Abstract
Purpose
Congenital adrenal hyperplasia (CAH) requires parents to inject their child with hydro-cortisone intramuscularly during times of illness and adrenal crisis. The purpose of this study was to describe circumstances surrounding adrenal crisis events in children with CAH; to explore parents’ perceptions of the consequences of having a child with a life-threatening condition; and to examine a relationship between parents’ perceived management ability and the impact CAH has on the family.
Methods
In Phase 1 of this mixed-methods, cross-sectional study, 77 parents were asked to complete questionnaires comprising measures of family life in the context of childhood illness. Descriptive statistics were computed with four separate analyses using linear mixed models allowing for correlation between responses from parents of the same family and for the variance to be different for fathers and mothers. The following relationships were examined: (1) parental management ability and type of provider instruction on how to manage adrenal crises; (2) parental management ability and child age; (3) the perceived impact of the condition on the family and management ability; and (4) the age of the child and number of adrenal crisis events. In Phase 2, 16 semi-structured interviews were conducted to elicit detailed descriptions of parents’ experiences in managing crises.
Results
There was a significant, positive relationship between detailed provider instruction to parents on adrenal crisis management and perceived management ability (p = .02), additionally the stronger the perceived management ability, the less impact CAH had on the family (p < .001). From birth to age 5, parents reported more frequent crisis events and less perceived ability to manage the condition when compared with parents of older children (p = .009). The threat of an adrenal crisis event is a pervasive concern for parents, especially when they are not being properly prepared by providers.
Practice Implications
Provider support is needed for these parents throughout childhood, but especially in the first 5 years of life when parents are adjusting to having a child with a life-threatening condition. Identifying gaps in parent education by healthcare providers is necessary to promote positive family outcomes.
Keywords: adrenal crisis, endocrine, congenital adrenal hyperplasia, parental management, mixed-methods
1 INTRODUCTION
Chronic conditions in children dramatically change the meaning of parenting and have varied impacts on family life (Knafl et al., 2013). Classic congenital adrenal hyperplasia (CAH), a rare, genetic condition resulting in lifelong adrenal insufficiency that affects approximately 1 in 15,000 live births annually (Speiser et al., 2010), is one such chronic condition. Individuals with CAH are at risk for life-threatening adrenal crisis resulting from deficient cortisol. Symptoms include vomiting, hypotension, hypoglycemia, pallor, tachycardia, confusion, and loss of consciousness. Management of CAH requires parents to administer oral steroids, typically hydrocortisone, up to three times daily, supplementing maintenance doses with oral “stress dosing” during times of illness and an emergency intramuscular (IM) injection of hydrocortisone when a child is unable to tolerate oral medications and/or if signs of adrenal crisis are present (Merke & Bornstein, 2005; Speiser et al., 2010; Witchel & Azziz, 2011). The need for stress dosing, either orally or by injection, related to simple viral and bacterial childhood illnesses and adrenal crisis events are frequent and unpredictable, often requiring parents to make complex treatment decisions (Merke & Bornstein, 2005). A 2014 qualitative study of parents having a child with CAH found that families have multiple challenges related to their child’s CAH diagnosis including communication struggles with healthcare providers, especially surrounding the time of diagnosis and subsequent treatment guidelines. Another concern parents expressed was the lack of social support, which left them feeling overwhelmed and isolated, and fearing their understanding of how to manage CAH was insufficient (Boyse, Gardner, Marvicsin, & Sandberg, 2014). The continuous threat of illness or adrenal crisis, and the knowledge that improperly responding to such a threat could result in a fatal outcome created an environment of uncertainty, stress, and potential dysfunction within the family (Fleming, Rapp, & Sloane, 2011).
Despite the importance of being able to effectively respond to an adrenal crisis episode, a 2011 study showed that only half of the 60 parents of children with CAH surveyed reported ever having received a demonstration from a healthcare professional on how to administer the emergency injection of hydrocortisone (Fleming et al., 2011). Additionally, the type of emergency education given to parents by healthcare providers varied considerably, with some parents receiving no formal instruction from providers, while others receiving both oral and written instruction as well as an actual injection demonstration from a provider on when and how and to correctly administer the injection (Fleming et al., 2011).
In addition to being able to respond effectively to the life-threatening aspect of CAH, parents must also handle day-to-day condition management. If a child is prescribed too much hydrocortisone, side effects can include growth suppression, obesity, and other cushingoid features. If the dose of hydrocortisone is not sufficient, children with CAH are at a high risk for precocious puberty, which can also lead to stunted growth and adrenal crisis. Daily management typically includes replacing deficient levels of cortisol and/or aldosterone while attempting to minimize androgen excess, prevent virilization, optimize linear growth (which is often compromised), and protect future fertility (Merke & Bornstein, 2005). Determining the proper dosage of steroids is typically achieved by obtaining routine laboratory work and measuring the height, weight and bone age, typically every 3–6 months, in a growing child (Merke & Bornstein, 2005).
The aims of this study were to describe circumstances surrounding adrenal crisis events in children with CAH (i.e., causes and frequency, parental preparation, preparation of others caring for the child); to explore parents’ perceptions of the consequences for themselves and their family of having a child with a life-threatening condition; and to examine a relationship between parents’ management ability and the impact CAH has on the family.
