Abstract
Unicompartmental knee replacement (UKR) is an effective treatment for end-stage, symptomatic unicompartmental osteoarthritis of the knee. However, certain aspects of the procedure are still debated. These areas of discussion include patient selection criteria, implant design and the discrepancy in survival rates between national registries and independent case series. These may contribute in limiting the more widespread acceptance of unicompartmental knee replacement.
The aim of this paper is to review the up-to-date evidence on UKR and discuss the most relevant controversies regarding this procedure.
Keywords: Unicompartmental arthroplasty, Unicompartmental arthritis, Knee arthroplasty, Knee arthritis, Partial knee replacement
1. Introduction
Unicompartmental knee replacement (UKR) is an effective treatment for end-stage, symptomatic osteoarthritis (OA) of the knee that is limited to a single compartment. Despite growing evidence in its favour, many surgeons still consider UKR as a niche option for a limited number of patients. It has been estimated that worldwide only 10% of orthopaedic surgeons perform unicompartmental knee replacements. This number is surprisingly low considering the potential efficacy and safety of a minimally invasive procedure that could be offered to a larger proportion of patients requiring knee replacement surgery. The indications for UKR play an important role in generating these controversies, alongside the discrepancy in clinical results reported in National Joint Registries and case series from high volume centres.
The aim of this paper is to review the up-to-date evidence on medial UKR and discuss the most relevant controversies concerning this procedure.
2. Historical overview
McKeever and MacIntosh first proposed the theory of UKR in the 1950s, with the introduction of a metallic component that was used to replace the tibial surface.1 The results of these procedures were unsatisfactory, with a high incidence of complications and poor functional results.
The first modern unicompartmental designs, the “St. Georg” and the “Marmor Knee”, were introduced in 1969 and 1972, respectively.2 Both presented a polyradial metallic femoral component and a flat tibial component made of polyethylene. Initially, the results were controversial. Wear and polyethylene deformation were the biggest problems, which led to the introduction of metal-backed tibial component.3 In the 1970s and 1980s, the understanding of OA as a pathology of the entire joint and the rising interest in total knee replacement led to a fervent development of these implants. In contrast, UKRs had limited innovation, such that some implants still in use remain almost unchanged.4
In the late 1980s, Goodfellow, Tibrewal et al. believed that some of the disappointments in previous attempts at UKR had arisen from inadequacies in prosthetic design, poor patient selection, and surgical techniques.5 The authors discussed the theoretical requirements of a successful UKR and presented their preliminary results using the Oxford meniscal components in a unicompartmental mode in 25 knees. It is worth noting that in 1976 Goodfellow & O’Connor had initially proposed the use of a meniscal bearing design of knee prosthesis and implanted these for bicompartmental tibiofemoral arthroplasty from 1978. Over the years, many of these issues have been addressed with refinements in prosthetic designs and UKR is widely accepted as a valid procedure in the treatment of unicompartmental osteoarthritis of the knee (Fig. 1, Fig. 2).
Fig. 1.
Preoperative weight-bearing radiographs showing bone-on-bone AMOA. The presence of osteophytes in the lateral compartment is not a contraindication for UKR using the Oxford criteria.
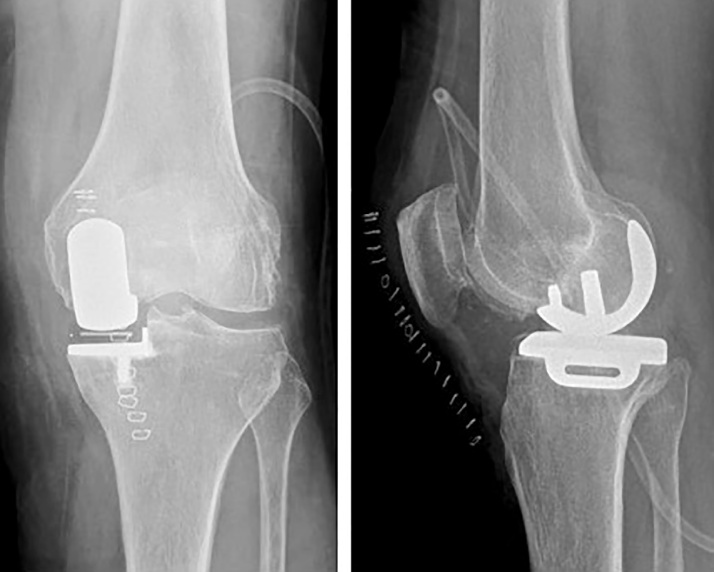
Fig. 2.
Immediate post-operative radiographs showing a mobile-bearing UKR. The joint line in re-established with full thickness cartilage in the lateral compartment.
3. Results of unicompartmental versus total knee replacement
Several studies have confirmed the excellent clinical outcome and survival of unicompartmental knee replacement (fixed or mobile bearing implants), with a reported ten-year survival greater than 90%.6, 7 In a prospective series of 1000 cases, Pandit et al. reported a ten-year survival of 96% for the Oxford Phase 3 Unicompartmental Knee Replacement.8 Some authors have expressed concern regarding the reproducibility of these results in non-designer centres,9 however the results of several studies (Table 1) demonstrate comparable survival rates for independent surgeons worldwide.
Table 1.
