Abstract
Accumulating evidence indicates that cell division cycle 7-related protein kinase(CDC7) plays an essential role in tumor cells and it could induces cell proliferation and could be related to prognosis in multiple types of cancer. However, the biological role and molecular mechanism of CDC7 in GBM still remains unclear. In this study, we identified that CDC7 expression was enriched in glioblastoma (GBM) tumors and was functionally required for tumor proliferation and its expression was associated to poor prognosis in GBM patients. Mechanically, CDC7 induced radio resistance in GBM cells and CDC7 knock down increased cell apoptosis when combined with radiotherapy. Moreover, CDC7 regulated The DNA repair/recombination protein 54L (RAD54L) expression via regulation of RAD54L promoter activity. Therapeutically, we found that CDC7 inhibitor attenuated tumor growth both in vitro and in vivo. Collectively, CDC7 promotes proliferation, induces radio resistance in GBM, and could become a potential therapeutic target for GBM.
Introduction
Glioblastoma (GBM) is one of the most common primary malignant intracranial tumors in human adults [1], [2]. The current standard methods of GBM therapy for including maximum surgical resection followed concurrent radiation and chemotherapy [3]. However, the median survival from diagnosis in GBM patients is only 15 months and the prognosis for these patients haven’t been significantly improved in the past 30 years [4], [5]. Recent studies indicated that genetic heterogeneity and invasive proclivity is essential in the therapeutic failure and therapy resistance of GBM [6], [7]. To this end, clarifying the molecular mechanism and potential pathways will be critical to improve clinical treatment of GBM.
DNA damage response and repair counteract the threats to genomic integrity, and variations in DNA repair capacity resulting from genetic polymorphisms could therefore correlate with cancer predisposition [8]. Genomic instability due to DNA damage by carcinogens has been implicated in the development of cancer and the resistance of radio therapy [8], [9], [10]. Recent evidence showed that repair of damage to DNA requires complex biological mechanisms that are tightly regulated and integrated [11]. The DNA repair/recombination protein 54 (RAD54) family of DNA translocase proteins function in concert with RAD51 to promote recombinational DNA repair has been proved in multiple types of cancers [12]. RAD54 translocation has also been proposed to act following homology recognition as a ‘heteroduplex pump’ to incorporate the invading ssDNA into the D-loop which is associated with local chromatin remodeling in vivo while simultaneously removing RAD51 during the generation of the heteroduplex product [13], [14], [15]. Thus, RAD54 protein plays an essential role in DNA damage repair and therapy resistance in tumor, however, the detailed mechanism of transcriptional and functional regulation of RAD54 still remains unclear.
Cell division cycle 7-related protein kinase(CDC7) has been identified as an enzyme that is essential for DNA replication and the overexpression of CDC7 and its downstream targets has been reported in multiple types of human cancers including ovarian cancer, melanoma, colorectal cancer, pancreatic cancer and glioblastoma [16], [17], [18], [19]. Bonte [16] et al reported that CDC7-Dbf4 kinase overexpression could be correlated with p53 inactivation then promotes tumor growth through regulation of cell cycles. CDC7 and DBF4 overexpression are proved to induce cell cycle arrest in S phase and it has been hypothesized that increased CDC7 activity may aid recovery or repair of stalled replication forks to enhance survival of tumor cells [20]. Therefore, alterations in CDC7/DBF4 protein activity during tumorigenesis may have important consequences for tumor cell survival, underlining the potential of CDC7 as an anticancer target [17], [21]. Erbayraktar et al. [19] reported that CDC7 inhibition reduces glioblastoma cell viability, suppresses cell proliferation, and triggers apoptosis in glioblastoma cell lines. However, the downstream target and the functional role of CDC7 in GBM still need further investigation.
In this study, we identified CDC7 as the most up-regulated kinase encoding genes in GBM and functionally required for tumor growth, tumorigenesis and infiltration of GBM. Moreover, CDC7-dependt transcriptional regulation of RAD54L is critical in DNA damage repair after radio therapy thus promotes radio resistance and tumor recurrence. Furthermore, we found that inhibition of CDC7 via shRNA or inhibitor could suppress tumor growth and enhance radio sensitivity of GBM cells both in vitro and in vivo. Altogether, CDC7 is a key regulator of tumor growth and radio resistance and could be a potential therapeutic target for GBM.
Materials and Methods
Ethics
All the usage of experimental animals and cell lines (nude mice) in this study are approved by the Scientific Ethics Committee of Xi’an Jiaotong University, Xi’an, China.
