Abstract
Introduction
The rotating hinge prosthesis was originally used and designed as a primary total knee arthroplasty implant, but was hampered due to poor outcomes and catastrophic failures. Newer rotating hinge implants can be utilized in complex revision total knee arthroplasties when appropriately indicated, but their outcome data is very difficult to interpret due to the strict and varied indications for use and subsequently small number of procedures performed. The goal of this review is to evaluate the current evidence on large cohort, rotating hinge knee prostheses used in the revision setting, in order to provide a clearer understanding of the indications, outcomes and complications.
Methods
The PubMed database was utilized to search the available literature regarding “hinged knee,” or “rotating hinge” devices. Exclusion criteria included papers focusing on primary arthroplasty, revision for oncologic issues, one-stage revision for infection or studies with less than fifty cases.
Results
Review of 115 abstracts after initial search, led to ten studies in the literature that met our inclusion and exclusion criteria. The data shows that rotating hinge knee implants have good survivorship ranging from 51% to 92.5% at 10 years post-operatively. Complication rates range from 9.2% to 63% with infection and aseptic loosening as the most common complications.
Conclusion
Rotating hinge knee prostheses are most commonly indicated for infection, aseptic loosening, instability and bone loss in the literature. They have good outcome scores and survivorship, but continue to have high complication and revision rates. The implant is a good option when utilized appropriately for patients that are not candidates for less constrained devices.
Keywords: Hinged knee, Rotating hinge, Revision TKA, Outcomes, Complications
1. Introduction
The rotating hinge knee prosthesis was originally used and designed as a primary total knee arthroplasty implant. Early constructs were fixed hinge designs that allowed motion only in the sagittal plane of flexion and extension.1 This stiff device did not allow for varus or valgus tilt, axial rotation or distraction, and led to transfer of force to the bone-cement interface and ultimately failure of the arthroplasty due to loosening or fracture.2 With high initial complication rates and the subsequent design of non-linked constrained components, the hinged prosthesis was mostly abandoned for use mainly in oncologic cases.3 Newer designs consisted of a rotating hinge construct that lowered force transmission to the bone interface with additional focus on an improved patellofemoral articulation.4, 5, 6, 7, 8, 9, 10, 11 Modular parts and metaphyseal sleeves and cones were developed to more accurately reproduce the joint line, manage severe bone loss and improve fixation.11, 12, 13, 14, 15 Outcome data regarding rotating hinge knee prostheses is very difficult to interpret due to small cohorts, old prosthesis designs, mixed indications and primary usage of hinged implants. As a result, outcomes and complication rates may not be clearly delineated in the literature. The goal of this study was to evaluate large cohort (greater than 50 cases) studies or series of rotating hinge knee prostheses used in the revision setting, in order to evaluate and provide a consensus for the indications, outcomes and complication rates.
2. Methods
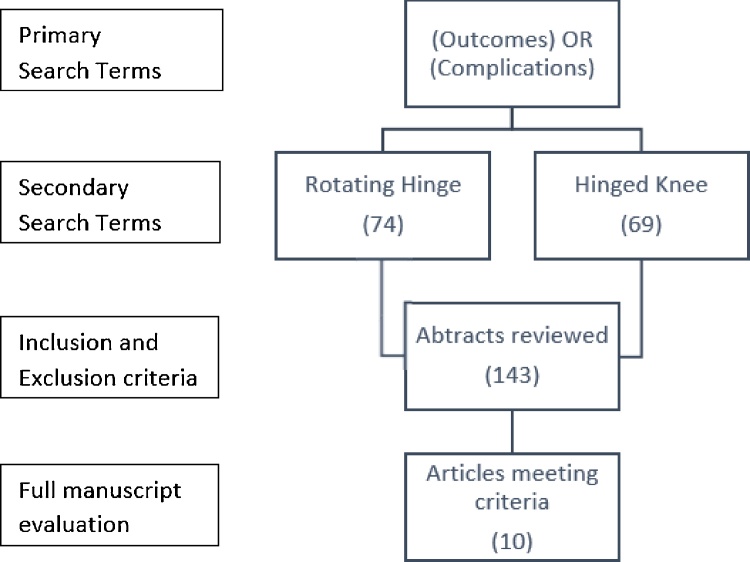
The PubMed database was utilized to search the available literature with the following primary and secondary keywords: “outcomes” OR “complications” with “hinged knee,” or “rotating hinge.” We included all articles published after January 1, 2000 with greater than 50 procedures being studied. Exclusion criteria included papers focusing on primary arthroplasty, revision for oncologic issues or one-stage revision for infection. Literature utilizing total femur, distal femur or proximal tibia replacements were not included. All abstracts were thoroughly reviewed by the lead author for adherence to inclusion and exclusion criteria. Articles that met both inclusion and exclusion criteria underwent a second review of the complete article to confirm satisfactory criteria requirements (Fig. 1). Ten articles met all inclusion and exclusion criteria, and each was reviewed for indications, survivorship, outcome scores, revisions, complication rates and common complications. Specific details for each article reviewed are summarized in the attached table with salient data discussed in the subsequent results and discussion sections (Table 1).