Ten-year survival for medial Oxford Phase 3 unicompartmental knees in non-designer studies.
| Study | Year | Location | Number of knees | Ten-year survival rate (95% CI) |
|---|---|---|---|---|
| Faour-Martin et al.10 | 2013 | Valladolid, Spain | 511 | 96.0 |
| Yoshida et al.11 | 2013 | Osaka, Japan | 1279 | 95.4 (91.2–99.7) |
| Kim et al.12 | 2015 | Seoul, South Korea | 166 | 90.5 (85.9–95.0) |
| Edmondson et al.13 | 2015 | East Sussex, United Kingdom | 364 | 88 (83.0–93.0) |
| Emerson et al.14 | 2016 | Texas, United States | 213 | 95.0 (91.8–98.80) |
Recent studies have highlighted the advantages of UKR over total knee replacement (TKR) in patients with medial compartment OA, including reduced blood loss and risk of transfusion,15, 16 better restoration of physiological gait pattern,17 shorter length of stay and a lower 30-day readmission rate,18 better patient-reported pain and function scores and forgotten joint scores.19, 20, 21, 22
Furthermore, a matched comparison of UKA and TKA based on NJR data including over 100,000 knee arthroplasties demonstrated that major medical complications, such as thromboembolism, infection, stroke and myocardial infarction occurred between a quarter and a half times less frequently in UKR than in TKR. Moreover, the mortality was significantly lower for UKR. However, the revision rate of UKR was 2.1 times higher than for TKR.23
In a further matched study on 15,000 patients from the National Joint Registry for England and Wales, the patient reported outcome measures score (PROMS) were superior for UKR (mean Oxford Knee Score (OKS) 38) than TKR (mean OKS 36). In addition, many more patients undergoing UKR achieved an OKS greater than 41.
However, unadjusted data from national registries show a significantly higher revision rate for UKR than for TKR, with the chance of revision of UKR at each estimated time point being more than double that of a TKR (Table 2).24, 25 A higher revision rate was also confirmed when patients were matched: UKR had worse implant survival both for revision (sub-hazard ratio 2·12, 95% CI 1·99–2·26) and for revision/reoperation (1·38, 1·31–1·44) than TKR at 8 years.23
Table 2.
United Kingdom National Joint Registry Kaplan-Meier estimates of the cumulative percentage probability of first revision (95% CI) in knee arthroplasty.
| Study | Arthroplasty | Fixation/Brand | Number of knee joints | Cumulative percentage probability of a first revision (95% CI) if time elapsed since primary operation is: |
||||
|---|---|---|---|---|---|---|---|---|
| 1 year | 3 years | 5 years | 7 years | 10 years | ||||
| UK NJR, 2016 | TKR | Cemented | 737,759 | 0.39 (0.38–0.41) | 1.50 (1.47–1.53 | 2.14 (2.10–2.18) | 2.65 (2.60–2.70) | 3.37 (3.30–3.45) |
| UK NJR, 2016 | TKR | Cementless | 38,428 | 0.58 (0.51–0.66) | 2.10 (1.95–2.26) | 2.89 (2.71–3.08) | 3.42 (3.22–3.64) | 4.19 (3.92–4.48) |
| UK NJR, 2016 | UKR | All | 75,719 | 1.13 (1.05–1.21) | 4.27 (4.12–4.44) | 6.44 (6.24–6.65) | 8.49 (8.24–8.76) | 11.94 (11.53–12.38) |
The interpretation of such data from national registries is controversial and it has been argued that survival “is not an objective measurement and should not be used to compare these two types of implant”, claiming a “different sensitivity of revision rate to clinical failure” for UKR and TKR. This was based on the observation that, of joint replacements with an OKS <20 (poor outcome), only 12% of TKR were revised compared with approximately 63% of UKR.26
Further, as evidenced in Table 3, outcome measures differ significantly between national arthroplasty registries and sample based clinical studies. In a systematic review of UKR with the Oxford partial knee (including 15 studies of which only 1 was based on data from designer surgeons) a 10 year survival rate of 93% was reported6. Contrastingly, UK registry data estimates a 12.04% probability of first revision at 10 years in the same implant.
Table 3.
Comparison of long-term outcomes for the Oxford partial knee in registry data and case series (systematic review of literature).
| Study | Implant | Number of knee joints | Cumulative percentage probability of a first revision (95% CI) if time elapsed since primary operation is: |
||||
|---|---|---|---|---|---|---|---|
| 1 year | 3 years | 5 years | 7 years | 10 years | |||
| UK NJR, 2016 | Oxford UKR | 50,033 | 1.16 (1.07–1.27) | 4.19 (4.00–4.38) | 6.31 (6.07–6.57) | 8.33 (8.02–8.64) | 12.04 (11.54–12.57) |
| Mohammad et al.6 | Oxford UKR | 8658 | 10 year survival rate: | 93% (91.9–93.3) | |||
In addition to the different threshold for revision, other factors may interact in a complex way to explain the higher incidence of revision of UKR and thus bias the comparison of UKR and TKR. Some of these factors are patient-related, such as the differences in the baseline characteristics of patients being offered each procedure. According to the traditional indications, UKR is often performed in younger patients who, because of their activity level, tend to achieve superior functional outcomes and live longer but then also have higher failure rates.23
4. Indications for UKR
The classic indications for UKR were outlined by Kozinn and Scott in 1989. They suggested that the ideal candidate would be a patient with a) isolated medial compartment disease, b) aged less than 60 years, c) low level of physical activity, d) weight less than 82 kg, e) a cumulative angular deformity of less than 15°, f) both cruciate ligaments intact, g) a pre-operative range of flexion of 90°, g) a flexion contracture of <5°, and h) minimal pain at rest, no radiographic or intraoperative evidence of chondrocalcinosis or patello-femoral osteoarthritis. Lastly, the patient should not have an inflammatory arthropathy.27
Many surgeons still follow these indications, although extended criteria are usually applied in relation to age and level of activity.
