Abstract
Study objective
Approximately 1 in 3 computed tomography (CT) scans performed for head injury may be avoidable. We evaluate the association of implementation of the Canadian CT Head Rule on head CT imaging in community emergency departments (EDs).
Methods
We conducted an interrupted time-series analysis of encounters from January 2014 to December 2015 in 13 Southern California EDs. Adult health plan members with a trauma diagnosis and Glasgow Coma Scale score at ED triage were included. A multicomponent intervention included clinical leadership endorsement, physician education, and integrated clinical decision support. The primary outcome was the proportion of patients receiving a head CT. The unit of analysis was ED encounter, and we compared CT use pre- and postintervention with generalized estimating equations segmented logistic regression, with physician as a clustering variable. Secondary analysis described the yield of identified head injuries pre- and postintervention.
Results
Included were 44,947 encounters (28,751 preintervention and 16,196 postintervention), resulting in 14,633 (32.6%) head CTs (9,758 preintervention and 4,875 postintervention), with an absolute 5.3% (95% confidence interval [CI] 2.5% to 8.1%) reduction in CT use postintervention. Adjusted pre-post comparison showed a trend in decreasing odds of imaging (odds ratio 0.98; 95% CI 0.96 to 0.99). All but one ED reduced CTs postintervention (0.3% to 8.7%, one ED 0.3% increase), but no interaction between the intervention and study site over time existed (P=.34). After the intervention, diagnostic yield of CT-identified intracranial injuries increased by 2.3% (95% CI 1.5% to 3.1%).
Conclusion
A multicomponent implementation of the Canadian CT Head Rule was associated with a modest reduction in CT use and an increased diagnostic yield of head CTs for adult trauma encounters in community EDs.
INTRODUCTION
Background
Stewardship of computed tomography (CT) imaging has been targeted as a key opportunity to improve the value of emergency care.1,2 Better imaging stewardship has the potential to avoid unnecessary radiation exposure, reduce costs, and eliminate the harms of overdiagnosis of “incidentalomas.”3,4 Reducing avoidable imaging may also decrease the length of emergency department (ED) stays and focus limited time and resources on patients more likely to benefit from ED care. There are multiple clinical decision rules,5 and their use during the evaluation of patients with head trauma is a recommended clinical strategy6 by both the American College of Emergency Physicians and the Choosing Wisely campaign.7
Importance
Despite multiple validated decision rules for evaluation of head trauma and more than a decade of research demonstrating their validity and generalizability,5 implementation of these rules in US clinical settings has been limited.8,9 Among studies reporting use of clinical decision rules, including the Canadian CT Head Rule, findings have been mixed. Some studies show no change, whereas others show increased imaging use10 without eliminating unwarranted imaging or increasing diagnostic yield5,11,12 despite expectations that Canadian CT Head Rule adherence will substantially decrease CT use.8,9,11
Goals of This Investigation
Previously, we reported that approximately one third of head CT imaging studies among adult trauma encounters would be avoided in our health system if the Canadian CT Head Rule were applied during clinical decisionmaking.9 The purpose of this study was to evaluate the association of implementing the Canadian CT Head Rule on rates of head CT use among adult ED trauma patients. Our secondary objective was to examine the association of clinical decision rule implementation with diagnostic yield, or the proportion of CT studies that identified radiographically significant brain injuries, given our goal to increase imaging appropriateness as opposed to solely reducing use.
MATERIALS AND METHODS
Study Design and Setting
We conducted a prospective, observational, interrupted time-series study to evaluate adult trauma encounters from January 2014 to December 2015 in 13 community EDs within an integrated health care delivery system, Kaiser Permanente Southern California, which provides health care for more than 4 million members and has an annual volume of ED patient visits at study sites ranging from 25,000 to 90,000, totaling approximately 900,000 visits per year. Of these ED visits, approximately 80% are by health plan members. None of the EDs had a trauma level designation during the study period.
We tested a multimodal intervention to implement the Canadian CT Head Rule into routine practice at 13 EDs. Components of the intervention included clinical leadership endorsement of the Canadian CT Head Rule, physician education, and clinical decision support. First, all clinical leaders of the participating EDs agreed to adopt the Canadian CT Head Rule as the recommended decision rule. Second, an electronic learning module was developed to educate physicians in regard to evaluation of traumatic head injury with the Canadian CT Head Rule, and to introduce the clinical decision support tool embedded into the electronic health record. Third, clinical decision support was triggered when the physician ordered a CT if information in the electronic health record indicated the scan was likely avoidable according to the Canadian CT Head Rule. During the study period, no other competing interventions were under way to reduce head CT imaging for trauma patients.