Fig. 1.
Flowchart for article selection.
Table 1.
Review of Published Literature for the Use of Rotating Hinge Prostheses in Revision Total Knee Arthroplasty.
| Study | No. of Knees | Follow up Range (mean) | Indications | Implant type | Survivorship | Clinical Outcomes | Revisions | Complication Rate | Post-operative Complications |
|---|---|---|---|---|---|---|---|---|---|
| Cottino et al. (2017) | 408 (334 revision) | 24–144 (48) months | Infection (35%), osteoarthritis (18%), instability (15%), aseptic loosening (13%), periprosthetic fracture (13%), nonunion (5%) |
Howmedica modular rotating hinge (59%), Zimmer NexGen RH Knee (31%), DePuy S-ROM Noiles Rotating Hinge (9%), Biomet Finn Rotating Hinge (0.5%) | 84.5% at 5 yrs, 71.3% at 10 yrs |
Knee Society Score: 51 to 81 Knee Society Functional Score: 26 to 36 | Total 59 (14.5%): Septic 21 (5.1%), aseptic 38 (9.3%) | 12% | Deep infection (11%), delayed wound healing (3%), stiffness (2.5%), aseptic loosening (2.5%), superficial infection (1.2%), |
| Farid et al. (2015) | 142 (131 revision) | 24–163 (57) months | Infection (43%), arthrofibrosis (11%), aseptic loosening (11%), instability (11%), periprosthetic fracture (5%) | Biomet Orthopedic Salvage System | 73% at 5 yrs, 51% at 10 yrs |
Knee Society Score: 36 to 77 | Total 49 (34.5%) Septic 21 (14.8%), aseptic 28 (19.7%) | <3 months (27%), >3 months (56%) | Aseptic loosening (16%), deep infection (15%), periprosthetic fracture (7%), quad/patellar tendon rupture (4%) |
| Guirea et al (2014) | 152 (62 revision) | 24 months | Osteoarthritis (56%), infection (13%), aseptic loosening (13%), instability (15%) | Aesculap EnduRo rotating hinge | 85.4% at 2 years | Knee Society Score: 32 to 81 Knee Society Functional Score: 32 to 56 | Total 14 (9.2%) Septic 5 (3.3%), aseptic 9 (5.9%) | 9.2% | Deep infection (3%), aseptic loosening (1%), periprosthetic fracture (1%), extensor dysfunction (1%) |
| Shen et al. (2014) | 475 (94 hinged knee) | 3–10 (6) years | Infection (31%), aseptic bone loss (69%) | N/A | N/A | N/A | Total 21 (22.3%) Septic 11 (11.7%), aseptic 10 (10.6%) |
22% | Infection (12%), aseptic loosening (11%), extensor mechanism failure (2%) |
| Baier et al (2013) | 78 | 60–108 (81) months | Aseptic loosening (45%), component malrotation (23%), instability (18%), stiffness (9%) | DePuy TC2 rotating hinge | N/A | Knee Society Score: 57 to 71 Knee Society Functional Score: 61 | Total 7 (8.9%) Septic 3 (4%), aseptic 4 (6%) | 28% | Arthrofibrosis (7%), aseptic loosening (6%), deep infection (4%), patellar complication (3%) |
| Smith et al (2013) | 111 (59 rotating hinge) | N/A | Infection (46%), instability (34%), aseptic loosening (24%), | Stryker Kinematic 1&2, Stryker Duracon Modular Rotating Hinge, Depuy S-ROM Revision Hinge, Biomet Finn Rotating Hinged | 77% at 1 yr, 52% at 5 yrs |
N/A | Total 28 (47.5%): Septic 14 (23.7%), aseptic 13 (22.0%) | 63% | Infection (24%), soft tissue failure (12%), aseptic loosening (7%), periprosthetic fracture (5%) |
| Hossain et al (2010) | 349 (74 rotating hinge) | 12–120 (58) months | Infection (33%), aseptic loosening (15%) | SMILES prosthesis, Styrker MRH, Depuy Noiles S-ROM | 92.5% at 10 yrs | Knee Society Score: 31 to 84 | Total 5 (6.8%): Septic 2 (2.7%), aseptic 3 (4.1%) | 7% | Aseptic loosening (3%), infection (3%), periprosthetic facture (1%) |
| Deehan et al (2008) | 72 (57 revision) | 3–18 (10) years | Aseptic loosening/bone loss (47%), instability (24%), infection (15%) | Howmedica kinematic rotating hinge | 90% at 5 yrs | Knee Society Score: 28 to 74 | Total 3 (4.2%) Septic 2 (2.8%), aseptic 1 (1.4%) | 36% | Persistent pain (14%), extensor dysfunction (7%), infection (7%), periprosthetic fracture (4%) |
