension in postmenopausal women in clinical practice is still lacking.
Sasang Constitution (SC) types and cold–heat patterns categorize individual characteristics that indicate health status and human individuality.17, 18 These classification systems are commonly used in Korean medicine (KM) practice, and they are being standardized for use as an alternative medicine. Previous studies have suggested that the effect of acupuncture differs depending on SC type and cold–heat pattern.19, 20 Symptoms must be assessed according to constitution and pattern identification, and treatment must be prescribed accordingly.21, 22 Recently, Lee et al's study showed that the prevalence of hypertension among the four SC types was the highest in the Taeeum (TE) type, and that the SC type could be a risk factor for hypertension.23
Hence, this study has two objectives: first, to establish evidence of the efficacy of acupuncture in lowering BP in postmenopausal women with prehypertension and stage 1 hypertension; second, to analyze the effects of acupuncture according to SC and pattern identification.
2. Methods
2.1. Study design
This study is a prospective, comparative, randomized, interventional cohort study. To evaluate the hypertensive effect of acupuncture, we will divide the participants into a treatment group and a no-treatment control group; the cohort model will be used to observe the long-term effects of acupuncture.
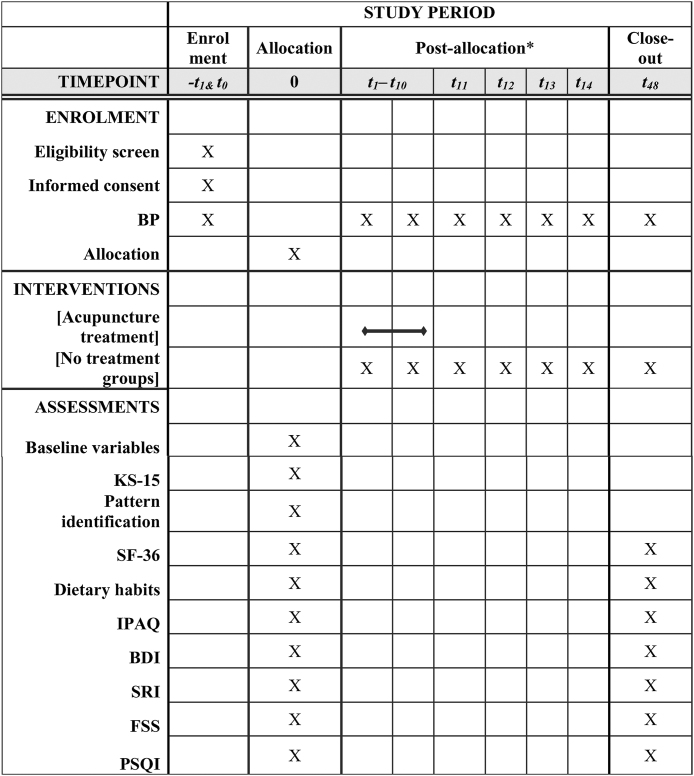
This study will consist of four sessions. Each session will include acupuncture treatment administered for 4 weeks, followed by a 20-week follow-up period in the acupuncture group. The participants in the control group will not receive acupuncture treatment; they will simply be observed for 24 weeks (Fig. 1). The no-treatment control group will be educated using a brochure containing information on hypertension while maintaining routine care, without acupuncture treatment. During the study period, lifestyle modifications, such as a low-salt diet, weight control, alcohol restriction, smoking cessation, lipid- and carbohydrate-intake control, dietary fiber intake, and exercise, will be implemented.
Fig. 1.
SPIRIT flow diagram : flowchart of the study-schedule of enrolment, interventions, and assessments.
The schedule of trial enrollment, interventions, and assessment is presented in the SPIRIT flow diagram (Fig. 1).
This study will be conducted in the Dunsan Korean Medicine Hospital of Daejeon University in Daejeon, Republic of Korea and has been approved by the relevant institutional review board.