2 METHODS
2.1 Guiding framework
This study was guided by the Family Management Style Framework (FMSF), which provides a structure for understanding family responses to a child’s chronic condition (Knafl, Deatrick, & Havill, 2012) (Figure 1). The FMSF is grounded in the originators’ research and syntheses of studies of family life in the context of childhood chronic conditions. It has been used in studies with families exploring the overall response to the child’s condition as well as studies of selected aspects of their response (e.g., information management) (Knafl et al., 2012). According to the FMSF, individuals in the family contribute to developing a family management style or pattern of response that can influence both individual and family outcomes (Knafl et al., 2012, 2013). The framework is comprised of four components: definition of the situation (the ways in which the child and child’s condition is viewed by the parent(s), management mindset, and parental mutuality), management behaviors (parenting goals, strategies, and behaviors linked to caring for a chronically ill child), and perceived consequences (actual or expected family, child, and illness outcomes that shape management behaviors). Additionally, the framework asserts that the contextual influences on the family (interchanges with healthcare providers and schools, social network, and access to resources) can either support or impede a family’s effort to manage the condition (Knafl et al., 2012, 2013).
FIGURE 1.
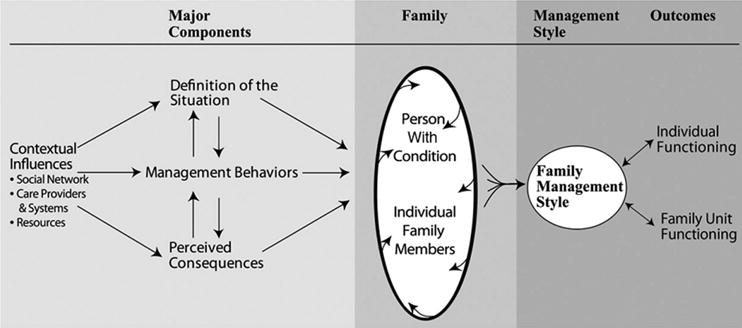
Family management style framework
2.2 Design
This descriptive, mixed-methods study was conducted in two phases. In Phase 1, parents were asked to complete online questionnaires about selected aspects of their experiences of family life in the context of having a child with CAH. In Phase 2, semi-structured interviews were conducted to elicit more detailed descriptions of parents’ experiences in managing CAH-related crises and their perceptions of how the consequences of living with the threat of crisis influenced their child’s and their family’s life. The purposive intent of the Phase 2 interview sample was to achieve maximum variation in terms of both the demographic profile of families (e.g., parents of boys and girls, families having children of varying ages, families from different geographic areas of the USA, etc.) and their experiences managing adrenal crisis events. Scores on the structured measures in Phase 1 were also examined so that parents reporting both high and low impact of the condition on their family as well as management ability were included in Phase 2. This design allowed for comparison and corroboration of the quantitative results with qualitative findings (Creswell & Clark, 2010) and provided a rich, comprehensive description of parents’ crisis management strategies and their perceptions of the adrenal crisis education they had received from healthcare providers.
2.3 Participants
Parents were recruited through CARES Foundation (CARES), a nonprofit organization, based in New Jersey, which provides support to families having a child with CAH (CARES Foundation, 2014). To be included in the study, the parent needed to be over the age of 18, English speaking, and have a child between the ages of birth and 18 years diagnosed with classic, salt-wasting CAH and free from any other complex health conditions. Furthermore, parents needed to have access to a telephone, computer, and email account. A parent was defined as a person who lived in the same household with the child and had the responsibility of caring for the child and managing the child’s CAH, even if the parent was not the biological mother or father. Recruitment for the study consisted of an “Invitation to Participate” letter that CARES emailed to its members who had previously expressed an interest in participating in the research. In addition, CARES provided a brief description of this research study within the research section of their website. Parents who contacted the authors were emailed the measures and consented to participate online.
2.4 Measures
Data were collected through a demographic/family information questionnaire, the Pediatric Quality of Life-Family Impact Module (PedsQL-FIM), two scales from the Family Management Measure (FaMM)-View of Condition Impact and Management Ability, and an individual semi-structured interview using an interview guide (with each parent participating separately). The demographic/family information questionnaire, developed by the authors, included information about the family, the child’s health status, and the frequency of adrenal crisis experience(s). The demographic/family information questionnaire was also used to gather data about the provider the child saw to manage CAH as well as how and when, if ever, the parent was instructed about management of an adrenal crisis. The PedsQL-FIM and the FaMM-View of Condition Impact and Management Ability scales provided additional information on the effects of living with a child who has a life-threatening illness. Varni’s 36-item Peds QL-FIM is designed to measure parent self-reported perceptions of the impact of the condition on their physical, emotional, social, and cognitive functioning; communication; and worry. The measure also examines parent-reported family daily activities and family relationships (Varni, Sherman, Burwinkle, Dickinson, & Dixon, 2004). The 10-item FaMM-View of Condition Impact scale is designed to address parents’ perceptions of the seriousness of the condition and its implications for their child’s and their family’s future (Knafl et al., 2012). The 12-item FaMM-Management Ability scale addresses parents’ perceptions of the overall manageability of the child’s condition, including knowing what needs to be done to take care of the condition and their ability to competently carry out the management of their child’s condition (Knafl et al., 2012). All three measures have well-established validity and reliability. Use of these measures contributed to a more complete understanding of parents’ perceptions of the impact of their child’s CAH on themselves and family life.
Phase 2 of the study entailed qualitative telephone interviews with the subsample of parents who participated in Phase 1. Topics for the interview guide focused on parents’ description of their crises management experiences and their perceived competence and ability to manage the condition based on the three components of the FMSF.