Reagents and Antibodies
Following reagents and primary antibodies are used in this study: DMEM-F12 (Gibco, 10565-018), Fetal bovine serum (Gibco, 10082-147), Accutase solution (Sigma, A6964-100), Alamar Blue (Invitrogen, DAL1100), RIPA buffer (Sigma, R0278), Phosphatase inhibitor cocktail (Sigma, P0044), Protease inhibitor cocktail (P8340), Bradford (BIORAD, 500-0006), BSA used in Bradford assay (BioLabs, B9001S), PageRuler plus prestained protein (Thermo scientific, 26619), iScript Reverse Transcription supermix for qRT-PCR (Bio-rad, 170-8841), shCDC7 lentivirus particles (pGFP-C-shLenti, Origene, TL320578V), PHA-767491 (AdooQ, A11164-100), Alexa Fluor® 488 Annexin V/Dead Cell Apoptosis Kit (Thermo Fisher Scientific,V13241). anti-CDC7 (Novus Biologicals, DCS-341, Mouse, used for WB and IHC), anti-CDC7 (Abcam, ab108332, Rabbit, used for FACs), anti-RAD54L (Novus Biologicals, NBP2-33916, Rabbit, used for WB), anti-RAD54L (Novus Biologicals, NB100-148, Mouse, used for WB), anti- Cleaved Caspase 3 (Cell Signaling Technology, #9664, Rabbit, used for WB), β-Actin (Sigma, A5316, Mouse, used for WB).
In Vitro Cell Cultures
Glioblastoma cell lines SHG44, T98G, U87, U373, U251, U138, normal human astrocytes NHA and HEK-293T cells are provided by Xi’an Jiaotong University. Cell lines are cultured in DMEM/F12 medium containing 10% FBS supplement (vol%). The culture medium is replaced every 5-10 days.
Lentivirus Infection
Cells were infected with the shRNA lentivirus or overexpression lentivirus at 24 h after seeding in a 6-well plate according to the manufacturer’s protocol. The efficacy of lentivirus infection was evaluated by qRT-PCR and western blot.
In Vitro Cell Proliferation Assay
GBM cells were transduced with shRNA lentivirus for 3 days, and the cells were dissociated into single cell suspension with Accutase. After the live cell number was measured by trypan blue method with Countesss Automated Cell Counter (Thermo Fisher Scientific, Waltham, MA, USA), 200μl cell suspension containing 2,000 cells was added into 96 well plates. The cell number was evaluated by alamarBlue according to manufacturer’s protocol every 2 days after seeding.
Luciferase Assays of RAD54L Promoter-Luciferase Constructs
pGL3-promoter-RAD54L plasmid was purchased from AxyBio (CDS-H10735-9). U87 cells were transfected via Lipofectamine™ 2000 with 1 μg of empty vector, or RAD54L promoter luciferase reporter and cultured for 10 days. Luciferase assays were performed using Bright-Glo reagent (Promega) on the Victor3 counter (Perkin Elmer, Waltham, MA).
RNA Isolation and Quantitative Real-Time PCR
RNA is isolated by using RNeasy mini kit (QIAGEN) according to the manufacturer’s instructions. RNA concentration is determined using a Nanodrop 2000 (Thermo scientific). cDNA is synthesized by using iScript reverse transcription supermix for qRT-PCR (Bio-rad) according to the manufacturer’s protocol. The reverse-transcribed cDNA is analyzed by quantitative RT-PCR (qRT-PCR), and 18S is used as an internal control. Each qRT-PCR includes a 10 μL reaction mixture per well that includes 2.5 μL cDNA, 0.5 μL forward primer (0.5 μM), 0.5 μL reverse primer (0.5 μM), 1.5 μL of DNase/RNase-free distilled water, and 5 μL SYBR green reagent (QIAGEN). The following cycles are performed during DNA amplification: 94°C for 2 min, 40 cycles of 94°C (30 s), 60°C (30 s), and 72°C (40 s). 18S is used as an internal control. The primer sequences are showed below: CDC7-Forward: GCTTCATAAAGCTTCTCAATATCTTTT, CDC71-Reverse: TTTTTCTCCCCAGCGTGAC, RAD54L-Forward: GAGCCCAGAGGACCTTGATA, RAD54L -Reverse: AACCACCTTGTCTGGACAGC, 18S-Forward: GGCCCTGTAATTGGAATGAGTC and 18S-Reverse: CCAAGATCCAACTACGAGCTT.
Western Blotting
The cell lysates are prepared in RIPA buffer containing 1% protease and 1% phosphatase inhibitor cocktail (Sigma Aldrich) on ice. The sample protein concentrations are determined by the Bradford method. Equal amounts of protein lysates (10 μg/lane) are fractionated on NuPAGE Novex 4–12% Bis-Tris Protein gel (Invitrogen) and transferred to a PVDF membrane (Invitrogen). Subsequently, the membranes are blocked with 5% skimmed milk for 1 h and then treated with the relevant antibody at 4°C overnight. Protein expression is visualized with Amersham ECL Western Blot System (GE Healthcare Life Sciences). β-Actin serves as a loading control.
