Abstract
Background
Arjunarishta (AA), a formulation used as cardiotonic is a hydroalcoholic formulation of Terminalia arjuna (Roxb.) Wight and Arn. (TA) belonging to family Combretaceae.
Objective
To evaluate the anti-hyperglycemic and anti-hyperlipidemic effect of Arjunarishta on high-fat diet fed animals.
Materials and methods
High-fat diet fed (HFD) Wistar rats were randomly divided into three groups and treated with phytochemically standardized Arjunarishta (1.8 ml/kg), and hydroalcoholic extract of T. arjuna (TAHA) (250 mg/kg) and rosuvastatin (10 mg/kg), for 3 months. Intraperitoneal glucose tolerance test, blood biochemistry, liver triglyceride and systolic blood pressure were performed in all the groups. Effect of these drugs on the expression of tumor necrosis factor-α (TNF-α) and insulin receptor substrate-1 (IRS-1) and peroxisome proliferators activated receptor γ coactivator 1-α (PGC-1α) were studied in liver tissue using Quantitative Real-time PCR.
Results
HFD increased fasting blood glucose, liver triglyceride, systolic blood pressure and gene expression of TNF-α, IRS-1 and PGC-1α. Treatment of AA and TAHA significantly reduced fasting blood glucose, systolic blood pressure, total cholesterol and triglyceride levels. These treatments significantly decreased gene expression of TNF-α (2.4, 2.2 and 2.6 fold change); increased IRS-1 (2.8, 2.9 and 2.8 fold change) and PGC-1α (2.9, 3.7 and 3.3 fold change) as compared to untreated HFD.
Conclusion
Anti-hyperglycemic, anti-hyperlipidemic effect of Arjunarishta may be mediated by decreased TNF-α and increased PGC-1α and IRS-1.
Keywords: Rosuvastatin, Type 2 diabetes, Insulin sensitizer genes, Arjunarishta
Graphical abstract

1. Introduction
Natural products have been considered the leading source of treatment for several human diseases due to their wide chemical diversity and biological actions. Diabetes remains the most common metabolic disorder, generally differentiated by hyperglycemia with disturbance of carbohydrate, fat, and protein metabolism resulting from defects in insulin secretion, action or both [1], [2].
Type 2 diabetes (T2DM) is associated with abnormal glucose utilization, insulin resistance, and hyperlipidemia. Lipoprotein abnormalities are the major cause of cardiovascular (CV) morbidity and mortality in diabetes patients who require additional lipid-lowering agents along with their antidiabetic medications while, available antidiabetic agents do not exert a favourable effect on lipid abnormalities [3]. The commonly used anti-hyperlipidemic agents such as statins adversely manipulate glycemic control. Due to this reason, the need for novel treatment strategies which offer more benefits to patients suffering from T2DM was created, focusing on treatments that produce better glycemic control, appetite regulation, blood pressure, lipid reduction and weight loss. Also, there has been a growing emphasis on therapy of hyperlipidemia associated with diabetes to develop newer antidiabetic agents with potential anti-hyperlipidemic effects [4].
Traditional Indian Medicinal System (TIMS) utilizes a large number of plants and derived preparations, which are often difficult to characterize through phytochemical, pharmacological, and toxicological investigations. Terminalia arjuna (Roxb.) Wight and Arn. (TA) and its traditional preparations were used in Ayurveda for their cardiotonic and antidiabetic effects for many years [5], [6]. Several clinical investigations have suggested its usefulness in relieving angina pain and in the treatment of coronary artery disease, heart failure and possibly hypercholesterolemia [7], [8], [9]. Raghavan and Krishnakumari have provided evidence for the beneficial effect of hydroalcoholic bark extract of TA (TAHA) in relation to the treatment of diabetes, reporting a reduction in serum glucose levels as well as protection against the destruction of pancreatic beta cells and kidney damage in animals with alloxan-induced diabetes [10].
Few studies have been undertaken to understand the mechanism of this plant in diabetes and its related complications [11]. Earlier studies indicated that the anti-inflammatory and antioxidant activities of TA could be the one of the mechanisms behind its antidiabetic effects [12]. Till date, the exact molecular mechanism of TA bark in diabetes is unknown. Chemically, TA contains polyphenols such gallic acid, ellagic acid, and triterpenoids like arjunolic acid, arjunic acid, arjunetin, arjungenin, arjunglucoside I and II [13].
In Ayurveda, Arjunarishta (AA) is an ancient hydroalcoholic Ayurvedic formulation having the highest percentage of TA and used for the treatment of CVD. It nourishes and strengthens the heart muscle and promotes cardiac functioning by regulating blood pressure and cholesterol [14].
Therefore, the present study was undertaken to evaluate the anti-hyperglycemic and anti-hyperlipidemic effects of phytochemically standardized AA in high-fat diet fed (HFD) animals.
2. Materials and methods
2.1. Test materials, extraction, and formulation
The dried bark of TA was purchased from Trimurti Traders, Pune, India. A botanist authenticated the plant material from Agharkar Research Institute, Pune, India. The sample was deposited at Agharkar Research Institute, Pune, India with voucher specimen no. S/B-109. The dried bark was extracted with ethanol : water (70:30 v/v) using Soxhlet extractor for 3 consecutive days at 65 °C. The extract was dried under vacuum using rotary evaporator at 45 °C. AA; traditional formulation containing TA was procured from the local market (Batch no. 25; Sandu Pharmaceuticals Ltd., Mumbai, India).