2.5 Data collection
In Phase 1, following the author’s university’s IRB approval, parents of children with CAH were recruited via an email from the CARES Foundation and interested participants then contacted the author via telephone, email, or text message. After consent was obtained, the demographic/family information questionnaire and the three measures were made available to the participants in one document via an online survey using Qualtrics software. Each person participating in the survey (including parents in the same family) received a secure, individualized electronic link. The author then contacted the selected parent(s) who were willing to be interviewed. When both parents were participating, they were asked to complete the questionnaires separately so that one parent did not influence the other’s responses. Each parent in Phase 2 was interviewed separately to provide a full accounting of their individual experiences. Data collection continued during Phase 2 until common themes repeatedly emerged to the point of saturation (Bowen, 2008).
2.6 Data analysis
Using the family information questionnaire, descriptive statistics were computed for both parents and children including variables such as age, gender, household income, as well as examining the timing of when, or if, providers gave parents the prescription for injectable hydrocortisone. Then, four separate analyses were conducted using F-tests generated by linear mixed models allowing for correlation between responses from parents of the same family and for the variance to be different for fathers and mothers (compound symmetry heterogeneous covariance). The first relationship examined was between parental management ability, using the FaMM-Management Ability Scale, and whether providers had demonstrated to parents how to give the injection based on the family information questionnaire. The second analysis investigated the relationship between parental management ability and child age. Next, the relationship between the impact the condition has on the family (FaMM-View of Condition Impact and PedsQL-Family Impact Module) and management ability (FaMM-Management Ability Scale) were examined.
Finally, the relationship between age of the child and the number of adrenal crisis events was examined. In the family information questionnaire, parents were asked to categorize the number of adrenal crisis events their child had experienced to date (no crisis events; 1–2 crisis events; 3–5 crisis events; or 5 or greater crisis events). The lowest number in each category was normalized (to obtain a minimum number of adrenal crisis events) with the current age of the child (to obtain a minimum number of adrenal crisis events per year) and modeled as a function of age less than or equal to 5 years or greater than 5 years. The age of 5 was chosen based on several factors including the child beginning school and being able to better articulate how they are feeling as well as parental responses when asked how their view of the condition has changed over the years in the Phase 2 interviews. Then, the relationship between the minimum number of adrenal crises per year and age of the child was modeled as possibly nonlinear using adaptive regression (Knafl & Ding, 2016).
A professional transcriptionist transcribed the audio recordings verbatim, and the transcriptions were checked against the tape for accuracy in an effort to gain a better understanding of the tone and emotion reflected in the parents’ responses. Following transcription, all interviews were coded using a combination of a start list of codes based on the FMSF and the online measures and codes inductively derived from interview data. Qualitative data analysis was supported using MAXQDA (Verbi Software, 2015), a software program that facilitates coding of qualitative data and retrieval of coded material. The analysis of interview data first focused on developing a thematic summary of each parent’s interview (Ayres, Kavanaugh, & Knafl, 2003; Sandelowski, 2011a). In order to balance the inherently reductionist nature of coding, a second analytic strategy entailed completion of narrative family case summaries of each interview. Case summaries are a useful strategy for grounding the analysis of individual codes in the context of the respondent’s overall experience (Sandelowski, 2011b). In families where both parents participated, the analysis addressed the extent to which parents had a shared or discrepant thematic profile to look for varying patterns of family management. Additionally, comparisons were made across all parents’ thematic summaries and across all families to provide a greater understanding of the nature and range of perceived consequences, for a variety of families, of having a child with CAH (Sandelowski, 2011a). Finally, quantitative scores from the measures were included in the summary matrices for further comparison within and across families based on all data sources. Using a within and across case analysis approach (Ayres et al., 2003; Sandelowski, 2011a) that included all data sources contributed to a thorough description of how participating parents perceived and managed their child’s CAH in the context of everyday family life.
3 PHASE 1 RESULTS
Seventy-seven parents participated in Phase 1 (60 mothers, 2 grandmothers, and 15 fathers). Of those parents, nine were dyads (eight mother/father, one grandmother/father) (Table 1). There was very little missing data; however, certain analyses were computed with varying data sets when this occurred. The mean parent age (n = 75) was 41.9 years for mothers and 40.7 years for fathers (two grandmothers participated as well, ages 75 and 44 years); the mean child age (n = 68) was 8.4 years. Forty-four parents reported having a girl with CAH (57%) and 33 parents (43%) a boy. The parents who participated in Phase 1 lived in 28 states within the USA as well as four parents from Ghana, Australia, UK, and Puerto Rico, which indicates that a large sample of healthcare providers were represented in terms of providers’ efforts to educate parents on CAH management. Of the 73 parents who shared household income information, about half (n = 39) had a yearly income less than $100,000 (US) per year.
TABLE 1.