Flow Cytometry Analysis
Harvest the cells after the incubation period and washing cold phosphate-buffered saline for 3 times (PBS). Re-centrifuge the washed cells (from step 2), discard the supernatant and suspend 5 × 105 cells in 100 μL 1X Annexin-binding buffer. Add 5 μL Alexa Fluor® 488 annexin V and 1 μL 100 μg/mL PI working solution which were prepared according to the protocol. Incubate the cells at room temperature for 15 minutes then add 400 μL 1× annexin -binding buffer, mix gently and keep the samples on ice. Analyze the stained cells by measuring the fluorescence emission at 530 nm and 575 nm with 488 nm excitation.
In Vivo Intracranial Xenograft Tumor Models
6-week-old nude mice are used for GBM intracranial implantation. All animal experiments are carried out in Xi’an Jiaotong University. The GBM suspension (1×105 cells in 5 μl of PBS) transduced with non-target or shCDC7 lentivirus is injected into the brains of nude mice after anesthesia. At least six mice are used for each group. Drug treatment is done through tail vein injection and starts from 5 days after tumor cells are implanted. Mice were monitored once a day for symptoms related to tumor growth including an arched back, unsteady gait, paralysis of legs and body weight loss. Mice were euthanized by over-dose anesthesia of ketamine and xylazine after a total body weight loss of 40% or severe symptoms were observed.
Statistical Analysis
All the data are presented as Mean ± SD. The number of replicates for each experiment is stated in the figure legend. Statistical differences between two groups are evaluated by two-tailed t test. The comparison among multiple groups are performed by one-way analysis of variance (ANOVA) followed by Dunnett’s posttest. The statistical significance of Kaplan-Meier survival plot is determined by log-rank analysis. Statistical analysis is performed by Prism 6 (Graphpad prism), unless mentioned otherwise in figure legend. P < .05 is considered as statistically significant.
Results
CDC7 Expression was Highly Enriched in GBM Cells
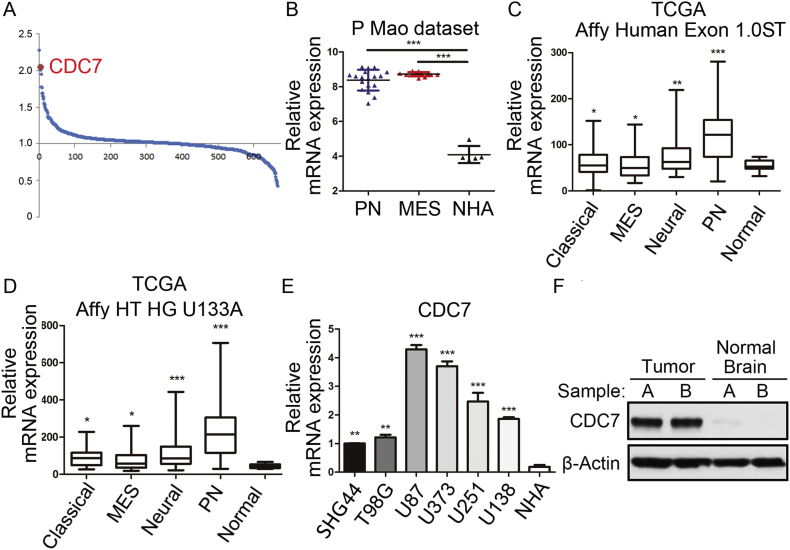
In this study, we first sought to characterize the role of CDC7 in GBM tumors. To this end, we analyzed the data from microarray database published in 2013 [22] and find that CDC7 was one of the most up-regulated kinase-encoding genes in GBM samples compared to normal human astrocyte cells (Figure 1, A and B). Additionally, we found that CDC7 expression was significantly enriched in all the 4 subtypes of GBM according to TCGA database (classical, mesenchymal, neural and proneural) compared with non-tumor tissue (Figure 1, C and D). To confirm this, qRT-PCR data by using 6 GBM cell lines and normal human astrocyte (NHA) was performed and the result exhibited the higher expression of CDC7 mRNA in GBM (Figure 1E). Similar to the mRNA expression, we used 2 paired samples of GBM tumor and normal brain from the same patients (labeled as patient A and B) and Western blotting data demonstrated the same result (Figure 1F). Taken together, these data indicated that BUB1B was preferentially expressed in GBM.
Figure 1.
CDC7 expression was highly enriched in GBM cells
(A) Genome-wide transcriptome microarray analysis from Mao’s dataset shows that CDC7 is one of the most up-regulated kinase encoding genes in GBM samples compared to normal tissue. (B) Analysis of Mao’s dataset indicated that CDC7 was highly expressed in both mesenchymal and proneural subtypes of GBM compared with normal astrocytes. (C-D) Analysis of TCGA database indicated that CDC7 was highly expressed in all the 4 subgroups of GBM (classical, mesenchymal, neural and proneural) compared with non-tumor tissue. (E) qRT-PCR analysis showed BUB1B mRNA expression was elevated in 6 GBM cell lines (SHG44, T98G, U87, U373, U251 and U138) compared with normal astrocytes (NHA). (F) Western blotting analysis indicated that CDC7 protein expression was enriched in GBM tissue compared with normal brain from the paired patient samples. β-actin served as a control.
