Abstract
Background
Variation in emergency physician computed tomography (CT) imaging utilization is well described, but little is known about what drives it. Physician empathy has been proposed as a potential characteristic affecting CT utilization.
Objectives
The objective was to describe empathy in a cohort of emergency physicians and evaluate its association with CT utilization. We also sought to compare emergency physician performance on an empathy psychometric test with performance on other psychometric tests previously proposed as predictors of CT utilization.
Methods
This cross-sectional study included two parts: 1) a secondary analysis of emergency department (ED) CT imaging utilization data in a large health system from July 2013 to June 2014 and 2) a survey study of the cohort of physicians responsible for this imaging using four psychometric scales: the Jefferson Scale of Empathy (JSE), a risk-taking subset of the Jackson Personality Index (RTS), the Stress from Uncertainty Scale (SUS), and the Malpractice Fear Scale (MFS). The study included data and physicians from four EDs: one urban, academic ED, two community, and one free-standing. A hierarchical, mixed-effects regression model was used to evaluate the association between emergency physician performance on the four scales and risk-adjusted CT imaging utilization. The model incorporated physician-specific CT utilization rates adjusted for propensity scores that were calculated using over 500 patient-level variables via random forest methods, physician demographics, and a random provider effect to account for the clustering of observations.
Results
CT variation analysis included 113,517 patients seen during the study period by the 74 eligible emergency physician survey respondents; 20,972 (18.5%) of these patients had at least one CT. The survey response rate was 74 of 82 (90.2%). Correlation coefficients between JSE and the other scales were not statistically significant. In subset analysis, there was a trend toward a physician’s number of years in practice and RTS score contributing to CT utilization for traumatic head CT. There were no significant associations between performance on any of the psychometric scales and CT utilization.
Conclusions
Performance on the JSE, RTS, SUS, or MFS was not predictive of risk-adjusted CT utilization in the ED. The underlying physician-based factors that mediate interphysician variation remain to be clearly identified.
Diagnostic imaging use is the fastest growing contributor to healthcare spending in the United States.1 Interventions that target practice variation in diagnostic imaging could improve healthcare delivery and reduce health care costs, cancer risk due to exposure to ionizing radiation, and downstream effects of incidental findings.2–6 In particular, there is significant variation in emergency physician utilization of computed tomography (CT) imaging, but the underlying causes of this variation remain unclear.7–13 Previous studies have suggested that physician characteristics, such as differences in physician risk tolerance or perceived malpractice risk, may account for the variation in emergency department (ED) decision-making.9–12,14–16
A previous qualitative study conducted by our group suggested that physician-based empathic factors such as the ability to care for patients by listening, reassuring, and identifying and addressing patient concerns play a large role in the decision-making process surrounding CT use in the ED.17,18 To our knowledge, empiric quantitative studies confirming these findings have not been conducted. We sought to determine quantitatively whether there is an association between empathy and CT use.
The Jefferson Scale of Empathy (JSE) is a validated psychometric tool that provides a quantitative measurement of empathy in healthcare providers.19–22 Previous work using the JSE has shown that a health professional’s capacity for empathy can change over the course of their education and training.23–25 To our knowledge, there is no evidence that empathy is associated with test use per se; however, higher physician JSE scores have been associated with improved clinical outcomes (in outpatients with diabetes and the common cold) and training programs have been shown to enhance empathy suggesting opportunities for targeted improvement.26–30 However, to our knowledge, the JSE has not previously been studied specifically in emergency physicians, nor has the link between JSE scores and variation in ED decision-making been explored.
We sought to describe empathy in a cohort of emergency physicians and evaluate the association between empathy and CT imaging utilization in the ED. We hypothesized that JSE scores in emergency physicians would be predictive of their CT imaging use (with more empathic physicians ordering fewer CTs to spare their patients from undue risk of unnecessary imaging). We also considered the possibility that the JSE could have a nonlinear relationship to CT use, hypothesizing that some more empathic physicians may order more CTs to decrease the likelihood of missing serious findings.
METHODS
Study Design
This study included two parts: 1) a secondary analysis of a retrospective cohort study of emergency physician CT imaging utilization data over 1 year and 2) a survey study of the same cohort of emergency physicians. Participating physicians were blinded to the study hypothesis. Survey results were deidentified, and the investigators were blinded to individual respondents’ scores on the surveys. The data from the two parts of the study were linked to evaluate the relationship between physician empathy, risk tolerance, malpractice fear, and stress from uncertainty instruments and CT utilization.
Study Setting and Population
This study was performed across four sites in a single healthcare system. The sites were: 1) a large, urban, academic, adult, tertiary care, Level I trauma center ED with over 90,000 annual visits; 2) an urban, community, Level II trauma center ED with over 70,000 annual visits; 3) an urban, community hospital ED with over 75,000 annual visits; and 4) a suburban, community, free-standing ED with over 30,000 annual visits. All four EDs are in the same geographic region. The first two sites have resident physicians, although the academic site is the main site for the residency and its affiliated medical school. All four sites have midlevel providers practicing in the ED under the supervision of the attending physicians. The decision to order a CT scan at these sites has no specific structure, guided instead by the individual attending emergency physician’s evaluation and assessment of each individual patient. At the time of the analysis there was no computerized clinical decision support with CT imaging guidelines. The institutional review board at each participating site approved the study protocol.
The survey cohort consisted of attending physicians practicing in the study EDs. No residents or midlevel providers were included. The secondary data set analysis included all patients 18 years of age and older under the care of these physicians from July 2013 to June 2014. The survey was administered only to physicians whose practice variation data was linkable from the first part of the study and who had seen > 25 patients for each condition. Four study authors were excluded because they were not blinded to the study hypothesis. The total number of attending emergency physicians practicing across the healthcare system and the number of patients that they cared for over a 1-year period determined the study size.
