Abstract
The nigrostriatal and mesocorticolimbic dopamine networks regulate reward-driven behavior. Regional alterations to mesolimbic dopamine D2/3 receptor expression are described in drug-seeking and addiction disorders. Parkinson's disease (PD) patients are frequently prescribed D2-like dopamine agonist (DAgonist) therapy for motor symptoms, yet a proportion develop clinically significant behavioral addictions characterized by impulsive and compulsive behaviors (ICBs). Until now, changes in D2/3 receptor binding in both striatal and extrastriatal regions have not been concurrently quantified in this population. We identified 35 human PD patients (both male and female) receiving DAgonist therapy, with (n = 17) and without (n = 18) ICBs, matched for age, disease duration, disease severity, and dose of dopamine therapy. In the off-dopamine state, all completed PET imaging with [18F]fallypride, a high affinity D2-like receptor ligand that can measure striatal and extrastriatal D2/3 nondisplaceable binding potential (BPND). Striatal differences between ICB+/ICB− patients localized to the ventral striatum and putamen, where ICB+ subjects had reduced BPND. In this group, self-reported severity of ICB symptoms positively correlated with midbrain D2/3 receptor BPND. Group differences in regional D2/3 BPND relationships were also notable: ICB+ (but not ICB−) patients expressed positive correlations between midbrain and caudate, putamen, globus pallidus, and amygdala BPNDs. These findings support the hypothesis that compulsive behaviors in PD are associated with reduced ventral and dorsal striatal D2/3 expression, similar to changes in comparable behavioral disorders. The data also suggest that relatively preserved ventral midbrain dopaminergic projections throughout nigrostriatal and mesolimbic networks are characteristic of ICB+ patients, and may account for differential DAgonist therapeutic response.
SIGNIFICANCE STATEMENT The biologic determinants of compulsive reward-based behaviors have broad clinical relevance, from addiction to neurodegenerative disorders. Here, we address biomolecular distinctions in Parkinson's disease patients with impulsive compulsive behaviors (ICBs). This is the first study to image a large cohort of ICB+ patients using positron emission tomography with [18F]fallypride, allowing quantification of D2/3 receptors throughout the mesocorticolimbic network. We demonstrate widespread differences in dopaminergic networks, including (1) D2-like receptor distinctions in the ventral striatum and putamen, and (2) a preservation of widespread dopaminergic projections emerging from the midbrain, which is associated with the severity of compulsive behaviors. This clearly illustrates the roles of D2/3 receptors and medication effects in maladaptive behaviors, and localizes them specifically to nigrostriatal and extrastriatal regions.
Keywords: dopamine, impulse control disorder, impulsive compulsive behaviors, mesocorticolimbic, Parkinson's disease, positron emission tomography
Introduction
Altered dopaminergic signaling in the nigrostriatal and mesolimbic circuits is the focus of many investigations of the pathophysiologic basis of addictive behaviors, such as drug seeking, compulsive gambling, and binge eating (Haber and Knutson, 2010). Within these networks, dopamine release from ventral midbrain projections is implicated in both the development and maintenance of addiction (Pettit et al., 1984; Yin et al., 2004). Reductions in striatal dopamine D2-like (D2/D3) receptor binding are consistently observed in patients with alcohol, cocaine, methamphetamine, opiate, and nicotine abuse (Trifilieff and Martinez, 2014). Moreover, ventral striatal decreases in D2/3 receptor expression are associated with impulsive behaviors, a risk factor for the development of addiction (Dalley et al., 2007), whereas decrements in dorsal striatal D2/3 receptor levels are linked to established patterns of addictive behavior (Nader et al., 2006). D2/3 receptors are also important in the ventral midbrain, where decreased D2/3 (auto)receptor binding is associated with greater impulsivity in healthy humans (Buckholtz et al., 2010).
Pramipexole and ropinirole, D3 preferring D2/3 agonists (DAgonists), produce improvements in the motor symptoms of Parkinson's disease (PD; Piercey, 1998). However, these D2/3-preferring medications can also induce impulsive and compulsive behaviors (ICBs), distinguished by an aberrant focus on reward-driven activities including gambling, shopping, sex, eating, and hobbies (Voon et al., 2007), as well as heightened novelty seeking (Voon et al., 2011). The causal nature of this effect is emphasized by the clinical finding that discontinuation or reduction of DAgonist in ICB+ individuals can result in symptom improvement (Claassen et al., 2013). Due to the receptor-level specificity of DAgonist compounds, investigation of mesocorticolimbic D2/3 levels in PD patients with ICB symptoms provides an opportunity to examine the role of D2/3 receptors in maladaptive reward-seeking behaviors in PD patients.