CDC7 was Functionally Required for GBM Proliferation Both InVitro and In Vivo
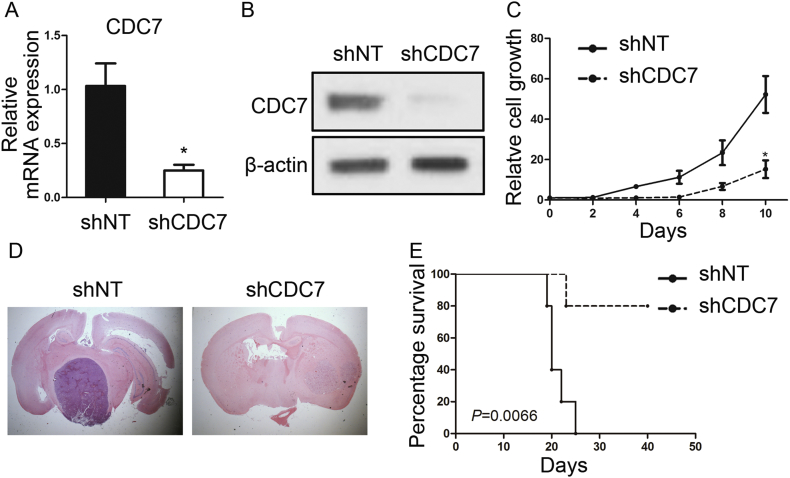
To examine the biological role of CDC7 in GBM, we picked one in vitro GBM cell line (U87) which had the highest CDC7 expression and transduced with either lentiviral shRNA clone for CDC7 (shCDC7) or a non-targeting shRNA (shNT, negative control). The efficiency for lentivirus infection was confirmed by qRT- PCR analysis. The result indicated CDC7 mRNA expression was significantly reduced in shCDC7 U87 cells (Figure 2A). Furthermore, Western blotting analysis exhibited that CDC7 protein expression was markedly decreased by shCDC7 (Figure 2B). In vitro cell growth kinetics of shCDC7 transfected U87 cells was diminished proportionally to the reduction levels of CDC7 (Figure 2C). Next, we investigated the effect of CDC7 knock-down on in vivo tumor formation. To this end, we used U87 cells-derived mouse intracranial tumor models. The results showed that mice xenografted with shNT transfected U87 rapidly formed lethal hyper vascular GBM-like tumors within 40 days while a longer survival could be observed in mice xenografted shCDC7 group (Figure 2, D and E). These findings indicated that CDC7 was required for GBM proliferation both in vitro and in vivo.
Figure 2.
CDC7 was functionally required for GBM proliferation both in vitro and in vivo
A. qRT-PCR analysis of U87 cells transduced with shRNA against CDC7 (shCDC7) or non- targeting control (shNT) (P < .05, n = 3, with t test). B. Western blotting analysis of U87 cells transduced with shRNA against CDC7 (shCDC7) or non-targeting control (shNT). β-actin served as a control. C. In vitro cell growth assay showed shRNA against CDC7 (shCDC7) inhibited cell proliferation of U87 cells (P < .05, n = 6, with t test). D. Representative images of H&E stained mouse brain section after the intracranial transplantation of U87 cells transduced with shRNA against CDC7 (shCDC7) or non-targeting control (shNT). E. Kaplan-Meier analysis of nude mice harboring intracranial tumor derived from U87 cells transduced with shNT (n = 5), shCDC7 (n = 5) (P = .0066, with log-rank test).