Selection of Participants
We included all adult ED trauma encounters with a Glasgow Coma Scale (GCS) score documented during routine ED triage. Trauma encounters were defined by International Classification of Diseases, Ninth Revision (ICD-9) or ICD-10 codes as defined by the Healthcare Cost and Utilization Project (Appendix E1, available online at http://www.annemergmed.com).13 We excluded ED encounters for individuals who were not members of a Kaiser Permanente Southern California health plan (≈20%) to ensure more accurate and complete data capture on patient characteristics such as chronic conditions, demographics, anticoagulant medications, and 30-day outcomes. We also excluded encounters with patients younger than 16 years to be consistent with the original Canadian CT Head Rule inclusion and exclusion criteria12 and our electronic learning module recommendations. These ED trauma encounters included all attending physicians regardless of specialty and excluded only encounters with providers who were residents, nonphysicians, or out-of-network physicians from our analysis.
Interventions
A research team member reviewed the published literature with clinical chiefs at the participating EDs. Clinical leaders were asked to promote the Canadian CT Head Rule as the standard of care expected in the evaluation of adults with minor head injury. These discussions began in the latter half of 2014, but the formal adoption of the Canadian CT Head Rule occurred in January 2015. The Canadian CT Head Rule was adopted and published on an internal physician Web portal for reference.
With an understanding that the implementation and regular use of decision rules generally require more than a clinical guideline or recommendation14 to succeed, the second step of our intervention was to create and disseminate physician education. A member of the research team and one of the ED clinical leaders developed a brief electronic learning module (approximately 15 minutes) that provided continuing medical education credit. The electronic learning module was made available on the internal physician Web portal and on a free video-hosting Web site, YouTube (https://youtu.be/vLIHg3y9jtw). The video was disseminated by e-mail to all emergency physicians and promoted by the clinical leaders during departmental meetings. The electronic learning module was launched immediately before the activation of clinical decision support in May 2015 and was continuously available throughout the study period.
Clinical decision support was triggered when the following 2 criteria were met: a chief complaint of trauma was listed at triage, and an order for head CT was placed. The clinical decision support was suppressed for any of the following contraindications: younger than 16 years or aged 65 years or older, any current use of anticoagulant (warfarin, heparin, clopidogrel, dabigatran, rivaroxaban, or apixaban), GCS score less than 15, or documented vomiting. The clinical decision support outputs a message at CT ordering that CT was “not recommended” unless one of the high-risk Canadian CT Head Rule criteria was met or the patient had a coagulation disorder. The clinical decision support allowed physicians to indicate, by selecting a radio button, whether one of the recommended criteria was met for the CT. Details of the clinical decision support are described in Appendix E2, available online at http://www.annemergmed.com.
Methods of Measurement
Using existing clinical and administrative data, including out-of-network claims that enable capture of any adverse patient outcomes among those treated out of network, we obtained information on several variables at both patient and physician levels. Patient variables included age, race, sex, GCS score, chronic conditions (represented by the Elixhauser Comorbidity Index),15,16 vomiting, anticoagulant use, alcohol intoxication (serum alcohol level >80 mg/dL), and arrival by emergency medical services (EMS). Patient information was collected by computerized query of structured data fields. Encounters for patients without documentation of chronic conditions, vomiting, anticoagulant use, elevated serum alcohol level, or EMS arrival were considered negative results. Physician characteristics included sex, years of clinical experience after residency (≤3, 4 to 10, 11 to 20, and >20 years), board-prepared or board-certified emergency physician status, and whether the physician completed the electronic learning module.
Outcome Measures
The primary outcome was head CT use, defined as the proportion of noncontrast head CT scans (Common Procedural Terminology code 70450) ordered among eligible adult trauma encounters. The secondary outcome was diagnostic yield, defined as the proportion of brain injury diagnoses (skull fractures or intracranial hemorrhages) among head CTs obtained for trauma (the numerator of the primary outcome). We characterized brain injuries diagnosed by CT as defined by a discharge diagnosis and included any encounters requiring a neurosurgical intervention within 30 days of the index ED visit. The diagnosis and procedure codes used have been validated in previous studies (Appendix E1, available online at http://www.annemergmed.com).17
Primary Data Analysis
We used generalized estimating equations segmented logistic regression to evaluate the odds of CT use before and after Canadian CT Head Rule implementation. The unit of analysis was ED encounter. Our model included terms for the baseline monthly trend (preintervention) of CT use and changes in level and trend of CT use before and after the intervention.18 The level change was defined as the difference in CT use between the last month of the preperiod and the first month postimplementation. The change in trend was assessed by comparing the pre- and postintervention monthly trends for CT use. Because our unit of analysis was ED encounter, we fit our model by using physician as a clustering variable to account for known correlation among encounters for the same physician.
All models were adjusted for the following patient clinical characteristics: age, race, sex, Elixhauser Comorbidity Index, vomiting, anticoagulant use, GCS score, alcohol intoxication, arrival by EMS, and medical center. We further adjusted for physician characteristics, including years of experience, ED residency, and completion of the electronic learning module. Using this data, we compared mean predicted and observed proportions of CTs ordered by month before and after the intervention.