2.2. Chemical characterization of selected test materials using HPLC-PDA analysis
Chemical characterization was carried using polyphenolics such as gallic acid, ellagic acid, and quercetin by HPLC method [15]. The method was modified as per laboratory conditions [15], [16]. Prominence HPLC system (Schimatzu, Japan) equipped with the binary pump, autosampler, a column oven and a photodiode array detector was used. Chromatographic separations were carried out using C-18 analytical column (150 × 4.6 mm, 5 μm particle size; Syncronis, Thermo Scientific, USA). Gradient elution with water containing 0.5% acetic acid as component A and acetonitrile : water containing 0.5% of acetic acid (80:20 v/v) as component B were used.
The non-linear gradient elution program: 0–10 min 10% of B; 10–20 min 20% of B; 20–30 min 40% of B; 30–40 min 60% of B; 40–45 min 70% of B; 45–55 min 10% of B and equilibrated with initial conditions for another 5 min. The flow rate and oven temperature were used at 1 ml/min and 25 °C respectively. All chromatograms were monitored at 270 nm. The method was validated for linearity, accuracy, and precision.
2.2.1. Reference compound preparation
Each reference compound (10 mg) was dissolved in 10 ml of methanol. Serial dilutions were carried out from the working stock solution in methanol (600 μg/ml). Calibration curves were plotted from concentration range of 3.125–100 μg/ml in triplicate.
2.2.2. Sample preparation
Sample preparation was done as per previously reported method [15]. Briefly, 10 mg of TAHA extract was dissolved in 10 ml methanol, and the solution was filtered through 0.45 μm membrane filter. AA (1 ml) was dried on a rotary evaporator for 0.5 h, and 5 ml of methanol was added. It was sonicated for 10 min and then centrifuged at 3000 rpm for 10 min. The supernatant (1 ml) was passed through 0.45 μm membrane filter. Sample solutions of 20 μl were used for HPLC analysis. The peaks of ellagic acid, gallic acid, and quercetin were identified by comparing their retention time values and UV spectra with those of standards. The marker contents for TAHA and AA were expressed as mg/g and μg/ml respectively.
2.3. Study animals and ethics committee approval
Male Wistar rats, weighing from 200 to 250 g body weight were used in this study. Animals were procured and maintained at National Toxicology Centre, APT Research Foundation, Pune, India. They were housed in makrolon cages under standard laboratory conditions (light and dark cycle of 12 h at temperature 21 ± 2 °C with a relative humidity of 55 ± 10%). The animals were fed with commercial HFD (45%) procured from VRK Nutritional Solutions, Pune, India. The composition of HFD is mentioned in Supp. Table no. 1. All animals had free access to water during the experimental period. The study protocol was approved by Institutional Animal Ethics Committee (Certificate was attached as Supp. Figure. No. 1). All institutional and national guidelines for the care and use of laboratory animals were followed.
2.4. Experimental design
Forty animals were randomly divided into five groups containing eight animals in each group. The detailed study groups were as follow: (Group I) Normal Diet + Vehicle (distilled water), (Group II) HFD + Vehicle (distilled water), (Group III) HFD + Rosuvastatin (10 mg/kg), (Group IV): HFD + AA (1.8 ml/kg), (Group V) HFD + TAHA (250 mg/kg).
According to the conversion table based on surface area, the adult human dose multiplied by 0.018 gave the dose for rat weighing 200 g [17]. The dose was selected based on adult human dose (20 ml per day). It was converted using USFDA guidance considering the weight of rat as 200 g. Animals were studied for glucose tolerance using intraperitoneal administration of glucose (2 g/kg). Blood was collected for evaluation of serum biochemical parameters such as total cholesterol (TC), triglyceride (TG) and high density lipoproteins (HDL). The animals were then sacrificed, and liver tissue was collected and stored at −70 °C for RNA isolation. RNA was isolated for gene expression studies.
2.5. Collection of blood samples and lipid profile test
The blood samples were collected on the 90th day from the retro-orbital venous plexus of rats without any coagulant for the separation of serum. Serum samples were analyzed for biochemical parameters with the help of commercially available kits produced by Crest Biosystem, Pune, India (Crest Biosystems a division of Coral Clinical Systems is a part of the innovative Tulip Group of Companies). Low density lipoprotein cholesterol (LDL-C) and very low density lipoprotein cholesterol (VLDL-C) were calculated by using Friedewald's equation [18].
2.6. Intraperitoneal glucose tolerance test (IPGTT)
Animals were fasted overnight before IPGTT. An IPGTT was performed on male Wistar rats 90 days after the onset of treatment. Rats were injected with d-glucose at 2 g/kg body weight. Blood samples were drawn from the tail vein before glucose administration at 60, 120 and 180 min thereafter. Blood glucose content was measured using a commercial Glucometer (Contour, Bayers). The results were expressed as area under the curve (AUC0–180 min) calculated by using GraphPad Prism 5.00 Software [San Diego, USA] [19], [20].
2.7. Systolic blood pressure determination
Systolic blood pressure was measured in consciously restrained animals with a tail-cuff sphygmomanometer, using a non-invasive blood pressure instrument (AD Instrument, Australia). Thirty minutes before the measurements, the animals were placed into restrainers, with the tail exposed. The tail cuff was fitted to the base of the tail, and the pulse sensor was place just behind the tail cuff. The pressure in the occlusion cuff and the pulse signal were recorded in a Power Lab/400 system. The initiation of the pulse signals, after the inflation peaks, was correlated with the pressures in the occlusion cuff to obtain the mean systolic blood pressure readings for each animal.