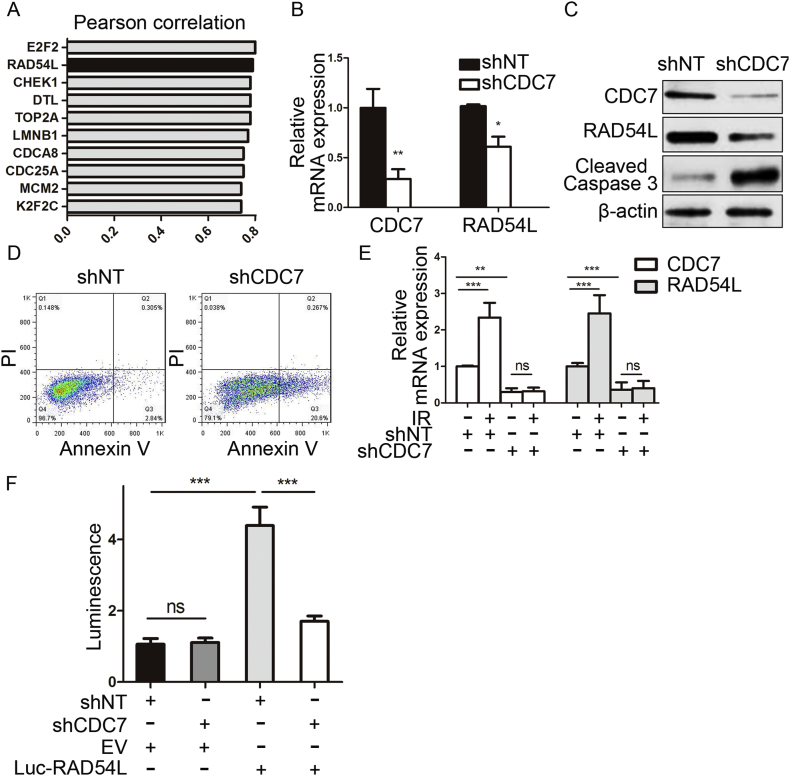
CDC7-Binding Region is Critical for the Activation of the RAD54L Promoter
To further assess the downstream target of CDC7 in GBM, we analyzed the data from TCGA dataset and the result indicated that RAD54L was one of the top genes which could be correlated to CDC7 mRNA (Figure 3A). Furthermore, shRNA-mediated-knockdown of CDC7 resulted in a marked decrease in RAD54L expression at mRNA level (Figure 3B). Additionally, artificial knockdown of CDC7 induced decrease of RAD54L and RAD51 at protein level (Figure 3C). We also found that depressed CDC7 resulted in an up-regulation of cleaved caspase 3 which is a marker for apoptosis in cells (Figure 3C). To address this, we performed flow cytometry for apoptosis with Annexin V (AV) antibody and Propidium Iodide (PI) by using U87 transduced with shCDC7 or shNT. The results indicated that proportions of cells undergoing early (AV+; PI−) and late (AV+; PI+) apoptosis were both dramatically increased after CDC7 knockdown in comparison to shNT cells (Figure 3D). Moreover, we found that RAD54L expression was elevated after U87 cells were exposed to radio therapy while this effects could be demolished by CDC7 knockdown (Figure 3E). We then performed a luciferase reporter assay with constructs driven by a human RAD54L promoter. As expected, shRNA-mediated-knockdown of CDC7 resulted in a marked decrease in transcription activity of RAD54L promoter region in U87 cells (Figure 3F). These data suggest that the CDC7-binding region was critical for RAD54L promoter activation in GBM cells.
Figure 3.
CDC7-binding region is critical for the activation of the RAD54L promoter. (A) Top 10 genes correlated to CDC7 mRNA expression in TCGA dataset. Pearson correlation analysis was performed. (B) qRT-PCR analysis for CDC7 and RAD54L mRNA expression in U87 cells transduced with shRNA against CDC7 (shCDC7) or non-targeting control (shNT). (P < .05, n = 3 with t test). (C) Western blotting analysis of U87 cells transduced with shRNA against CDC7 (shCDC7) or non-targeting control (shNT). β-actin served as a control. (D) Flow cytometry analysis for apoptosis with Annexin V antibody and Propidium Iodide using U87 cells transduced with shNT or shCDC7. E. RT-PCR analysis for CDC7 and BUB1B mRNA expression in U87 cells transduced with shNT or shCDC7 with or without radiation treatment (12 Gy) (P < .01, with t tests). F. Luciferase activity assay showed shRNA-mediated-knockdown of CDC7 resulted in a marked decrease in transcription activity of RAD54L promoter in U87 cells(P < .01, with t tests).
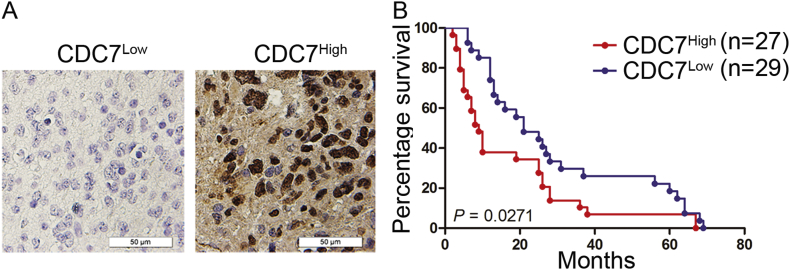
CDC7 Expression was Associated with Poor Prognosis in GBM Patients
To clarify the function of CDC7 in GBM, we collected 56 GBM samples from patients underwent surgery in our institution from 2009 to 2016 and performed immunohistone staining to evaluate the expression of CDC7. The results indicated that high CDC7 expression could be related to poor prognosis in GBM patients when compared to low CDC7 expression patients (Figure 4, A and B).