Data Collection and Processing
The four study EDs are part of a larger health system that includes an integrated electronic health record. Electronic health record data from all sites are stored in a central data warehouse, from which we obtained CT utilization data and encounter-level information. Patient-specific data included demographic information (age, sex, race, etc.). Encounter-level data included vitals, labs, current outpatient medications and those given in the ED, past medical history, chief complaint, emergency severity index, day of the week, time of day, and care area, etc., totaling over 500 variables (see Data Supplement S1, available as supporting information in the online version of this paper). CT use was attributed to the attending physician working at the time the CT was ordered. CTs could have been ordered by the attending physician or residents or midlevel providers caring for the patient under the supervision of the attending physician. No EDs involved in the study permit a triage physician or nurse to order CTs. The primary outcome for each model was whether a patient received a particular type of CT scan during their ED visit. For patients with multiple body areas imaged (i.e., different CT types) in a single encounter, each type was considered in the analysis. However, for the purposes of the main model of overall CT utilization, subjects who received multiple CTs were counted only once for the outcome of any CT performed (Figure 1). Electronic health record text data in numerical fields were converted or dropped if a numerical value could not be obtained; errant text data in categorical fields were converted into a structured format through regular expression searches. Data elements were smoothed and discretized using k-means clustering for continuous data.31
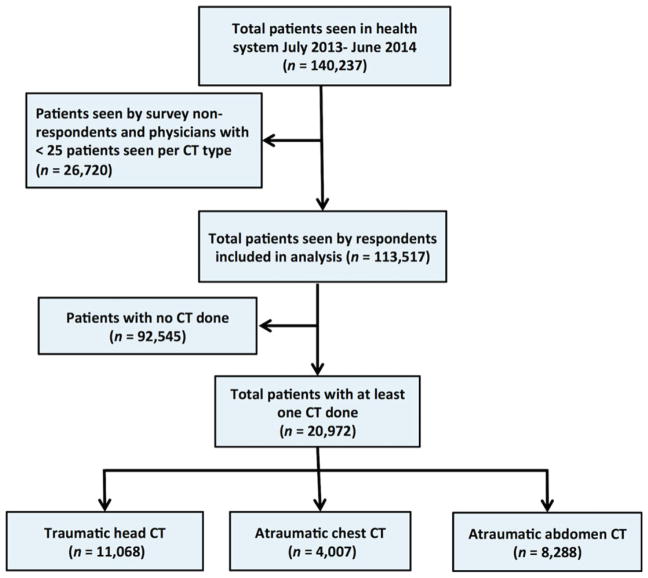
Figure 1.
Flow diagram of patients included in the analysis.
Surveys were administered on paper and included questions from four self-reported psychometric survey instruments. Before completing the survey, physicians were verbally consented to participate. To address loss to follow-up, physicians practicing during the study period were contacted via e-mail to complete the survey. To mitigate reporting bias, participants were blinded to the study hypothesis. Six respondents returned surveys containing up to two missing items. Missing items were assigned a zero value when scoring the corresponding instrument.
The four psychometric survey instruments administered were: 1) the JSE, 2) a risk-taking subscale (RTS) of the Jackson Personality Index, 3) the Stress from Uncertainty Scale (SUS), and 4) the Malpractice Fear Scale (MFS).14,19,20,32,33 Attending emergency physician demographic data were also collected, including physician age, sex, race, ethnicity, years in practice, and primary clinical practice site. The JSE is a psychometric tool widely used and validated in healthcare professionals and trainees.19,21 The JSE has been well validated in terms of test–retest reliability (coefficient of 0.65),21 internal consistency,19,21 predictive validity,22 criterion-related validity,19,34 and construct validity.19,21 The alpha reliability estimate for physicians taking the test was 0.87.19 It consists of 20 items, each rated on a 7-point Likert scale. A proprietary scoring algorithm is used to determine the individual’s score. Possible scores range from 20 to 140, with higher scores corresponding to higher levels of empathy. The JSE was validated in a study of 704 physicians from a single health system, only 23 of whom were emergency physicians.19 To our knowledge, it has not otherwise been applied specifically to a large or focused study of emergency physicians. The RTS is a subset of the Jackson Personality Index and has been used to measure general risk-taking behavior in emergency physicians.9,14,35 It has six items, each rated on a 6-point Likert scale. Possible scores range from 6 to 36, and higher scores correspond to increased risk-taking. The SUS is a validated psychometric tool that measures physician’s stress from uncertainty in patient care.33 It was validated with a Cronbach’s alpha of 0.90.33 It has 13 items, each rated on a 6-point Likert scale. Potential scores range from 13 to 78, with higher scores corresponding to higher stress due to uncertainty. The MFS is a validated scale with six items that has been used previously to study fear of malpractice in primary care and emergency physicians.9,36–38 The scale was developed based on expert opinion and factor analysis; its developers reported a Cronbach’s alpha of 0.88.14 Items are rated on a 5-point Likert scale. Possible scores range from 6 to 30, with higher scores corresponding to increased fear of malpractice.
Data Analysis
We used a hierarchical, mixed-effects logistic regression model to evaluate the association between physician personal characteristics and physician performance on the four psychometric scales with CT imaging utilization (R Statistical Software, glmer package). Since there are validated, well-accepted clinical decision-making tools for CT imaging use that aim to decrease imaging variation in cases of suspected pulmonary embolism and head injury, four models were developed to examine how empathy may affect: 1—overall CT utilization and also CT utilization amongst imaging studies that have high (2—traumatic head and 3—atraumatic chest) and low (4—atraumatic abdominal pain) levels of evidence and clinical practice guideline recommendations.39–45 Abdominal CTs included abdomen/pelvis protocols, but not pelvis-only protocols. Model construction followed a purposeful covariate selection strategy while examining for interactions between the different psychometric scores.46 We determined a priori an appropriate events-to-covariates ratio of 10:1 or greater.47 To account for the clustering of observations, random effects at the physician and hospital level were included. We adjusted for potential confounders at the encounter level by incorporating propensity scores for CT imaging into the model. Propensity scores were determined by random forest methodology.48 Random forest methodology was chosen because of its excellent performance in terms of covariate balance and effect estimation, ability to handle a large number of predictors (>500 in this study), and nonparametric nature.49 Each random forest (R statistical software, cforest package) was generated with 1000 trees and examined a random selection of 25 encounter-level variables at each node split (approximately the square root of the number of independent variables).48 Goodness of fit was assessed through the Akaike information criterion and the Hosmer-Lemeshow test.
