Abstract
Objective
To describe the process by which a group of subject matter experts (SMEs) in the area of occupational health and primary care developed a clinical decision support (CDS) tool addressing work-related issues, which are important in the care of patients with diabetes mellitus (DM). The CDS is intended for primary care clinicians caring for employed adults with DM.
Methods
The SME’s selected guidelines for the management of DM in working adults, reviewed pertinent literature, and developed specific recommendations for action in the clinical setting.
Results
Multiple factors at work may adversely affect DM management. Clinicians can support working patients through education and care strategies to improve control.
Conclusions
Improved recognition of factors at work that can have an impact on DM care provides opportunities for improved management of DM among working adults.
INTRODUCTION AND OVERVIEW
Subject matter experts (SMEs) convened by the Association of Occupational and Environmental Clinics (AOEC), at the request of the National Institute for Occupational Safety and Health (NIOSH), developed a Knowledge Resource for a clinical decision support (CDS) tool to address aspects of diabetes care that are impacted by occupational factors.1 The tool could be incorporated into electronic health record (EHR) systems in primary cares offices to assist with the recognition of work factors that can affect diabetes management. The work group included three members Katherine Kirkland, DrPH, Laura Welch, MD, and Anna Allen, MD, MPH, and two participants from NIOSH:, Douglas Trout, MD, MHS, and Sherry Baron, MD, MPH.
Reasons for focus on diabetes in the Primary Care setting
Work factors can affect diabetes management.2 Poor diabetes management can compromise a workers’ ability to perform their job duties. Among adults aged 44–64, 16.2% have either diagnosed or undiagnosed diabetes.3 In 2012, diabetes was estimated to cost $245 billion in direct and indirect costs. The direct medical costs were 2.3 times higher for those with diabetes. There was a calculated cost of $69 billion in disability, work loss and premature death for those with diabetes. One study by Stewart, et al, estimated a $3.65 billion/year in lost productivity time (LPT) due to diabetic neuropathy.4
Standardized medication, activity and food regimens are the standard of care to regulate blood glucose. This may not be possible if there is no place to store medication or food, and breaks are not regular. Davila et al. found that adults working over 40 hours per week were more likely to have suboptimal glycemic control (HbA1c level) compared to those working 20 hours or less. Factors such as time constraints and the negative impact of shift work on diet could explain these findings.5 Shift work and extended work shifts can complicate diabetes management by introducing nutrients counter to circadian signals that control glucose metabolism. In addition, physical activity levels, both work-related and leisure-time, vary considerably across occupations and may have an impact on glycemic control.2,3,6
Diabetes can affect multiple body systems that can influence work capability. Blood glucose fluctuations can cause changes in mental status, possibly interfering with decision-making activities and coordination. Diabetes (Type 1 and 2) is associated with decreased vasodilator response and sweat gland response. Thermoregulation can be further inhibited by obesity and medications. Many medications use to treat diabetes and its complications can cause increased heat production or decreased heat loss7,8.
Long-term sequela can include cataracts, kidney disease and heart disease. Cataracts can cause difficulty in poor lighting conditions. The medications to treat kidney and heart disease can further impact temperature regulation and alertness. Special considerations for personal protective equipment, such as protective footwear, may be important for those with diabetic neuropathies. One study comparing white collar and blue collar workers found that blue collar workers were more likely to require protective footwear and were at higher risk for having diabetic neuropathy.3
A number of studies have systematically examined the efficacy of EHRs and CDS to improve diabetic control. EHR’s with diabetic CDS support can contribute to positive changes in clinician performance and glycemic control, especially among patients who previously had greater difficulty with control9. There are no studies of EHR CDS for diabetes and work. If a CDS tool improved management of diabetes by consideration of work related factors, the extra steps in a workflow are more likely to be accepted by medical providers.