Figure 4.
CDC7 expression was associated with poor prognosis in GBM patients. (A) Representative images of IHC stained patient samples. (B) Analysis of patient samples indicated the inverted correlation between CDC7expression and post-surgical survival of GBM patients.
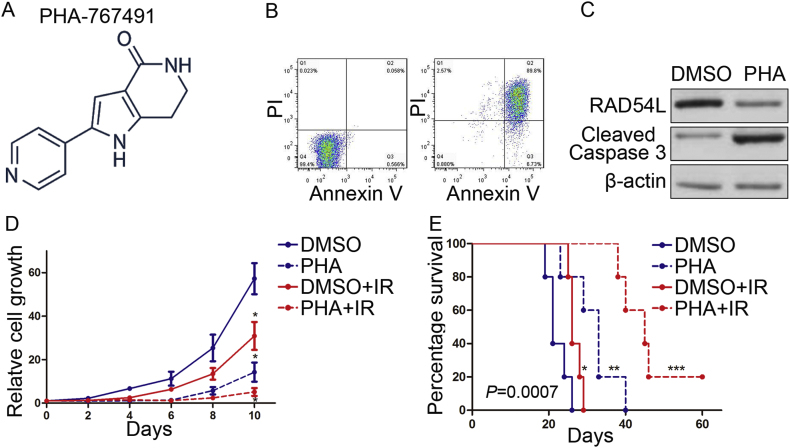
CDC7 Inhibitor Inhibited Tumor Growth and Radio Resistance of GBM Cells
Based on the inhibitory effects of CDC7 silencing on the GBM cells proliferation and tumorigenicity, we sought to find a potential target for clinical treatment for GBM. To this end, a CDC7 inhibitor PHA-767491 was used to clarify the effects of CDC7 inhibition on GBM (Figure 5A). Flow cytometry analysis showed that PHA-767491 treatment increased cell apoptosis in U87 cells (Figure 5B). Moreover, Western blotting data indicated that inhibition of CDC7 by PHA-767491 induced reduction of RAD54L and the expression of cleaved caspase 3 was elevated at the same time (Figure 5C). Furthermore, in vitro cell proliferation was significantly eliminated by PHA-767491 when combined with radiation compared with radio therapy alone (Figure 5D). More importantly, systemic treatment of U87-derived mouse brain tumors with PHA-767491 significantly attenuated the tumor growth and radio sensitivity, thereby extending the survival of tumor bearing mice compared to the vehicle treated counterparts (Figure 5E). Altogether, CDC7 inhibitor inhibited tumor growth and radio resistance of GBM cells both in vitro and in vivo.
Figure 5.
The CDC7 inhibitor reduced tumorigenicity and radio resistance of GBM. (A) Chemical structure of CDC7 inhibitor PHA-767491. (B) Flow cytometry analysis for apoptosis with Annexin V antibody and Propidium Iodide using U87 cells treated with PHA-767491 or DMSO. (C) Western blotting analysis of U87 cells t treated with PHA-767491 or DMSO. β-actin served as a control. (D) In vitro cell growth assay showed that PHA-767491 decreased cell proliferation of U87 when combined with radiation (P < .05, with t tests). E. Kaplan-Meier analysis was performed for the comparison of survival in U87 implanted mice treat with or without PHA-767491 (P = .0007, with log-rank test).
Discussion
Radio therapy is effective for tumor cells mainly through targeting DNA double-strand and induces DNA damage, the DNA repair pathways of tumor cells can influence the efficacy of radio therapy and plays an important functional role in therapy resistance and recurrence in tumor [23]. Recently evidence showed that varies of DNA repair pathways can be differentially activated after radiation [24], [25], [26]. In this study, we identified CDC7-RAD54L pathway as an activated molecular mechanism after radio therapy and was functionally required for tumorigenesis and radio resistance in GBM. Mechanically, we found that CDC7 regulates RAD54L expression via regulation of RAD54L promoter activity. Therapeutically, we confirmed that inhibition of CDC7 via either shRNAs or small molecule inhibitor could reduce tumor growth and enhance radio sensitivity in GBM. Altogether, CDC7 is a transcriptional regulator for RAD54L which is essential for tumor growth and radio resistance.