We also analyzed the relationship between JSE, physician demographics, and the three additional psychometric scales using hierarchical linear regression (R statistical software, lme4 package). The validity of model assumptions was analyzed though diagnostic plots (residual plots, normal QQ plots, etc.), and goodness of fit was assessed through the coefficient of determination.
To test for the possibility of selection bias amongst our responders, demographic factors (age and years in practice) and CT utilization rates of the 74 physicians who responded to the survey were compared with those of the nonrespondents using t-tests. We considered a p-value of <0.05 significant for the preliminary t-tests and linear regression. We adjusted the p-value for the four logistic models (using Bonferroni correction such that a p-value of <0.0125 was considered significant).
RESULTS
A total of 140,237 patients visited the four EDs during the 12-month study period. Of these, 113,517 were under the care of the survey respondents and were included in the analysis. There were 20,972 (18.5%) patients with at least one CT performed during their ED visit. Figure 1 provides a flow diagram from the total patients seen in the EDs during the study period through those included in each model in the analysis. Table 1 shows the demographic and clinical characteristics of the 113,517 patient encounters included in the analysis.
Table 1.
Patient Characteristics and CT Imaging
| Category | All Patients, N = 113,517 | No CT Performed, n = 92,545 | Any CT Performed, n = 20,972 | p-value (No CT vs. CT) | Traumatic Head CT, n = 11068 | Atraumatic chest CT, n = 4,007 | Atraumatic Abdominal CT, n = 8,288 |
|---|---|---|---|---|---|---|---|
| Age (y) | 52 ± 9 | 50 ± 8 | 59 ± 7 | <0.001 | 63 ± 10 | 62 ± 6 | 56 ± 7 |
| Sex | |||||||
| Male | 50,827 (44.8) | 41,780 (45.1) | 9,047 (43.1) | <0.001 | 5,039 (45.5) | 1,781 (44.4) | 3,524 (42.5) |
| Female | 62,690 (55.2) | 50,765 (54.9) | 11,925 (56.9) | <0.001 | 6,029 (54.5) | 2,226 (55.6) | 4,764 (57.5) |
| Race | |||||||
| Black or African-American | 30,760 (27.1) | 26,255 (28.4) | 4,505 (21.5) | <0.001 | 2,210 (20.0) | 838 (20.9) | 1,774 (21.4) |
| White | 59,544 (52.5) | 46,592 (50.3) | 12,952 (61.8) | <0.001 | 7,162 (64.7) | 2,576 (55.6) | 4,923 (59.4) |
| Asian | 816 (0.7) | 687 (0.74) | 129 (0.6) | 0.049 | 71 (0.6) | 26 (0.6) | 50 (0.6) |
| Other | 20,219 (17.8) | 17,178 (18.5) | 3,041 (14.5) | <0.001 | 19 (0.2) | 511 (12.8) | 1,393 (16.8) |
| Unknown | 339 (0.3) | 280 (0.3) | 59 (0.3) | 0.61 | 173 (1.6) | 9 (0.2) | 22 (0.3) |
| Ethnicity | |||||||
| Hispanic or Latino origin | 22,703 (20.0) | 18,299 (19.8) | 4,404 (21.0) | <0.001 | 1,992 (18.0) | 801 (20.0) | 1,409 (17.0) |
| Not of Hispanic or Latino origin | 90,814 (80.0) | 74,246 (80.2) | 16,568 (79.0) | <0.001 | 9,076 (82.0) | 3,206 (80.0) | 6,879 (83.0) |
| Insurance type | |||||||
| Medicaid | 39,198 (34.5) | 33,921 (36.7) | 5,277 (25.2) | <0.001 | 2,500 (22.6) | 1,057 (26.4) | 2,282 (27.5) |
| Medicare | 29,277 (25.8) | 22,073 (23.9) | 7,204 (34.4) | <0.001 | 4,383 (39.6) | 1,248 (31.1) | 2,445 (29.5) |
| Managed care | 12,146 (10.7) | 9,937 (10.7) | 2,209 (10.5) | 0.387 | 922 (8.3) | 477 (11.9) | 1,007 (12.2) |
| Medicare managed care | 9,279 (8.2) | 6,823 (7.3) | 2,456 (11.7) | <0.001 | 1454 (8.3) | 468 (11.7) | 851 (10.3) |
| Self-pay | 7,144 (6.3) | 6,384 (6.8) | 760 (3.6) | <0.001 | 437 (3.9) | 110 (2.7) | 301 (3.6) |
| Blue Cross Blue Shield | 12,522 (11.0) | 10,110 (10.9) | 2,412 (11.5) | 0.016 | 982 (8.9) | 487 (12.2) | 1,141 (13.8) |
| Acuity level* | |||||||
| Immediate | 1,389 (1.2) | 1,028 (11.1) | 361 (1.7) | <0.001 | 293 (2.6) | 84 (2.1) | 95 (1.1) |
| Emergent | 38,015 (33.5) | 29,690 (32.1) | 8,325 (39.7) | <0.001 | 5,159 (46.6) | 1,639 (40.9) | 2,431 (29.3) |
| Urgent | 61,975 (54.6) | 50,322 (54.4) | 11,653 (55.6) | 0.002 | 5,218 (47.1) | 1,753 (43.7) | 5,593 (67.5) |
| Less urgent | 10,398 (9.2) | 9,886 (10.7) | 512 (2.4) | <0.001 | 328 (3.0) | 189 (4.7) | 115 (1.4) |
| Nonurgent | 1,112 (1.0) | 11,106 (12.0) | 6 (0.0) | <0.001 | 4 (0.0) | 1 (0.0) | 0 (0.0) |
| Unspecified | 628 (0.6) | 513 (0.5) | 115 (0.5) | 0.91 | 66 (0.6) | 28 (0.7) | 54 (0.7) |
Data are reported as mean ± SD or n (%).