Process of selection of the recommendations
The occupational factors determined by the work group to impact clinical care of diabetes, and could be reasonably included in an EHR CDS, were work schedules, work environmental conditions such as extreme temperatures, managing hypoglycemia in safety sensitive duties, and the application of the workplace components of the American with Disabilities Act to diabetic patients. Safety sensitive duties are those workplace activities in which impairment of mental status or coordination could lead to injury to oneself or others.1
The American Diabetes Association maintains recommendations for diabetes management.10 General guidelines for approaching the impact of diabetes on employment, including how an assessment should be performed and what accommodations may be needed, such as employment in safety sensitive occupations.11 There are no evidence-based guidelines related to workplace factors or evidence to support specific interventions in the workplace for persons with diabetes. Given this situation, and our review of the literature, the work group developed recommendations in consideration of validated diabetes management principles addressing issues workers with diabetes routinely encounter in the workplace: shift work, ability to take breaks, exposure to heat or temperature extremes, ability to eat/drink/take medication as needed, and level of physical activity.12
EVALUATING OF EVIDENCE/STRENGTH OF THE RECOMMENDATIONS
Concern about the health effects of shift work on diabetes management has been discussed since the 1970s.13 The literature indicates a correlation between diabetes and shiftwork especially in men and those working rotating shifts14. Studies have shown that shift work can impact metabolic factors important in diabetes care.15,16,17 A patient that is employed in nontraditional work shifts may have difficulty managing blood glucose due to variation of eating times, circadian rhythm signaling and determining when to take medications.18,19,20
Hypoglycemia is important for those in safety sensitive work activities. Sudden incapacitation due to a decrease in blood glucose can put the patient and those around him or her in danger. The American Diabetes Association characterizes hypoglycemia via a list of symptoms. The most important for safety sensitive jobs are confusion, including delirium; lightheadedness or dizziness; sleepiness; blurred/impaired vision; seizures and unconsciousness.9 Temperature extremes, both hot and cold, can put an employee with diabetes at risk due to microvascular and neurologic changes.6,7 This impedes the ability thermo-regulate effectively in hot environments. Decreased blood flow from cold temperatures in combination with decreased sensation in the extremities can place the patient at risk for trauma.
Our recommendations also included information about the American with Disabilities Act to educate the provider, the patient and possibly the employer on rights and responsibilities. The patient has the right to reasonable accommodations but if the patient cannot perform the essential job tasks, the employer also has rights. These are fully explained in Questions & Answers about Diabetes in the Workplace and the Americans with Disabilities Act.21 Complete details about how the authors conducted their literature search and evaluated the research are found in the Final knowledge report for the Work and Diabetes Subject Matter Expert Group, which is being published as a companion to this article.1
RECOMMENDED INTERVENTION
Decision to use a trigger HbA1C level
After review of the literature and discussion of common work flow issues in primary care practices, the work group decided to develop recommendations that would be triggered primarily for those patients with poorly controlled disease. While the work group considered using diagnosis codes and existing occupational information from the EHR, this approach would have required an EHR to already have accessible and structured (ie, coded) occupational health information in the system and may also cause notification fatigue for providers who may have many patients with well controlled diabetes.
The recommendation to maintain all diabetics at a level of HbA1c ≤ 7 is based on the National Institute of Diabetes, Digestive and Kidney Diseases (NIDDK) which defines an HbA1c of 6.5 or above as diabetes22. However, anecdotal evidence based on discussions with primary care providers (PCP) determined that this would be a limiting factor in the usefulness of most EHR CDS due to notification fatigue. The work group decided to use HbA1C≥8.0 and hypoglycemia as triggers to activate the CDS tool since those patients could benefit most from education about diabetes and the workplace. The final recommendations were made to enable the PCP to direct efforts to patients most in need of education. Ideally, the level of HbA1C that triggers the CDS could be altered based on a clinic’s specific needs and patient population.