2.2. Participants
The inclusion and exclusion criteria for this study are listed in Table 1. All participating physicians will be asked to design an informed consent form. Participants will be recruited by these KM physicians.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion criteria |
| 1. Postmenopausal women under 65 years of age.24 |
| 2. Subjects with prehypertension or stage 1 hypertension meeting JNC 7 BP criteria: systolic blood pressure (SBP) 120–159mmHg or diastolic blood pressure (DBP) 80–99mmHg on at least three office measurements. |
| Exclusion criteria |
| 1. Secondary hypertension |
| - Renal diseases: e.g., chronic renal failure, renal artery stenosis |
| - Endocrine diseases: e.g., adrenal disease, thyroid disease |
| - Other biological causes: e.g., neurologic disorder, obstructive sleep apnea, cancer, infectious disease |
| - Use of medications that affect blood pressure: e.g., glucocorticoids, central nervous system depressants |
| 2. Ongoing treatment for cerebrovascular disease or heart diseases |
| 3. Uncontrolled diabetes mellitus |
| 4. Prior hormonal therapy within the past month |
| 5. Korean medicine treatment within the past month. |
| 6. Previous hypersensitive reactions after acupuncture treatment. |
2.3. Sample size
We propose to recruit up to 200 participants for the cohort study. A control group will be set up to compare the effects of acupuncture treatment. Thirty control group subjects will be enrolled to ensure normality when comparing the effects between groups. On the basis of the results of a pilot study by Liu et al,12 the sample size of the treatment group should be a minimum of 97 per group. Considering the long follow-up period (2 years) and four sessions of acupuncture treatment, we believed that many participants should be included, as it is a cohort study and acupuncture seems to carry minimal risk. Therefore, for this study, we will recruit 170 participants for the acupuncture treatment group. In addition, to compare the effect of acupuncture with a control group, we will enroll 30 participants for the control group, which is the minimum number of participants for comparison analysis.
2.4. Intervention
The participants in the acupuncture group will receive acupuncture treatments 10 times over a period of 4 weeks (2 or 3 times/week). The participants in the control group will receive no acupuncture treatment. All subjects will be educated about lifestyle modifications, such as diet management, exercise, and so on.
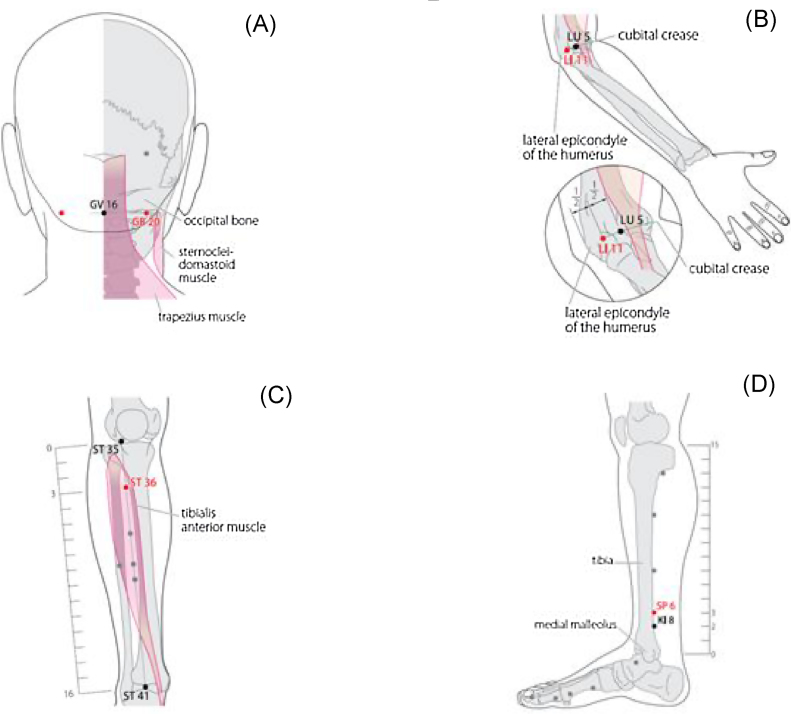
Acupuncture will be applied at eight acupoints: the bilateral Fengchi (GB20), Quchi (LI11), Zusanli (ST36), and Sameumgyo (SP6) points (Fig. 2). These acupoints were decided by consensus of five acupuncture experts who specialize in KM. These regimens have also been used previously in two studies conducted by this research group.9, 25
Fig. 2.
Acupuncture point locations (Both). (A) GB20; (B) LI11; (C) ST36; (D) SP6.