2.8. TG levels in liver, peritoneal and epididymal tissue
TG was extracted from liver, peritoneal and epididymal tissue overnight in 500 μl heptane-isopropanol (3:2) at 4 °C. TG content was measured using a colorimetric kit as described above. The organic layer was collected and dried. The residue was dissolved in isopropanol for measuring triglyceride content with a colorimetric kit. All values of tissue triglyceride content were corrected for respective tissue weight and intra-assay co-efficient variation was 7.8% [21].
2.9. Hematology
To evaluate the toxicological effect of chronic supplementation of TAHA and AA, hematological parameters such as white blood cells (WBC), red blood cells (RBC), platelet count, hemoglobin (Hb) level, mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), mean corpuscular volume (MCV) were determined by the use of automated hematological analyzer.
2.10. RNA isolation and real-time PCR analysis
Total RNA was isolated using the TRI reagent (Sigma–Aldrich), according to the manufacturer's instructions. Total RNA (2 μg) was reverse transcribed into first-strand cDNA (ABI) following the manufacturer's procedure. The synthesized cDNA (50 ng/μl) was used as a template for polymerase chain reaction (PCR) amplification. Real-time PCR was performed using step one Real-time PCR system (ABI).
PCR was carried out for 45 cycles using the following conditions: denaturation at 95 °C for 45 s, annealing at 62.7 °C for 30 s, and elongation at 72 °C for 15 s. The relative expression levels of the target genes were calculated as a ratio to the housekeeping gene GAPDH. All the samples were in triplicate and each time no template control was done during plate run. Melting curve analysis was performed to assess the specificity of the amplified PCR products. A dissociation curve analysis of all primers showed a single peak. The primers used for SYBR Green Real-time PCR are mentioned in the Supp. Table 2. All relative quantification analysis was represented in the form of relative expression to the normal group (delta delta Ct) [22].
2.11. Statistical analysis
The experimental data were expressed as mean ± SEM. The significance of difference among the various treated groups and control group were analyzed by mean of one-way ANOVA followed by Dunnett's multiple comparison tests using GraphPad Prism 5.00 Software [San Diego, USA]. p < 0.01 and p < 0.05 were considered as statistically significant.
3. Results
3.1. HPLC-PDA analysis
Phytochemical standardization of AA and TAHA was carried out using selected marker-based approach. Polyphenolic compounds such as gallic acid, ellagic acid, and quercetin were used as chemical markers for standardization purpose. The marker contents were estimated using earlier reported HPLC-PDA method modified with column and mobile phase gradient. The optimized chromatographic conditions showed good resolution of all the peaks. The presence of marker contents in the AA and TAHA was identified using retention time (tR) and UV spectra matching with corresponding reference standards (Fig. 1). The tR for gallic acid, ellagic acid, and quercetin was found to be 2.36, 24.71 and 31.98 min respectively. The spectral overlays showed the presence of UV spectra at 270 nm and were matched with the reference standard (see inset of Fig. 1). Quantitative estimation of these marker compounds was carried out using external standard calibration method. The calibration plots of concentration versus peak area were constructed in the range of 3.125–100 μg/ml.
Fig. 1.
HPLC chromatogram of a. Reference standard spike polyphenols gallic acid, ellagic acid, and quercetin; b. Hydroalcoholic extract of T. arjuna (TAHA); c. Arjunarishta (AA).
The content of gallic acid, ellagic acid, and quercetin was 2.443 ± 0.090, 7.901 ± 0.786 and 3.20 ± 0.351 mg/g respectively in TAHA whereas 92.18 ± 1.184, 244.6 ± 8.676 and 15.82 ± 1.832 μg/ml respectively in AA (Table 1 and Fig. 1). These quantitative estimations were consistent with earlier reports on AA and TAHA.
Table 1.
Retention time and relative concentration of polyphenols in Arjunarishta (AA) and the hydroalcoholic extract of T. arjuna (TAHA).
| Sr. no. | Compound name | Rt (min) |
(μg/ml of AA) | (mg/g of TAHA) | ||
|---|---|---|---|---|---|---|
| Reference standard | AA | TAHA | ||||
| 1 | Gallic acid | 2.362 | 2.248 | 2.358 | 92.18 ± 1.184 | 2.443 ± 0.090 |
| 2 | Ellagic acid | 24.711 | 24.720 | 24.709 | 244.6 ± 8.676 | 7.901 ± 0.786 |
| 3 | Quercetin | 31.987 | 31.944 | 31.974 | 15.82 ± 1.832 | 3.20 ± 0.351 |
Results were expressed as mean ± SEM.
3.2. Hematology
Treatment with rosuvastatin, AA, and TAHA for 90 days did not alter the hematological investigations. No significant changes were observed on WBC, RBC, platelet, hemoglobin, percent hematocrit, MCV, MCH and MCHC in treated animals.
3.3. Intraperitoneal glucose tolerance test (IPGTT)
Glucose homeostasis was assessed in HFD fed animals treated with test materials by glucose tolerance test before and at the end of the experiment. Oral treatment of AA and TAHA significantly reduced AUC of blood glucose levels by 33.1% (p < 0.01) and 43.6% (p < 0.01; AUC0–180 min) as compared to diabetes control (DC) animals respectively (Fig. 2).
Fig. 2.