Lab data, such as HbA1C and the plasma glucose, in EHR systems can be used an objective measurement of glucose control that can trigger the CDS. If there is evidence of hypoglycemia either from lab data or patient provided information, the diagnosis could be added to the patient problem list, triggering the hypoglycemia CDS. Therefore, the work group determined that the target populations for this project were patients at primary care clinics that had a significant number of patients with diabetes. The primary criterion is that the patient be currently working. There are two groups of employed patients specifically targeted for this project: those patients with elevated HbA1C, and those patients demonstrating symptomatic or serious hypoglycemia, with ‘serious’ defined as a situation requiring help from a third party and ‘symptomatic’ defined as an event during which typical symptoms of hypoglycemia are accompanied by a measured plasma glucose of less than or equal to 70mg/dL.23
If/then statements
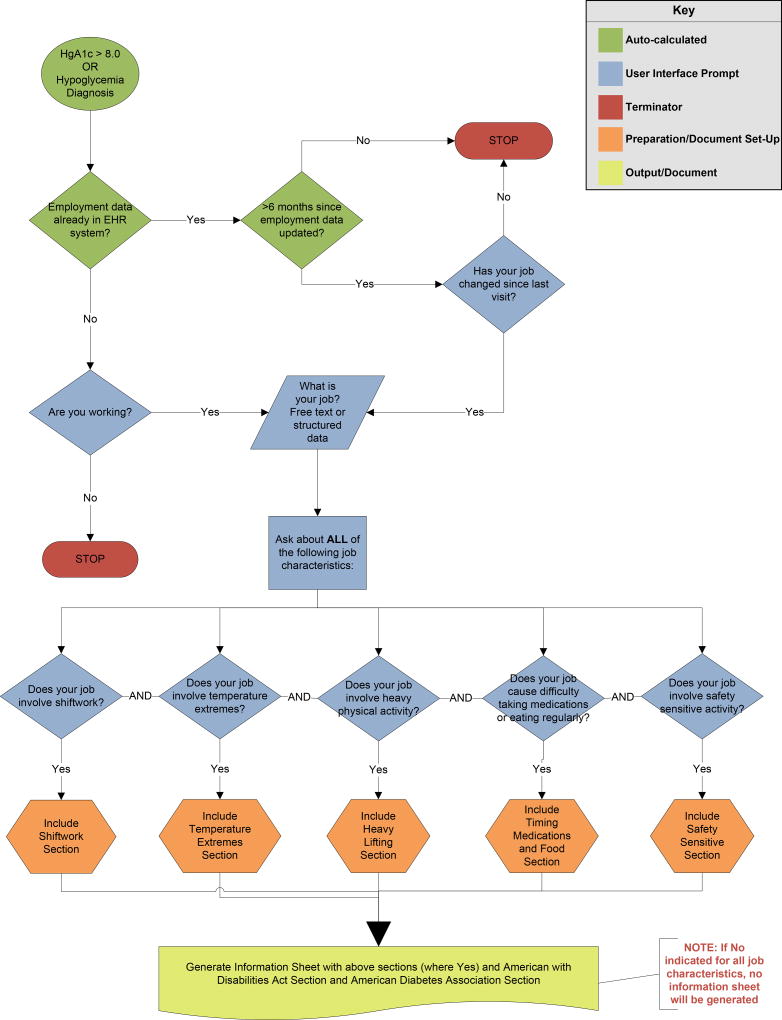
Once the CDS is triggered by evidence of elevated HGA1C or hypoglycemia, the clinicians would be prompted to ask about the work-related risk factors identified by the work group. The clinician does not have to ask the patient about each job feature individually, but could pose a comprehensive question and gather ‘yes’ responses to any given job feature. The yes responses would then trigger patient and provider information.