| Joshi et al (2008) | 78 | 56–130 (94) months | Aseptic loosening (60%), instability (31%), periprosthetic fracture (5%), extensor mechanism failure (4%) | Waldemar Endo-Model Rotational Knee Prosthesis | 73% | Knee Society Score: 38 to 86 Knee Society Functional Score: 33 to 61 | Total 8 (12.8%) Septic 2 (2.6%), Aseptic 8 (10.3% | 27% | Instability (5%), aseptic loosening (5%), infection (3%) |
| Springer et al (2001) | 69 (57 revision) | 24–199 (75) months | Instability (43%), nonunion (14%), periprosthetic fracture (13%), infection 9%) | Howmedica kinematic rotating hinge | N/A | Knee Society Score: 33 to 77 Knee Society Functional Score: 19 to 23 | Total 19 (27%) Septic 5 (7.2%), Aseptic 14 (20.2%) | 49% | Deep infection (15%), aseptic loosening (15%), patellar complication (13%), periprosthetic fracture (10%), superficial infection (9%) |
3. Results
3.1. Indications and contraindications
The most common modes of failure of a primary total knee arthroplasty are aseptic loosening, infection, pain and instability with varying incidences based upon the literature. Instability has been shown to account for approximately 25% of all revisions within 1 year and 20% of all cases beyond 5 years.16 A recent review of the National Joint Registries by Khan et al. in 2016 showed that aseptic loosening is the cause for TKA revision in 30% of cases, with infection causing 15% and non-specific pain the reason for 10% of revisions.17 Kim et al. retrospectively reviewed 256 revision TKAs and found that 45% were due to polyethylene wear, 26% from infection and 17% due to implant loosening.18 Sharkey et al. reported a similar infection incidence of 27% in a retrospective review of 781 revision TKA. Conversely, they found that 40% were due to component loosening and only 7.5% were due to knee instability.19 Finally, Kamath et al. reviewed the National Inpatient Sample database of 301,718 revision TKAs, and reported infection as the most common cause of revision at 25%, with mechanical loosening at 18.5%.20
For this review, we excluded literature on primary osteoarthritis and oncologic issues as possible indications, and focused on specific cases for revision. The most common indications for rotating hinge revision TKA were: infection, aseptic loosening, instability and bone loss. Smith et al. cited 46% of all revisions requiring rotating hinge implant, and Farid et al. reported 43% of all cases were indicated for infection. Farid et al. stated that all cases had severe periarticular bone loss and soft tissue deficiencies, with an average of 4 prior arthroplasties, however, Smith et al. did not delineate why a rotating hinge implant was used instead of a less constrained device.1, 21 In regards to aseptic loosening, Joshi et al. reported 60% of their revision rotating hinge implants were indicated as a result of polyethylene wear leading to aseptic loosening.22 Baier et al. indicated 45% of their rotating hinge cases due to aseptic loosening, if patients complained of weight-bearing pain or had osteolysis on serial radiographs.23 Again, there was no statement in either study on why a rotating hinge was used instead of a less constrained device. Deehan et al. indicated 24% of patients for ligamentous instability, while Smith et al. and Joshi et al. indicated 34% and 30% respectively.11, 14, 22 Finally, Shen et al. indicated 69%, Deehan 47% and Springer 43% of their hinged revision total knee arthroplasty cases for significant bone loss.7, 14, 24