We evaluated potential associations by facility, years of physician experience, and whether the patient met any of the Canadian CT Head Rule high-risk criteria to identify any heterogeneity in the immediate difference or change in CT use after the implementation. We also examined whether the intervention altered the ordering of appropriate CTs by modeling the odds of a likely appropriate CT (age ≥65 years, vomiting, GCS score <15, and serum alcohol level >80 mg/dL) among encounters during which a CT was ordered.
To assess changes in diagnostic yield, we compared the proportion of CTs with skull fractures, hemorrhagic intracranial injury, or receipt of a neurosurgical procedure before and after the intervention, using univariate χ2 tests.
Last, to assess individual physician CT ordering behavior before and after the intervention, we performed a subgroup analysis limited only to emergency medicine–trained providers with encounters in both the pre- and the postperiods. For each provider, we calculated the percentage of encounters with CTs ordered in their respective pre- and postintervention periods. To formally test for a change in this percentage, we fit a generalized estimating equations linear regression with percentage of encounters with CTs ordered as the outcome and intervention (post- versus preintervention) as the independent variable. This model included provider as a clustering variable and medical center, years of experience, and completion of the electronic learning module as covariates. We also graphically depicted this change by creating a parallel line plot ordered by preintervention CT percentage.19 This graph portrays the magnitude of the change and presents performance by physician overall and stratified by each study ED.
All analyses were conducted with SAS (version 9.3; SAS Institute, Inc., Cary, NC). All tests of statistical significance were 2-sided with α=.05. The study was approved by the Kaiser Permanente Southern California Institutional Review Board.
RESULTS
Characteristics of Study Subjects
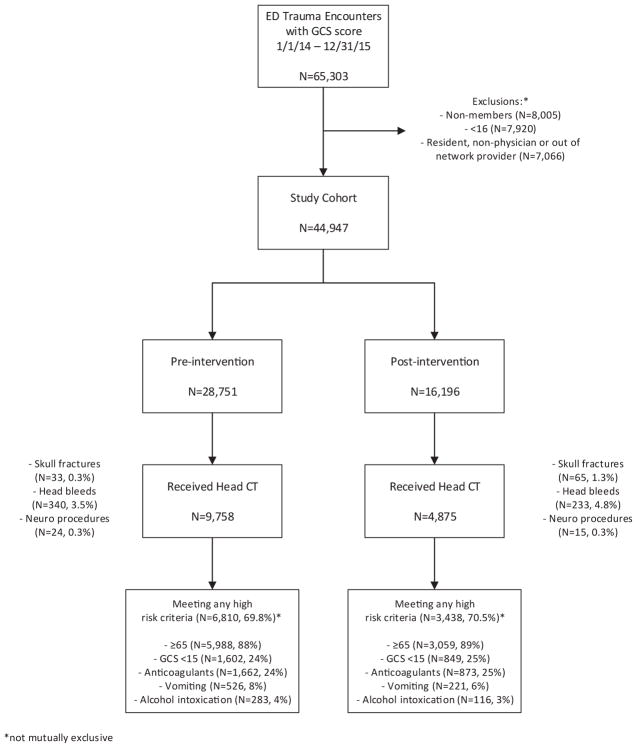
A total of 44,947 ED trauma encounters (28,751 pre- and 16,196 postintervention) including 41,108 patients (26,740 pre- and 15,394 postintervention) and 1,991 physicians (1,751 pre- and 1,576 postintervention) were included in the analytic cohort (Figure 1). Of these encounters, patients had a mean age of 59 years, were 53.6% women, and were racially diverse (Table 1). Providers evaluated a mean of 23 trauma encounters (median 9) in the study cohort (Table E1, available online at http://www.annemergmed.com, for provider characteristics). Overall 14,633 (32.6%) of all trauma encounters received a head CT.
Figure 1.
Sample of adult ED trauma encounters with a GCS score before and after implementation of provider education and computerized decision support intended to increase adherence to the Canadian CT Head Rule. The sample included encounters at 13 community EDs in Southern California.
Table 1.
Patient characteristics of 44,947 ED trauma encounters from January 1, 2014, to December 31, 2015, with cohorts stratified into pre- and postintervention groups.