If the CDS is triggered, the PCP should ask about relevant features of current job(s) that are recognized to impact diabetes management: shift work, ability to take breaks, exposure to heat or temperature extremes, ability to eat/drink/take medication as needed, and level of physical activity. As noted above in the section: Development of clinical criteria and potential interventions the PCP does not have to get detailed information about each job feature. The CDS will provide the information and the PCP will be prompted to either print out materials based on the CDS recommendations or provide the patient with pre-printed materials.
To reduce notification fatigue, programming should be in place such that this CDS does not appear if the patient has been asked about these job features within the past 6 months. The patient information should be available to be printed outside of the CDS triggers for unexpected situations.
The IF/THEN statement behind the CDS is:
-
IF:
Patient demonstrates ‘not-at-target’ diabetes (elevated HbA1C ≥ 8 is recommended)
-
OR
Patient demonstrates symptomatic or serious hypoglycemia
-
THEN:
Clinicians should ask about relevant features of current job(s) that are recognized to impact diabetes management: shift work, ability to take breaks, exposure to heat or temperature extremes, ability to eat/drink/take medication as needed, and level of physical activity. If the patient answers “yes” to any of the features, then the CDS would populate a menu of educational materials to educate/counsel concerning management based on the relevant job characteristics. The clinician could click on one or more materials to be printed for the patient. The work group’s recommended educational materials is found in the full technical report21, though each clinic may want to tailor this information to the language, literacy and other characteristics of their clinic population.
CASE EXAMPLE
A 35-year-old man with a history of diabetes, hypertension and hyperlipidemia presents for an annual reevaluation. He brings in his blood glucose readings which indicate poor diabetic control with multiple readings above 200 mg/dl (maximum 294 mg/dl), but no low blood glucose readings or signs or symptoms of hypoglycemia. He works at the local chemical plant as a process engineer. Other clinical information includes HbA1c of 9.6 three months ago and 9.0 last week. The patient is taking oral hypoglycemic medications. In this scenario the HbA1c ≥8 will trigger the CDS.
The CDS will lead the provider to ask the patient if he is working, what his job is, whether his job involves shift work, temperature extremes, or heavy physical activity, and whether his job causes difficulties in allowing him to eat and take medications regularly. In this case, the patient indicates that his job does involved shift work – he alternates between day shift and night shift and finds it difficult to adjust his medication during night shifts.
Based on that type of information (above) provided during the visit, the CDS will generate an Information Sheet which will include level-appropriate (6th grade reading level ) material explaining issues related to managing diabetes while performing shift work, along with steps that can be taken to assist in diabetes control, and specific recommendations to aid in control of diabetes.
The information sheet will include further reading for patients (including primarily information from the American Diabetes Association and information concerning the Americans with Disabilities Act) and further reading for physicians.
A graphical representation of the process flow is available in the Final Knowledge Report for the Work and Diabetes Subject Matter Expert Group1.
Limitations
The CDS was designed to offer background information to providers to support the educational material presented in the patient handout. More detailed information about the workplace factors, which may affect clinical care for diabetics, is not always covered in depth in primary care training. The references allow providers to refresh or learn about occupational medicine concepts. These reference pages could offer the opportunity to increase interest in occupational factors and medical care beyond diabetes
One concern of the work group was the effect it may have on a patient’s job status. While the Americans with Disabilities Act provides legal protections (see technical report for details of the ADA)1 the reality is that some employers will find any required work accommodation as a signal to find reasons to dismiss the employee. Review of the EEOC website does not reveal which complaints are due to diabetes but does show a broad range and significant number of employment cases resolved by the EEOC21. However, if the patient and provider are aware, medication selection, timing and dosing might be adjusted to workplace requirements.
Another job-related risk is that a patient can be designated as unfit to perform safety sensitive activities which can impact employment options and salary. However, if the patient does pose a potential risk, there is an ethical responsibility of the clinician to protect the not only the patient but also co-workers, and the public. This issue could be a stressor in the physician-patient relationship and could require dedicated time to explain to the patient or consultation with an occupational medicine specialist.