CDC7 is a serine/threonine kinase that phosphorylates mini chromosome maintenance protein 2 (MCM2) of the eukaryotic pre-replication complex [27] and has been proved to be required for initiation of DNA replication [28]. CDC7 expression is significantly enriched in a wide range of different types of cancers and targeting CDC7 kinase was suggested as a new approach for cancer therapy [29]. Previous studies showed that CDC7 promotes tumor growth and tumorigenesis mainly through its effect on regulating cell cycle and DNA replication [18]. Tudzarova [30] et al discovered a new p53-dependent stress pathway that regulates CDC7 which functions through post-transcriptional and post-translational regulatory mechanisms. Besides these findings, for the first time, we identified CDC7 as a key regulator for tumor growth and recurrence in GBM. Interestingly, we found that CDC7 induces radio resistance in GBM but this mechanism may not base on its effects on cell cycle regulation but depends on DNA damage repair mechanism. To investigate this, we successfully identified RAD54L as a potential downstream target for CDC7 through bioinformatics analysis for TCGA dataset. Furthermore, we found CDC7 could activate RAD54L promoter then regulates RAD54L expression at transcription level. Thus, CDC7-RAD54L pathway promotes DNA damage repair then induces radio resistance in GBM cells. However, despite these new findings, the binding site for CDC7 on RAD54L promoter region still remains unclear. Therefore, further studies including CHIP-sequencing and CHIP-sequencing needs to be performed to clarify either CDC7 binds to RAD54L promoter directly or not.
PHA-767491 hydrochloride is a first-generation CDC7 inhibitor with well-characterized anti-tumor activity [19]. Montagnoli [31] et al showed that PHA-767491 hydrochloride inhibits cell proliferation and induces apoptosis in multiple cell lines in a comprehensive panel of cancer cell lines. Recent studies showed that PHA-767491 effectively reduces cell viability in GBM cell lines [19]. In this study, we confirmed that PHA-767491 could inhibit cell proliferation and induce apoptosis in GBM, which is similar to the previous studies. Moreover, we found PHA-767491 is efficient for reducing tumorigenesis and is able to enhance radio sensitivities via suppressed RAD54L expression both in vitro and in vivo. These findings implied that PHA-767491 might be a potential therapeutic candidate for GBM treatment. Further studies for pharmacokinetics will be performed to evaluate the efficiency and safety for this inhibitor before it’s suitable for clinical trials.
Acknowledgements
This research was supported by the grants "High Technology Research and Development Program of Shaanxi Province (No. 2014K11–01–01–03)". We thank all the members in the Department of Neurosurgery, Xi’an Jiaotong University.
References
- 1.Ostrom QT, Gittleman H, Liao P. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007-2011. Neuro Oncol. 2014;16(Suppl. 4):iv1-63. doi: 10.1093/neuonc/nou223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ostrom QT, Gittleman H, Fulop J. CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2008-2012. Neuro Oncol. 2015;17(Suppl. 4):iv1–iv62. doi: 10.1093/neuonc/nov189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson DR, Galanis E. Medical management of high-grade astrocytoma: current and emerging therapies. Semin Oncol. 2014;41(4):511–522. doi: 10.1053/j.seminoncol.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Linz U. Commentary on effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial (Lancet Oncol. 2009;10:459-466) Cancer. 2010;116(8):1844–1846. doi: 10.1002/cncr.24950. [DOI] [PubMed] [Google Scholar]
- 5.Stupp R, Mason WP, van den Bent MJ. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 6.Dhami J, Chang E, Gambhir SS. Withaferin A and its potential role in glioblastoma (GBM) J Neurooncol. 2017;131(2):201–211. doi: 10.1007/s11060-016-2303-x. [DOI] [PubMed] [Google Scholar]
- 7.Shen X, Kan S, Liu Z. EVA1A inhibits GBM cell proliferation by inducing autophagy and apoptosis. Exp Cell Res. 2017;352:130–138. doi: 10.1016/j.yexcr.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 8.Lord CJ, Ashworth A. The DNA damage response and cancer therapy. Nature. 2012;481(7381):287–294. doi: 10.1038/nature10760. [DOI] [PubMed] [Google Scholar]
- 9.Lieberman HB. DNA damage repair and response proteins as targets for cancer therapy. Curr Med Chem. 2008;15(4):360–367. doi: 10.2174/092986708783497328. [DOI] [PubMed] [Google Scholar]