| Patient Characteristics | Preintervention (January 1, 2014, to May 14, 2015) (n=28,751) | Postintervention (May 15, 2015, to December 31, 2015) (n=16,196) | Total (n=44,947) | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| No. | % | No. | % | No. | % | |
| Age, mean (SD) | 58.99 | (23.39) | 58.64 | (23.01) | 58.86 | (23.25) |
| Women | 15,275 | 53.13 | 8,832 | 54.53 | 24,107 | 53.63 |
| Ethnicity | ||||||
| Asian | 2,078 | 7.23 | 1,148 | 7.09 | 3,226 | 7.18 |
| Black | 3,099 | 10.78 | 1,810 | 11.18 | 4,909 | 10.92 |
| Hispanic | 9,389 | 32.66 | 5,402 | 33.35 | 14,791 | 32.91 |
| White | 13,728 | 47.75 | 7,561 | 46.68 | 21,289 | 47.36 |
| Other | 457 | 1.59 | 275 | 1.70 | 732 | 1.63 |
| Marital status | ||||||
| Partnered | 12,159 | 42.29 | 7,082 | 43.73 | 19,241 | 42.81 |
| Nonpartnered | 15,922 | 55.38 | 8,707 | 53.76 | 24,629 | 54.80 |
| Other/unknown | 670 | 2.33 | 407 | 2.51 | 1,077 | 2.40 |
| Poverty*† | 3,032 | 10.55 | 1,690 | 10.43 | 4,722 | 10.51 |
| Completed high school† | 23,735 | 82.55 | 13,054 | 80.60 | 36,789 | 81.85 |
| Elixhauser score, mean (SD) | 2.21 | (1.70) | 2.10 | (1.72) | 2.17 | −1.71 |
| Arrived by ambulance | 9,953 | 34.62 | 5,398 | 33.33 | 15,351 | 34.15 |
| Vomiting | 1,560 | 5.43 | 789 | 4.87 | 2,349 | 5.23 |
| Prescribed anticoagulants | 3,811 | 13.26 | 2,223 | 13.73 | 6,034 | 13.42 |
| GCS score <15 | 3,085 | 10.73 | 1,744 | 10.77 | 4,829 | 10.74 |
| Alcohol intoxication | 449 | 1.56 | 214 | 1.32 | 663 | 1.48 |
Percentages are column percentages.
Based on poverty income limits for a 4-person household ($34,575).
Based on population-based geocoding data at the census-track level, defined by patient address at the encounter.
Main Results
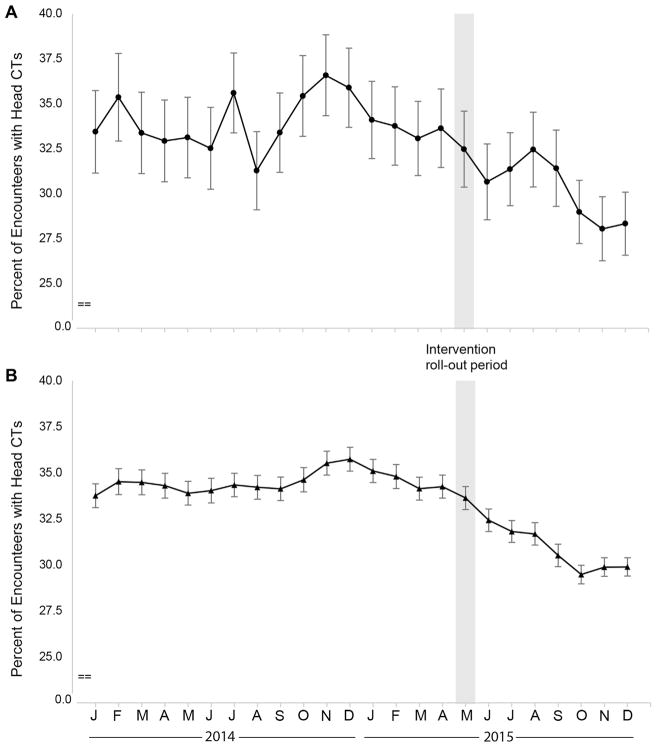
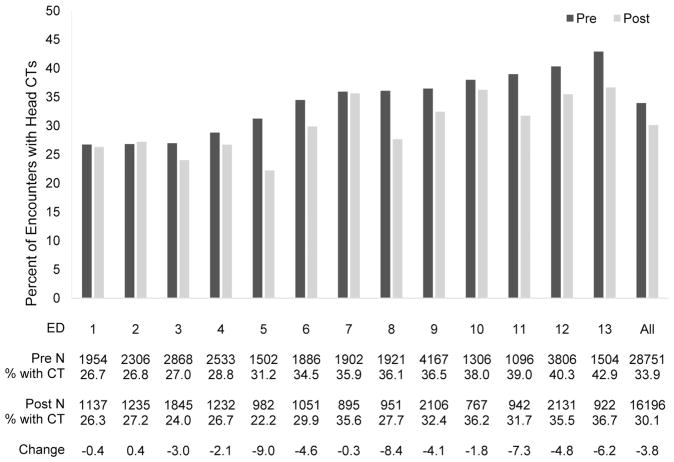
There was a 5.3% (95% confidence interval [CI] 2.5% to 8.1%) absolute and 15.8% relative reduction in the proportion of encounters resulting in CT use between the end of the preintervention period (March 2015) to the end of the postintervention follow-up period (December 2015) (Figure 2A). After the intervention, all but 1 of the 13 EDs reduced head CT use (Figure 3). One ED’s use increased 0.4% postintervention, but the absolute reduction in mean CT use pre- and postintervention for the other 12 EDs ranged from 0.3% to 8.7%, with an average decrease of 3.8% overall.
Figure 2.