Phase 1—parent and child participant characteristics
| Parent characteristics | |
| Parenting role | n (%) |
| Mother | 60 (78) |
| Father | 15 (19) |
| Grandmother | 2 (3) |
| Racial identification | n (%) |
| American Indian/Alaskan Native | 1 (1.3) |
| Asian | 2 (2.7) |
| Black | 1 (1.3) |
| White | 71 (94.7) |
| Ethnicity | n (%) |
| Hispanic | 4 (5.3) |
| Non-Hispanic | 72 (94.7) |
| Yearly family income | n (%) |
| <$50,000 | 10 (13.7) |
| $50,000–80,000 | 12 (16.4) |
| $80,000–100,000 | 15 (20.6) |
| $100,000–150,000 | 14 (19.2) |
| >$150,000 | 22 (30.1) |
| Age of mother | |
| Mean (SD) | 41.98 (7.4) |
| Range | 26–54 |
| Age of father | |
| Mean (SD) | 40.71 (4.9) |
| Range | 33–47 |
| Age of grandmother | |
| Mean (SD) | 59.5 (21.9) |
| Range | 44–75 |
| Child characteristics | |
| Racial identification | n (%) |
| American Indian/Alaskan Native | 1 (1.3) |
| Asian | 2 (2.7) |
| Black | 1 (1.3) |
| White | 71 (94.7) |
| Ethnicity | n (%) |
| Hispanic | 6 (7.9) |
| Non-Hispanic | 70 (92.1) |
| Wears medical alert tag | n (%) |
| Yes | 51 (66) |
| No | 26(34) |
| Gender of child | n (%) |
| Male | 33 (43) |
| Female | 44 (57) |
| Age of child | |
| Mean (SD) | 8.4 (5.3) |
| Range | 1 month-18 years |
Of the 68 parents who responded to a question inquiring when their child’s provider gave them a prescription for intramuscular hydrocortisone, 10 parents stated they received the prescription 1 month after diagnosis, 3 responded between 6 and 12 months, and 4 stated it took over 1 year to receive it, meaning that 25% of parents surveyed did not receive the prescription within 1 month of diagnosis.
The Cronbach’s alphas for the Quality of Life-Family Impact Model and the View of Condition Impact and Condition Management Ability scales from the Family Management Measure used in this study were .96, .73, and .81, respectively. How parents perceived providers’ instructions about how to give the injection (e.g., written guidelines, injection demonstration) varied; however, there was a significant relationship (p = .02) between parents having directly been shown by a provider how to correctly administer the injection and higher scores on the FaMM-Management Ability scale, indicating parents believed they were capable of managing the condition.
When examining adrenal crisis event occurrences in Phase 1, there was a significant, nonlinear relationship between the age of child and the average number of adrenal crisis events experienced each year, with the number of crises decreasing over time. Parents reported children having 0.77 adrenal crisis events per year (a minimum number of one adrenal crisis episode every 1.3 years) in the first 5 years of life; however, after the age of 5, parents reported 0.27 adrenal crisis events per year (a minimum of one adrenal crisis episode every 3.7 years) (Figure 2). Additionally, mean ability to manage the condition was significantly lower (40.9 vs. 44.1; p = .009) for parents of children 5 and under compared with parents of children over 5 years of age, indicating that parents feel better able to manage the condition as the child gets older.
FIGURE 2.
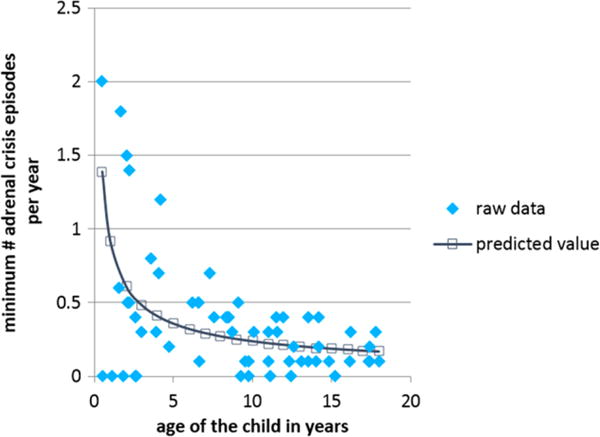
Phase 1—minimum number of adrenal crisis episodes and age of the child
Furthermore, when examining parental management ability and the impact the condition has on the family using both family impact measures, as management ability increased, there was a decrease in the perceived impact of CAH on the family (p < .001).
4 PHASE 2 RESULTS
In Phase 2, 16 parents selected from Phase 1 were interviewed, 7 mother/father dyads and 2 single mothers. Of the nine families, four had boys with CAH and five had girls with CAH. Ages of the children at the time of the interviews ranged from 2 to 15 years, which highlighted varied parent experiences such as school encounters and age-dependent child care needs. The parents interviewed were heterogeneous in nature when examining demographic variables such as family income, age of the child, and where in the USA they resided.
4.1 Definition of the situation
According to the FMSF, definition of the situation includes how parents view the condition and the child, their management mindset, and parental mutuality (Knafl et al., 2012). Parents stated certain aspects of their child’s CAH management were going very well such as administering daily medication, their child’s current height and weight, and their child’s performances in school. All felt that, overall, their child was thriving, happy, and well-adjusted. However, there were some clear distinctions made by parents between their family and others without a child with CAH. For example, the decision for one parent not to work outside the home because of the extra attention needed for the CAH child, not allowing grade school aged children to play at friends’ houses, and not allowing nonfamily members to babysit were linked to their child’s CAH and described as unique challenges faced by the family. When asked what was the most important information to relay to parents having a child just diagnosed with the condition, the majority of parents responded that being prepared to manage an adrenal crisis event was paramount.
So knowing that if you are going to be outdoors on hot summer days you need plenty of fluids and salt tablets and you always need to have your shot kit with you. You need to know if you’re going to be away from the home all day that you need to have all of your different medicines with you. You can’t get caught not prepared for the situation.
Parents in seven dyads described a strong sense of “being on the same page” regarding how they managed their child’s CAH. None of the dyads expressed any discrepant management views, nor any significant tension in their relationship related to their child’s CAH. Parents described a dramatic difference in how they initially viewed CAH at the time of diagnosis and how they viewed it now, with an emphasis on the condition becoming easier to manage over time. All of the parents having a child over the age of 5 reported that their view of the condition began to change around the time their child turned 5 years old, which supports the Phase 1 finding that parents find the condition more manageable when their child becomes school age. According to parents, one reason for this change in their view of the condition was their child being able to articulate how he/she was feeling physically and emotionally. Additionally, by the time the child was 4, all of the parents had successfully managed an adrenal crisis. At the time of the interview, their management mindset was one of confidence.