By contrast, the Oxford group outlined a more liberal set of criteria for mobile-bearing medial UKR based on the pathoanatomy of OA. According to these indications, the ideal candidate for UKR would be a patient with symptomatic anteromedial osteoarthritis (AMOA) or avascular osteonecrosis of the knee.4 AMOA is specific pattern of knee OA with bone on bone wear in the medial compartment, anterior cruciate and medial collateral ligaments that are functionally intact and full-thickness cartilage in the lateral compartment.28
Accordingly, the traditional contraindications, including weight, age, activity, the state of the patellofemoral joint and chondrocalcinosis could be ignored for mobile-bearing UKR.4, 29, 30 Recent studies have confirmed that obesity has no adverse effect on the outcome of fixed bearing UKR.31, 32, 33 Additionally, it has been reported that the presence of lateral osteophytes in a varus knee is not associated with cartilage wear in the lateral compartment and should not be considered as a contraindication to medial UKR.34, 35, 36
Active infection, inflammatory disease, ligamentous instability or medial collateral ligament contracture, absence of the anterior cruciate ligament, and history of high tibial osteotomy remain contraindications for UKR.4
If the indications proposed by Kozinn and Scott are applied to the knee arthroplasty population, it has been reported that around 6% to 12% of patients would be considered as appropriate candidates for UKR,37, 38, 39 whereas up to 50% of patients may be eligible using the more modern Oxford criteria for mobile-bearing UKR.29, 40
5. Surgeon related considerations
Surgeon-related factors include technical skills and non-technical skills. Technical skills play an important role in TKR: it has been demonstrated that high-volume surgeons achieve better results and lower complications.41 This is even more important in UKR, where the revision rate for the lowest volume surgeons is four times higher than that for the highest volume surgeons.42
A further surgeon-related factor is represented by patient selection and indications. The surgeons’ attitude towards UKR and TKR is inevitably reflected in the relative proportions of primary UKR and TKR in his practice. For mobile bearing UKR, it has been demonstrated that surgeons performing UKR in more than 20% of their knee arthroplasties achieve acceptable revision rates, and those who perform around 50% achieve optimal results.43
A recent meta-analysis reviewing the results of the Phase 3 cemented Oxford UKR studying the relative relevance of usage and caseload, revealed that the proportion of UKR performed was more important than the number of procedure per year. With a usage above 20% of volume, the revision rate was low regardless of caseload. In contrast, a usage below 20% of the volume of the practice reflected in a high revision rate, despite the number of procedures performed.44
These results stress the importance of indications, which are key to determining the outcome of UKR. In mobile-bearing UKR, broader indications lead to the best results, which are similar to those reported in case series from high volume centres. This is the case even in the hands of low-volume surgeons if they adhere to the recommended indications.
6. Implant related considerations
6.1. Fixed vs mobile bearing
UKR can be performed using either a fixed bearing (FB) or a mobile bearing (MB). In a prospective study of 48 patients, randomized into either FB or MB UKA, Li et al. found better knee kinematics and lower incidence of radiolucencies with MB but equivalent Knee Society, WOMAC, and SF-36 scores.45 Cheng et al. found equivalent range of motion, limb alignment, patient-reported outcomes, incidence of aseptic loosening, and reoperation rates between the two bearing designs. However, the time to reoperation and failure mode were different. Early failure from bearing dislocation occurred with the MB design while late failure from polyethylene wear occurred with the FB design.46 Kwon et al. used finite element analysis to investigate the effects of PE insert contact pressure and stress in opposite compartments for fixed- and mobile-bearing UKA. They reported that fixed-bearing UKA increased the overall risk of progressive OA in the knee due to higher stress on the opposite compartment. They also found that with mobile bearings lower stress on the opposite compartment reduced the overall risk of progressive OA in the knee. However, the polyethylene insert of mobile-bearing showed pronounced backside stress at the inferior surface.47 In their systematic review, Ko et al. reported that the overall reoperation rate per hundred component years was similar between the mobile bearings (1.39) and fixed bearings (1.38). They also found that the overall incidence of complications is similar for fixed and mobile bearing designs in UKA.48
In a systematic review on the causes of failure of the Oxford Phase 3 UKR, which is the most commonly used MB implant, the incidence of bearing dislocation was 1.5%.49 However a meta-analysis comparing a variety of implants reported a dislocation rate of 0.29% in the MB group.50
6.2. Cemented vs cementless
Cementless UKR have been available for over 20 years. However, their diffusion and development have been limited by the unacceptable failure rate of the first implants. These failures were often related to materials and design issues. In the last ten years, specialist centres have presented the results of modern cementless implants reporting excellent results and survival.
A recent systematic review revealed that “cementless fixation is a safe and effective alternative to cementation in medial unicompartmental knee arthroplasty”. The clinical outcome, reoperation and revision rate were similar to those of cemented implants in case series, with some advantages over cementation such as a lower incidence of radiolucent lines, avoidance of cementation errors and faster surgical time.51
Although cemented and cementless implants had similar performances in case series and RCTs from high volume centres, the revision rate of cementless UKR was almost half that of cemented UKR in the New Zealand Joint Registry (0.67/100 vs 1.33/100 components-year),52 suggesting that cementless fixation has the potential to improve the survival of UKR in national registries.