Effect of Arjunarishta (AA) and the hydroalcoholic extract of T. arjuna (TAHA) on IPGTT in HFD fed rats (A) blood glucose levels and (B) AUC0–180 min. Results were expressed as mean ± SEM [N = 8]. *p < 0.05 and ***p < 0.001 as compared to diabetes control.
3.4. Systolic blood pressure
Hypertension effect was tested on experimental animals after 30 and 90 days of initiating the study. Elevated systolic blood pressure was observed in the DC animals by 12% in comparison to healthy control (HC) animals. As shown in Fig. 3, a significant reduction of systolic blood pressure was demonstrated in animals treated with AA (p < 0.01), TAHA (p < 0.05), and rosuvastatin (p < 0.05) as compared to DC animals.
Fig. 3.
Effect of Arjunarishta (AA) and the hydroalcoholic extract of T. arjuna (TAHA) on systolic blood pressure in HFD fed rats (A) 1 month and (B) 3 month. Results were expressed as mean ± SEM [N = 8]. *p < 0.05 and **p < 0.01 as compared to diabetes control.
3.5. Metabolic parameters
HFD-fed animals showed a significant increase in TC, TG, LDL-C, VLDL-C (p < 0.001) and a significantly decreased level of HDL-C (p < 0.001) compared with the HC animals. HFD-fed animals with TAHA, AA, and rosuvastatin showed a significant fall in the level of TC, TG, LDL-C, VLDL-C (p < 0.05) and a significantly increased level of HDL-C compared with the DC animals (p < 0.05) (Table 2).
Table 2.
Effect of Arjunarishta (AA) and the hydroalcoholic extract of T. arjuna (TAHA) on metabolic parameters in HFD fed rats.
| Metabolic parameters |
|||||
|---|---|---|---|---|---|
| TG (mg/ml) | TC (mg/ml) | HDL (mg/ml) | LDL (mg/ml) | VLDL (mg/ml) | |
| Healthy control | 110.25 ± 3.33*** | 157.25 ± 4.77*** | 41.0 ± 2.65*** | 93.75 ± 4.56*** | 22.05 ± 0.66*** |
| Diabetic control | 264.5 ± 6.99 | 303.0 ± 9.11 | 23.75 ± 1.25 | 226.0 ± 8.09 | 52.9 ± 1.40 |
| Rosuvastatin | 150.75 ± 5.76*** | 243.75 ± 14.65* | 31.75 ± 2.25* | 181.5 ± 13.88* | 30.15 ± 1.15*** |
| AA | 182.75 ± 5.93*** | 239.25 ± 7.28*** | 33.0 ± 2.19* | 169.5 ± 9.53** | 36.55 ± 1.18*** |
| TAHA | 200.5 ± 5.38*** | 235.75 ± 6.68*** | 32.25 ± 1.70* | 163.0 ± 8.40*** | 40.1 ± 1.08*** |
Results were expressed as mean ± SEM [N = 8]. *p < 0.05, **p < 0.01, ***p < 0.001 when compared with diabetic control group. TG, Triglyceride; TC, Total Cholesterol; HDL, High-density lipoprotein; LDL, Low-density lipoprotein; VLDL, Very low-density lipoprotein.
3.6. TG levels in liver, peritoneal, and epididymal tissues
HFD-fed animals showed a significant increase in TG levels in liver, peritoneal and epididymal tissue after 30 and 90 days (p < 0.05) compared with the HC animals. HFD-fed animals with TAHA, AA, and rosuvastatin showed a significant fall in the level of TG in liver, peritoneal, and epididymal tissue after 30 and 90 days compared with the DC animals (p < 0.05) (Table 3).
Table 3.
Effect of Arjunarishta (AA) and the hydroalcoholic extract of T. arjuna (TAHA) on triglyceride levels in liver, peritoneal, and epididymal tissues after 30 and 90 days treatment.
| Group | Liver (mg/dl) | Peritoneal (mg/dl) | Epididymal (mg/dl) | |
|---|---|---|---|---|
| Healthy control | After 30 days | 266.4 ± 16.15* | 332.8 ± 22.25* | 318.9 ± 36.35* |
| After 90 days | 464.2 ± 23** | 296.3 ± 58.75*** | 236.9 ± 27.71*** | |
| Diabetic control | After 30 days | 381.1 ± 25.24 | 530.9 ± 36.05 | 600.9 ± 61.75 |
| After 90 days | 753.5 ± 50.51 | 533.6 ± 20.99 | 421.5 ± 10.15 | |
| Rosuvastatin | After 30 days | 280.5 ± 14.15* | 272.1 ± 17.5** | 314.6 ± 23.5** |
| After 90 days | 553.6 ± 41.1* | 373.4 ± 40.64* | 260 ± 22.5** | |
| AA | After 30 days | 237.9 ± 42.51** | 285.6 ± 31.51** | 190 ± 37.24*** |
| After 90 days | 327.3 ± 20.4*** | 304.7 ± 43.65** | 263 ± 4.676*** | |
| TAHA | After 30 days | 238.3 ± 19.11** | 327.2 ± 25.09** | 503.7 ± 6.35 |
| After 90 days | 251.0 ± 6.35*** | 249.3 ± 28.32*** | 240.1 ± 8*** | |
Values were expressed as mean ± SEM [N = 8]. *p < 0.05, **p < 0.01, ***p < 0.001 when compared with diabetic control group.
3.7. Molecular mechanism study
AA and TAHA were found to be modulating expression of insulin sensitizing genes. Significant reduction in pro-inflammatory cytokine TNF-α gene expression was observed in animals treated with AA and TAHA.