KM doctors manually manipulate the acupuncture needles with de-qi sensation and maintain the needles in position for 30 minutes, with intermittent manual stimulation. They insert the needles to a depth of 3.15 mm. All KM doctors who will be conducting acupuncture treatment are licensed KM doctors with at least 3 years of experience in acupuncture. We will use sterile, disposable needles with a length of 30 mm and a diameter of 0.25 mm (Dongbang Acupuncture Inc, Poryong, Korea). Because blood pressure changes every time, all subjects will be given treatment and blood pressure will be measured at similar times during the study period (Fig. 2).
2.5. Primary outcome
The primary outcome of the study is the change in SBP and DBP between baseline and after acupuncture treatment. During the treatment period, BP will be measured after each treatment using a conventional mercury sphygmomanometer (a baumanometer, U.S.A. standard type). In the control group, BP will be measured at the time of randomization and at 4 weeks after randomization. During the follow-up period, BP will be measured 4 times at 4-week intervals in both groups.
At each time point, the patient will be allowed to rest for at least 5 minutes before the first measurement of BP, and after that, BP will be measured again twice, at 2-minute intervals.2 Patients will be advised to avoid intake of caffeine-containing beverages, smoking, and exercise for 30 minutes prior to BP measurement, as well as to avoid heavy intake of food a day before the visit. The assessors will be trained for at least 5 hours about BP measurement to standardize the measurement method before this study.
2.6. Secondary outcomes
The secondary outcomes are the body mass index (BMI, kg/m2) and the Short Form-36 (SF-36). BMI will be assessed at baseline and after each session.26 The SF-36 questionnaire is widely used for assessing the quality of life; it includes 36-item measures for eight multi-item dimensions of health: physical functioning, social functioning, role limitations due to physical problems, role limitations due to emotional problems, mental health, energy/vitality, pain, and general health perception. The SF-36 will be administered at baseline and after each session.27. SF-36 scores will be calculated using Quality Metric Health Outcomes Scoring Software 5.0. Secondary outcomes will be assessed at baseline, after 4 weeks of acupuncture treatment, and at each follow-up visit.
2.7. Covariates
Blood pressure-related factors, such as diet, physical inactivity, mood, quality of sleep, fatigue, and pattern differentiation (KM) will be measured as covariates in the analysis.
To assess diet, the subjects’ dietary intake will be recorded using a 3-day diary, 24-hour recall method, and the diary contents will be recalled for 2 weekdays and 1 weekend day. To help subjects calculate the amount of food intake during the recording of dietary contents, we will provide rice bowls, soup bowls, side dishes, and measuring spoons representing serving units.28, 29 Nutrient intake, including salt intake, will be analyzed using the Computer Aided Nutritional Analysis Program (CAN PRO) version 5.0 software (Korean Nutrition Society, Seoul, Korea). Changes in calorie intake, sodium intake, and diet will be measured. The CAN PRO software program was devised by a qualified nutritionist in the Dunsan Korean Medicine Hospital of Daejeon, and categorizes foods into dietary programs and evaluates nutrients in the program.