Emergency Severity Index.
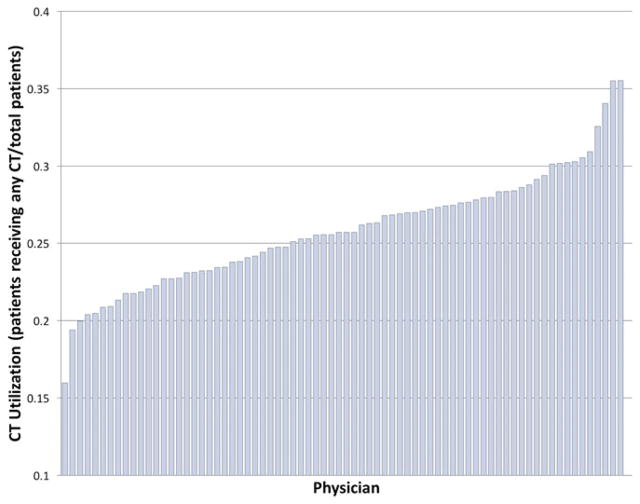
Surveys were distributed to 82 eligible emergency physicians employed in our health care system. Of these eligible physicians, 74 (90.2%) responded. Our respondents had a mean (±SD) age of 44 (±9) years; 60% were male, 77% were white, and 50% were in academic practice. Eight physicians did not complete the survey. No significant differences were found between the two groups (age p = 0.116, years in practice p = 0.207, CT utilization rate p = 0.312). Table 2 shows the demographics and characteristics of the respondents. All 74 physicians met minimum volume criteria and could be linked to the secondary dataset analysis. Table 3 and Figure 2 describe the variation in CT utilization between the physicians and by indication. There was substantial variation by indication but not by site.
Table 2.
Characteristics and Demographics of the Physician Survey Respondents
| Category | All Physicians (N = 74) |
|---|---|
| Age (y) | 44 ± 9 |
| Sex | |
| Male | 44 (60) |
| Female | 30 (40) |
| Race | |
| Black or African-American | 5 (7) |
| White | 57 (77) |
| Asian | 6 (8) |
| Other | 4 (5) |
| Native Hawaiian or Pacific Islander | 2 (3) |
| Ethnicity | |
| Hispanic or Latino origin | 3 (4) |
| Not of Hispanic or Latino origin | 71 (96) |
| Hospital type | |
| Academic | 37 (50) |
| Community | 14 (19) |
| Community/teaching | 23 (31) |
| Years in practice, including residency | 15.5 ± 8.4 |
| Psychometric scores | |
| Jefferson Scale of Empathy | 114 ± 12 |
| Risk-taking Scale | 21 ± 6 |
| Stress from Uncertainty Scale | 36 ± 12 |
| Malpractice Fear Scale | 17 ± 6 |
Data are reported as mean ± SD or n (%).
Table 3.
Variation in CT Utilization by Indication and Location
| Indication | Academic* (n = 37) | Community/Teaching* (n = 23) | Community (n = 14) | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Mean ± SD | CV | Mean ± SD | CV | Mean ± SD | CV | |
| Overall | 26.2 ± 4.2 | 16.2 | 25.7 ± 3.5 | 13.7 | 24.7 ± 2.7 | 10.9 |
| Traumatic head | 10.6 ± 2.2 | 20.4 | 10.7 ± 1.9 | 17.6 | 9.7 ± 1.9 | 19.3 |
| Atraumatic chest | 3.9 ± 0.6 | 14.9 | 3.9 ± 0.5 | 12.3 | 3.8 ± 0.3 | 7.1 |
| Atraumatic abdominal pain | 7.5 ± 1.3 | 17.4 | 7.9 ± 1.5 | 19.3 | 7.3 ± 1.0 | 13.9 |
Resident involvement in the care of patients at these sites (Sites 1 and 2 as described in text).
CT = computed tomography; CV = coefficient of variation.
Figure 2.
CT utilization by physician: Displayed as ratio of patients who received any CT divided by the number of patients cared for by the physician during the study period. CT = computed tomography.
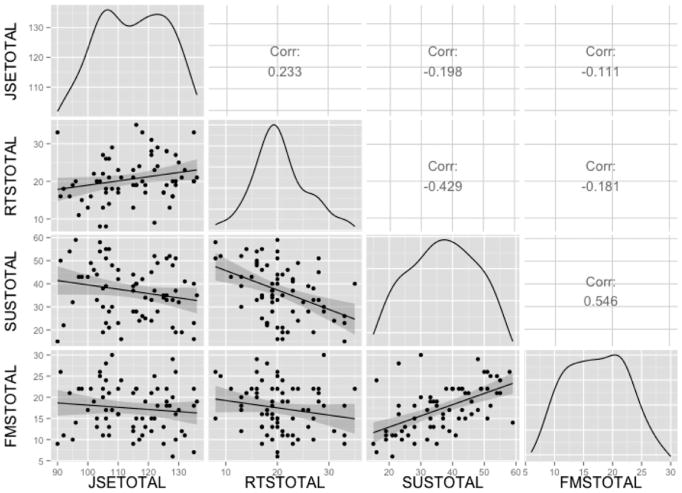
Psychometric scores for each scale were used to produce distribution plots and scatter plot matrices and correlation coefficients between the four psychometric scales (Figure 3). There were no statistically significant correlation coefficients that suggested strong associations (>0.8) between the scales. The coefficients (and their p-values) were 0.233 (p = 0.08) for JSE and RTS, −0.198 (p = 0.14) for JSE and SUS, −0.111(p = 0.48) for JSE and MFS, −0.429 (p = < 0.001) for RTS and SUS, −0.181 (p = 0.096) for RTS and MFS, and 0.546 (p = < 0.001) for SUS and MFS (Data Supplement S2, available as supporting information in the online version of this paper). Analysis using a mixed-effects regression model revealed no significant relationships between survey scores and CT utilization rates, including aggregate rates and rates for studies with both high and low levels of evidence and guideline recommendations (Table 4). In a subset analysis, there was a trend toward a physician’s number of years in practice and the RTS score contributing to CT utilization for traumatic head CT, which after Bonferroni correction was not significant. To account for possible threshold effects within the JSE scale, we divided the risk scale into quartiles, quintiles, and 15 bins. There were no threshold effects identified for the JSE.