3.2. Outcomes and complications
Cottino et al. in 2017 published the largest series to date on rotating hinge prostheses used in non-oncologic cases, evaluating 408 knees undergoing arthroplasty with a rotating hinge. Their results, which were consistent with previous data, showed significant improvement in knee functional scores and a cumulative revision incidence of 9.7% at 2 years and 22.5% at 10 years, with septic failures accounting for the majority of revisions. When evaluating for only aseptic loosening, they found a much lower cumulative incidence of 1.7% at 2 years and only 4.5% at 10 years when compared to previous data. In the same series, they had 22 intra-operative complications including periprosthetic femur/tibia fractures and patellar tendon avulsions. Survivorship was found to be 84.5% at 5 years and 71.3% at 10 years. Post-operatively, the majority of complications, not including septic failure, were delayed wound healing or decreased range of motion. Finally, there was a trend for lower risk of revision in patients with metaphyseal cones used during implantation, likely due to long term biological fixation to host bone and decreased stress across the bone-cement interface.25
When comparing the other studies in this review to Cottino et al., there was consistent improvement in knee scores in all papers with Springer et al. reporting only modest improvement in functional knee scores after rotating hinge implantation.7 Survivorship was also similar with Hossain et al. having a 92.5% survivorship at 10 years and Deehan et al. reporting 90% at 5 years.14, 26 However, Smith et al. reported worse survivorship of 52% at 5 years and Farid et al. cited 51% at 10 years.1, 21 Both groups hypothesized that these lower survivorship rates were due to the higher number of patients with a prior diagnosis of infection, which put them at a higher risk for failure. Revision rates were quite variable among all studies with rates as low as 8.9% and as high as 47.5% (Table 1). Cottino et al. had one of the lowest complication rates at 12%, with Shen at al. having a 22% and Baier et al. having a 28% complication rate.23, 24, 25 However, Smith et al. had a very high complication rate of 63% and Springer et al. also had a high complication rate of 49% at the end of their study.7, 11
4. Discussion
The original hinge designs were fixed hinge devices that only allowed movement in one plane, flexion and extension. The lack of rotation at the joint line led to a transmission of force at the bone-implant interface, causing aseptic loosening and fracture.11 These first generation hinged devices were commonly designed with metal-to-metal articulations that increased failure gut to particulate wear debris fretting, and often fracture.1 It was observed that a natural external rotation of approximately 9–13 ° through the knee joint occurred during walking, which prompted design of a second generation of prosthesis.27 These next set prostheses were developed with a focus on providing a rotational axis to limit the transmission of force through the bone-cement interface.28 These devices showed promise with good early outcomes, but continued to have an unacceptably high complication rate, as high as 80% in the literature.1, 27 The first- and second-generation implants have since been replaced with the new third generation implant that is the basis for modern rotating hinge knee devices.