- 10.Jackson SP. The DNA-damage response: new molecular insights and new approaches to cancer therapy. Biochem Soc Trans. 2009;37(Pt 3):483–494. doi: 10.1042/BST0370483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li WQ, Hu N, Hyland PL. Genetic variants in DNA repair pathway genes and risk of esophageal squamous cell carcinoma and gastric adenocarcinoma in a Chinese population. Carcinogenesis. 2013;34(7):1536–1542. doi: 10.1093/carcin/bgt094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heyer WD, Li X, Rolfsmeier M. Rad54: the Swiss Army knife of homologous recombination? Nucleic Acids Res. 2006;34(15):4115–4125. doi: 10.1093/nar/gkl481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wright WD, Heyer WD. Rad54 functions as a heteroduplex DNA pump modulated by its DNA substrates and Rad51 during D loop formation. Mol Cell. 2014;53(3):420–432. doi: 10.1016/j.molcel.2013.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hicks WM, Yamaguchi M, Haber JE. Real-time analysis of double-strand DNA break repair by homologous recombination. Proc Natl Acad Sci U S A. 2011;108(8):3108–3115. doi: 10.1073/pnas.1019660108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sinha M, Peterson CL. A Rad51 presynaptic filament is sufficient to capture nucleosomal homology during recombinational repair of a DNA double-strand break. Mol Cell. 2008;30(6):803–810. doi: 10.1016/j.molcel.2008.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bonte D, Lindvall C, Liu H. Cdc7-Dbf4 kinase overexpression in multiple cancers and tumor cell lines is correlated with p53 inactivation. Neoplasia. 2008;10(9):920–931. doi: 10.1593/neo.08216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Melling N, Muth J, Simon R. Cdc7 overexpression is an independent prognostic marker and a potential therapeutic target in colorectal cancer. Diagn Pathol. 2015;10:125. doi: 10.1186/s13000-015-0360-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huggett MT, Tudzarova S, Proctor I. Cdc7 is a potent anti-cancer target in pancreatic cancer due to abrogation of the DNA origin activation checkpoint. Oncotarget. 2016;7(14):18495–18507. doi: 10.18632/oncotarget.7611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Erbayraktar Z, Alural B, Erbayraktar RS. Cell division cycle 7-kinase inhibitor PHA-767491 hydrochloride suppresses glioblastoma growth and invasiveness. Cancer Cell Int. 2016;16:88. doi: 10.1186/s12935-016-0364-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tenca P, Brotherton D, Montagnoli A. Cdc7 is an active kinase in human cancer cells undergoing replication stress. J Biol Chem. 2007;282(1):208–215. doi: 10.1074/jbc.M604457200. [DOI] [PubMed] [Google Scholar]
- 21.Sasi NK, Tiwari K, Soon FF. The potent Cdc7-Dbf4 (DDK) kinase inhibitor XL413 has limited activity in many cancer cell lines and discovery of potential new DDK inhibitor scaffolds. PLoS One. 2014;9(11) doi: 10.1371/journal.pone.0113300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mao P, Joshi K, Li J. Mesenchymal glioma stem cells are maintained by activated glycolytic metabolism involving aldehyde dehydrogenase 1A3. Proc Natl Acad Sci U S A. 2013;110(21):8644–8649. doi: 10.1073/pnas.1221478110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim JK, Jeon HY, Kim H. The molecular mechanisms underlying the therapeutic resistance of cancer stem cells. Arch Pharm Res. 2015;38(3):389–401. doi: 10.1007/s12272-014-0531-1. [DOI] [PubMed] [Google Scholar]
- 24.Pan Y, Zhang Q, Atsaves V. Suppression of Jab1/CSN5 induces radio- and chemo-sensitivity in nasopharyngeal carcinoma through changes to the DNA damage and repair pathways. Oncogene. 2013;32(22):2756–2766. doi: 10.1038/onc.2012.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rusin P, Walczak A, Zwierzchlejska A. DNA damage and repair of head and neck cancer cells after radio- and chemotherapy. Z Naturforsch C J Biosci. 2009;64(7-8):601–610. doi: 10.1515/znc-2009-7-821. [DOI] [PubMed] [Google Scholar]
- 26.Zhestianikov VD, Akimov AA, Savel'eva GE. The suppression of the repair of radio-induced DNA damage in Escherichia coli cells by indazolin derivatives and proksifein. Tsitologiia. 1996;38(11):1203–1210. [PubMed] [Google Scholar]
- 27.Lei M, Kawasaki Y, Young MR. Mcm2 is a target of regulation by Cdc7-Dbf4 during the initiation of DNA synthesis. Genes Dev. 1997;11(24):3365–3374. doi: 10.1101/gad.11.24.3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bruck I, Kaplan D. Dbf4-Cdc7 phosphorylation of Mcm2 is required for cell growth. J Biol Chem. 2009;284(42):28823–28831. doi: 10.1074/jbc.M109.039123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Montagnoli A, Moll J, Colotta F. Targeting cell division cycle 7 kinase: a new approach for cancer therapy. Clin Cancer Res. 2010;16(18):4503–4508. doi: 10.1158/1078-0432.CCR-10-0185. [DOI] [PubMed] [Google Scholar]
- 30.Tudzarova S, Mulholland P, Dey A. p53 controls CDC7 levels to reinforce G1 cell cycle arrest upon genotoxic stress. Cell Cycle. 2016;15(21):2958–2972. doi: 10.1080/15384101.2016.1231281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Montagnoli A, Valsasina B, Croci V. A Cdc7 kinase inhibitor restricts initiation of DNA replication and has antitumor activity. Nat Chem Biol. 2008;4(6):357–365. doi: 10.1038/nchembio.90. [DOI] [PubMed] [Google Scholar]