Dopaminergic projections from the ventral midbrain to striatal, limbic, and cortical regions in the brain reward circuit are critical for reward network function (Haber and Knutson, 2010). A small number of PET studies using [11C]raclopride (Steeves et al., 2009) and [11C]-(+)-PHNO (Payer et al., 2015) have reported reduced baseline D2/3 receptor levels in the ventral striatum in ICB+ patients; this finding may be due to either decreased ventral striatal D2/3 receptor expression, or increased ventral striatal extracellular dopamine levels, which could in theory reduce the number of available D2/3 receptors. Due to its moderate affinity for the D2/3 receptor, [11C]raclopride provides an estimate of striatal D2/3 receptor levels but has not typically been used to estimate extrastriatal D2/3. [11C]-(+)-PHNO, a higher affinity D3-preferring D2/3 agonist radioligand, can be used to estimate D2/3 receptor levels in striatal and select extrastriatal regions (a relatively low signal-to-noise ratio in most cortical regions restricts extrastriatal use; Hall et al., 1989; Egerton et al., 2010). One [11C]FLB-457 study noted increased binding in the anterior cingulate cortex and midbrain of ICB+ patients during a control task and gambling task, respectively (Ray et al., 2012). However, although [11C]FLB-457 can be used to estimate extrastriatal D2/3 levels, it does not provide accurate binding estimates in the striatum (Farde et al., 1997). To date, no single study of ICBs in PD patients has concurrently evaluated D2/3 receptor levels in the midbrain, striatal, limbic, and cortical regions of the reward circuit, or the relationships between regional D2/3 mediated neurotransmission in this network.
An approach capable of concurrently evaluating striatal and extrastriatal areas could provide a greater understanding regarding the interaction between important components of the reward network (including the ventral midbrain, striatum, and the orbitofrontal, prefrontal, and anterior cingulate cortices). [18F]fallypride is a high-affinity D2/3 radioligand that can provide accurate estimates of binding in both striatal and extrastriatal regions, allowing for quantification of dopamine D2/3 receptor levels [i.e., nondisplaceable binding potential (BPND)] throughout the mesocorticolimbic network (Kessler et al., 2000; Mukherjee et al., 2002). We assessed a cohort of PD patients (with and without ICB and matched for disease severity) to examine the localization of D2/3 BPND differences, thus determining the relationship between D2/3 receptor levels and self-reported severity of reward-based behaviors. We hypothesized that D2/3 BPND reductions in ICB+ patients would localize to the ventral striatum, with distinctions in the midbrain and anterior cingulate cortex (Steeves et al., 2009; Ray et al., 2012; Payer et al., 2015). Finally, in an effort to examine putative differences in the reward-network between groups and to better understand the interaction between the dopaminergic system in the midbrain and in terminal field locations, we evaluated the relationship between midbrain D2/3 receptor expression and receptor expression throughout the nigrostriatal and mesolimbic networks.
Materials and Methods
Participants.
Subjects (n = 35; sex = 11 F/24 M; age = 61.8 ± 8.5 years) were recruited from the Movement Disorders Clinic at Vanderbilt University Medical Center, and provided written, informed consent in accordance with the Vanderbilt Institutional Review Board. We screened patients diagnosed with idiopathic PD (meeting UK Brain Bank criteria), who were taking DAgonist medication (including pramipexole, ropinirole, and rotigotine) with or without concomitant levodopa therapy. A clinical determination of active ICB symptoms was based on behavioral interview with the patient care partner (Mestre et al., 2013). ICBs were defined as clinically problematic compulsive behaviors with onset following DAgonist administration according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, 2000), with specific attention toward the previously reported categories of compulsive shopping, eating (with modified DSM-IV-TR criteria for binge-eating disorder including overeating as well as episodes of binge-eating), hypersexuality, gambling, and hobbyism (Voon et al., 2007; Weintraub et al., 2012). Before the interview, participants completed the Questionnaire for Impulsive-Compulsive Disorders in Parkinson's Disease-Rating Scale (QUIP-RS). As per the methods of Weintraub et al. (2009), answers to QUIP-RS items could be used to guide the clinical interview, but were not used to singularly define an explicit cutoff mark in the diagnosis of ICB. As a result, certain patients within the ICB− group may have expressed an increased proclivity toward shopping, eating, sexual behavior, gambling, or hobbyism relative to others in the same group; however, these behaviors were not deemed clinically problematic in these subjects. Although previous investigations of ICB have often concentrated on compulsive gambling, recruitment efforts were not limited to a single subcategory, and reflected the distribution in the local population.