An interrupted time series demonstrating the percentage of adult trauma patients receiving a head CT scan before (January 2014 to May 14, 2015) and after (May 15, 2015 to December 2015) implementation of the Canadian CT Head Rule. A, The percentage of CTs performed. B, The predicted results, adjusting for patient, physician, and facility characteristics.
Figure 3.
A pre-post comparison of head CT use for adult trauma encounters in 13 EDs before and after an intervention to implement the Canadian CT Head Rule.
In multivariate analysis, CT use did not change over time in the months before the implementation of the Canadian CT Head Rule (odds ratio [OR] 1.00; 95% CI 0.99 to 1.00). Subsequently, there was no immediate change in the level of CT use (OR 0.94; 95% CI 0.86 to 1.04) in the first month after the intervention, but there was a 2% reduction in the monthly trend (OR 0.98; 95% CI 0.96 to 0.99) for the 7 postintervention months compared with the preintervention period (Figure 2B).
Other independent patient predictors of CT use included older patient age (OR 1.02; 95% CI 1.02 to 1.02), higher Elixhauser Comorbidity Scores (OR 1.05; 95% CI 1.03 to 1.07), anticoagulant use (OR 1.19; 95% CI 1.11 to 1.26), GCS score less than 15 (OR 1.82; 95% CI 1.70 to 1.95), arrival by ambulance (OR 1.06; 95% CI 1.01 to 1.11), and alcohol intoxication (OR 3.64; 95% CI 3.05 to 4.35). The proportion of CTs ordered at the various facilities varied pre- and postintervention (P<.001) (Figure 3).
Physicians who completed an emergency medicine residency were more likely to order a CT (OR 1.63; 95% CI 1.55 to 1.71) compared with those who trained in non–emergency medicine residencies. Physicians who had less than 3 years of experience since residency ordered more CTs than those who had been practicing for 11 to 20 years (OR 0.86; 95% CI 0.80 to 0.92) or greater than 20 years (OR 0.79; 95% CI 0.73 to 0.85). There was no difference in CT ordering between physicians who completed the electronic learning module and those who did not (OR 1.06; 95% CI 0.94 to 1.19) (Table 2).
Table 2.
Output from a multivariate segmented logistic regression with generalized estimation equations methods* to predict the odds of receiving a head CT.
| Variable | OR | 95% CI | |
|---|---|---|---|
| Baseline monthly trend preimplementation | 1.00 | 0.99 | 1.00 |
| Change from the last preintervention month to the first postintervention month | 0.94 | 0.86 | 1.04 |
| Change in monthly trend postimplementation | 0.98 | 0.96 | 0.99 |
| Age | 1.02 | 1.02 | 1.02 |
| Women | 0.97 | 0.93 | 1.02 |
| Race (reference=white) | |||
| Asian | 1.28 | 1.17 | 1.39 |
| Black | 0.89 | 0.82 | 0.97 |
| Hispanic | 1.14 | 1.08 | 1.20 |
| Other | 1.01 | 0.83 | 1.23 |
| High school education | 1.00 | 0.92 | 1.10 |
| Poverty | 0.98 | 0.91 | 1.06 |
| Marital status (reference=nonpartnered) | |||
| Partnered | 0.93 | 0.89 | 0.97 |
| Other/unknown | 0.76 | 0.63 | 0.90 |
| Elixhauser | 1.05 | 1.03 | 1.07 |
| Vomiting | 0.99 | 0.89 | 1.09 |
| Anticoagulants | 1.19 | 1.11 | 1.26 |
| GCS score <15 | 1.82 | 1.70 | 1.95 |
| Medical center no. (reference=ED 13) | |||
| 1 | 0.50 | 0.44 | 0.57 |
| 2 | 0.53 | 0.47 | 0.60 |
| 3 | 0.55 | 0.49 | 0.61 |
| 4 | 0.52 | 0.46 | 0.59 |
| 5 | 0.58 | 0.51 | 0.66 |
| 6 | 0.73 | 0.65 | 0.83 |
| 7 | 0.69 | 0.61 | 0.78 |
| 8 | 0.72 | 0.63 | 0.81 |
| 9 | 0.82 | 0.74 | 0.91 |
| 10 | 0.76 | 0.67 | 0.87 |
| 11 | 0.76 | 0.67 | 0.87 |
| 12 | 0.77 | 0.70 | 0.86 |
| Emergency medicine residency | 1.63 | 1.55 | 1.71 |
| Years practicing (reference<3) | |||
| 3–10 | 0.96 | 0.90 | 1.02 |
| 11–20 | 0.86 | 0.80 | 0.92 |
| >20 | 0.79 | 0.73 | 0.85 |
| Physician completed education of the Canadian CT Head Rule | 1.06 | 0.94 | 1.19 |
| Arrived by ambulance | 1.06 | 1.01 | 1.11 |
| Alcohol intoxication | 3.64 | 3.05 | 4.35 |
Physician treated as a repeated measure to account for correlation between encounters from the same provider.