In the first few months [after diagnosis] it was trying to understand it. It was educating. It was learning about it. It was researching. It was trying to understand how it happened, why it happened … The first couple of years were the roughest but as he’s grown and gotten better, it is easier.
Parents in all nine families had experienced an adrenal crisis event, with parents in eight of the nine families describing multiple crisis episodes. Parents acknowledged that these life-threatening events contributed greatly to how they viewed the illness and their management capacity. Parental accounts of adrenal crisis episodes were most often linked to gastrointestinal illnesses involving repeated vomiting as well as trauma related to accidental injuries related to outdoor activities. Adrenal crisis events were described as inherently stressful, and parents stated that knowing that their child could die if their response was not effective was both overwhelming and terrifying.
And the doctors would explain to you ‘Now he’s not going to die as long as you just do what you’re supposed to do.’
It [adrenal crisis event] was the most terrifying thing I’ve ever experienced. It was because we did not have all of the information, so we weren’t prepared.
One day my wife and him they were outside, and he was playing normal and fine. He wasn’t sick, he didn’t have a cold, he didn’t have anything that would have caused it. He was running across the yard and the next thing you know he was face down in the yard.
With few exceptions, parents labeled their child’s life and their family life as “normal,” and the parents who were partnered described a strong sense of agreement in their approach to managing the condition. Over time, parents developed a daily routine for condition management that they viewed as manageable. However, during illness and adrenal crisis, there were management challenges, and during these times, the parental view of the condition and the child would temporarily change.
4.2 Management behavior
The Management Behavior Component of the FMSF includes parenting philosophy and management approach, including management routines (Knafl et al., 2012). Parents described daily management of CAH as relatively straightforward, consisting of giving their child oral steroids two to three times a day. However, four dyads described a highly structured routine that could not be compromised in any way when discussing the exact timing of administering the medication.
Going back to us being super science-based we’re very, very strict on like eight hours, her medication every eight hours. So we do follow this one hundred percent, and she has her medication at like eight, four and midnight.
Across families, one parent, either the mother or the father, was usually responsible for daily management including medication administration, communicating their child’s special health needs to others in their child’s social network, and taking their child for healthcare provider visits. However, both parents reported being trained and capable of giving the hydrocortisone injection when needed. Although parents in the seven dyads described a shared view of the condition, several parents expressed that they felt they and their partner had differing management approaches. For example, regarding stress dosing and giving the IM injection, one parent might feel more anxious and take the “better safe than sorry” approach of giving the stress dose, while the other parent was more willing to “wait it out”; however, none of the parents described this as a source of significant conflict.
I’d say when it comes to time … when he gets a little bit sick, sometimes she’ll get into a mentality of ‘oh it’s not that big of deal,’ and I have a much quicker trigger finger. I am ready to start stress dosing.
He constantly worries. He is just always worried about what we did [stress dosing]. I’m more like, well, I always felt like we could get him help you know what I mean? There are hospitals everywhere is how I feel. But he’s like, he’s very anxious.
Regarding parenting philosophy, every parent interviewed discussed making a conscious choice to treat their child normally and not unnecessarily restrict activities because of the condition. They also described their family life in general as similar to that of other families.
I think it’s extremely important to make these children feel that they’re really not that different. That everybody has something and this happens to be what you have, what your child has. And they can do anything they want to do you shouldn’t limit them.
4.3 Perceived consequences
Perceived consequences are the extent to which family life is focused on the child and future expectations for the child and how the family is viewed as linked to the condition (Knafl et al., 2012). Parents described how efforts to incorporate CAH management as part of the usual family routine were successful; however, unpredictable, acute illnesses and the possibility of adrenal crisis could dramatically disrupt that routine. Parents remained hopeful regarding their child’s future, but also expressed concerns for their child’s health and wellbeing in regards to puberty/adolescence as well as their anticipation that they would have less control over the treatment regimen and response to crises as the child becomes a young adult.
My expectation is she’s going to have a normal life. And she’s got a pretty good head on her shoulders.
We all worry about him being by himself or somebody not knowing he’s sick or not knowing what’s going on and that bothers me. I think I want him to live next door to me.
Yeah and I think about that when she goes to college, you know? Is she going to be equipped? Are the medical centers going to be equipped if she gets hurt or if she drinks too much and she’s vomiting the next day? You know I think about those things.
Parents in eight of the nine families interviewed had children other than their child with CAH. When asked, parents stated they felt CAH had minimal impact on the siblings; however, parents noted that siblings did experience distress during adrenal crisis episodes in their child with CAH. Parents expressed concern that some of the events experienced by siblings, especially related to paramedics at the home and hospitalizations of the child with CAH, would create long-lasting negative childhood memories for siblings. Additionally, parents in three families stated that siblings exhibited jealous behavior regarding the extra attention that the child with CAH received because of special care needs, illness, or crisis.