Physical activity will be investigated using a questionnaire about the activities conducted during a week. The questionnaire evaluates intense activity, moderate physical activity, and walking activity. The participants will be evaluated in terms of total physical activity, specifically total walking activity, and how many hours they spent sitting during the week before the visit. These data will be used to calculate the amount of physical activity based on the IPAQ point-conversion method.30, 31
The mood of the participants will be investigated using a questionnaire on depression (Beck Depression Inventory [BDI]), and a short form of the Stress Response Inventory (SRI) for evaluation of stress. The BDI is composed of 21 variables that measure symptoms experienced during the past week. The BDI consists of emotional, motivational, and somatic symptoms of depression. Each item is scored on a four-point scale, ranging from 0 to 3.32, 33 The SRI comprises 22 questions covering three factors: somatization (nine questions), depression (eight questions), and anger (five questions). Each item is scored on a five-point scale, ranging from 0 to 4.34
Quality of sleep will be investigated using the Pittsburgh Sleep Quality Index (PSQI). The PSQI is a sleep survey that is frequently used to evaluate sleep quality and determine sleep disabilities during the previous month; its reliability and validity have been proven in multiple studies. The PSQI is a scale that assesses seven items: subjective sleep quality, sleep latency, sleep time, habitual sleep efficiency, factors that interfered with sleep, administration of sleeping pills, and daytime functional difficulties. The PSQI has internal consistency and a reliability coefficient (Cronbach alpha) of 0.83 for its seven components.35
To investigate the participants’ fatigue status, the Fatigue Severity Scale (FSS) will be used. The FSS is a self-reported survey that emphasizes the functional and behavioral aspects of fatigue; it comprises nine questions. It uses a Likert scale, in which scores from 1 to 7 can be chosen according to the subjective degree of disability. Fatigue level is then expressed as an average score derived by dividing the sum of scores for all items by nine.36
The SC type and the cold–heat pattern identification will also be investigated using the questionnaire. A simplified Korea Sasang Constitution Diagnostic Questionnaire (KS-15), comprising 15 questions on body type (one question on BMI, six questions on personality, and eight questions on protein deficiency) will also be administered. Cronbach alpha coefficients representing internal consistency are 0.509 for men and 0.494 for women. The agreement of experts on the KS-15 has been reported as 58.34% (72.8% for Taeeumin, 54.8% for noise, 44.1% for Soyangin). The agreement of the test group was reported as being 63.1% (63% for Taeeumin, 83.3% for Noise, 51.9% for Soyangin).17
The cold–heat pattern questionnaire is composed of eight questions about Cold and seven questions about Heat. Cronbach alpha coefficients representing internal consistency have been reported to be −0.79 for Cold and −0.83 for Heat.18
All covariates will be assessed at baseline and at the start of each session.
2.8. Randomization
Subjects will be randomly assigned to either the acupuncture group or a control group in a 17:3 ratio. Based on the assigned code provided by a random assignment program in a random number table generated using SAS Version 9.4, identification codes will be assigned to participants who agree to participate in the clinical study and who meet the selection/exclusion criteria. Random numbers will be assigned based on the random assignment table, sealed in envelopes, and provided to the test institute before clinical testing.
2.9. Statistical analysis
Statistical analysis will be performed for all variables. We will analyze the effect and safety by using the intent-to-treat (ITT) principle. Quantitative variables will be described using frequency tables for the different categories, and quantitative variables as the mean and standard deviation. Participants’ characteristics will be described and the differences between groups will be analyzed using the t-test and chi-square test. Changes in outcome within each group will be analyzed by the paired t-test, and differences between groups will be analyzed using ANCOVA.
The primary analyses will be based on the available data without imputation of missing values, but additional analyses will be performed on a completed data set in which all patients who did not start treatment or were lost to follow-up were included with their baseline values or last observation during follow-up. Significance will be considered as p < 0.05. Logistic regression analysis will be performed to estimate the prevalence of hypertension and to assess the independent effects of various lifestyle factors that may have an effect on the prevalence of hypertension. The relative risk by factors that are presumed to be related to the occurrence of hypertension will be assessed using odds ratios (ORs), using the regression coefficient and standard error of the linear logistic regression model.
2.10. Data management
Regular monitoring will be conducted for data quality control. Moreover, investigators will be convened to discuss practical issues that may be encountered, such as dealing with serious adverse events, revising the protocol, as well as addressing certain important issues that may be raised by investigators and participants.
2.11. Blinding
It is impossible that participants be blinded to group allocation, because participants in the control group will not receive any treatment. However, assessors and the statistician will be blinded to group allocation.
2.12. Safety
The assessment of safety is based mainly on the frequency of adverse events, which includes all serious adverse events. Information regarding adverse events will be summarized by presenting the number and percentage of participants experiencing any adverse event. Any other information (e.g., severity or relatedness to acupuncture) will also be collected.
3. Discussion
Most related studies have been performed over a short duration of 4–6 weeks, i.e., involving 10–12 treatments.37, 38, 39 To date, no study has been performed with the intent to observe the effect of long-term acupuncture treatment. Our study will be performed over a period of 24 months, and hence, is expected to reveal the long-term effects of acupuncture treatment in postmenopausal women with prehypertension and stage 1 hypertension. Since these results will be based on long-term follow-up observation, they are likely to be reliable.