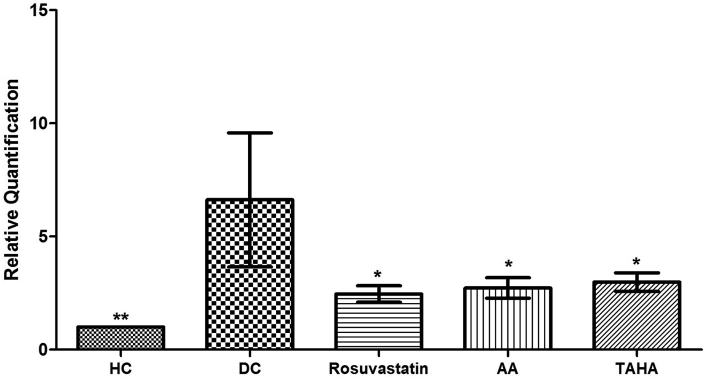
3.7.1. Inflammatory gene expression
The expression of the inflammatory gene in the liver is given in Fig. 4. The inflammatory gene, TNF-α was markedly upregulated in DC animals compared to HC animals, indicating the increase in cytokine levels which results into inflammation. Whereas, treatment with AA, TAHA, and rosuvastatin markedly downregulated (p < 0.05) mRNA expression of TNF-α (2.4, 2.2 and 2.6 fold change respectively) as compared to DC animals.
Fig. 4.
Effect of Arjunarishta [AA] and the hydroalcoholic extract of T. arjuna [TAHA] on the inflammatory gene in liver tissues after 90 days treatment. Values were expressed as mean ± SEM [N = 8]. *p < 0.05, **p < 0.01, ***p < 0.001 when compared with diabetes control group.
3.7.2. Insulin sensitizer gene expression
The expression of insulin sensitizer gene in the liver is given in Fig. 5. The insulin sensitizer genes including IRS-1 and PGC-1α were downregulated in DC animals as compared to HC animals (p < 0.05), indicating the insulin resistance through the inflammatory pathway. AA, TAHA, and rosuvastatin treatment significantly enhanced mRNA expression of IRS-1 (2.8, 2.9 and 2.8 fold change) and PGC-1α (2.9, 3.7 and 3.3 fold change) as compared to DC animals.
Fig. 5.
Effect of Arjunarishta [AA] and the hydroalcoholic extract of T. arjuna [TAHA] on insulin sensitizer genes in liver tissues after 90 days treatment. Values were expressed as mean ± SEM [N = 8]. *p < 0.05, **p < 0.01, ***p < 0.001 when compared with diabetes control group.
4. Discussion
The hyperglycemic state developed in HFD fed animal was due to the association of insulin resistance and glucose intolerance. The treatment effect on glucose tolerance and tissue utilization of glucose was studied using IPGTT. The IPGTT is advantageous as it was performed under physiological conditions and simulated a post-absorptive state in which the production and release of insulin and its responsiveness are necessary [23]. The IPGTT and AUC measure the rate of tissue uptake and glucose utilization. Oral treatment of AA, TAHA and rosuvastatin significantly reduced in blood glucose excursion as compared to DC animals (Fig. 2). A similar effect was produced by rosuvastatin and TAHA in diabetic animals [24]. The IPGTT results were in accordance with previous reports on the anti-glycemic potential of TA [25].
Regulation of dyslipidemia remains important in the diabetes etiology and complications. The study results indicate that prophylactic treatment with AA, TAHA, and rosuvastatin improves altered biochemical parameters in the HFD-fed animals, suggesting its beneficial effects in hyperlipidemia by significantly lower levels of TG, LDL-C, VLDL-C, TC and enhanced level of HDL-C. The study results as shown in Table 2 are supported with previous reports on the anti-hyperlipidemic potential of TAHA and rosuvastatin [26], [27]. DC animals demonstrated the significant increase in TC, TG, LDL-C, VLDL-C, whereas significantly decreased a level of HDL-C was observed in comparison to HC animals. HFD-fed animals with TAHA, AA, and rosuvastatin showed a significant fall in the level of total cholesterol, TG, LDL-C, VLDL-C and a significantly increased level of HDL-C compared with the DC animals.
Hyperglycemia and hyperlipidemia play an important role in the development of hypertension. Therefore, the anti-hypertensive effect was tested on experimental animals after 30 and 90 days of initiating the study. Elevated systolic blood pressure was observed in DC animals as compared to HC animals. As shown in Fig. 3, a significant reduction upto normal level was demonstrated in animals treated with AA, TAHA, and rosuvastatin as compared to DC animals. Similar findings on TAHA study has been previously reported [28], [29], [30]. Also, hematological results were similar to earlier reports for TAHA [26].
An abnormal accumulation of TG in liver, peritoneal, and epididymal tissues plays an important role in the pathophysiology of insulin resistance, atherosclerosis, hypertriglyceridemia, and T2DM [31], [32]. As shown in Table 3, study results demonstrated that tissue TG levels in DC animals were increased significantly as compared to HC animals. However, significant fall in the TG level was observed in AA, TAHA and rosuvastatin treated animals. Therefore, study findings on TG levels suggest improved condition of hypertriglyceridemia leading to T2DM. Even if the diabetes animals revealed a hypertriglyceridemic condition, it should be stressed that AA and TAHA displayed a higher capacity than that showed by rosuvastatin treatment.