Finally, for some parents, having a child with CAH resulted in challenging reproductive decisions. Six parents interviewed described making a decision to not have other children after their child with CAH because they did not feel capable of managing the care of more than one child with an episodically life-threatening condition. Parents in one family did have subsequent children, but opted for prenatal treatment of dexamethasone (the baby she was carrying was a girl) in an effort to prevent virilization, while parents in another family chose to have another child but not take dexamethasone and knowingly risk having another girl with possible virilization. Parents in another family chose to do a preimplantation genetic diagnosis to determine if CAH was present in any of the embryos produced through in-vitro fertilization prior to implantation in an effort to ensure their subsequent child did not have the condition. A recurrent theme concerning the perceived consequences for families having a child with CAH was the need for additional or special planning. Family planning after having one child with CAH, planning for potential adrenal crisis events, and planning for their child’s health and safety as they grow into adolescents and young adults were areas parents described as requiring additional planning and decision-making challenges because of their child’s CAH.
4.4 Contextual influences on family management
There were multiple contextual influences that parents discussed in the interviews that they perceived as relating to the family management of CAH. These contextual influences included healthcare providers, school personnel, babysitters, extended family, and extracurricular activities in which the child participated, primarily sports.
4.4.1 Interchanges with healthcare providers and school personnel
Parents stated that although they were satisfied with the relationships they had with their current pediatric endocrinologists, providers did not offer support to them emotionally and did not refer them to family support groups—local nor national.
[The doctor] sat down, and he explained the medical terms of it all… And then basically he re-described the whole scenario to us in terms that I can understand.
As far as [providers] being there emotionally, I don’t know if his doctors ever really played that role. I think – I just don’t see them – or I can’t cite an example where there’s the pat on the back or the hug. Nothing like that.
The management of CAH, especially during times of illness, remains complicated and stressful for parents. Although parents reported feeling pleased with their current pediatric endocrinologists, parents from five families described not being appropriately prepared by their initial providers for adrenal crisis events, which prompted them to change healthcare providers. Parents stated that their current providers have educated them on how to administer the emergency injection of hydro-cortisone; however, the process had been demonstrated only one time by either their pediatric endocrinologists or their staff members (i.e., nurses, physician assistants, medical assistants). Four parents voiced concern that one-time instruction was insufficient in terms of feeling confident in their ability to effectively manage an adrenal crisis.
They [initial pediatric endocrinologist office] did not demonstrate anything. They actually could not even give us a correct dosage of how much to put in the syringe. They gave us a piece of paper that had instructions on it and sent us on our way.
We actually asked for it [prescription for injectable hydrocortisone] at our doctor’s visit. I knew about it from the websites I had looked at. And we had a written piece of paper they [pediatric endocrinologist’s office] gave us on how to give it. So basically, we watched a You-Tube video on our own [to learn how to give the injection].
Consistent with the significant relationship between parents having been shown how to given the injection by healthcare providers and an increased perception of management ability in Phase 1, parents who expressed satisfaction in the interviews regarding how their providers have prepared them to handle adrenal crisis events described being taught how to administer the injection by a nurse or doctor face-to-face.
Parents described educating their child’s school nurse or daycare provider on CAH and reviewing injection instructions with school nurses on a yearly basis. Overall, parents reported favorable experiences with school personnel regarding nurse preparation and teacher understanding of the condition; however, several parents describe an often lengthy and repetitive process of nurse/staff education as well as anxiety whenever a new nurse joined the school staff or when the child changed schools.
From very early on when she was getting ready to start a new school, my wife would go and make an appointment before school started with the school nurse, bring the shot kit and spare meds and all of the other stuff to leave with them in their medicine cabinet during the school year. Bring them a letter that our pediatric endocrinologist would write to explain what was going on, warning signs, how to react, who the emergency contacts are, that’s been something she’s done you know every year. But each time when she has change schools, you know moved up from you know kindergarten to first grade to elementary, we have to start all over with the nurse and how is that nurse going to respond. But it’s usually gone well.
4.5 Social network
4.5.1 Babysitters
Parents in seven of the families interviewed discussed specific management challenges related to times when babysitters were needed for their child with CAH. These challenges were related to fear over their child becoming ill while under the care of the babysitter, not knowing how much instruction to give the babysitter regarding the injection (i.e., Is a demonstration on how to give the injection necessary?), and misgivings that teenage babysitters would be unable to handle an adrenal crisis event. Parents stated that they preferred to use family members who had been taught how to respond to a crisis as babysitters; furthermore, they described varying strategies to educate babysitters on their child’s condition.
I have taught the babysitter how to give the injection. And I write it down on a piece of paper… like really simple steps if they would have to. But I would always emphasize to just call 911.
This is my son, so if you’re going to be around my son, you’re going to know what to do. You’re going to know what to look for. You’re going to understand. Now what might happen to him if I leave the room, if I run to the store, if whatever. If you’re with my child you’re going to know what he has and how to do the basic treatment of it.
4.5.2 Extended family
Parents from six families described their extended families as supportive and helpful, especially with regards to child care. However, other parents relayed struggles with how their extended families dealt with the diagnosis initially, expressed concern over extended family members’ inability to fully understand the challenges associated with CAH management, and stated that their families were too afraid to help with their child’s care. These struggles created tension within the family.
Some of the other people, like my mom and our friends that watch him for short periods of time … I don’t think they understand the severity of the condition. They just see him, and to them he’s a normal kid.
I tried to educate my family and his but they’re just not interested–they don’t understand it. And I guess me and my husband both have felt a little bit of animosity towards them because they don’t. I guess they don’t show the worry or see the seriousness in it. And that’s kind of made us a little bit mad.