Recent studies of acupuncture in BP control involved small samples. We recommend increasing the number of samples to develop a standardized research model that can be performed repeatedly. The results of this study can be used to develop a standard treatment model for repeated acupuncture treatment.
Previous studies have shown that the parasympathetic nervous is affected by acupuncture stimulation, and over time, its function is activated, resulting in decreased heart rate and decreased SBP.19, 20 In this study, acupuncture treatment can be affected by many different factors such as SC type and the cold-heat pattern. As mentioned previously, Kim et al21 and Lee et al22 have reported that different treatment approaches must be tailored to each individual's constitution. We hope that this study will help explain why the same acupuncture treatment produces different results according to individual characteristics. To eliminate the effect of variables other than acupuncture treatment that can affect blood pressure, the research subjects will be asked to maintain a steady lifestyle throughout the study period, and data on their diet, exercise rate, and use of medication will be collected.
Adequate treatment in the prehypertensive phase will be effective in preventing hypertension. The results of this study will contribute to lowering the prevalence of cardiovascular disease and improving the quality of life. It will provide clinical evidence that early detection and intervention will reduce the prevalence of cardiovascular disease, particularly in subjects experiencing prehypertension and stage 1 hypertension, improving health and preventing the risk of cardiovascular disease.
In conclusion, we hypothesize that after 2 years, the BP and hypertensive transition rate will be lower in the treatment group after four acupuncture sessions, than in the control group, and second, that the effect of acupuncture treatment on hypertension will differ according to the SC type and the pattern identification. The results of this study will yield insight into whether acupuncture can be used to lower BP in postmenopausal women. Analysis of the effect of acupuncture on individuals with different SC types and cold–heat patterns will reveal the factors influencing acupuncture effects.
4. Trial status
Recruitment for the study began in October 2014 and continued until approximately February 2015. Patients were followed up until approximately December 2016. Data management, comprising quality control, is ongoing.
Declarations
Ethics approval and consent to participate
Ethical approval for the study protocol was obtained from the Institutional Review Board of the Dunsan Korean Medicine Hospital of Daejeon University in Daejeon (approval no. 14-02, 14-02-03). Written informed consent will be obtained from all participants prior to enrollment in the study. They will also be informed that participation in the study is entirely voluntary and refusal to participate will not affect their medical care.
Trial registration
The protocol was registered with the Korea National Research Institute of Health Clinical Research Information Service (Registration number: KCT0002130, date of registration: 18 November 2016; Study protocol version 2.2).
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
This study was supported by the “Establishment of Korean Medicine Genome and Epidemiology Infrastructure” project (K18091) and “The Construction of Database of Mibyeong Clinical Research Based on Healthy Koreans” (NRF-2014M3A9D7034351) of the Korea Institute of Oriental Medicine.
Footnotes
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.imr.2017.11.003.
Contributor Information
Bok-Nam Seo, Email: florence@kiom.re.kr.
Ji-Eun Park, Email: jepark@kiom.re.kr.
Young-Eun Kim, Email: jade2010@kiom.re.kr.
Kyung-Won Kang, Email: gyungwon.gang@gmail.com.
In-Chan Seol, Email: seolinch@dju.kr.
Sun-Mi Choi, Email: smchoi@kiom.re.kr.
Appendix I. Supplementary data.