6.3. Navigation and robotics
Technological advancement in UKR seeks to optimise the precision of manually controlled intra-operative variables which may impact on outcomes and prosthesis survival. Subsequently, several computer navigation and robotic assisted systems have been developed which are focussing on improving the accuracy of lower leg alignment, component positioning and soft tissue balancing. Early results have been promising; in a study of 68 patients at a mean 9 year follow-up, Song reported significantly improved outcomes and pain scores in the navigated UKA group. Furthermore, post-operative X-ray confirmed better coronal alignment in the navigated group, with fewer radiological outliers.53 Similarly, early research suggests robotic assisted systems improve precision and reduce outliers compared to conventional knee arthroplasty. In a cadaveric trial, Citak established more accurate implant positioning in both components using the MAKO robotic system.54 This success translated to clinical practice − with the first 10 patients treated with the MAKO system all within 1.6° of the mechanical axis .55 Moreover, in a study of 52 patients undergoing UKA using the MAKO system, Plate illustrated soft tissue balancing was accurate up to 0.53 mm compared to the operative plan, with 83% of cases within 1 mm at 0°, 30°, 60°, 90°, and 110° of flexion.56
Although these findings suggest the potential to improve the accuracy of implant positioning, so far there is no evidence to show an improvement in clinical outcomes or survival for robotic assisted implants. Further studies are needed to balance the increased reliability and reproducibility of intraoperative variables against the higher costs of navigation and robotic surgery.
7. Cost-effectiveness of UKR
In an era of value-based healthcare, the cost-effectiveness of surgical alternatives for the same clinical condition warrant consideration. Using a Markov analytical model, Ghomrawi calculated lifetime costs, quality-adjusted life year (QALY) gains and incremental cost-effectiveness ratio (ICER) for UKR and TKR. Results in patients over 65 years of age were emphatic – with lower lifetime costs and higher QALYs for UKR. Indeed, the potential societal cost savings for performing UKR rather than TKR was estimated at $84 to $544 million in 2020.57
In younger patients (45 and 55 years of age), TKR had an ICER of $30,300/QALY and $63,000/QALY respectively. However, UKR would become cost-effective with only incremental improvements in implant survivorship (an average 1.5% drop in 10 year revision rate). Soohoo echoed these findings, reporting UKR to have similar lifetime costs and improved effectiveness comparative to TKR in patients aged 65, but only as long as UKR survival was within 3–4 years of TKR survival.58 Smith agreed, suggesting the use of UKR rather than TKR in patients over the age of 70 would lead to savings of approximately £1500 per patient.59
Focused analysis of hospital billing figures favours the cost-effectiveness of UKR further. Shankar reported reduced operative time, fewer transfusions and shorter hospital stays with UKR compared to TKR − resulting in a reduction in total costs of $4846 per patient. Moreover, supply and implant costs were also significantly lower using UKR ($4149) compared to TKR ($5787).60
The results of these analyses of cost-effectiveness suggest the use of UKR in carefully selected patients offers substantial financial benefit alongside QALY gains. Given the anticipated rise in utilisation of knee arthroplasty, the significance of these economic implications should not be ignored.
However, care should be taken in the analysis of cost-effectiveness with regard to clinical decision making, which should always be patient centred.
8. Discussion
Unicompartmental knee replacement is a successful treatment for end-stage, symptomatic anteromedial osteoarthritis of the knee. Compared to TKR, UKR have a lower incidence of complications, morbidity, mortality, a faster recovery, better functional outcomes and is more cost-effective. However, the revision rate is higher.
Despite the controversies around the revision rate as a means of comparison of UKR and TKR, it cannot be ignored and should be taken into consideration when deciding which procedure to perform. The higher risk of revision and reoperation should be balanced against the many advantages of UKR. A matched study on data from the National Joint Registry suggested that “If 100 patients receiving TKR received UKR instead, the result would be around one fewer death and three more reoperations in the first 4 years after surgery”.23
In contrast with the hypothesis raised by Kozin and Scott that the use of broader indications would increase the revision rate, the Oxford group have demonstrated that a usage proportion greater than 20% is related with superior outcomes.43, 44
A higher usage is achievable if broader modern indications are used and traditional contraindications are ignored. While it is not surprising that a higher caseload correlates with superior results, it is interesting to notice that the proportion of usage of UKR is even more important. Hypothetically, this finding can explain part of the discrepancy in revision rate between the national registries and case series from high volume centres.
The NJR (national joint registry UK) reports that for surgeons performing UKR, the most common number of UKR performed every year is one, and the second most common number is two.24 This implies that the surgeon has a low surgical caseload per year or their indications are narrow. Consequently, that surgeon is going to perform a UKR only in those patients in whom he is not happy to perform a TKR, i.e. those who are particularly young and/or without bone-on-bone wear. However it is known that patients with early osteoarthritis (not bone on bone) who undergo arthroplasty are at high risk of achieving poor results, therefore once again highlighting the importance of careful patient selection.61
A few studies have assessed the influence of preoperative MRI findings on the indications and results of UKR focusing on the presence and location of subchondral bone marrow lesions (BMLs) and extent of cartilage loss. Berend et al. concluded that medial tibial BMLs were not associated with inferior outcomes, either in patients with partial- or full-thickness cartilage loss, suggesting that BMLs are not a contraindication for medial UKA.62, 63 In contrast, Hamilton et al. suggested that the evidence of partial thickness cartilage loss is correlated with inferior clinical results and that medial UKR should be performed only in presence of full thickness cartilage loss.61
Altinel and Sharpe both concluded that pre-operative MRI for assessing ACL status was not of sufficient practical nor diagnostic value and thus did not advocate its use prior to UKR.64, 65
Baker et al. recently reported from the NJR UK that the risk of revision decreased as both centre volume and surgeon volume increased for the Oxford implant, the most commonly used in England and Wales. Their study suggested a minimum annual procedure volume of 13 – both for hospital volume and surgeon volume.66
The current evidence suggests that excellent clinical results and survival are achievable with both mobile and fixed bearing UKR, each device having advantages and disadvantages. The debate should be focused on the controversies between UKR and TKR rather than bearing type in UKR.