Lastly, while the information may be useful, if the busy PCP feels it is taking too much time with minimal benefit, they may disregard the CDS any time it appears. However, properly programmed workflow with adequate PCP education, should help both the medical provider and patient develop better awareness of the relationship between work and diabetes control Materials will need to be developed that meet the literacy levels of patients and inform primary care providers about each of these issues without significantly interfering with patient care time. Some of this information can be integrated into existing educational information including information on food intake and medication use.
CONCLUSION
The development process for the clinical decision support tool was an iterative process that required input from a variety of experts over the year. The group initially started out with grand goals to discuss not only short term management but also long-term effects such as cataracts, kidney disease, and cardiovascular risk factors. As we began to try to quantify the individual factors and visualize how to present the decision matrix, it became evident that we needed to curb our ambitions for both the provider and those that would have to implement the programming.
With EHR systems, patient outcomes can be extracted and analyzed if an appropriate data field is selected. Although HgA1c and glucose level does not represent the whole of the patient, they offer a disease-specific result that can be monitored. We believe EHR systems have the potential to offer specialized, directed medical knowledge that can improve patient outcomes. In this case, the goal is to improve the health and safety of workers with diabetes by addressing factors that may sometimes be overlooked. We look forward to feedback from participating clinics on the effectiveness of this effort.
Diabetes CDS Decision Logic Flowchart
Acknowledgments
NIOSH co-lead SME, Sherry Baron MD, MPH – NIOSH secondary SME, Other NIOSH: Stacey Marovich, Eileen Storey, MD, MPH
References
- 1.Final knowledge report for the Diabetes Subject Matter Expert Group. Submitted by the Diabetes Subject Matter Expert Group: Laura Welch, MD (chair); Anna Allen, MD, MPH; Douglas Trout, MD, Sherry Baron, MD, MPH; Katherine Kirkland, DrPH, MPH. December 2015. 2015 Produced under contract 212-2014-M-59011. available at www.acoem.org/ (web site TBD)
- 2.Lee S-M, Koh D, Chui WK, Sum C-F. Diabetes Management and Hypoglycemia in Safety Sensitive Jobs. Safety and Health at Work. 2011;2(1):9–16. doi: 10.5491/SHAW.2011.2.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Diabetes Statistics Report. 2014 https://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf.
- 4.Stewart WF, Ricci J, Chee E, Hirsch A, Brandenburg N. Lost Productive Time and Costs Due to Diabetes and Diabetic Neuropathic Pain in the US Workforce. J Occup Environ Med. 2007 Jun;49(6):672–9. doi: 10.1097/JOM.0b013e318065b83a. [DOI] [PubMed] [Google Scholar]
- 5.Davila EP, Florez H, Trepka MJ, Fleming LE, Niyonsenga T, Lee DJ, Parkash J. Long work hours is associated with suboptimal glycemic control among US workers with diabetes. Am. J. Ind. Med. 2011;54:375–383. doi: 10.1002/ajim.20923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Church TS, Blair S, Cocreham S, Johannsen N, Johnson W, Kramer K, Mikus C, Myers V, Nauta M, Rodarte R, Sparks L, Thompson A, Earnest C. Effects of Aerobic and Resistance Training on Hemoglobin A1c Levels in Patients With Type 2 Diabetes A Randomized Controlled Trial. JAMA. 2010 Nov 24;304(20):2253–2262. doi: 10.1001/jama.2010.1710. Erratum in JAMA. 2011 Mar 2;305(9):892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yardley JE, Stapleton JM, Sigal RJ, Kenny GP. Do heat events pose a greater health risk for individuals with type 2 diabetes? Diabetes Technol Ther. 2013 Jun;15(6):520–9. doi: 10.1089/dia.2012.0324. Epub 2013 Mar 26. Review. [DOI] [PubMed] [Google Scholar]
- 8.Heimhalt-El Hamriti M, Schreiver C, Noerenberg A, Scheffler J, Jacoby U, Haffner D, Fischer DC. Impaired skin microcirculation in paediatric patients with type 1 diabetes mellitus. Cardiovasc Diabetol. 2013 Aug 12;12:115. doi: 10.1186/1475-2840-12-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reed M, Huang J, Graetz I, Brand R, Hsu J, Fireman B, Jaffe M. Outpatient Electronic Health Records and the Clinical Care and Outcomes of Patients With Diabetes Mellitus. Ann Intern Med. 2012 Oct 2;157(7):482–489. doi: 10.7326/0003-4819-157-7-201210020-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Diabetes Association. http://www.diabetes.org/living-with-diabetes/treatment-and-care/blood-glucose-control/hypoglycemia-low-blood.html.