The current rotating hinge knee system design has been translated for incorporation in various modular segmental or non-segmental distal femoral replacements, proximal tibial replacements and total femur replacements. Several improvements in conventional hinge knee design have taken place to improve outcomes and expand its use in primary and revision TKA settings. Anatomical design of components, such as an asymmetric tibia, allows the surgeon to customize the tibial component to each patient’s anatomic requirements. Design changes to the patellofemoral component, including deepening of the anterior femoral groove, aims to improve the lateral subluxation resistance and provide smooth patellar tracking.1 Central location of the hinge axis keeps the femoral condyles in a consistent sagittal plane allowing for normal patellar tracking. In many conventional hinge designs, the hinge mechanism bears compressive load until full extension is achieved. Condylar load sharing designs help ensure condylar loading for the entire knee range of motion, which decreases the stress on the hinge link and lowers wear of the hinge device. In the native knee, the femur naturally rests in internal rotation on the tibia during extension, but rotates externally through flexion as the tight medial collateral ligament holds the medial femoral condyle in position, acting as a medial pivot. As the knee continues to flex, the concave anatomy of the medial tibial plateau helps to facilitate posterior roll-back of the lateral femoral condyle on the tibia as the femur externally rotates. This natural rotation reverses during extension to provide a “screw home” mechanism to help lock the knee for standing.29 Kinematic guided motion was introduced in rotating hinge knee implants in order to help re-create this natural range of motion by providing medial pivot, lateral roll back, and screw home mechanisms.28
Designs with center of rotation posteriorly can cause non-anatomic opening of the joint, which may result in increased stress on cement surfaces and accelerated polyethylene wear. Hinge-post modularity allows for ease of implantation without excessive distraction during component assembly while also maintaining adequate jump height. The ability to change instrumentation can be beneficial by easing the intra-operative conversion from a less constrained implant to a hinge knee. The ability to use modular components and metaphyseal fixation devices is also crucial as improved metaphyseal fixation has been shown to improve survival rates of these devices.28
Despite the varying data in the literature for revision of a total knee arthroplasty, it is the Orthopedic Surgeon’s responsibility to fully evaluate each individual patient to determine the most appropriate surgical management. The basis for component selection is then predicated on the inherent stability of the knee after the primary procedure. Patients with stable knees may be managed with less constrained constructs based upon the type and cause of instability (Table 1). In the setting of revision arthroplasty, rotating hinge knee implants should be reserved for knees with global instability due to 1) significant bone loss and subsequent loss of collateral ligament insertion due to infection, trauma, osteolysis or 2) complete loss of ligamentous stability due to multiple revisions, radical debridement associated with infections and stripping of ligamentous complex from distal femur in an extremely stiff knee. Secondary indications include usage in oncologic reconstruction, compromised extensor mechanism function, severe recurvatum, peri-prosthetic fractures, conversion from arthrodesis, complex revisions in patients with neuromuscular disease and severe flexion/extension gap imbalance in which the knee is at risk for dislocation with an unlinked prosthesis (which provides only varus-valgus stability).30, 31, 32
Early fixed-hinged knee designs had very high complication rates and poor outcomes due to aseptic loosening and fracture at the bone-cement interface due to excessive transmission of force through the implant.11, 33, 34, 35, 36, 37 After the rotating hinge design improved the mechanics of the prosthesis, review of the current literature showed significant improvements in both functional knee scores and survivorship (Table 1).
Even after focusing on articles with greater than 50 cases of rotating hinge knee implants for revision TKA, excluding oncologic and primary cases, the data is very heterogeneous and difficult to compare. Each article reviewed utilized different implants and many of the studies mixed primary cases with revisions, or distal femoral replacements with rotating hinge implants. Revision and complication rates were difficult to compare as each paper had different definitions of complications and often mixed revision cases with reoperation for other post-operative complications.