The following are the supplementary data to this article:
References
- 1.Chobanian A.V., Bakris G.L., Black H.R., Cushman W.C., Green L.A., Izzo J.L. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.Jones D.W., Hall J.E. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure and evidence from new hypertension trials. Hypertension. 2004;43:1–3. doi: 10.1161/01.HYP.0000110061.06674.ca. [DOI] [PubMed] [Google Scholar]
- 3.Zhang W., Li N. Prevalence, risk factors, and management of prehypertension. Int J Hypertens. 2011;2011:605359. doi: 10.4061/2011/605359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Hagan T.S., Wharton W., Kehoe P.G. Interactions between oestrogen and the renin angiotensin system – potential mechanisms for gender differences in Alzheimer's disease. Am J Neurodegener Dis. 2012;1:266–279. [PMC free article] [PubMed] [Google Scholar]
- 5.Maas A.H., Franke H.R. Women's health in menopause with a focus on hypertension. Neth Heart J. 2009;17:68–72. doi: 10.1007/BF03086220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zilberman J.M., Cerezo G.H., Del Sueldo M., Fernandez-Pérez C., Martell-Claros N., Vicario A. Association between hypertension, menopause, and cognition in women. J Clin Hypertens. 2015;17:970–976. doi: 10.1111/jch.12643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lenzer J. Cochrane review finds no proved benefit in drug treatment for patients with mild hypertension. BMJ. 2012;345:e5511. doi: 10.1136/bmj.e5511. [DOI] [PubMed] [Google Scholar]
- 8.Diao D., Wright J.M., Cundiff D.K., Gueyffier F. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev. 2012;8:Cd006742. doi: 10.1002/14651858.CD006742.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li D.Z., Zhou Y., Yang Y.N., Ma Y.T., Li X.M., Yu J. Acupuncture for essential hypertension: a meta-analysis of randomized sham-controlled clinical trials. Evid Based Complement Alternat Med. 2014:279478. doi: 10.1155/2014/279478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Du Y.Z., Gao X.X., Wang C.T., Zheng H.Z., Lei Y., Wu M.H. Acupuncture lowering blood pressure for secondary prevention of stroke: a study protocol for a multicenter randomized controlled trial. Trials. 2017;18:428. doi: 10.1186/s13063-017-2171-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee H., Kim S.Y., Park J., Kim Y.J., Lee H., Park H.J. Acupuncture for lowering blood pressure: systematic review and meta-analysis. Am J Hypertens. 2009;22:122–128. doi: 10.1038/ajh.2008.311. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y., Park J.E., Shin K.M., Lee M., Jung H.J., Kim A.R. Acupuncture lowers blood pressure in mild hypertension patients: a randomized, controlled, assessor-blinded pilot trial. Complement Ther Med. 2015;23:658–665. doi: 10.1016/j.ctim.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 13.Dodin S., Blanchet C., Marc I., Ernst E., Wu T., Vaillancourt C. Acupuncture for menopausal hot flushes. Cochrane Database Syst Rev. 2013;7:Cd007410. doi: 10.1002/14651858.CD007410.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou W., Lonqhurst J.C. Neuroendocrine mechanisms of acupuncture in the treatment of hyertension. Evid Based Complement Alternat Med. 2012;2012:878673. doi: 10.1155/2012/878673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cevik C., Iseri S.O. The effect of acupuncture on high blood pressure of patients using antihypertensive drugs. Acupunct Electrother Res. 2013;38:1–15. doi: 10.3727/036012913x13831831849448. [DOI] [PubMed] [Google Scholar]
- 16.Zhao X.F., Hu H.T., Li J.S., Shang H.C., Zheng H.Z., Niu J.F. Is acupuncture effective for hypertension?. A systematic review and meta-analysis. PLOS ONE. 2015;10:e0127019. doi: 10.1371/journal.pone.0127019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baek Y.H., Jang E.S., Park K.H., Yoo J.H., Jin H.J., Lee S.W. Development and validation of brief KS-15 (Korea Sasang Constitutional Diagnostic Questionnaire) based on body shape, temperament and symptoms. J Sasang Constitut Med. 2015;27:211–221. [Google Scholar]
- 18.Yeo M.K., Park K.H., Bae K.H., Jang E.S., YS L. Development on the questionnaire of cold-heat pattern identification based on usual symptoms for health promotion—focused on reliability study. Korean J Orient Physiol Pathol. 2016;30:116–123. [Google Scholar]
- 19.Haker E., Egerkvist H., Bjerring P. Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activites in healthy subjects. J Auton Nerv Syst. 2000;79:52–59. doi: 10.1016/s0165-1838(99)00090-9. [DOI] [PubMed] [Google Scholar]
- 20.Mori H., Nishijo K., Kawamura H., Abo T. Unique immunomodulation by electro-acupuncture in humans possibly via stimulation of the autonomic nervous system. Neurosci Lett. 2002;320:21–24. doi: 10.1016/s0304-3940(02)00012-5. [DOI] [PubMed] [Google Scholar]
- 21.Kim J.S., Hwang M.W., Lee J.H., Lee E.J., Koh B.H., Yoo J.H. Development of clinical practice guidenes for Sasang constitutional medicine symptomatology: purpose, development strategy and procedure. J Sasang Constitut Med. 2013;25:23–33. [Google Scholar]
- 22.Lee Y.S., Kim S.H., Lee S.W. Researches trend of Korea Institute of Oriental Medicine in Sasang Constitution Field, from 2007 to 2010. Korea J Oriental Med. 2012;18:59–74. [Google Scholar]
- 23.Lee J., Lee E., Yoo J., Kim Y., Koh B. The sasang constitutional types can act as a risk factor for hypertension. Clin Exp Hypertens. 2011;33:525–532. doi: 10.3109/10641963.2011.561901. [DOI] [PubMed] [Google Scholar]
- 24.http://www.nlm.nih.gov/medlineplus/ency/article/000894.htm.