Patients completed the self-reported Movement Disorders Society-United Parkinson's Disease Rating Scale (MDS-UPDRS) part II (an assessment of the impact of PD on activities of daily living; Goetz et al., 2008; Weintraub et al., 2012). Cognitive impairment was assessed with the Montreal Cognitive Assessment (MoCA), and premorbid intelligence screened using the American version of the National Adult Reading Test (AMNART; Grober and Sliwinski, 1991; Nasreddine et al., 2005). Depression symptoms were screened using the Center for Epidemiological Studies Depression Scale Revised (CESD-R; Radloff, 1977). Patients were excluded if (1) they had an implanted deep brain stimulator; (2) were prescribed psychoactive medications that could alter dopamine receptor availability; (3) were demented, or suffered from comorbid neuropsychiatric, cerebrovascular, or cardiovascular disease; (4) scored <22 in the MoCA (to exclude possible cognitive impairment); or (5) had contraindications for MRI or PET. Levodopa and DAgonist dosages were converted to levodopa-equivalent dose using accepted criteria (Tomlinson et al., 2010). From the pool of individuals who had completed the initial screening visit, subjects were selectively enrolled in the imaging portion of the study based on the determination of ICB status and matched by UPDRS-II severity, to ensure size-matched groups. From the 90 PD patients who had completed the initial screening and behavioral interview, 17 ICB+ and 18 ICB− patients were ultimately included in the study.
The structural MRI and [18F]fallypride PET scan were completed in the off-dopamine (levodopa and DAgonist) state. Of note, in the Off condition, patients refrained from all dopaminergic medications (washout was at least 40 h for DAgonist and 16 h for Levodopa) before assessments, as this period is sufficient to eliminate DAgonist effects while minimizing patient discomfort (the half-life of levodopa and immediate-release DAgonists are ∼1.5 and 6 h respectively; Fabbrini et al., 1987; Tompson and Oliver-Willwong, 2009).
Magnetic resonance imaging.
Structural MRI scans were completed before PET scans. Patients were scanned at 3.0T (Philips) using body coil transmission and 8-channel SENSE reception. All underwent a multimodal imaging protocol consisting of the following scans: (1) T1-weighted (MPRAGE; spatial resolution = 1 × 1 × 1 mm3; TR/TE = 8.9/4.6 ms), and (2) T2-weighted FLAIR (spatial resolution = 1 × 1 × 1 mm3; TR/TE = 4000/120 ms).
Fallypride PET data acquisition.
[18F]fallypride [(S)-N-[(1-allyl-2-pyrrolidinyl)methyl]-5-(3[18F]fluoropropyl)-2,3-dimethoxybenzamide] was synthesized in the radiochemistry laboratory adjacent to the PET unit, in alignment with the synthesis and quality control procedures outlined by U.S. Food and Drug Administration Investigational New Drug Applicaiton 47245 and 120035. Data were collected on a GE Discovery STE PET/CT scanner. Serial scan acquisition began simultaneously with a 5.0 mCi slow bolus injection of [18F]fallypride (specific activity >3000 Ci/mmol). Arterial blood sampling was not performed. CT scans were collected before each of the three emissions scans for the purpose of attenuation correction. Together, the scans lasted ∼3.5 h with two breaks of 15–20 min (beginning ∼70 and 135 min after the beginning of the scan, respectively) included for patient comfort
Fallypride PET data processing.
Following attenuation correction and decay correction, serial PET scans were coregistered with each other using the Statistical Parametric Mapping software (SPM8, Wellcome Trust Centre for Neuroimaging; http://www.fil.ion.ucl.ac.uk/spm/software/) to correct for motion across scanning periods with the last dynamic image of the first series as the reference image. The mean PET image produced by realignment was then coregistered to the subject's corresponding high-resolution T1 MRI image using FSL's FLIRT with 6 degrees of freedom (FSL v5.0.2.1, FMRIB). Regions-of-interest (ROIs), including the caudate, putamen, globus pallidus, ventral striatum, amygdala, midbrain, thalamus, and cerebellum, were manually segmented on the T1-weighted MRI scans by a neuroradiologist (R.M.K.) and neurologist (D.O.C.) experienced in PET and MRI data analysis, and transferred to the coregistered PET images through the FLIRT FSL transformation matrix. These regions were selected due to their importance in the nigrostriatal and mesolimbic circuits (Haber and Knutson, 2010), implicating them as areas where ICB-related differences in dopaminergic signaling could be evident. Manual segmentation methods followed established anatomical criteria, capturing the central portion of the selected region to gather the most representative sample and avoid partial volume effects, and were applied so as to avoid the potential confound of intersubject structural variability.
The caudate, putamen, and globus pallidus were manually drawn on axial slices ∼2–12 mm above the ACPC line. The ventral striatum was segmented on coronal slices with the criteria of Mawlawi et al. (2001). The amygdala can be identified on axial slices 6–20 mm below the ACPC line, 12–28 mm lateral to the midline, and 2–12 mm behind the plane of the anterior commissure (Schaltenbrand and Wahren, 1998). To avoid contamination by signals from striatal regions with high BPND because of partial volume averaging, amygdala ROIs were defined 10–16 mm beneath the ACPC plane. The midbrain was drawn on axial slices in the ventral midbrain 9–14 mm below the ACPC line, and the thalamus was segmented 2–12 mm above the ACPC line (Schaltenbrand and Wahren, 1998). The cerebellar ROI was drawn centrally within the structure to avoid partial voluming of midbrain or cortical signal, and contained an approximately equal distribution of gray and white matter. To account for potentially divergent structure size between groups, ROI volumes were collected and preserved for statistical analysis. For voxelwise analyses, subject-space BPND images were registered to Montreal Neurological Institute space using FSL's FNIRT (FSL v5.0.2.1, FMRIB).