Despite varying proportions of CTs ordered at the participating study EDs, there was no statistically significant association with each facility over time (pinteraction=0.36), but there was a difference in the effect of the intervention between the last preintervention month and the first postmonth (pinteraction for immediate change=0.01). There was no association with years of physician experience (pinteraction for immediate change=0.51; pinteraction for change during the subsequent postintervention period=0.56). In addition, the intervention effect on CT use was similar for patients with and without high-risk criteria (pinteraction for immediate change=0.63; pinteraction for change during the subsequent postintervention period=0.70).
Furthermore, we found improvements in the ordering of rule-compliant CTs after the intervention. Although there was no immediate change in compliant CT ordering (OR 0.99; 95% CI 0.82 to 1.19), there was a 6% increase in the monthly trend (OR 1.07; 95% CI 1.02 to 1.10) in the postintervention period compared with the preintervention one.
Overall, the yield of head CTs improved 2.3% (95% CI 1.5% to 3.1%) postintervention (3.8% pre- and 6.1% postintervention); increases were observed in the proportion of encounters with an identified skull fracture (1.0% increase; 95% CI 0.65% to 1.34%) or hemorrhagic intracranial injury (1.3% increase; 95% CI 0.59% to 2.0%). Our study was not powered to detect statistical significance for these specific injuries. However, there was little difference in the receipt of a neurosurgical procedure (0.1% increase; 95% CI −0.1% to 0.2%) before and after the intervention. These patterns were consistent among head CTs that satisfied high-risk criteria. Additionally, the subgroup analysis of only emergency medicine–trained providers with pre- and postencounters showed that the percentage of head CTs ordered decreased by 2.7 percentage points (95% CI 0.6% to 4.8%) after the intervention. Graphs for the individual changes by provider are shown in Appendix E2, available online at http://www.annemergmed.com.
LIMITATIONS
Our study has several limitations to help interpret our results within the confines of our study design. First, we included all trauma encounters and were unable to restrict the denominator to head trauma visits only. This may have biased our results toward the null by inflating the denominator with trauma encounters not related to head injury; thus, our estimates are likely to be conservative. Another limitation is that the actual implementation of the Canadian CT Head Rule across the various medical centers may not have been uniform because we used a pragmatic design that allowed the actual implementation of this clinical decision support in an integrated health system. This is likely to explain some variation in CT use between sites and is also likely to bias our results toward the null because EDs with limited implementation were included in the analysis. We also cannot make any inferences about what made the clinical decision support successful because we do not know which component of the implementation was associated with successful reduction in CT imaging, although physician education with electronic learning did not appear to be associated with CT imaging and requires further investigation. Future work using qualitative methods and standardized implementation may help to untangle the complexity surrounding how to develop and implement a successful clinical decision support for reducing CT overuse and may yield a larger influence.
We acknowledge that the duration of the postintervention period was only 7 months. It is possible that we did not capture the full consequences of uptake of new behaviors during a longer period; therefore, our results may be biased toward the null. In contrast, it is possible that the association of the intervention will not be sustained over time.
Quasi-experiments have limitations in regard to the causal inference one may attribute to the intervention of interest. However, our study design attempted to mitigate this limitation through an interrupted time-series strategy with an extended preimplementation period. The interrupted time-series strategy to evaluate a health system intervention is a favored methodology in quasi-experimental studies and helps to disentangle secular trends from the association of the intervention of interest.18,20–22
DISCUSSION
Implementation of the Canadian CT Head Rule in community ED settings was associated with a reduction in head CT use during a 7-month period and an increase in the diagnostic yield of CT-identified injuries requiring neurosurgical intervention. We observed a 5% absolute reduction in head CT imaging for all trauma encounters after a multicomponent intervention to implement the Canadian CT Head Rule across 13 community EDs. The proportion of CTs ordered at each ED varied before and after the intervention, but the magnitude of the association did not vary by ED setting or by years of physician experience. Twelve of the 13 participating EDs showed a reduction in CT ordering after the intervention.
To our knowledge, this is the first study to evaluate the association of implementing the Canadian CT Head Rule (or any head trauma decision rule) in a community ED setting in the United States. A benefit of our integrated health care system’s robust data warehouse is that it allows the capture of detailed patient characteristics and longitudinal follow-up to enable robust risk adjustment and outcome ascertainment among a diverse population visiting EDs of various annual volumes. Our finding that all 12 of 13 participating EDs showed a decrease in CT use with an increased diagnostic yield in identified injuries is promising. Although our study does not evaluate whether the Canadian CT Head Rule was actually applied during each encounter, our analysis reflects a pragmatic examination of a simple intervention that many EDs should be able to replicate and spread. Quasi-experimental designs have limitations, and our study is a reflection of a community ED setting in an integrated health system. This study thus may or may not be more applicable to other US EDs than one performed in an academic setting.