Cementless fixation is a viable alternative to cementation, with consistent evidence supporting its clinical use. The early data from national registries are encouraging. It has to be taken into consideration that the results of cementless devices are strongly influenced by the implant design. Most of the recent evidence on cementless UKR is in relation to the Oxford prosthesis. Caution is therefore required in extending the results of this specific implant to other prosthetic designs.
Finally, navigation and robotics aim to improve the accuracy and reproducibility of the surgical procedure. So far, the results suggest that these techniques are successfully achieving this goal. However, there is no evidence of improved clinical outcome and/or survival from their use to justify the increased cost of the procedure. Further studies are needed to address this controversy.
9. Conclusions
Unicompartmental knee replacement is safe and effective for the treatment of anteromedial osteoarthritis of the knee.
Long-term studies suggest that compared to TKR, UKR has superior clinical and functional outcomes, significantly reduced morbidity and mortality, and is more cost effective. However, the revision rate is higher; this data is controversial and is likely to be influenced by the susceptibility of UKR to revision and the use of inappropriate indications.
A usage of 20% of caseload implies the implementation of “optimal indications” and surgical technique. This practice correlates with a lower revision rate and should be the aim of surgeons who want to undertake UKR. Surgeons with a low volume UKR practice (less than 13 per year) should consider the possibility of higher complication rates and may wish to consider other options, including referring these cases to a colleague with a higher volume UKR practice.
A better understanding of the optimal indications, patient selection and usage of UKR, as well as design, material and technical improvements have the potential to decrease the revision rate and improve the survival of UKR in national registries.
Conflict of interest
The authors have no conflict of interest to declare.
Contributor Information
Stefano Campi, Email: campi@gmail.com.
Saket Tibrewal, Email: mrtibrewal@gmail.com.
Rory Cuthbert, Email: rory.cuthbert@nhs.net.
Sheo B. Tibrewal, Email: sb.tibrewal@virgin.net.
References
- 1.MacIntosh D.L., Hunter G.A. The use of the hemiarthroplasty prosthesis for advanced osteoarthritis and rheumatoid arthritis of the knee. J Bone Joint Surg Br. 1972;54(2):244–255. [PubMed] [Google Scholar]
- 2.Marmor L. The modular knee. Clin Orthop Relat Res. 1973;94:242–248. doi: 10.1097/00003086-197307000-00029. [DOI] [PubMed] [Google Scholar]
- 3.Palmer S.H., Morrison P.J., Ross A.C. Early catastrophic tibial component wear after unicompartmental knee arthroplasty. Clin Orthop Relat Res. 1998;350:143–148. [PubMed] [Google Scholar]
- 4.Goodfellow J., OC J., Dodd C.A.F., Murray D.W. Oxford University Press; New York: 2006. Unicompartmental Arthroplasty with the Oxford Knee. [Google Scholar]
- 5.Goodfellow J.W., Tibrewal S.B., Sherman K.P., O'Connor J.J. Unicompartmental oxford meniscal knee arthroplasty. J Arthroplasty. 1987;2(1):1–9. doi: 10.1016/s0883-5403(87)80025-6. [DOI] [PubMed] [Google Scholar]
- 6.Mohammad H.R., Strickland L., Hamilton T.W., Murray D.W. Long-term outcomes of over 8,000 medial oxford phase 3 unicompartmental knees-a systematic review. Acta Orthop. 2017:1–7. doi: 10.1080/17453674.2017.1367577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parratte S., Ollivier M., Lunebourg A., Abdel M.P., Argenson J.N. Long-term results of compartmental arthroplasties of the knee: long term results of partial knee arthroplasty. Bone Joint J. 2015;97-B(10 (Suppl. A)):9–15. doi: 10.1302/0301-620X.97B10.36426. [DOI] [PubMed] [Google Scholar]
- 8.Pandit H., Jenkins C., Gill H.S., Barker K., Dodd C.A., Murray D.W. Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br. 2011;93(2):198–204. doi: 10.1302/0301-620X.93B2.25767. [DOI] [PubMed] [Google Scholar]
- 9.Labek G., Sekyra K., Pawelka W., Janda W., Stockl B. Outcome and reproducibility of data concerning the Oxford unicompartmental knee arthroplasty: a structured literature review including arthroplasty registry data. Acta Orthop. 2011;82(2):131–135. doi: 10.3109/17453674.2011.566134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Faour-Martin O., Valverde-Garcia J.A., Martin-Ferrero M.A. Oxford phase 3 unicondylar knee arthroplasty through a minimally invasive approach: long-term results. Int Orthop. 2013;37(5):833–838. doi: 10.1007/s00264-013-1830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoshida K., Tada M., Yoshida H., Takei S., Fukuoka S., Nakamura H. Oxford phase 3 unicompartmental knee arthroplasty in Japan–clinical results in greater than one thousand cases over ten years. J Arthroplasty. 2013;28(Suppl. 