Regional DA D2/3 levels were estimated using the simplified reference region method (Lammertsma et al., 1996) performed in PMOD software (PMOD Technologies) to measure [18F]fallypride binding potential (BPND; the ratio of specifically bound [18F]fallypride to its nondisplaceable concentration as defined under equilibrium conditions). Voxelwise estimates were generated using a published basis function fitting approach (Gunn et al., 1997) conducted in the PXMOD module of PMOD. The rate constants were specified by the user as k2a minimum = 0.006 min−1 and k2a maximum = 0.6 min−1. The cerebellum was selected as the reference region due to its relatively limited expression of D2/3 receptors in the cerebellum (Camps et al., 1989), it was selected as the reference region (Kessler et al., 2009). ROI BPND values were determined by evaluating the average BPND within an ROI overlaid on the subject-space voxelwise map, which was generated in the previous PET processing steps.
Experimental design and statistical analysis.
Group differences between ICB+ (n = 17; sex = 11 M/6 F) and ICB− subjects (n = 18; sex = 13 M/5 F) in demographic and clinical parameters, ROI volume, and the proportion of levodopa daily dose (LEDD) accounted for by DAgonists were evaluated using Mann–Whitney U tests. We also examined whether scores on the QUIP-RS were significantly correlated with LEDD for either group. Sex and DAgonist regimen differences were evaluated with a χ2 test. To test the hypothesis that ICB+ patients have different dopamine D2/3 receptor expression in striatal and extrastriatal areas, mean group regional [18F]fallypride BPND was analyzed via a general linear regression model (GLM), where within-ROI BPND was the dependent variable and ICB status was the primary independent variable. Age was included as a covariate, due to previous evidence of an effect of age on D2/3 receptor status (Mukherjee et al., 2002). UPDRS-II was also specified as a covariate, as PD severity has been shown to influence D2/3 binding (Kaasinen et al., 2000). UPDRS-II was selected because of past indications that it accurately tracks disease severity, and the fact that measurements of short term motor symptoms fluctuate and are highly sensitive to medication status (Harrison et al., 2009). Although study design led to equivalent age and UPDRS-II values between groups, these factors were included as covariates to account for residual confounding effects. A separate model was used to test mean differences in each ROI. A voxelwise analysis completed using SPM8 assessed group differences in D2/3 BPND across cortical regions, given that this was an exploratory analysis that sought to capture distinctions in subregions of larger structures. Age was included as a covariate in this analysis. Subcortical areas were excluded through the use of an explicit cortical mask in the voxelwise analysis, to improve statistical power and to ensure that the considerable difference in D2/3 density between the basal ganglia and cortex did not serve as a confounding factor (Joyce et al., 1991). Significance criteria consisted of an uncorrected p < 0.001, and multiple-comparisons correction was accomplished by controlling cluster-level False discovery rate (FDR) at 0.05.
A secondary analysis investigated associations between D2/3 receptor binding in each ROI and scores on the QUIP-RS, a clinical measure of ICB severity. A partial Pearson's correlation was used to examine these relationships, specifying age and UPDRS-II score as covariates. As an exploratory method, we examined whether the relationship between midbrain BPND and BPND in other regions differed in ICB+ patients. Because the midbrain provides key dopaminergic inputs to the nigrostriatal and mesolimbic tracts, and midbrain binding potential significantly correlates with binding potential in other components of the reward circuit (Zald et al., 2010), this analysis served to probe potential differences in dopaminergic network integrity. To accomplish this, we used a linear regression model including midbrain BPND as the dependent variable, age and UPDRS-II scores as covariates, and ICB status, BPND of the other six ROIs, and the interaction between ICB status and BPND of the other six ROIs (caudate, putamen, ventral striatum, globus pallidus, thalamus, and amygdala) as independent variables. To avoid overfitting, the first principal component of age and UPDRS-II was used as a single covariate. A separate model was used for the caudate, putamen, ventral striatum, globus pallidus, and thalamus, where the variables of non-midbrain ROI BPND and interaction between group status and non-midbrain ROI BPND were present for one ROI at a time in a pairwise manner. For ROIs where a significant interaction was observed, midbrain-ROI correlations were examined using a Pearson's partial correlation test with age and UPDRS-II as covariates. FDR was controlled at 0.1 to correct for multiple comparisons in the ROI-based GLM and correlation analyses, and all reported results survived this correction threshold. All analyses were performed using SPSS Statistics 24 (IBM) and R (R Foundation for Statistical Computing, 2016).