- 25.Kim J.H., Jung H.J., Kim T.H., Lee S., Kim J.E., Kang K.W. Auricular acupuncture for prehypertension and stage 1 hypertension: study protocol for a pilot multicentre randomised controlled trial. Trials. 2013;14:303. doi: 10.1186/1745-6215-14-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaufman J.S., Asuzu M.C., Mufunda J., Forrester T., Wilks R., Luke A. Relationship between blood pressure and body mass index in lean populations. Hypertension. 1997;30:1511–1516. doi: 10.1161/01.hyp.30.6.1511. [DOI] [PubMed] [Google Scholar]
- 27.Jenkinson C., Stewart-Brown S., Petersen S., Paice C. Assessment of the SF-36 version 2 in the United Kingdom. J Epidemiol Community Health. 1999;53:46–50. doi: 10.1136/jech.53.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jonnalagadda S.S., Mitchell D.C., Smiciklas-Wright H., Meaker K.B., Van Heel N., Karmally W. Accuracy of energy intake data estimated by a multiple-pass, 24-hour dietary recall technique. J Am Diet Assoc. 2000;100:303–308. doi: 10.1016/s0002-8223(00)00095-x. quiz 309–11. [DOI] [PubMed] [Google Scholar]
- 29.Lee MSWMK, Kim S.A., Oh S.I., Kwak C.S. Reproducibility of nutrient intake estimated by three-day 24-hour dietary recall of middle-aged subjects for 6 month intervals. Korean J Community Nutr. 2003;8:603–609. [Google Scholar]
- 30.Lee P.H., Macfarlane D.J., Lam T.H., Stewart S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115. doi: 10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chun M.Y. Validity and reliability of Korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med. 2012;33:144–151. doi: 10.4082/kjfm.2012.33.3.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beck A.T., Ward C.H., Mendelson M., Mock J., Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 33.Rhee M.K., Lee Y.H., Jung H.Y., Choi J.H., Kim S.H., Kim Y.K. A standardization study of Beck Depression Inventory II—Korean version (K-BDI) Korean J Psychopathol. 1995;4:96–104. [Google Scholar]
- 34.Choi S.M., Kang T.Y., JM W. Development and validation of a modified form of the stress response inventory for workers. J Korean Neuropsychiatr Assoc. 2006;45:541–553. [Google Scholar]
- 35.Buysse D.J., Reynolds C.F., 3rd, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 36.Taylor R.R., Jason L.A., Torres A. Fatigue rating scales: an empirical comparison. Psychol Med. 2000;30:849–856. doi: 10.1017/s0033291799002500. [DOI] [PubMed] [Google Scholar]
- 37.Zhang J., Ng D., Sau A. Effects of electrical stimulation of acupuncture points on blood pressure. J Chiropr Med. 2009;8:9–14. doi: 10.1016/j.jcm.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yin C., Seo B., Park H.J., Cho M., Jung W., Choue R. Acupuncture, a promising adjunctive therapy for essential hypertension: a double-blind, randomized, controlled trial. Neurol Res. 2007;29(Suppl 1):S98–S103. doi: 10.1179/016164107X172220. [DOI] [PubMed] [Google Scholar]
- 39.Kalish L.A., Buczynski B., Connell P., Gemmel A., Goertz C., Macklin E.A. Stop Hypertension with the Acupuncture Research Program (SHARP): clinical trial design and screening results. Control Clin Trials. 2004;25:76–103. doi: 10.1016/j.cct.2003.08.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.