The liver is an important principal organ for metabolism of carbohydrate, lipids and proteins leads to energy storage in the form of TG. HFD feeding conditions enhance cholesterol and TG in the liver exhibits hypertriglyceridemia and hyperlipidemia eventually in T2DM. To study the possible mechanism behind the anti-hyperglycemic, anti-hyperlipidemic and anti-hypertriglyceridemic activity, a gene expression study was investigated on liver-targeted genes involved in inflammatory and insulin signaling pathways.
Previous reports on TAHA demonstrated that cardiotonic and anti-hyperglycemic activity is associated with their anti-inflammatory effects [12], [33]. TNF-α has acted as a potential therapeutic target for new onset diabetes and mechanistic correlations between TNF-α and BMI, HOMA-IR, HOMA-B and insulin have been established in T2DM [34], [35]. To explore possible mechanism of AA and TAHA on animals, we have investigated the expression level of TNF-α related to anti-inflammation. As shown in Fig. 4, TNF-α was markedly upregulated in DC animals in comparison to HC animals, indicating HFD-induced enhancement of cytokine secretion, which results in inflammation. These findings were consistent with an earlier report published on TNF-α [36]. Whereas treatment with AA, TAHA, and rosuvastatin markedly downregulated (p < 0.05) mRNA expression of TNF-α as compared to diabetes control. Gene expression studies suggested the anti-inflammatory effect could be one of the mechanisms behind the anti-hyperglycemic potential of AA and TAHA.
Our study suggested that anti-glycemic potential of AA could be due to increase in facilitated glucose transport into the cell mediated through IRS-1. However, confirmatory studies on other intermediate genes involved in insulin signaling pathway need to be analyzed to understand the precise mechanism. Another targeted insulin sensitizer gene: PGC-1α is transcription co-activator to modulate glucose/fatty acid metabolism through enhanced gluconeogenesis and promotion of fatty acid oxidation suggesting key drug target for anti-hyperglycemic and insulin resistance-related disorders [37], [38], [39], [40]. Study results as illustrated in Fig. 5, IRS-1 and PGC-1α were downregulated in DC animals as compared to HC animals indicating HFD-induced cytokine secretion, which results in insulin resistance through the inflammatory mechanism. AA, TAHA, and rosuvastatin treatment significantly enhanced mRNA expression of IRS-1 and PGC-1α. Gene expression finding suggests that treatment with AA and TAHA might be restoring insulin sensitization along with anti-hyperglycemic effect by its anti-inflammatory activity. Further, upregulation of PGC-1α expression is well documented to induce gluconeogenic enzymes such as phosphoenolpyruvate carboxykinase and glucose 6-phosphate, thereby enhancing glucose uptake. This supports our study finding in a similar manner.
Treatment with AA and TAHA showed considerable modulation of targeted genes involved in inflammation and insulin signaling pathway as compared to rosuvastatin. Rosuvastatin is a competitive HMG-CoA reductase inhibitor indicated for the treatment of dyslipidemia, hypercholesterolemia, and hypertriglyceridemia [41]. The gene expression results of rosuvastatin are found to be consistent with earlier expression reports of statins [42].
Overall, the study demonstrated that AA and TAHA have multiple therapeutic effects mediated by insulin sensitization through its anti-inflammatory mechanism; decrease in the systolic blood pressure, TC, glucose and TG levels, which were elevated in the disease condition. Additionally, these results might be correlated with previous evidence of arjunolic acid, which acts as an anti-diabetes against hyperglycemia [43].
5. Conclusion
The present study represents the action of AA and TAHA in the treatment of hyperglycemia, hyperlipidemia, and hypertriglyceridemia. Activation of PGC-1α and IRS-1 due to a decrease in the gene expression of TNF-α is the key mechanism of activity. Further studies are needed to confirm signaling pathways for Ayurvedic formulation AA with multiple doses.
Conflict of interest
None
Sources of funding
None.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.jaim.2017.07.004.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Maniyar Y., Bhixavatimath P. Antihyperglycemic and hypolipidemic activities of aqueous extract of Carica papaya Linn. leaves in alloxan-induced diabetes rats. J Ayurveda Integr Med. 2012;3:70–74. doi: 10.4103/0975-9476.96519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaballu F.A., Gaballu Y.A., Khyavy O.M., Mardomi A., Ghahremanzadeh K., Shokouhi B. Effects of a triplex mixture of Peganum harmala, Rhuscoriaria, and Urticadioica aqueous extracts on metabolic and histological parameters in diabetes rats. Pharm Biol. 2015;53:1104–1109. doi: 10.3109/13880209.2014.960943. [DOI] [PubMed] [Google Scholar]