Results
Demographic and clinical features
Demographic and clinical features for patients meeting the ICB inclusion criteria (n = 17) and those without ICBs (n = 18) are presented in Table 1. QUIP-RS scores were significantly greater in ICB+ patients after correction for multiple comparisons (p < 0.0001). DAgonist and levodopa equivalent daily doses in the On condition were comparable across groups. No significant group difference was observed in the type of DAgonist prescribed (Table 1-3) or the fraction of LEDD accounted for by DAgonist as opposed to levodopa (p = 0.99), and PET acquisition parameters were similar (Tables 1-1 and 1-2, respectively). LEDD did not significantly correlate with QUIP-RS scores for either group. Hypersexuality, compulsive eating, compulsive shopping, and hobbyism were all included among the expressed ICB subcategories; no subjects were identified as participating in pathological gambling.
Table 1.
Demographic and clinical evaluation from the two participant groups
| Variables | PD ICB− | PD ICB+ | p |
|---|---|---|---|
| N | 18 | 17 | |
| Sex, M/F | 13/5 | 11/6 | 0.72 |
| Age, years | 62.7 ± 10.1 | 60.9 ± 6.6 | 0.17 |
| Disease duration, years | 6.1 ± 4.5 | 5.7 ± 3.2 | 0.99 |
| CES-D | 15.1 ± 7.2 | 16.3 ± 10.3 | 0.89 |
| MDS-UPDRS Part II | 23.2 ± 7.7 | 20.3 ± 7.7 | 0.19 |
| QUIP-RS total | 18.1 ± 11.9 | 36.5 ± 10.1 | <0.0001* |
| ICB symptom distribution (based on semistructured behavioral interview) | |||
| Hobbyism | n/a | 12/17 | |
| Eating | n/a | 11/17 | |
| Sex | n/a | 11/17 | |
| Shopping | n/a | 4/17 | |
| Gambling | n/a | 0/17 | |
| Laterality score (− = left worse, + = right worse) | −3.1 ± 9.6 | −1.8 ± 12.0 | 0.74 |
| Dopamine replacement therapy | |||
| Total LEDD, mg/d | 693.9 ± 406.3 | 673.8 ± 440.0 | 0.69 |
| Agonist single-dose equivalent, mg/d | 135.4 ± 76.4 | 103.9 ± 65.1 | 0.19 |
Data are shown as mean ± SD.
*Indicates uncorrected p < 0.05.
No significant group difference observed in the type of DAgonist prescribed (Table 1-3) or the fraction of LEDD accounted for by DAgonist as opposed to levodopa (p = 0.99; Table 1-1). PET acquisition parameters were similar (Table 1-2).
PD ICB+, PD with symptoms consistent with ICB; PD ICB−, PD without ICBs.
PET acquisition time parameters. Download Table 1-1, DOCX file (51.3KB, docx)
PET acquisition time parameters. Acquisition parameters related to DY period start times and break lengths for both groups. Download Table 1-2, DOCX file (52.1KB, docx)
Dopamine agonist medication distribution. The number of individuals prescribed pramipexole, ropinirole, or rotigotine is listed for each group. No other dopamine agonist medications were represented, and no individual was prescribed multiple medications concurrently. No significant differences were found in the distribution of dopamine agonist medications prescribed to the ICB+ and ICB- groups, indicating that treatment differences are unlikely to be a confounding factor. Download Table 1-3, DOCX file (53.5KB, docx)
Mean regional fallypride binding potential
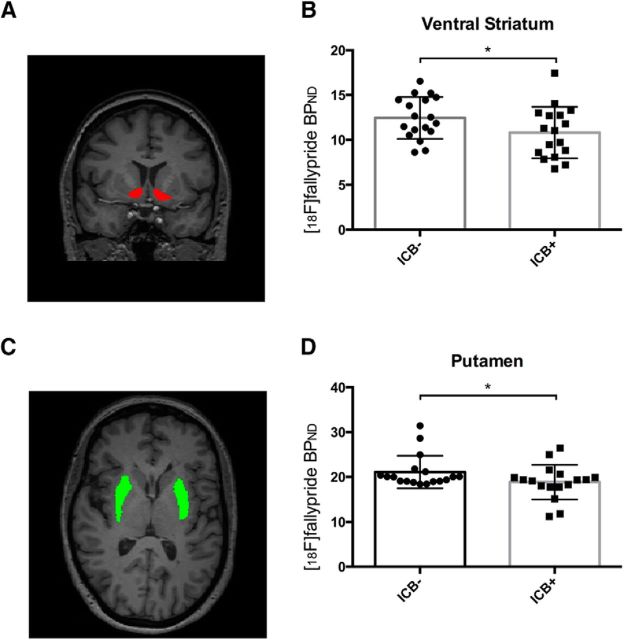
When we examined group differences in mean regional BPND using a GLM with age and UPDRS-II specified as covariates, [18F]fallypride binding was significantly lower in the bilateral ventral striatum (unstandardized B = 1.99; df = 31; p = 0.023) and putamen (unstandardized B = 2.43; df = 31; p = 0.026) of ICB+ (n = 17) compared with the ICB− (n = 18) patients, surviving FDR correction. There were no significant ROI volume differences between the ICB+ and ICB− groups; therefore ROI size was not considered as a confounding factor. The voxelwise analysis did not reveal any significant clusters in cortical regions. Figure 1 presents the age- and UPDRSII-adjusted mean regional BPNDs for the ventral striatum and putamen. Visualization of the segmentation protocol for all regions is displayed in Fig. 1-1 alongside a full description of ROI volumes and within-ROI BPND values (Figs. 1-2 and 1-3, respectively).