Our results validate our previous expectations that adherence to the Canadian CT Head Rule using clinical decision support would be associated with decreased CT use.11 However, our previous estimates and current results would suggest there is still an opportunity for further improvement and fidelity in applying the Canadian CT Head Rule for adults with head trauma. It is also promising that the modest reductions in CT use observed here in community settings were similar to those observed at academic-based Level I trauma centers.8,9,11,23,24 However, our findings differ from those of a similar study of Canadian CT Head Rule implementation in Canada, which found a negative or null effect on CT use.10 This may be a result of differences in the patient populations, medical cultures, physician training, or other variation between US and Canadian health care systems. Our intervention also used clinical decision support, which was not a part of the Canadian intervention. This component of our intervention may play a key role in sustained success and help close the evidence-to-practice gap.25 Clinical decision support was associated with decreased CT use and increased the yield of identified injuries, which supports the integration of clinical decision support for head trauma into routine practice in modern US EDs.
Despite our attempt to promote use of the Canadian CT Head Rule through continuing medical education, the importance of education for decision support is yet ill defined. Using clinical decision support may be critical to the success in reducing CT use, but the more nebulous effect of leadership, education, and other cultural factors requires further investigation. Influencing physicians to apply decision rules is complex, and, although our results are favorable, we hypothesize there is still ample room for improvement in the application of the Canadian CT Head Rule in our study EDs. Including other components of implementation strategies, such as audit and feedback,26,27 may result in even greater reductions in avoidable CT use.
In summary, a multicomponent intervention (including clinical leadership endorsement, education, and electronic health record decision support) to implement the Canadian CT Head Rule for adult trauma encounters in community EDs was associated with a decrease in CT use and an increased diagnostic yield. Clinical decision support may be a critical factor in successful implementation of a clinical decision rule. Our work demonstrates the feasibility and positive influence of implementation of a clinical decision rule on head CT use for trauma encounters.
Supplementary Material
Editor’s Capsule Summary.
What is already known on this topic
Implementation of validated clinical decision rules such as the Canadian CT Head Rule to address the potential overuse of imaging in head injury has been associated with inconsistent changes in emergency department (ED) practice.
What question this study addressed
Does a multimodal intervention to increase Canadian CT Head Rule adherence affect computed tomography (CT) use in adults with minor head injury?
What this study adds to our knowledge
In nearly 45,000 encounters at 13 community EDs within an integrated health system, intervention was associated with a 5.3% absolute reduction in head CT use.
How this is relevant to clinical practice
This intervention may be associated with a similar modest decrease in head CT if implemented in other settings.
Acknowledgments
The authors acknowledge Ellen J. Rippberger, MPH, and Visanee V. Musigdilok, MPH, for their administrative assistance and for their review and edits of the article.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist. Internal funding from the Kaiser Permanente Southern California Care Improvement Research Team supported this project. Dr. Melnick is supported, in part, by grant K08HS021271 from the Agency for Healthcare Research and Quality.
Footnotes
Author contributions: All authors interpreted the data and edited and approved the final article. ALS and TT drafted the article. ALS and BZH conceived the study. ALS and MHK designed the intervention. ALS, BZH, TT, ES, AKV, and MKG analyzed the data. BZH designed the study and performed data collection. ES designed the analysis methods. ALS takes responsibility for the paper as a whole.
All authors attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
References
- 1.Sierzenski PR, Linton OW, Amis ES, Jr, et al. Applications of justification and optimization in medical imaging: examples of clinical guidance for computed tomography use in emergency medicine. Ann Emerg Med. 2014;63:25–32. doi: 10.1016/j.annemergmed.2013.08.027. [DOI] [PubMed] [Google Scholar]
- 2.Sharp AL, Cobb EM, Dresden SM, et al. Understanding the value of emergency care: a framework incorporating stakeholder perspectives. J Emerg Med. 2014;47:333–342. doi: 10.1016/j.jemermed.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 3.Cawood TJ, Hunt PJ, O’Shea D, et al. Recommended evaluation of adrenal incidentalomas is costly, has high false-positive rates and confers a risk of fatal cancer that is similar to the risk of the adrenal lesion becoming malignant: time for a rethink? Eur J Endocrinol. 2009;161:513–527. doi: 10.1530/EJE-09-0234. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell J, Parangi S. The thyroid incidentaloma: an increasingly frequent consequence of radiologic imaging. Semin Ultrasound CT MR. 2005;26:37–46. doi: 10.1053/j.sult.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Harnan SE, Pickering A, Pandor A, et al. Clinical decision rules for adults with minor head injury: a systematic review. J Trauma. 2011;71:245–251. doi: 10.1097/TA.0b013e31820d090f. [DOI] [PubMed] [Google Scholar]