Figure 3.
Scatterplot matrix and distribution of psychometric scores of physicians. Distribution of emergency physician scores on the Jefferson Scale of Empathy (JSE), a risk-taking subscale (RTS) of the Jackson Personality Index, the Stress from Uncertainty Scale (SUS), and the Malpractice Fear Scale (MFS) with scatterplot matrix and correlation between the scales.
Table 4.
Logistic Regression Models to Predict Risk-adjusted CT Utilization Rate by Provider
| All CTs, aOR (95% CI) | p-value | Traumatic Head, aOR (95% CI) | p-value | Atraumatic Chest, aOR (95% CI) | p-value | Atraumatic Abdomen, aOR (95% CI) | p-value | |
|---|---|---|---|---|---|---|---|---|
| Propensity score | 1.069 (1.067–1.070) | <0.001 | 1.072 (1.069–1.075) | <0.001 | 1.137 (1.138–1.141) | <0.001 | 1.12 (1.119–1.126) | <0.001 |
| Physician sex (male) | 0.977 (0.857–1.113) | 0.724 | 1.084 (0.898–1.309) | 0.40 | 0.876 (0.760–1.01) | 0.069 | 0.990 (0.845–1.161) | 0.91 |
| Physician ethnicity (not Hispanic or Latino) | 0.970 (0.720–1.305) | 0.839 | 1.057 (0.684 – 1.634) | 0.80 | 1.048 (0.765–1.435) | 0.77 | 1.093 (0.749–1.594) | 0.64 |
| Year practicing | 0.995 (0.987–1.003) | 0.199 | 0.987 (0.975–0.998) | 0.02 | 1.005 (0.995–1.015) | 0.31 | 0.995 (0.981–1.002) | 0.10 |
| Jefferson Scale of Empathy | 0.996 (0.992–1.001) | 0.163 | 0.997 (0.990 –1.004) | 0.43 | 0.998 (0.992 –1.003) | 0.44 | 0.995 (0.989–1.001) | 0.12 |
| Risk-taking Scale | 0.990 (0.978–1.002) | 0.105 | 0.982 (0.965 –1.000) | 0.05 | 1.004 (0.991–1.018) | 0.55 | 0.990 (0.975–1.005) | 0.17 |
| Malpractice Fear Scale | 1.001 (0.989–1.013) | 0.859 | 0.992 (0.974 – 1.009) | 0.37 | 0.997 (0.984–1.010) | 0.67 | 1.00 (0.985–1.015) | 0.98 |
| Stress from Uncertainty Scale | 1.001 (0.994–1.008) | 0.786 | 0.995 (0.986–1.006) | 0.42 | 1.004 (0.996–1.011) | 0.34 | 0.998 (0.989–1.006) | 0.69 |
aOR = adjusted odds ratio; CT = computed tomography.
A secondary analysis exploring for nonlinear relationships between empathy and CT use was conducted by adding a squared term for JSE. In the secondary analysis, the JSE2 term had an odds ratio of 0.993 (95% CI = 0.987–0.999), which after Bonferroni correction was not significant.
DISCUSSION
Key Results
Physician characteristics have been proposed as contributors to overuse of diagnostic imaging in the ED.9,18 Our objective was to evaluate the association between empathy and clinical decision-making regarding CT imaging in the ED, with the hypothesis that JSE scores of attending emergency physicians would be predictive of their CT imaging use. In this cross-sectional analysis of CT utilization and survey of emergency physicians, we found substantial variation in CT use between physicians and by indication for CT but not by study site. However, none of the physician characteristics, including demographics, years in practice, and self-reported scores on instruments that measure empathy, risk aversion, fear of malpractice, and stress from uncertainty, were predictive of risk-adjusted ED CT utilization over a 1-year period in a large health system. We also evaluated whether physician-based psychometric scores correlated with CT utilization for scans with varying levels of evidence. The presence or lack of imaging guidelines did not contribute to the effect of any of the four psychometric scales on risk-adjusted CT variation.
Empathy in emergency physicians has not previously been quantified and, to our knowledge, the JSE has not previously been exclusively validated for emergency physicians. Interestingly, there appears to be a bimodal distribution in JSE scores among our respondents (Figure 3). It is unclear if this characteristic is unique to emergency physicians, as it has not been described in other specialties.