Despite these limitations, this manuscript provides the most focused review of large cohort studies on rotating hinge knee implants in the literature. This information can help guide orthopaedic surgeons indicate and plan for the usage of a rotating hinge device in the future.
5. Conclusion
Rotating hinge knee prostheses are an important tool in an Orthopaedic Surgeon’s armamentarium in the setting of complex knee revision arthroplasty. The designs have been improved significantly over the last several decades with the current literature showing improved clinical outcomes, reasonable survivorship while also having higher complication rates. Rotating hinge total knee arthroplasties are most commonly indicated as treatment for infection, aseptic loosening, instability and bone loss. As such, they must be utilized only when appropriately indicated, with proper technique, when all other implants would be ineffective, while being cognizant of the high risk for complications in the post-operative period.
References
- 1.Manning D.W., Chiang P.P., Freiberg A.A. Revision Total Knee Arthroplasty. 2005. Hinge implants; pp. 219–236. [Google Scholar]
- 2.Morgan H., Battista V., Leopold S.S. Constraint in primary total knee arthroplasty. J Am Acad Orthop Surg. 2005;13(8):515–524. doi: 10.5435/00124635-200512000-00004. http://www.jaaos.org/content/13/8/515. long%5Cnhttp://www.ncbi.nlm.nih.gov/pubmed/16330513 [DOI] [PubMed] [Google Scholar]
- 3.Barrack R.L. Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res. 2001;392:292–299. doi: 10.1097/00003086-200111000-00038. http://www.ncbi.nlm.nih.gov/pubmed/11716398 [DOI] [PubMed] [Google Scholar]
- 4.Ruggieri P., Mavrogenis A.F., Pala E., Abdel-Mota’al M., Mercuri M. Long term results of fixed-hinge megaprostheses in limb salvage for malignancy. Knee. 2012;19(5):543–549. doi: 10.1016/j.knee.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Höll S., Schlomberg A., Gosheger G. Distal femur and proximal tibia replacement with megaprosthesis in revision knee arthroplasty: a limb-saving procedure. Knee Surg Sport Traumatol Arthrosc. 2012;20(12):2513–2518. doi: 10.1007/s00167-012-1945-2. [DOI] [PubMed] [Google Scholar]
- 6.Myers G.J.C., Abudu A.T., Carter S.R., Tillman R.M., Grimer R.J. The long-term results of endoprosthetic replacement of the proximal tibia for bone tumours. J Bone Jt Surg – Br Vol. 2007;89-B(12):1632–1637. doi: 10.1302/0301-620X.89B12.19481. [DOI] [PubMed] [Google Scholar]
- 7.Springer B.D., Hanssen A.D., Sim F.H., Lewallen D.G. The kinematic rotating hinge prosthesis for complex knee arthroplasty. Clin Orthop Relat Res. 2001;392:283–291. doi: 10.1097/00003086-200111000-00037. [DOI] [PubMed] [Google Scholar]
- 8.Nishitani K., Nakagawa Y., Suzuki T., Koike K., Nakamura T. Rotating-hinge total knee arthroplasty in a patient with genu recurvatum after osteomyelitis of the distal femur. J Arthroplasty. 2007;22(4):630–633. doi: 10.1016/j.arth.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 9.Gehrke T., Kendoff D., Haasper C. The role of hinges in primary total knee replacement. Bone Joint J. 2014;96-B(11 Suppl. A):93–95. doi: 10.1302/0301-620X.96B11.34143. [DOI] [PubMed] [Google Scholar]
- 10.Rand J.A., Chao E.Y., Stauffer R.N. Kinematic rotating-hinge total knee arthroplasty. J Bone Joint Surg Am. 1987;69:489–497. [PubMed] [Google Scholar]