- 11. [accessed 10/11/2016];Recommendations of the American Diabetes Association: Diabetes and Employment, Diabetes Care. 2014 Jan;37(1) http://care.diabetesjournals.org/content/37/Supplement_1/S112. [Google Scholar]
- 12. [accessed10/11/2016];Recommendations of the National Quality Forum. http://www.qualityforum.org/setting_priorities/improving_healthcare_quality.aspx.
- 13.Winget Charles M, PhD, Hughes Lewis, PhD, LaDou Joseph., MD Physiological Effects of Rotational Work Shifting: A Review. J Occup Med. 1978 Mar; doi: 10.1097/00043764-197803000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Gan Y, Yang C, Tong X, Sun H, Cong Y, Yin X, Li L, Cao S, Dong X, Gong Y, Shi O, Deng J, Bi H, Lu Z. Shift work and diabetes mellitus: a meta-analysis of observational studies. Occup Environ Med. 2014 Jul 16; doi: 10.1136/oemed-2014-102150. pii: oemed-2014-102150. doi: 10.1136/oemed-2014-102150. [Epub ahead of print] Review. [DOI] [PubMed] [Google Scholar]
- 15.Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A. 2009 Mar 17;106(11):4453–8. doi: 10.1073/pnas.0808180106. Epub 2009 Mar 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004 Dec 7;141(11):846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 17.Schiavo-Cardozo D, Lima MM, Pareja JC, Geloneze B. Appetite-regulating hormones from the upper gut: disrupted control of xenin and ghrelin in night workers. Clin Endocrinol (Oxf) 2013 Dec;79(6):807–11. doi: 10.1111/cen.12114. Epub 2013 Apr 5. [DOI] [PubMed] [Google Scholar]
- 18.Roden M, Koller M, Pirich K, Vierhapper H, Waldhauser F. The circadian melatonin and cortisol secretion pattern in permanent night shift workers. Am J Physiol. 1993 Jul;265(1 Pt 2):R261–7. doi: 10.1152/ajpregu.1993.265.1.R261. [DOI] [PubMed] [Google Scholar]
- 19.Kalsbeek A, la Fleur S, Fliers E. Circadian control of glucose metabolism. Mol Metab. 2014 Mar 19;3(4):372–83. doi: 10.1016/j.molmet.2014.03.002. eCollection 2014 Jul. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Atkinson G, Fullick S, Grindey C, Maclaren D. Exercise, energy balance and the shift worker. Sports Med. 2008;38(8):671–85. doi: 10.2165/00007256-200838080-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. [Accessed 3/31/2017];U.S. Equal Employment Opportunity Commission. https://www.eeoc.gov/laws/types/diabetes.cfm.
- 22. [Accessed 3/31/2017];National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis/a1c-test.
- 23.Seaquist ER1, Anderson J, Childs B, Cryer P, Dagogo-Jack S, Fish L, Heller SR, Rodriguez H, Rosenzweig J, Vigersky R. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013 May;36(5):1384–95. doi: 10.2337/dc12-2480. Epub 2013 Apr 15. [DOI] [PMC free article] [PubMed] [Google Scholar]