- 3.Tang W.H., Maroo A. Ischemic heart disease and congestive heart failure in diabetes patients. Med Clin North Am. 2004;88:1037–1061. doi: 10.1016/j.mcna.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 4.Datta A., Bagchi C., Das S., Mitra A., Patil A.D., Tripathi S.K. Antidiabetes and antihyperlipidemic activity of hydroalcoholic extract of Withania coagulans Dunal dried fruit in experimental rat models. J Ayurveda Integr Med. 2013;4:99–106. doi: 10.4103/0975-9476.113880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh G., Singh A.T., Abraham A., Bhat B., Mukherjee A., Varma R. Protective effects of Terminalia arjuna against Doxorubicin-induced cardiotoxicity. J Ethnopharmacol. 2008;117:123–129. doi: 10.1016/j.jep.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Amalraj A., Gopi S. Medicinal properties of Terminalia arjuna (Roxb.) Wight &Arn.: a review. J Tradit Complement Med. 2017;7:65–78. doi: 10.1016/j.jtcme.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Subramaniam S., Subramaniam R., Rajapandian S., Uthrapathi S., Gnanamanickam V.R., Dubey G.P. Anti-Atherogenic activity of ethanolic fraction of Terminalia arjuna bark on hypercholesterolemic rabbits. Evid Based Complement Altern Med. 2011 doi: 10.1093/ecam/neq003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bharani A., Ganguly A., Bhargava K.D. Salutary effect of Terminalia Arjuna in patients with severe refractory heart failure. Int J Cardiol. 1995;49:191–199. doi: 10.1016/0167-5273(95)02320-v. [DOI] [PubMed] [Google Scholar]
- 9.Gauthaman K., Banerjee S.K., Dinda A.K., Ghosh C.C., Maulik S.K. Terminalia arjuna (Roxb.) protects rabbit heart against ischemic-reperfusion injury: role of antioxidant enzymes and heat shock protein. J Ethnopharmacol. 2005;96:403–409. doi: 10.1016/j.jep.2004.08.040. [DOI] [PubMed] [Google Scholar]
- 10.Raghavan B., Kumari S.K. Effect of Terminalia arjuna stem bark on antioxidant status in liver and kidney of alloxan diabetes rats. Indian J physiol Pharmacol. 2006;50:133–142. [PubMed] [Google Scholar]
- 11.Lele R.D. Beyond reverse pharmacology: mechanism-based screening of Ayurvedic drugs. J Ayurveda Integr Med. 2010;1:257–265. doi: 10.4103/0975-9476.74435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Halder S., Bharal N., Mediratta P.K., Kaur I., Sharma K. Anti-inflammatory, immunomodulatory and antinociceptive activity of Terminalia arjuna Roxb bark powder in mice and rats. Indian J Exp Biol. 2009;47:577–583. [PubMed] [Google Scholar]
- 13.Jain S., Yadav P.P., Gill V., Vasudeva N., Singla N. Terminalia arjuna a sacred medicinal plant: phytochemical and pharmacological profile. Phytochem Rev. 2009;8:491–502. [Google Scholar]
- 14.Ragini H., Amita P., Jain A.K. An approach to standardize Arjunarishta: a well known ayurvedic formulation using UV and Colorimetric method. J Med Pharm Allied Sci. 2012;01:77–84. [Google Scholar]
- 15.Lal U.R., Tripathi S.M., Jachak S.M., Bhutani K., Singh I. HPLC analysis and standardization of Arjunarishta – an Ayurvedic cardioprotective formulation. Sci Pharm. 2009;77:605–616. [Google Scholar]
- 16.Chitlange S.S., Kulkarni P.S., Patil D., Patwardhan B., Nanda R.K. High- fingerprint for quality control of Terminalia arjuna containing Ayurvedic churna formulation. J AOAC Int. 2009;92:1016–1020. [PubMed] [Google Scholar]
- 17.Ghosh M.N. 6th ed. Hilton & Company; 2015. Fundamentals of experimental pharmacology. [Google Scholar]
- 18.Wu Z., Shen S., Jiang J., Tan D., Jiang D., Bai B. Protective effects of grape seed extract fractions with different degrees of polymerisation on blood glucose, lipids and hepatic oxidative stress in diabetes rats. Nat Prod Res. 2015;29:988–992. doi: 10.1080/14786419.2014.965165. [DOI] [PubMed] [Google Scholar]
- 19.Sattar E.A., Harraz F.M., Ghareib S.A., Elberry A.A., Gabr S., Suliaman M.I. Antihyperglycaemic and hypolipidaemic effects of the methanolic extract of Caralluma tuberculata in streptozotocin-induced diabetes rats. Nat Prod Res. 2011;25:1171–1179. doi: 10.1080/14786419.2010.490782. [DOI] [PubMed] [Google Scholar]
- 20.Lee B., Shi L., Kassel D.B., Asakawa T., Takeuchi K., Christopher R.J. Pharmacokinetic, pharmacodynamic, and efficacy profiles of alogliptin, a novel inhibitor of dipeptidyl peptidase-4, in rats, dogs, and monkeys. Eur J Pharmacol. 2008;589:306–314. doi: 10.1016/j.ejphar.2008.04.047. [DOI] [PubMed] [Google Scholar]
- 21.Deshpande M.S., Shengule S., Apte K.G., Wani M., Piprode V., Parab P. Anti-obesity activity of Ziziphus mauritiana: a potent pancreatic lipase inhibitor. Asian J Pharm Clin Res. 2013;6:168–173. [Google Scholar]