Figure 1.
Mean regional [18F]fallypride binding potential analysis. A, C, Representative coronal and axial slices for a single subject show an example of the manual segmentation routine for two different structures, including (A) ventral striatum and (C) putamen. B, D, Bar graphs of the mean [18F]fallypride BPND in each corresponding region, with error bars representing the SD of the mean, and scatterplots representing individual regional means. There were significant differences in mean regional BPND between the ICB+ and ICB− groups in the ventral striatum (A, B) and putamen (C, D). Visualization of the segmentation protocol for all regions is displayed in Figure 1-1 alongside a full description of ROI volumes and within-ROI BPND values (Figures 1-2 and 1-3, respectively). *p < 0.05, survival of FDR correction for multiple comparisons.
Manual segmentation protocol for [18F]fallypride binding potential analysis. (A-G) Representative coronal and axial slices for a single subject show an example of the manual segmentation routine for four different structures, including (A) caudate, (B) amygdala, (C) putamen, (D) thalamus, (E) ventral striatum, (F) midbrain, and (G) globus pallidus. Download Figure 1-1, TIF file (15.8MB, tif)
Mean ROI volumes. Mean volumes are listed alongside standard deviations, in mm3. No significant differences were found in structure size between the ICB+ and ICB- groups, indicating that structural volume is unlikely to be a confounding factor. Download Figure 1-2, TIF file (1.5MB, tif)
Mean ROI BPND. Age and UPDRS-II corrected BPND is listed for each group alongside standard error of the mean. Significant differences were found in between the ICB+ and ICB- groups in the ventral striatum and putamen. Download Figure 1-3, DOCX file (68.5KB, docx)
Relationships between regional [18F]fallypride BPNDs and clinical measures
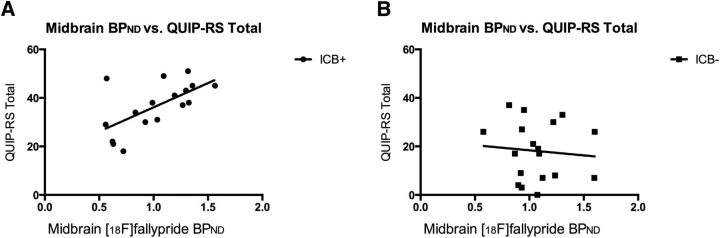
When all regional BPND values were compared with QUIP-RS scores, a significant positive correlation between midbrain BPND and QUIP-RS scores was observed for the ICB+ group (r = 0.633; df = 13; p = 0.011), surviving FDR correction. This association was not present in the ICB− group (r = −0.129; df = 13; p = 0.634). To better define whether the relationship between QUIP-RS and midbrain BPND was significantly different between groups, a post hoc analysis was conducted using a linear regression model including midbrain BPND as the dependent variable, the first principal component of age and UPDRS-II score as a covariate, and ICB status, QUIP-RS score, and the interaction between ICB status and QUIP-RS score as independent variables. A significant interaction term was present for this analysis (p = 0.009). For both groups, no significant correlation was observed between BPND and QUIP-RS in any other ROI (see Fig. 2-1 for a full listing of correlation coefficients). Figure 2 displays a scatterplot of BPND versus QUIP-RS and a representative segmentation for the midbrain.
Figure 2.
Midbrain [18F]fallypride binding potential versus QUIP-RS. A, Scatterplot of [18F]-fallypride BPND in the substantia nigra (x-axis) versus scores on the QUIP-RS (y-axis) fit with a linear regression. A significant correlation between midbrain BPND and QUIP-RS score was observed for the ICB+ group (r = 0.633, p = 0.011), but not the ICB− group (r = −0.129, p = 0.634). No significant correlation was observed between BPND and QUIP-RS in any other region. B, Representative axial slice for a single subject show an example of the manual segmentation routine for the midbrain. A full listing of correlation coefficients and p values for all analyzed ROIs is provided in Figure 2-1.