Interpretation
Our findings differ from some previous studies evaluating the studied scales and ED decision-making. Higher RTS scores among physicians have been shown to correlate with greater use of diagnostic imaging in patients with abdominal pain (accounting for 11%–15% of imaging variation), as well as greater use of head CTs in pediatric (but not adult) patients with minor head injuries.9,10,38 Our study, which included a much larger sample size across a healthcare system and more robust risk adjustment methods than previous work, found no correlation between RTS scores and CT use for adult patients, including subset analyses for traumatic head CT and atraumatic abdominal CT. This indicates that emergency physician risk aversion may not play as large a role in diagnostic imaging variation in adult patients as previously reported. We could have observed these findings if physicians had limited effect on CT use in the ED as described by Wong et al.50 However, significant variation exists in CT utilization between physicians in our system (Figure 2). Given these data and our previous qualitative findings, we still believe that physician characteristics are important contributors to this variation.17,18 So, either the scales we used did not adequately measure the physician characteristics that contribute, the interactions of the characteristics are more complex than our models could describe, or our study was underpowered. Given the sample size we used and positive correlations found in previous, smaller studies, insufficient power is unlikely. To increase survey response rate, surveys were administered in person when possible to emergency physicians—both in clinical and in nonclinical environments. The respondents in this study completed the survey at varied times during their shifts, as well as in nonclinical environments. Because the JSE has never been validated in emergency physicians, it is unclear how static the scores would be before, after, or during a busy shift. Given the disruptive, high-stress ED environment, it is possible that test–retest validity of the JSE would not hold before, during, and after a busy ED shift. Therefore, measurement failure is one explanation for the lack of association between the JSE and CT utilization.
Based on anecdotal evidence prior to the analysis, the authors discussed a possible nonlinear relationship between empathy and CT utilization (e.g., very empathic physicians may order fewer tests or many tests depending on their views on overuse). Therefore, we decided to conduct a secondary analysis exploring for nonlinear relationships between empathy and CT. However, we did not find a significant relationship. We believe, however, that based on a trend toward significance, this relationship should be further investigated, e.g., with a larger sample size of physicians, after formalized validation of the JSE in emergency physicians, or with more standardized survey administration. Furthermore, if the interactions of the physician characteristics that contribute to variation in CT utilization are more complex than our models could describe, future research should attempt to better describe these types of interactions both qualitatively and quantitatively. In particular, clinician empathy is inherently complex but understudied in the ED.51,52
Similarly, mixed evidence exists for the role of stress from uncertainty and fear of malpractice in imaging use. Lower levels of stress from diagnostic uncertainty may correlate with lower care costs for internists.53 However, other studies have shown no correlation between practice variation and stress from uncertainty.9,10 In a study of emergency physicians, those with higher malpractice fear scores had higher rates of laboratory ordering and hospital admission in patients with low-risk chest pain.14 Other studies have shown no correlation between practice variation and MFS scores.9,10 We also found no correlation between CT utilization and either the SUS or the MFS scores.
Generalizability
To increase the external validity to our results, we included four practice sites across our health system, including a large, tertiary academic center and three community hospitals. There was a high (74/82 = 90%) response rate among the physicians surveyed. There are limited data available about the current demographics of emergency physicians in the United States. A study in 1999 of 6,719 emergency physicians showed 83% male physicians and 82% white.54 A more recent survey study of 435 emergency physicians in an academic emergency medicine journal reported a mean age of 58.5 years, 56.6% male, and 54.5% in academic practice.55 Our respondents, who had a mean age of 44 (±9) years, were 60% male, 77% white, and 50% in academic practice, are likely representative of emergency physician demographics across the United States. Since this study was conducted across a single health system within the same state, its generalizability may be limited due to regional and local practice patterns (i.e., CT use) and local culture (i.e., responses to the scales used).
LIMITATIONS
There are several limitations of this study. Although the propensity scores incorporated over 500 encounter-level variables, there may be unmeasured confounders that our regression models could not account for. For example, resident and midlevel providers can order CTs independently from the supervising attending physicians in our system. We did not directly control for this, instead choosing to adjust for differences across sites with the assumption that—on the aggregate—residents and mid-level providers would order CTs in accordance with the attending’s physician’s practice style. Half of the physicians surveyed work primarily at a large academic teaching institution where the presence of residents and consulting services may affect clinical practice variation due to the role they play in the decision to order a CT. The survey data were collected approximately 1 year after the CT variation data were collected, and the constructs tested by the four scales may have changed in individual physicians over this time period. The trend toward physician’s number of years in practice and RTS score contributing to CT utilization for traumatic head CT suggests that a larger sample size could more readily distinguish whether or not this is a trend or a true contributing factor to CT utilization in this situation. For patients who received multiple CTs, the choice of the outcome of any CT performed may have decreased the variability we saw in CT use between providers.
CONCLUSION
Variation in ED practice remains a target for improving healthcare quality, safety, efficiency, and costs, yet the physician factors as measured in this analysis were not associated with physician-level variation in computed tomography utilization. The underlying physician-based factors that mediate interphysician variation remain to be clearly identified. Future research should evaluate the Jefferson Scale of Empathy exclusively in emergency physicians and administer surveys in a more controlled manner (e.g., nonclinical setting). Additional research should seek to describe and quantify the role of physician empathy in emergency care.
Supplementary Material
Variables included in random forest model for propensity scores.
Linear regression to predict JSE by physician demographics and the three other psychometric scales.
Acknowledgments
ERM is supported, in part, by grant number K08HS021271 from the Agency for Healthcare Research and Quality (www.ahrq.gov). AKV is supported by the Emergency Medicine Foundation (www.emergencymedicinefoundation.org) Health Policy Scholar Award. He also works under contract with the Centers for Medicare and Medicaid Services (www.cms.gov) in the development of hospital outcome and efficiency measures inclusive of hospital imaging use. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, the Centers for Medicare & Medicaid Services, or the Emergency Medicine Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors express their gratitude to Caitlin Johnson for facilitating the IRB process.
Footnotes
Presented at the Society for Academic Emergency Medicine (SAEM) New England Regional Meeting, Worcester, MA, April 2016; and the SAEM Annual Meeting, New Orleans, LA, May 2016.
The authors have no potential conflicts to disclose.