- 22.Hardikar A.A., Satoor S., Karandikar M., Joglekar M., Puranik A., Wong W. Multigenerational undernutrition increases susceptibility to obesity and diabetes that is not reversed after dietary recuperation. Cell Metab. 2015;22:312–319. doi: 10.1016/j.cmet.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 23.Mopuri R., Ganjayi M., Banavathy K.S., Parim B.N., Meriga B. Evaluation of anti-obesity activities of ethanolic extract of Terminalia paniculata bark on high fat diet-induced obese rats. BMC Complement Altern Med. 2015;15:76. doi: 10.1186/s12906-015-0598-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simsek S., Schalkwijk C.G., Wolffenbuttel B.H. Effects of rosuvastatin and atorvastatin on glycaemic control in Type 2 diabetes—the CORALL study. Diabet Med. 2012;29:628–631. doi: 10.1111/j.1464-5491.2011.03553.x. [DOI] [PubMed] [Google Scholar]
- 25.Parveen K., Khan R., Siddiqui W.A. Antidiabetes effects afforded by Terminalia arjuna in high fat-fed and streptozotocin-induced type 2 diabetes rats. Int J Diabetes Metab. 2011;19:23–33. [Google Scholar]
- 26.Ram A., Lauria P., Gupta R., Kumar P., Sharma V.N. Hypocholesterolaemic effects of Terminalia arjuna tree bark. J Ethnopharmacol. 1997;55:165–169. doi: 10.1016/s0378-8741(96)01493-6. [DOI] [PubMed] [Google Scholar]
- 27.Nigam G.K., Ansari M.N., Bhandari U. Effect of rosuvastatin on methionine-induced hyperhomocysteinaemia and haematological changes in rats. Basic Clin Pharmacol Toxicol. 2008;103:287–292. doi: 10.1111/j.1742-7843.2008.00293.x. [DOI] [PubMed] [Google Scholar]
- 28.Dwivedi S., Agarwal M.P. Antianginal and cardioprotective effects of Terminalia arjuna an indigenous drug in coronary artery disease. J Assoc Physicians India. 1994;42:287–289. [PubMed] [Google Scholar]
- 29.Sandhu J.S., Shah B., Shenoy S., Chauhan S., Lavekar G.S., Padhi M.M. Effects of Withania somnifera (Ashwagandha) and Terminalia arjuna (Arjuna) on physical performance and cardiorespiratory endurance in healthy young adults. Int J Ayurveda Res. 2010;1:144–149. doi: 10.4103/0974-7788.72485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khaliq F., Parveen A., Singh S., Gondal R., Hussain M.E., Fahim M. Improvement in myocardial function by Terminalia arjuna in streptozotocin-induced diabetes rats: possible mechanisms. J Cardiovasc Pharmacol Ther. 2013;18:481–489. doi: 10.1177/1074248413488831. [DOI] [PubMed] [Google Scholar]
- 31.Shimabukuro M., Zhou Y.T., Levi M., Unger R.H. Fatty acid-induced beta cell apoptosis: a link between obesity and diabetes. Proc Natl Acad Sci U S A. 1998;95:2498–2502. doi: 10.1073/pnas.95.5.2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McGarry J. Banting lecture: dysregulation of fatty acid metabolism in the etiology of type 2 diabetes. Diabetes. 2002;51:7–18. doi: 10.2337/diabetes.51.1.7. [DOI] [PubMed] [Google Scholar]
- 33.Parveen A., Babbar R., Agarwal S., Kotwani A., Fahim M. Mechanistic clues in the cardioprotective effect of Terminalia arjuna bark extract in isoproterenol-induced chronic heart failure in rats. Cardiovasc Toxicol. 2011;11:48–57. doi: 10.1007/s12012-010-9099-2. [DOI] [PubMed] [Google Scholar]
- 34.Swaroop J.J., Rajarajeswari D., Naidu J.N. TNF-α with insulin resistance in type 2 diabetes mellitus. Stud IJMR Assoc. 2012:127–130. doi: 10.4103/0971-5916.93435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Joshi K., Awte S., Bhatnagar P., Walunj S., Gupta R., Joshi S. Cinnamomum zeylanicum extract inhibits proinflammatory cytokine TNF∝: in vitro and in vivo studies. Res Pharm Biotechnol. 2010;2:14–21. [Google Scholar]
- 36.Borst S.E., Conover C.F. High-fat diet induces increased tissue expression of TNF-alpha. Life Sci. 2005;77:2156–2165. doi: 10.1016/j.lfs.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 37.Liang H., Ward W.F. PGC-1alpha: a key regulator of energy metabolism. Adv Physiol Educ. 2006;30:145–151. doi: 10.1152/advan.00052.2006. [DOI] [PubMed] [Google Scholar]
- 38.Handschin C., Spiegelman B.M. Peroxisome proliferator-activated receptor gamma coactivator 1 coactivators, energy homeostasis and metabolism. Endocr Rev. 2006;27:728–735. doi: 10.1210/er.2006-0037. [DOI] [PubMed] [Google Scholar]
- 39.Sumantran V.N., Tillu G. Cancer, inflammation, and insights from ayurveda. Evid Based Complement Altern Med. 2012 doi: 10.1155/2012/306346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gupta R., Walunj S., Awate S., Kulkarni R., Joshi S., Sabharwal S. Ethanolic extract of cinnamon potentiates in vitro pparγ reporter activity in presence of pgc1α and src1 and improves glucose tolerance in mice. Int Res J Biotechnol. 2011;2:47–57. [Google Scholar]
- 41.Olsson A.G., McTaggart F., Raza A. Rosuvastatin: a highly effective new HMG-CoA reductase inhibitor. Cardiovasc Drug Rev. 2002;20:303–328. doi: 10.1111/j.1527-3466.2002.tb00099.x. [DOI] [PubMed] [Google Scholar]
- 42.Wang W., Wong C.W. Statins enhance peroxisome proliferator-activated receptor gamma coactivator-1alpha activity to regulate energy metabolism. J Mol Med (Berl) 2010;88:309–317. doi: 10.1007/s00109-009-0561-1. [DOI] [PubMed] [Google Scholar]
- 43.Manna P., Ghosh J., Das J., Sil P.C. Streptozotocin induced activation of oxidative stress responsive splenic cell signaling pathways: protective role of arjunolic acid. Toxicol Appl Pharmacol. 2010;244:114–129. doi: 10.1016/j.taap.2009.12.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.