- 6.Rivara FP, Kuppermann N, Ellenbogen RG. Use of clinical prediction rules for guiding use of computed tomography in adults with head trauma. JAMA. 2015;314:2629–2631. doi: 10.1001/jama.2015.17298. [DOI] [PubMed] [Google Scholar]
- 7.ABIM Foundation. [Accessed June 29, 2017];The American College of Emergency Physicians: Choosing Wisely: ten things physicians and patient’s should question. 2014 Available at: http://www.choosingwisely.org/doctor-patient-lists/american-college-of-emergency-physicians/
- 8.Melnick ER, Szlezak CM, Bentley SK, et al. CT overuse for mild traumatic brain injury. Jt Comm J Qual Patient Saf. 2012;38:483–489. doi: 10.1016/s1553-7250(12)38064-1. [DOI] [PubMed] [Google Scholar]
- 9.Sharp AL, Nagaraj G, Rippberger EJ, et al. Computed tomography use for adults with head injury: describing likely avoidable ED imaging based on the Canadian CT Head Rule. Acad Emerg Med. 2017;24:22–30. doi: 10.1111/acem.13061. [DOI] [PubMed] [Google Scholar]
- 10.Stiell IG, Clement CM, Grimshaw JM, et al. A prospective cluster-randomized trial to implement the Canadian CT Head Rule in emergency departments. CMAJ. 2010;182:1527–1532. doi: 10.1503/cmaj.091974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Korley FK, Morton MJ, Hill PM, et al. Agreement between routine emergency department care and clinical decision support recommended care in patients evaluated for mild traumatic brain injury. Acad Emerg Med. 2013;20:463–469. doi: 10.1111/acem.12136. [DOI] [PubMed] [Google Scholar]
- 12.Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357:1391–1396. doi: 10.1016/s0140-6736(00)04561-x. [DOI] [PubMed] [Google Scholar]
- 13.Barrett MSC. Methods Series Report: External Cause of Injury Code (E Code) Evaluation Report (Updated With 2012 HCUP Data) Rockville, MD: Healthcare Cost & Utilization Project (HCUP); 2015. [Google Scholar]
- 14.Rosenberg A, Agiro A, Gottlieb M, et al. Early trends among seven recommendations from the Choosing Wisely campaign. JAMA Intern Med. 2015;175:1913–1920. doi: 10.1001/jamainternmed.2015.5441. [DOI] [PubMed] [Google Scholar]
- 15.Li B, Evans D, Faris P, et al. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD-9 and ICD-10 administrative databases. BMC Health Serv Res. 2008;8:12. doi: 10.1186/1472-6963-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Austin SR, Wong YN, Uzzo RG, et al. Why summary comorbidity measures such as the Charlson comorbidity index and Elixhauser score work. Med Care. 2015;53:e65–e72. doi: 10.1097/MLR.0b013e318297429c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carroll CP, Cochran JA, Guse CE, et al. Are we underestimating the burden of traumatic brain injury? surveillance of severe traumatic brain injury using Centers for Disease Control International Classification of Disease, Ninth Revision, Clinical Modification, traumatic brain injury codes. Neurosurgery. 2012;71:1064–1070. doi: 10.1227/NEU.0b013e31826f7c16. discussion 1070. [DOI] [PubMed] [Google Scholar]
- 18.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27:299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 19.Schriger DL, Cooper RJ. Achieving graphical excellence: suggestions and methods for creating high-quality visual displays of experimental data. Ann Emerg Med. 2001;37:75–87. doi: 10.1067/mem.2001.111570. [DOI] [PubMed] [Google Scholar]
- 20.Fretheim A, Zhang F, Ross-Degnan D, et al. A reanalysis of cluster randomized trials showed interrupted time-series studies were valuable in health system evaluation. J Clin Epidemiol. 2015;68:324–333. doi: 10.1016/j.jclinepi.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Taljaard M, McKenzie JE, Ramsay CR, et al. The use of segmented regression in analysing interrupted time series studies: an example in pre-hospital ambulance care. Implement Sci. 2014;9:77. doi: 10.1186/1748-5908-9-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pape UJ, Millett C, Lee JT, et al. Disentangling secular trends and policy impacts in health studies: use of interrupted time series analysis. J R Soc Med. 2013;106:124–129. doi: 10.1258/jrsm.2012.110319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ip IK, Raja AS, Gupta A, et al. Impact of clinical decision support on head computed tomography use in patients with mild traumatic brain injury in the ED. Am J Emerg Med. 2015;33:320–325. doi: 10.1016/j.ajem.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Parma C, Carney D, Grim R, et al. Unnecessary head computed tomography scans: a level 1 trauma teaching experience. Am Surg. 2014;80:664–668. doi: 10.1177/000313481408000720. [DOI] [PubMed] [Google Scholar]
- 25.Lang ES, Wyer PC, Haynes RB. Knowledge translation: closing the evidence-to-practice gap. Ann Emerg Med. 2007;49:355–363. doi: 10.1016/j.annemergmed.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 26.Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(6):CD000259. doi: 10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Le Grand Rogers R, Narvaez Y, Venkatesh AK, et al. Improving emergency physician performance using audit and feedback: a systematic review. Am J Emerg Med. 2015;33:1505–1514. doi: 10.1016/j.ajem.2015.07.039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.