9):168–171. doi: 10.1016/j.arth.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Kim K.T., Lee S., Kim J.H., Hong S.W., Jung W.S., Shin The Survivorship and W.S. Clinical results of minimally invasive unicompartmental knee arthroplasty at 10-year follow-up. Clin Orthop Surg. 2015;7(2):199–206. doi: 10.4055/cios.2015.7.2.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edmondson M., Atrey A., East D. Survival analysis and functional outcome of the Oxford unicompartmental knee replacement up to 1 years follow up at a District General Hospital. J Orthop. 2015;12(Suppl. 1):S105–S110. doi: 10.1016/j.jor.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emerson R.H., Alnachoukati O., Barrington J., Ennin K. The results of Oxford unicompartmental knee arthroplasty in the United States: a mean ten-year survival analysis. Bone Joint J. 2016;98-B(10 (Suppl. B)):34–40. doi: 10.1302/0301-620X.98B10.BJJ-2016-0480.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schwab P.E., Lavand'homme P., Yombi J.C., Thienpont E. Lower blood loss after unicompartmental than total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3494–3500. doi: 10.1007/s00167-014-3188-x. [DOI] [PubMed] [Google Scholar]
- 16.Siman H., Kamath A.F., Carrillo N., Harmsen W.S., Pagnano M.W., Sierra R.J. Unicompartmental knee arthroplasty vs total knee arthroplasty for medial compartment arthritis in patients older than 75 years: comparable reoperation, revision, and complication rates. J Arthroplasty. 2017;32(6):1792–1797. doi: 10.1016/j.arth.2017.01.020. [DOI] [PubMed] [Google Scholar]
- 17.Wiik A.V., Aqil A., Tankard S., Amis A.A., Cobb J.P. Downhill walking gait pattern discriminates between types of knee arthroplasty: improved physiological knee functionality in UKA versus TKA. Knee Surg Sports Traumatol Arthrosc. 2015;23(6):1748–1755. doi: 10.1007/s00167-014-3240-x. [DOI] [PubMed] [Google Scholar]
- 18.Drager J., Hart A., Khalil J.A., Zukor D.J., Bergeron S.G., Antoniou J. Shorter hospital stay and lower 30-day readmission after unicondylar knee arthroplasty compared to total knee arthroplasty. J Arthroplasty. 2016;31(2):356–361. doi: 10.1016/j.arth.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Fabre-Aubrespy M., Ollivier M., Pesenti S., Parratte S., Argenson J.N. Unicompartmental knee arthroplasty in patients older than 75 results in better clinical outcomes and similar survivorship compared to total knee arthroplasty. A matched controlled study. J Arthroplasty. 2016;31(12):2668–2671. doi: 10.1016/j.arth.2016.06.034. [DOI] [PubMed] [Google Scholar]
- 20.Lum Z.C., Lombardi A.V., Hurst J.M., Morris M.J., Adams J.B., Berend K.R. Early outcomes of twin-peg mobile-bearing unicompartmental knee arthroplasty compared with primary total knee arthroplasty. Bone Joint J. 2016;98-B(10 (Suppl. B)):28–33. doi: 10.1302/0301-620X.98B10.BJJ-2016-0414.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zuiderbaan H.A., van der List J.P., Khamaisy S. Unicompartmental knee arthroplasty versus total knee arthroplasty: which type of artificial joint do patients forget? Knee Surg Sports Traumatol Arthrosc. 2017;25(3):681–686. doi: 10.1007/s00167-015-3868-1. [DOI] [PubMed] [Google Scholar]
- 22.Burn E., Sanchez-Santos M.T., Pandit H.G. Ten-year patient-reported outcomes following total and minimally invasive unicompartmental knee arthroplasty: a propensity score-matched cohort analysis. Knee Surg Sports Traumatol Arthrosc. 2016 doi: 10.1007/s00167-016-4404-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liddle A.D., Judge A., Pandit H., Murray D.W. Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet. 2014;384(9952):1437–1445. doi: 10.1016/S0140-6736(14)60419-0. [DOI] [PubMed] [Google Scholar]
- 24.2016. National Joint Registry for England, Wales and Northern Ireland. 13th Annual Report. [Google Scholar]
- 25.Chawla H., van der List J.P., Christ A.B., Sobrero M.R., Zuiderbaan H.A., Pearle A.D. Annual revision rates of partial versus total knee arthroplasty: a comparative meta-analysis. Knee. 2017;24(2):179–190. doi: 10.1016/j.knee.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 26.Goodfellow J.W., O'Connor J.J., Murray D.W. A critique of revision rate as an outcome measure: re-interpretation of knee joint registry data. J Bone Joint Surg Br. 2010;92(12):1628–1631. doi: 10.1302/0301-620X.92B12.25193. [DOI] [PubMed] [Google Scholar]
- 27.Kozinn S.C., Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989;71(1):145–150. [PubMed] [Google Scholar]
- 28.White S.H., Ludkowski P.F., Goodfellow J.W. Anteromedial osteoarthritis of the knee. J Bone Joint Surg Br. 1991;73(4):582–586. doi: 10.1302/0301-620X.73B4.2071640. [DOI] [PubMed] [Google Scholar]
- 29.Pandit H., Jenkins C., Gill H.S. Unnecessary contraindications for mobile-bearing unicompartmental knee replacement. J Bone Joint Surg Br. 2011;93(5):622–628. doi: 10.1302/0301-620X.93B5.26214. [DOI] [PubMed] [Google Scholar]