4.5.3 Extracurricular activities/coaches/sports
Parents in seven families had children who were actively participating in at least one school- or community-based sport including soccer, volleyball, hockey, track, and t-ball. The two children not participating in sports were the two youngest—ages 2 and 3. Parents relayed how sports participation was a source of concern and described fears that physical exertion might trigger an adrenal crisis; however, parents also stated that they wanted their children with CAH to participate in sports because of the benefits, both socially and physically, associated with being on a sports team. Parents discussed the importance of instructing coaches about the signs and management of a crisis. Of the seven children currently playing sports, parents in one family had chosen not to inform the coach about the condition; however, one of those parents brings the emergency injection kit to every practice and competition and stays near the child. Parents in only one family had instructed their child’s coaches about how to give the injection and confirmed that the coach was willing to administer an injection if needed.
Because there is a lot of explaining that needs to go on [for the coaches]. We have to say if you don’t do the right thing, he’s going to go into a death spiral so it’s a fine line.
4.5.4 Access to resources
Parents in five of the families reported leaving their initial pediatric endocrinologists soon after the time of diagnosis because of dissatisfaction with the provider’s level of knowledge about CAH as well as a lack of education on adrenal crisis from the provider. Two different mothers stated:
Because what I was finding was that it could be fatal if not treated correctly. And the endocrinologist we had at the time was not somebody we liked at all and did not explain this to us.
I didn’t feel like she [the pediatric endocrinologist] had much experience… I think it’s rare and there’s not very many cases period. But she couldn’t put us at ease basically.
For parents in four of the families, this required finding a pediatric endocrinologist in another state and a far distance from their homes. Parents reported having to drive long distances to see pediatric endocrinologists two to three times per year.
Yeah now we’ve been stable now for I think two years with the one we got but we still have to drive three and a half hours away [to see new pediatric endocrinologist].
There’s not one [a pediatric endocrinologist] –the closest one to us is about three hours. And we did actually start out with that endocrinologist but she started him on the prednisolone instead of the hydrocortisone, and he wasn’t growing. She blamed us, said it was our fault and diagnosed him as failure to thrive and pretty much told us to prepare ourselves. So I called the CARES Foundation and got a list of good doctors, and I made an appointment at Vanderbilt and that’s where we went and we just stayed there ever since. It is a 8–9 hour drive.
Overall, parents detailed certain challenges related to managing the contextual influences on the family with regards to their child’s CAH. These included a lack of detailed and thorough adrenal crisis preparation from healthcare providers, repeated adrenal crisis education needs for people in their child’s social network such as teachers, babysitters, and coaches, as well as interactions with their extended family related to their child’s condition.
5 DISCUSSION
This study provided evidence that over time parents adapt to the management challenges of having a child with CAH, but the threat of adrenal crisis remains an ongoing concern. Parents stated that their children are, for the most part, living normal lives despite having CAH. However, this appears at odds with parental responses when asked about their child’s interactions with others in their social network, as parents described being hesitant to allow their child to play at friends’ homes and challenges finding child care with which they were comfortable with.
Living with the uncertainty of an adrenal crisis is challenging for parents, especially in the context of not being properly prepared by healthcare providers to manage adrenal crisis events. When parents are not properly prepared on how to manage the life-threatening aspects of CAH, the result can be a reliance on EMS services and emergency departments to manage crisis events. For example, one quarter of parents surveyed did not receive the prescription or injectable hydrocortisone within a month of their child’s birth. Due to the need for an immediate, effective response to the signs and symptoms of adrenal crisis, a reliance on outside emergency services could lead to serious injury and possible death of the child if the response is not swift or treatment is misunderstood.
Additional stressors for these families include how to best interact and educate others in their child and family’s life regarding CAH management, especially adrenal crisis events. For example, finding appropriate child care, which includes care providers trained to give a hydrocortisone injection, is a particular challenge and has the potential to leave families feeling isolated and unable to function optimally. The child’s social environment including school, daycare, and extracurricular activities also produces challenges for parents regarding fear of adrenal crisis episodes when they are not present. Finally, unsupportive healthcare providers who focus entirely on physiological outcomes related to CAH, but fail to provide emotional support and repeated instruction/demonstration on adrenal crisis response further created frustration for parents trying to manage and inherently stressful, life-threatening condition.
There were some limitations to this study. Parents participating in this study had sought out some form of support online through the CARES Foundation; thus, these parents were likely to express strong motivation to educate themselves about CAH. They may have had greater knowledge of the condition and demonstrated stronger self-education practices than parents not associated with the organization. On the other hand, the parents registered with CARES were a diverse group with regard to geographic location, age, and socioeconomic status. The majority of participants were Caucasian, which is not surprising as in the USA the incidence of CAH is much lower in the African American, Hispanic, and Asian populations (Pass & Neto, 2009). Parents of adolescents were underrepresented, so issues specific to this age group may have been missed. Finally, families without computer access were not included in this study, which may have further limited sample variability; however, the majority of homes in the USA have some form of Internet access (File & Ryan, 2014).
5.1 Practice implications
Understanding and identifying gaps in parent education by healthcare providers, especially concerning times of adrenal crisis, is necessary to promote positive family outcomes, both from an emotional standpoint as well a child health perspective. Provider support is needed for these parents throughout childhood, but especially in the first 5 years of life when parents are adjusting to having a child with a life-threatening condition and children frequently acquire common childhood illnesses that require stress dosing of hydrocortisone as well as associated hospitalizations (Rushworth, Falhammar, Munns, Maguire, & Torpy, 2016). Developing interventions that encourage appointments with healthcare providers to include a focus on the nonmedical aspects of life with CAH in an effort to increase emotional support from providers to families is needed. For example, regular appointments and check-ups with providers should include discussions about how families are handling the child’s extracurricular activities, school environment, height and weight difficulties, and child care when a parent is unavailable, as these are all aspects of CAH management that have the potential to disrupt family life. Moreover, developmentally appropriate education for the child throughout the lifespan and during the time of transition from a pediatric endocrinologist to an adult endocrinologist to prepare youth in the management of their chronic health condition is needed. Finally, detailed and uniform education from providers on how to effectively handle adrenal crisis episodes has great potential in preventing costly emergency room visits and providing peace of mind to caregivers of children with CAH.