QUIP-RS and BPND correlation coefficients. The results of partial Pearson's correlation tests, corrected for age and UPDRS-II. For each ROI, the correlation coefficient and significance value is listed, separating between the ICB+ and ICB- groups. A significant correlation between QUIP-RS and midbrain BPND was found exclusively in the ICB+ group. Download Figure 2-1, DOCX file (47.5KB, docx)
Regional [18F]fallypride BPND relationships
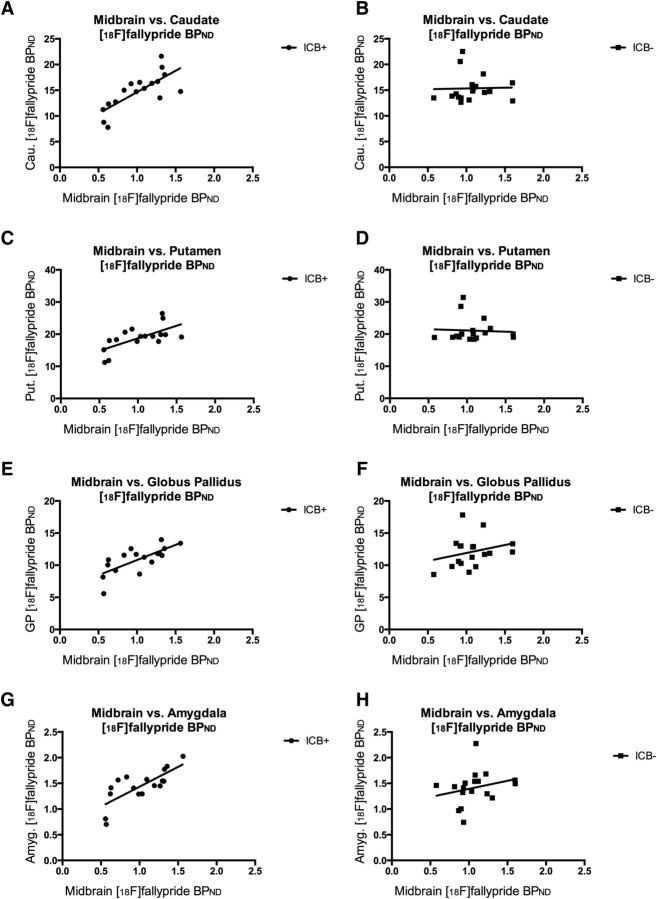
When we examined the relationship between binding in the midbrain and binding in other reward-related regions (df = 30), significant group differences in the midbrain-ROI correlation (FDR corrected; defined by significant interaction term) were observed in the caudate (unstandardized B = −0.71; p = 0.031), putamen (unstandardized B = −0.79; p = 0.024), globus pallidus (unstandardized B = −0.65; p = 0.044), and amygdala (unstandardized B = −0.60; p = 0.047). The ICB+ group expressed significant positive BPND correlations (df = 13) between the midbrain BPND and caudate (r = 0.706, p = 0.003), putamen (r = 0.589, p = 0.021), globus pallidus (r = 0.668, p = 0.007), and amygdala (r = 0.709, p = 0.003) BPNDs. There were no significant correlations (df = 14) between BPNDs in in these regions and the midbrain for the ICB− group (caudate: r = 0.001, p = 0.99; putamen: r = −0.126, p = 0.643; globus pallidus: r = 0.262, p = 0.328; amygdala: r = 0.243, p = 0.364). Figure 3 presents scatterplots of midbrain BPND versus BPND in the regions where a significant interaction term was observed for the ICB+ and ICB− groups. Scatterplots in ROIs where no significant difference was observed are presented in Fig. 3-1.
Figure 3.
Midbrain [18F]fallypride binding potential versus [18F]fallypride binding potential in other regions. A–G, Scatterplots of midbrain BPND (x-axis) versus BPND in regions where a significant group × BPND interaction was observed (y-axis) fit with a linear regression for the ICB+ and ICB− groups. This effect appeared in the (A, B) caudate (ICB+: r = 0.706, p = 0.003; ICB−: r = 0.001, p = 0.99), (C, D) putamen (ICB+: r = 0.589, p = 0.021; ICB−: r = −0.126, p = 0.643), (E, F) globus pallidus (ICB+: r = 0.668, p = 0.007; ICB−: r = 0.262, p = 0.328), and (G, H) amygdala (ICB+: r = 0.709, p = 0.003; ICB−: r = 0.243, p = 0.364), indicating a divergent BPND relationship between the structures. Figure 3-1 includes a visualization of scatterplot results, in addition to a listing of correlation coefficients and p values for ROIs that were not associated with a significant group × BPND interaction term.