The following supporting information is available in the online version of this paper
References
- 1.Medicare Payment Advisory Commission. A Data Book: Health Care Spending and the Medicare Program. 2014. [Google Scholar]
- 2.Newhouse JP, Graham RP, McCoy MA, et al. Institute of Medicine: Committee on Geographic Variation in Health Care Spending and Promotion of High-Value Care. 2013. Variation in health care spending: target decision making, not geography. [PubMed] [Google Scholar]
- 3.Venkatesh AK, Schuur JD. A “Top Five” list for emergency medicine: a policy and research agenda for stewardship to improve the value of emergency care. Am J Emerg Med. 2013;31:1520–4. doi: 10.1016/j.ajem.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 4.Berland LL, Silverman SG, Gore RM, et al. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol. 2010;7:754–73. doi: 10.1016/j.jacr.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Pickhardt PJ, Hanson ME, Vanness DJ, et al. Unsuspected extracolonic findings at screening CT colonography: clinical and economic impact. Radiology. 2008;249:151–9. doi: 10.1148/radiol.2491072148. [DOI] [PubMed] [Google Scholar]
- 6.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169:2078–86. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stiell IG, Wells GA, Vandemheen K, et al. Variation in ED use of computed tomography for patients with minor head injury. Ann Emerg Med. 1997;30:14–22. doi: 10.1016/s0196-0644(97)70104-5. [DOI] [PubMed] [Google Scholar]
- 8.Jain S, Elon LK, Johnson BA, Frank G, Deguzman M. Physician practice variation in the pediatric emergency department and its impact on resource use and quality of care. Pediatr Emerg Care. 2010;26:902–8. doi: 10.1097/PEC.0b013e3181fe9108. [DOI] [PubMed] [Google Scholar]
- 9.Pines JM, Hollander JE, Isserman JA, et al. The association between physician risk tolerance and imaging use in abdominal pain. Am J Emerg Med. 2009;27:552–7. doi: 10.1016/j.ajem.2008.04.031. [DOI] [PubMed] [Google Scholar]
- 10.Andruchow JE, Raja AS, Prevedello LM, Zane RD, Khorasani R. Variation in head computed tomography use for emergency department trauma patients and physician risk tolerance. Arch Intern Med. 2012;172:660–1. doi: 10.1001/archinternmed.2011.2243. [DOI] [PubMed] [Google Scholar]
- 11.Stanley RM, Hoyle JD, Jr, Dayan PS, et al. Emergency department practice variation in computed tomography use for children with minor blunt head trauma. J Pediatr. 2014;165:1201–6e2. doi: 10.1016/j.jpeds.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 12.Chen YA, Gray BG, Bandiera G, MacKinnon D, Deva DP. Variation in the utilization and positivity rates of CT pulmonary angiography among emergency physicians at a tertiary academic emergency department. Emerg Radiol. 2015;22:221–9. doi: 10.1007/s10140-014-1265-6. [DOI] [PubMed] [Google Scholar]
- 13.Mutrie D, Bailey SK, Malik S. Individual emergency physician admission rates: predictably unpredictable. CJEM. 2009;11:149–55. doi: 10.1017/s1481803500011118. [DOI] [PubMed] [Google Scholar]
- 14.Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patients with possible acute cardiac ischemia. Ann Emerg Med. 2005;46:525–33. doi: 10.1016/j.annemergmed.2005.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Probst MA, Kanzaria HK, Schriger DL. A conceptual model of emergency physician decision making for head computed tomography in mild head injury. Am J Emerg Med. 2014;32:645–50. doi: 10.1016/j.ajem.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoffman JR, Kanzaria HK. Intolerance of error and culture of blame drive medical excess. BMJ. 2014;349:g5702. doi: 10.1136/bmj.g5702. [DOI] [PubMed] [Google Scholar]
- 17.Melnick ER, Shafer K, Rodulfo N, et al. Understanding overuse of computed tomography for minor head injury in the emergency department: a triangulated qualitative study. Acad Emerg Med. 2015;22:1474–83. doi: 10.1111/acem.12824. [DOI] [PubMed] [Google Scholar]
- 18.Melnick ER. How to make less more: empathy can fill the gap left by reducing unnecessary care. BMJ. 2015;351:h5831. doi: 10.1136/bmj.h5831. [DOI] [PubMed] [Google Scholar]
- 19.Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ Psychol Measure. 2001;61:349–65. [Google Scholar]
- 20.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloksi JJ, Magee M. The Jefferson Scale of Physician Empathy: further psychometric data and differences by gender and specialty at item level. Acad Med. 2002;77:S58–60. doi: 10.1097/00001888-200210001-00019. [DOI] [PubMed] [Google Scholar]
- 21.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–9. doi: 10.1176/appi.ajp.159.9.1563. [DOI] [PubMed] [Google Scholar]
- 22.Hojat M, Mangione S, Nasca TJ, Gonnella JS, Magee M. Empathy scores in medical school and ratings of empathic behavior in residency training 3 years later. J Soc Psychol. 2005;145:663–72. doi: 10.3200/SOCP.145.6.663-672. [DOI] [PubMed] [Google Scholar]
- 23.Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84:1182–91. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 24.Hojat M, Mangione S, Nasca TJ, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38:934–41. doi: 10.1111/j.1365-2929.2004.01911.x. [DOI] [PubMed] [Google Scholar]
- 25.Mangione S, Kane GC, Caruso JW, Gonnella JS, Nasca TJ, Hojat M. Assessment of empathy in different years of internal medicine training. Med Teach. 2002;24:370–3. doi: 10.1080/01421590220145725. [DOI] [PubMed] [Google Scholar]
- 26.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359–64. doi: 10.1097/ACM.0b013e3182086fe1. [DOI] [PubMed] [Google Scholar]
- 27.Del Canale S, Louis DZ, Maio V, et al. The relationship between physician empathy and disease complications: an empirical study of primary care physicians and their diabetic patients in Parma, Italy. Acad Med. 2012;87:1243–9. doi: 10.1097/ACM.0b013e3182628fbf. [DOI] [PubMed] [Google Scholar]