Acknowledgments
Funding Information
This research was funded by the National Institute of Nursing Research Grant #5T32NR007091-18, an American Nurses Foundation/SNRS Research Grant, and a CARES Foundation Research Grant.
Footnotes
The authors report no actual or potential conflicts of interests.
References
- Ayres L, Kavanaugh K, Knafl K. Within-case and across-case approaches to qualitative data analysis. Qualitative Health Research. 2003;13(6):871–883. doi: 10.1177/1049732303013006008. [DOI] [PubMed] [Google Scholar]
- Boyse KL, Gardner M, Marvicsin DJ, Sandberg DE. It was an overwhelming thing”: Parents’ needs after infant diagnosis with congenital adrenal hyperplasia. Journal of Pediatric Nursing. 2014;29(5):436–441. doi: 10.1016/j.pedn.2014.01.007. https://doi.org/10.1016/j.pedn.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen GA. Naturalistic inquiry and the saturation concept: A research note. Qualitative research. 2008;8(1):137–152. [Google Scholar]
- CARES Foundation. 2014 Retrieved from http://www.caresfoundation.org.
- Creswell JW, Clark VLP. Designing and conducting mixed methods research. Thousand Oaks, CA: SAGE; 2010. [Google Scholar]
- File T, Ryan C. Computer and Internet Use in the United States: 2013-American Community Survey Reports. 2014 Retrieved from http://www.census.gov/content/dam/Census/library/publications/2014/acs/acs-28.pdf.
- Fleming L, Rapp C, Sloane R. Caregiver knowledge and self-confidence of stress dosing of hydrocortisone in children with congenital adrenal hyperplasia. Journal of Pediatric Nursing. 2011;26:55–60. doi: 10.1016/j.pedn.2011.03.009. https://doi.org/10.1016/j.pedn.2011.03.009. [DOI] [PubMed] [Google Scholar]
- Knafl GJ, Ding K. Adaptive regression for modeling nonlinear relationships. Switzerland: Springer International Publishing; 2016. [Google Scholar]
- Knafl K, Deatrick J, Havill N. Continued development of the family management style framework. Journal of Family Nursing. 2012;18(1):11–34. doi: 10.1177/1074840711427294. https://doi.org/10.1177/1074840711427294. [DOI] [PubMed] [Google Scholar]
- Knafl K, Deatrick J, Knafl G, Gallo A, Grey M, Dixon J. Patterns of family management of childhood chronic conditions and their relationship to child and family functioning. Journal of Pediatric Nursing. 2013;28:523–535. doi: 10.1016/j.pedn.2013.03.006. https://doi.org/10.1016/j.pedn2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knafl K, et al. Family Management Measure (FaMM) 2012 Retrieved from http://nursing.unc.edu/research/office-of-research-support-consultation/resources/family-management-measure-famm/
- Merke DP, Bornstein SR. Congenital adrenal hyperplasia. Lancet. 2005;365(9477):2125–2136. doi: 10.1016/S0140-6736(05)66736-0. [DOI] [PubMed] [Google Scholar]
- Pass K, Neto U. Update: Newborn screening for endocrinopathies. Endocrinology Metabolism Clinics of North America. 2009;38:827–837. doi: 10.1016/j.ecl.2009.08.005. [DOI] [PubMed] [Google Scholar]
- Rushworth RL, Falhammar H, Munns CF, Maguire AM, Torpy DJ. Hospital admission patterns in children with CAH: Admission rates and adrenal crises decline with age. International Journal of Endocrinology. 2016;2016:1–8. doi: 10.1155/2016/5748264. https://doi.org/10.1155/2016/5748264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandelowski M. “Casing” the research case study. Research in Nursing and Health. 2011a;34(2):153–159. doi: 10.1002/nur.20421. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Parallelism in constant comparison analysis. Research in Nursing and Health. 2011b;34(6):433–434. doi: 10.1002/nur.20455. [DOI] [PubMed] [Google Scholar]
- Speiser P, Azziz R, Baskin L, Ghizzoni L, Hensle T, Merke D, White P. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency: An endocrine clinical practice guideline. Journal of Clinical Endocrinology & Metabolism. 2010;95(9):4133–4160. doi: 10.1210/jc.2009-2631. https://doi.org/10.1210/jc.2009-2631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni J, Sherman S, Burwinkle T, Dickinson P, Dixon P. The PEDsQL family impact module: Preliminary reliability and validity. Health and Quality of Life Outcomes. 2004;2:55–60. doi: 10.1186/1477-7525-2-55. https://doi.org/10.1186/1477-7525.2-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VERBI Software. MAXQDA 12 Reference Manual (v1.0) 2015 [Google Scholar]
- Witchel S, Azziz R. Congenital adrenal hyperplasia. Journal of Pediatric Adolescent Gynecology. 2011;24:116–126. doi: 10.1016/j.jpag.2010.10.001. https://doi.org/10.1016.j.jpag.2010.10.001. [DOI] [PubMed] [Google Scholar]