- 30.Berend K.R., Lombardi A.V., Jr., Adams J.B. Obesity, young age, patellofemoral disease, and anterior knee pain: identifying the unicondylar arthroplasty patient in the United States. Orthopedics. 2007;30(Suppl. 5):19–23. [PubMed] [Google Scholar]
- 31.Cavaignac E., Lafontan V., Reina N. Obesity has no adverse effect on the outcome of unicompartmental knee replacement at a minimum follow-up of seven years. Bone Joint J. 2013;95-B(8):1064–1068. doi: 10.1302/0301-620X.95B8.31370. [DOI] [PubMed] [Google Scholar]
- 32.Zengerink I., Duivenvoorden T., Niesten D., Verburg H., Bloem R., Mathijssen N. Obesity does not influence the outcome after unicompartmental knee arthroplasty. Acta Orthop Belg. 2015;81(4):776–783. [PubMed] [Google Scholar]
- 33.Woo Y.L., Chen Y.Q., Lai M.C. Does obesity influence early outcome of fixed-bearing unicompartmental knee arthroplasty? J Orthop Surg (Hong Kong) 2017;25(1) doi: 10.1177/2309499016684297. [DOI] [PubMed] [Google Scholar]
- 34.Hamilton T.W., Choudhary R., Jenkins C. Lateral osteophytes do not represent a contraindication to medial unicompartmental knee arthroplasty: a 15-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):652–659. doi: 10.1007/s00167-016-4313-9. [DOI] [PubMed] [Google Scholar]
- 35.Waldstein W., Kasparek M.F., Faschingbauer M., Windhager R., Lateral-compartment Boettner F. Osteophytes are not associated with lateral-compartment cartilage degeneration in arthritic varus knees. Clin Orthop Relat Res. 2017;475(5):1386–1392. doi: 10.1007/s11999-016-5155-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Faschingbauer M., Renner L., Waldstein W., Boettner F. Are lateral compartment osteophytes a predictor for lateral cartilage damage in varus osteoarthritic knees? Data from the Osteoarthritis Initiative. Bone Joint J. 2015;97-B(12):1634–1639. doi: 10.1302/0301-620X.97B12.36465. [DOI] [PubMed] [Google Scholar]
- 37.Laskin R.S. Unicompartmental knee replacement: some unanswered questions. Clin Orthop Relat Res. 2001;392:267–271. [PubMed] [Google Scholar]
- 38.Stern S.H., Becker M.W., Insall J.N. Unicondylar knee arthroplasty. An evaluation of selection criteria. Clin Orthop Relat Res. 1993;286:143–148. [PubMed] [Google Scholar]
- 39.Berger R.A., Meneghini R.M., Sheinkop M.B. The progression of patellofemoral arthrosis after medial unicompartmental replacement: results at 11 to 15 years. Clin Orthop Relat Res. 2004;428:92–99. doi: 10.1097/01.blo.0000147700.89433.a5. [DOI] [PubMed] [Google Scholar]
- 40.Hamilton T.W., Pandit H.G., Jenkins C., Mellon S.J., Dodd C.A.F., Murray D.W. Evidence-Based indications for mobile-bearing unicompartmental knee arthroplasty in a consecutive cohort of thousand knees. J Arthroplasty. 2017;32(6):1779–1785. doi: 10.1016/j.arth.2016.12.036. [DOI] [PubMed] [Google Scholar]
- 41.Lau R.L., Perruccio A.V., Gandhi R., Mahomed N.N. The role of surgeon volume on patient outcome in total knee arthroplasty: a systematic review of the literature. BMC Musculoskelet Disord. 2012;13:250. doi: 10.1186/1471-2474-13-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liddle A.D., Pandit H., Judge A., Murray D.W. Effect of surgical caseload on revision rate following total and unicompartmental knee replacement. J Bone Joint Surg Am. 2016;98(1):1–8. doi: 10.2106/JBJS.N.00487. [DOI] [PubMed] [Google Scholar]
- 43.Liddle A.D., Pandit H., Judge A., Murray D.W. Optimal usage of unicompartmental knee arthroplasty: a study of 41,986 cases from the National Joint Registry for England and Wales. Bone Joint J. 2015;97-B(11):1506–1511. doi: 10.1302/0301-620X.97B11.35551. [DOI] [PubMed] [Google Scholar]
- 44.Hamilton T.W., Rizkalla J.M., Kontochristos L. The interaction of caseload and usage in determining outcomes of unicompartmental knee arthroplasty: a meta-analysis. J Arthroplasty. 2017 doi: 10.1016/j.arth.2017.04.063. [DOI] [PubMed] [Google Scholar]
- 45.Li M.G., Yao F., Joss B., Ioppolo J., Nivbrant B., Wood D. Mobile vs. fixed bearing unicondylar knee arthroplasty: a randomized study on short term clinical outcomes and knee kinematics. Knee. 2006;13(5):365–370. doi: 10.1016/j.knee.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 46.Cheng T., Chen D., Zhu C. Fixed- versus mobile-bearing unicondylar knee arthroplasty: are failure modes different? Knee Surg Sports Traumatol Arthrosc. 2013;21(11):2433–2441. doi: 10.1007/s00167-012-2208-y. [DOI] [PubMed] [Google Scholar]
- 47.Kwon O.R., Kang K.T., Son J. Biomechanical comparison of fixed- and mobile-bearing for unicomparmental knee arthroplasty using finite element analysis. J Orthop Res. 2014;32(2):338–345. doi: 10.1002/jor.22499. [DOI] [PubMed] [Google Scholar]