- 28.Chen JT, LaLopa J, Dang DK. Impact of patient empathy modeling on pharmacy students caring for the underserved. Am J Pharm Educ. 2008;72:40. doi: 10.5688/aj720240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fernandez-Olano C, Montoya-Fernandez J, Salinas-Sanchez A. Impact of clinical interview training on the empathy level of medical students and medical residents. Med Teach. 2008;30:322–4. doi: 10.1080/01421590701802299. [DOI] [PubMed] [Google Scholar]
- 30.Rakel D, Barrett B, Zhang Z, et al. Perception of empathy in the therapeutic encounter: effects on the common cold. Patient Educ Couns. 2011;85:390–7. doi: 10.1016/j.pec.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dougherty J, Kohavi R, Sahami M. Supervised and unsupervised discretization of continuous features. Machine Learning: Proceedings of the Twelfth International Conference. 1995;12:194–202. [Google Scholar]
- 32.Jackson D. Jackson Personality Inventory Manual. Port Huron, MI: Research Psychologists Press; 1976. [Google Scholar]
- 33.Gerrity MS, DeVellis RF, Earp JA. Physicians’ reactions to uncertainty in patient care. A new measure and new insights. Med Care. 1990;28:724–36. doi: 10.1097/00005650-199008000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Hojat M, Gonnella JS, Mangione S, et al. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36:522–7. doi: 10.1046/j.1365-2923.2002.01234.x. [DOI] [PubMed] [Google Scholar]
- 35.Pines JM, Isserman JA, Szyld D, Dean AJ, McCusker CM, Hollander JE. The effect of physician risk tolerance and the presence of an observation unit on decision making for ED patients with chest pain. Am J Emerg Med. 2010;28:771–9. doi: 10.1016/j.ajem.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 36.Fiscella K, Franks P, Zwanziger J, Mooney C, Sorbero M, Williams GC. Risk aversion and costs: a comparison of family physicians and general internists. J Fam Pract. 2000;49:12–7. [PubMed] [Google Scholar]
- 37.Franks P, Williams GC, Zwanziger J, Mooney C, Sorbero M. Why do physicians vary so widely in their referral rates? J Gen Intern Med. 2000;15:163–8. doi: 10.1046/j.1525-1497.2000.04079.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wong AC, Kowalenko T, Roahen-Harrison S, Smith B, Maio RF, Stanley RM. A survey of emergency physicians’ fear of malpractice and its association with the decision to order computed tomography scans for children with minor head trauma. Pediatr Emerg Care. 2011;27:182–5. doi: 10.1097/PEC.0b013e31820d64f7. [DOI] [PubMed] [Google Scholar]
- 39.Wells PS, Anderson DR, Rodger M, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med. 2001;135:98–107. doi: 10.7326/0003-4819-135-2-200107170-00010. [DOI] [PubMed] [Google Scholar]
- 40.Le Gal G, Righini M, Roy PM, et al. Prediction of pulmonary embolism in the emergency department: the revised Geneva score. Ann Intern Med. 2006;144:165–71. doi: 10.7326/0003-4819-144-3-200602070-00004. [DOI] [PubMed] [Google Scholar]
- 41.Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357:1391–6. doi: 10.1016/s0140-6736(00)04561-x. [DOI] [PubMed] [Google Scholar]
- 42.Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000;343:100–5. doi: 10.1056/NEJM200007133430204. [DOI] [PubMed] [Google Scholar]
- 43.Jagoda AS, Bazarian JJ, Bruns JJ, Jr, et al. Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Ann Emerg Med. 2008;52:714–48. doi: 10.1016/j.annemergmed.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 44.Fesmire FM, Brown MD, Espinosa JA, et al. Critical issues in the evaluation and management of adult patients presenting to the emergency department with suspected pulmonary embolism. Ann Emerg Med. 2011;57:628–52. e75. doi: 10.1016/j.annemergmed.2011.01.020. [DOI] [PubMed] [Google Scholar]
- 45.Howell JM, Eddy OL, Lukens TW, et al. Clinical policy: critical issues in the evaluation and management of emergency department patients with suspected appendicitis. Ann Emerg Med. 2010;55:71–116. doi: 10.1016/j.annemergmed.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 46.Hosmer JD, Lemeshow S, Sturdivant RX. Applied Logistic Regression Chapter 4: Model-Building Strategies and Methods for Logistic Regression. New York: John Wiley & Sons, Inc; 2013. pp. 89–151. [Google Scholar]
- 47.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 48.Breiman L. Random forests. Mach Learn. 2001;45:5–32. [Google Scholar]
- 49.Lee BK, Lessler J, Stuart EA. Improving propensity score weighting using machine learning. Stat Med. 2010;29:337–46. doi: 10.1002/sim.3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wong HJ, Sistrom CL, Benzer TI, et al. Use of imaging in the emergency department: physicians have limited effect on variation. Radiology. 2013;268:779–89. doi: 10.1148/radiol.13130972. [DOI] [PubMed] [Google Scholar]
- 51.Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63:e76–84. doi: 10.3399/bjgp13X660814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gleichgerrcht E, Decety J. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS One. 2013;8:e61526. doi: 10.1371/journal.pone.0061526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Allison JJ, Kiefe CI, Cook EF, Gerrity MS, Orav EJ, Centor R. The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Mak. 1998;18:320–9. doi: 10.1177/0272989X9801800310. [DOI] [PubMed] [Google Scholar]
- 54.Moorhead JC, Gallery ME, Hirshkorn C, et al. A study of the workforce in emergency medicine: 1999. Ann Emerg Med. 2002;40:3–15. doi: 10.1067/mem.2002.124754. [DOI] [PubMed] [Google Scholar]
- 55.Kanzaria HK, Brook RH, Probst MA, Harris D, Berry SH, Hoffman JR. Emergency physician perceptions of shared decision-making. Acad Emerg Med. 2015;22:399–405. doi: 10.1111/acem.12627. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Variables included in random forest model for propensity scores.
Linear regression to predict JSE by physician demographics and the three other psychometric scales.