- 11.Smith T.H., Gad B.V., Klika A.K., Styron J.F., Joyce T.A., Barsoum W.K. Comparison of mechanical and nonmechanical failure rates associated with rotating hinged total knee arthroplasty in nontumor patients. J Arthroplasty. 2013;28(1) doi: 10.1016/j.arth.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Neumann D.R.P., Hofstaedter T., Dorn U. Follow-up of a modular rotating hinge knee system in salvage revision total knee arthroplasty. J Arthroplasty. 2012;27(5):814–819. doi: 10.1016/j.arth.2011.08.015. [DOI] [PubMed] [Google Scholar]
- 13.Kowalczewski J., Marczak D., Synder M., Sibiński M. Primary rotating-hinge total knee arthroplasty: good outcomes at mid-term follow-up. J Arthroplasty. 2014;29(6):1202–1206. doi: 10.1016/j.arth.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Deehan D.J., Murray J., Birdsall P.D., Holland J.P., Pinder I.M. The role of the rotating hinge prosthesis in the salvage arthroplasty setting. J Arthroplasty. 2008;23(5):683–688. doi: 10.1016/j.arth.2007.05.055. [DOI] [PubMed] [Google Scholar]
- 15.Meneghini R.M., Lewallen D.G., Hanssen A.D. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg-Am Vol. 2009;91(Suppl. 2):131–138. doi: 10.2106/JBJS.H.01061. [DOI] [PubMed] [Google Scholar]
- 16.Browne J.A., Parratte S.P.M. Instability In total knee arthroplasty. In: Scott W.N., Diduch D.R., Hanssen A.D., Iorio R., Long W.J., editors. Insall & Scott Surgery of the Knee. 6th ed. Elsevier; Philadelphia, PA: 2017. pp. 1927–1935. [Google Scholar]
- 17.Khan M., Osman K., Green G., Haddad F.S. The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint J. 2016;98-B(1):105–112. doi: 10.1302/0301-620X.98B1.36293. [DOI] [PubMed] [Google Scholar]
- 18.Kim K.T., Lee S., Ko D.O., Seo B.S., Jung W.S., Chang B.K. Causes of failure after total knee arthroplasty in osteoarthritis patients 55 years of age or younger. Knee Surg Relat Res. 2014;26(1):13–19. doi: 10.5792/ksrr.2014.26.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharkey P.F., Lichstein P.M., Shen C., Tokarski A.T., Parvizi J. Why are total knee arthroplasties failing today – has anything changed after 10 years? J Arthroplasty. 2014;29(9):1774–1778. doi: 10.1016/j.arth.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 20.Kamath A.F., Ong K.L., Lau E. Quantifying the burden of revision total joint arthroplasty for periprosthetic infection. J Arthroplasty. 2015;30(9):1492–1497. doi: 10.1016/j.arth.2015.03.035. [DOI] [PubMed] [Google Scholar]
- 21.Farid Y.R., Thakral R., Finn H.A. Intermediate-term results of 142 single-design, rotating-hinge implants: frequent complications may not preclude salvage of severely affected knees. J Arthroplasty. 2015;30(12):2173–2180. doi: 10.1016/j.arth.2015.06.033. [DOI] [PubMed] [Google Scholar]
- 22.Joshi N., Navarro-Quilis A. Is there a place for rotating-hinge arthroplasty in knee revision surgery for aseptic loosening? J Arthroplasty. 2008;23(8):1204–1211. doi: 10.1016/j.arth.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 23.Baier C., Lüring C., Schaumburger J. Assessing patient-oriented results after revision total knee arthroplasty. J Orthop Sci. 2013;18(6):955–961. doi: 10.1007/s00776-013-0467-1. [DOI] [PubMed] [Google Scholar]
- 24.Shen C., Lichstein P.M., Austin M.S., Sharkey P.F., Parvizi J. Revision knee arthroplasty for bone loss: choosing the right degree of constraint. J Arthroplasty. 2014;29(1):127–131. doi: 10.1016/j.arth.2013.04.042. [DOI] [PubMed] [Google Scholar]