- 48.Ko Y.B., Gujarathi M.R., Oh K.J. Outcome of unicompartmental knee arthroplasty: a systematic review of comparative studies between fixed and mobile bearings focusing on complications. Knee Surg Relat Res. 2015;27(3):141–148. doi: 10.5792/ksrr.2015.27.3.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim S.J., Postigo R., Koo S., Kim J.H. Causes of revision following Oxford phase 3 unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1895–1901. doi: 10.1007/s00167-013-2644-3. [DOI] [PubMed] [Google Scholar]
- 50.Peersman G., Stuyts B., Vandenlangenbergh T., Cartier P., Fennema P. Fixed- versus mobile-bearing UKA: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3296–3305. doi: 10.1007/s00167-014-3131-1. [DOI] [PubMed] [Google Scholar]
- 51.Campi S., Pandit H.G., Dodd C.A.F., Murray D.W. Cementless fixation in medial unicompartmental knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):736–745. doi: 10.1007/s00167-016-4244-5. [DOI] [PubMed] [Google Scholar]
- 52.Association NZO . 2016. NZJR 17 Year Report. [Google Scholar]
- 53.Song E.K., N M., Lee S.H., Na B.R., Seon J.K. Comparison of outcome and survival after unicompartmental knee arthroplasty between navigation and conventional techniques with an average 9-year follow-up. J Arthroplasty. 2016;31(2):395–400. doi: 10.1016/j.arth.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 54.Citak M., Suero E.M., Citak M. Unicompartmental knee arthroplasty: is robotic technology more accurate than conventional technique? Knee. 2013;20(4):268–271. doi: 10.1016/j.knee.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 55.Pearle A.D., O'Loughlin P.F., Kendoff D.O. Robot-assisted unicompartmental knee arthroplasty. J Arthroplasty. 2010;25(2):230–237. doi: 10.1016/j.arth.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 56.Plate J.F., Mofidi A., Mannava S. Achieving accurate ligament balancing using robotic-assisted unicompartmental knee arthroplasty. Adv Orthop. 2013;2013:837167. doi: 10.1155/2013/837167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ghomrawi H.M., Eggman A.A., Pearle A.D. Effect of age on cost-effectiveness of unicompartmental knee arthroplasty compared with total knee arthroplasty in the U.S. J Bone Joint Surg Am. 2015;97(5):396–402. doi: 10.2106/JBJS.N.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Soohoo N.F., Sharifi H., Kominski G., Lieberman J.R. Cost-effectiveness analysis of unicompartmental knee arthroplasty as an alternative to total knee arthroplasty for unicompartmental osteoarthritis. J Bone Joint Surg Am. 2006;88(9):1975–1982. doi: 10.2106/JBJS.E.00597. [DOI] [PubMed] [Google Scholar]
- 59.Smith W.B., 2nd, Steinberg J., Scholtes S., McNamara I.R. Medial compartment knee osteoarthritis: age-stratified cost-effectiveness of total knee arthroplasty, unicompartmental knee arthroplasty, and high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):924–933. doi: 10.1007/s00167-015-3821-3. [DOI] [PubMed] [Google Scholar]
- 60.Shankar S., Tetreault M.W., Jegier B.J., Andersson G.B., Della Valle C.J. A cost comparison of unicompartmental and total knee arthroplasty. Knee. 2016;23(6):1016–1019. doi: 10.1016/j.knee.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 61.Hamilton T.W., Pandit H.G., Inabathula A. Unsatisfactory outcomes following unicompartmental knee arthroplasty in patients with partial thickness cartilage loss: a medium-term follow-up. Bone Joint J. 2017;99-B(4):475–482. doi: 10.1302/0301-620X.99B4.BJJ-2016-1061.R1. [DOI] [PubMed] [Google Scholar]
- 62.Berend K.R., Lombardi A.V., Jr., Jacobs C.A. The combination of preoperative bone marrow lesions and partial-thickness cartilage loss did not result in inferior outcomes after medial unicompartmental knee arthroplasty. J Arthroplasty. 2017;32(10):3000–3003. doi: 10.1016/j.arth.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 63.Jacobs C.A., Berend K.R., Lombardi A.V., Jr., Christensen C.P. The location and severity of preoperative subchondral bone marrow lesions were not associated with inferior postoperative outcomes after medial unicompartmental knee arthroplasty or total knee arthroplasty. J Arthroplasty. 2016;31(11):2476–2480. doi: 10.1016/j.arth.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 64.Altinel L., Er M.S., Kacar E., Erten R.A. Diagnostic efficacy of standard knee magnetic resonance imaging and radiography in evaluating integrity of anterior cruciate ligament before unicompartmental knee arthroplasty. Acta Orthop Traumatol Turc. 2015;49(3):274–279. doi: 10.3944/AOTT.2015.14.0013. [DOI] [PubMed] [Google Scholar]
- 65.Sharpe I., Tyrrell P.N., White S.H. Magnetic resonance imaging assessment for unicompartmental knee replacement: a limited role. Knee. 2001;8(3):213–218. doi: 10.1016/s0968-0160(01)00086-2. [DOI] [PubMed] [Google Scholar]
- 66.Baker P., Jameson S., Critchley R., Reed M., Gregg P., Deehan D. Center and surgeon volume influence the revision rate following unicondylar knee replacement: an analysis of 23,400 medial cemented unicondylar knee replacements. J Bone Joint Surg Am. 2013;95(8):702–709. doi: 10.2106/JBJS.L.00520. [DOI] [PubMed] [Google Scholar]