- 25.Cottino U., Abdel M.P., Perry K.I., Mara K.C., Lewallen D.G., Hanssen A.D. Long-term results after total knee arthroplasty with contemporary rotating-hinge prostheses. J Bone Joint Surg Am. 2017;99(4):324–330. doi: 10.2106/JBJS.16.00307. [DOI] [PubMed] [Google Scholar]
- 26.Hossain F., Patel S., Haddad F.S. Vol. 468. 2010. Midterm assessment of causes and results of revision total knee arthroplasty; pp. 1221–1228. (Clinical Orthopaedics and Related Research). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guenoun B., Latargez L., Freslon M., Defossez G., Salas N., Gayet L.E. Complications following rotating hinge endo-modell (Link??) knee arthroplasty. Orthop Traumatol Surg Res. 2009;95(7):529–536. doi: 10.1016/j.otsr.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 28.Bottlang M., Erne O.K., Lacatusu E., Sommers M.B., Kessler O. A mobile-bearing knee prosthesis can reduce strain at the proximal tibia. Clin Orthop Relat Res. 2006;447:105–111. doi: 10.1097/01.blo.0000203463.27937.97. [DOI] [PubMed] [Google Scholar]
- 29.Sharma A.K.R. Contact mechanics of the human knee. In: Scott W.N., Diduch D.R., Hanssen A.D., Iorio R., Long W.J., editors. Insall & Scott Surgery of the Knee. Elsevier; 6th ed. Philadelphia, PA: 2018. pp. 329–337. [Google Scholar]
- 30.Dennis D.A., Berry D.J., Engh G. Revision total knee arthroplasty. J Am Acad Orthop Surg. 2008;16(8):442–454. doi: 10.5435/00124635-200808000-00003. http://www.jaaos.org/content/16/8/442.abstract [DOI] [PubMed] [Google Scholar]
- 31.Lombardi A.V. Management of knee instability: use of hinged implants. In: Scuderi G.R., Tria A.J. Jr, Long W.J., Kang M.N., editors. Techniques in Revision Hip and Knee Arthroplasty. 1st ed. Elsevier; Philadelphia, PA: 2015. pp. 119–129. [Google Scholar]
- 32.Sculco T.P. The role of constraint in total knee arthoplasty. J Arthroplasty. 2006;21(Suppl. 4):54–56. doi: 10.1016/j.arth.2006.02.166. [DOI] [PubMed] [Google Scholar]
- 33.Lettin A.W., Deliss L.J., Blackburne J.S., Scales J.T. The Stanmore hinged knee arthroplasty. J Bone Joint Surg Br. 1978;60-B(3):327–332. doi: 10.1302/0301-620X.60B3.681408. http://www.ncbi.nlm.nih.gov/pubmed/681408 [DOI] [PubMed] [Google Scholar]
- 34.Karpinski M.R., Grimer R.J. Hinged knee replacement in revision arthroplasty. Clin Orthop Relat Res. 1987;220:185–191. [PubMed] [Google Scholar]
- 35.Jones E.C., Insall J.N., Inglis A.E., Ranawat C.S., Anonymous GUEPAR knee arthroplasty results and late complications. Clin Orthop Relat Res. 1979;140:145–152. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=477066 [PubMed] [Google Scholar]
- 36.LeNobel J., Patterson F.P. GUEPAR total knee prosthesis. Experience at the Vancouver general hospital. J Bone Joint Surg Br. 1981;63-B(2):257–260. doi: 10.1302/0301-620X.63B2.7217152. http://www.ncbi.nlm.nih.gov/pubmed/7217152 [DOI] [PubMed] [Google Scholar]
- 37.Bargar W.L., Cracchiolo A., Jr, Amstutz H.C. Results with the constrained total knee prosthesis in treating severely disabled patients and patients with failed total knee replacements. J Bone Joint Surg Am. 1980;62(4):504–512. http://www.ncbi.nlm.nih.gov/pubmed/7380852%5Cnpapers2://publication/uuid/8B2DC269-9D30-4AC6-AA60-2EBA1ABBA4BA [PubMed] [Google Scholar]