Midbrain [18F]fallypride binding potential vs. [18F]fallypride binding potential in other regions. (A-G) Scatterplots of midbrain BPND (x-axis) vs. BPND in regions where no significant group*BPND interaction was observed (y-axis) fit with a linear regression for the ICB+ and ICB- groups. No interaction effect was observed in the (A-B) ventral striatum (ICB+: r=0.499, P=0.058; ICB-: r=0.593 P=0.016) or (C-D) thalamus (ICB+: r=0.395, P=0.145; ICB-: r=0.380 P=0.146), indicating the lack of a divergent BPND relationship between the structures. Download Figure 3-1, DOCX file (48KB, docx)
Discussion
Because the clinical phenotype of compulsive participation in reward-based behaviors is causally linked to DAgonist use, investigating how D2/3 receptors relate to behavioral symptoms could prove useful to the broader study of dopamine and compulsive behaviors. Our main finding replicates and extends previous work in the neurobiology of addiction, where PD patients with ICB have reduced D2/3 BPND, localizing to the ventral striatum and putamen. In these patients, we observe a significant positive relationship between midbrain D2/3 BPND levels and the severity of reward-seeking behavior (QUIP-RS), and positive correlations between D2/3 receptor levels in the midbrain, striatum, and amygdala. These results indicate that D2/3 receptor status in PD patients may play a key role in the manifestation of DAgonist-induced ICBs. The precise mechanism of this influence may include premorbid, PD-related, or treatment-related changes to D2/3 receptor number and function, ultimately influencing how a patient can regulate reward-based behavior.
Ventral striatal dopamine and ICB status
The ventral striatum is a crucial structure to reinforcement learning in the initial stages of addiction (O'Doherty et al., 2004; Everitt and Robbins, 2005). Ventral striatal dopamine transmission mediates the maintenance of both the psychostimulant and reinforcement effects of drugs of abuse (Pettit et al., 1984; Caine and Koob, 1994) and a number of previous studies demonstrate reduced D2/3 levels in human psychostimulant, alcohol, and opiate addiction (Trifilieff and Martinez, 2014). However, this association has not been universally observed across the spectrum of maladaptive reward-seeking behavior, where reductions are notably absent in primary gambling addiction (Nutt et al., 2015). Our findings are consistent with previous reports of decreased baseline ventral striatal D2/3 BPND in PD patients with ICB, as reported with [11C]raclopride (Steeves et al., 2009) and [11C]-(+)-PHNO (Payer et al., 2015). Although these radioligands have differing affinities for D2 and D3 receptors, lower D2/3 receptors in the ventral striatum are clearly associated with PD patients who develop behavioral changes over the course of treatment (Narendran et al., 2006; Tziortzi et al., 2011).
Within the ventral striatum, D2/3 receptors localize to both presynaptic mesolimbic terminal autoreceptors and postsynaptic indirect-pathway medium spiny neurons (Anzalone et al., 2012; Kenny et al., 2013). The decreased ventral striatal D2/3 receptor levels observed in substance abuse, extreme obesity, and impulsive disorders have been associated with decreased function of the indirect pathway, which mediates behavioral flexibility and avoidance learning in response to novel stimuli (Kenny et al., 2013; Nakanishi et al., 2014). In contrast, the direct pathway is characterized by the expression of dopamine D1 receptors, which are involved in reward motivation (Kenny et al., 2013; Nakanishi et al., 2014). Notably, PET studies of D1 receptor expression in PD have reported no differences in the striatum (Cropley et al., 2008) emphasizing dissimilar direct pathway effects. Therefore, the findings of decreased ventral striatal D2/3 receptor levels (Steeves et al., 2009; Payer et al., 2015), unaltered striatal D1 receptor levels (Cropley et al., 2008), and increased ventral striatal extracellular dopamine (Steeves et al., 2009) suggest that when an imbalance between the direct and indirect pathways in the ventral striatum is coupled with increased DA release in response to rewarding stimuli, increased reward motivation in the setting of decreased avoidance learning could lead to the manifestation of ICBs in PD.
A key unanswered question is whether the lower ventral striatal D2/3 binding precedes, or emerges after, dopamine-related treatment. Preclinical models of addiction support the former hypothesis, where decreased ventral striatal D2/3 receptor expression in animals is associated with greater trait impulsivity (as indexed by the ability to withhold premature motor responses) as well as drug-taking behavior in rodents and nonhuman primates (Nader et al., 2006; Dalley et al., 2007). By contrast, overexpression of ventral striatal D2 increases motivation for long-term effortful outcomes over short-term reward (Trifilieff et al., 2013), as well as reducing drug intake (Thanos et al., 2008). However, divergent patterns of PD neurodegeneration or cellular responses to medication could also effect the manifestation of group differences, through PD-related dopaminergic denervation of nigrostriatal projections (Rinne et al., 1990) or mechanisms of agonist-induced receptor internalization, respectively (Itokawa et al., 1996). In particular, animal studies suggest that DAgonist administration can selectively decrease dopamine D2/3 receptor levels in the nucleus accumbens/ventral striatum (Engber et al., 1993).
The dorsal striatum and habitual behavior
Previous studies in PD have not observed altered dorsal striatal D2/3 BPND in relation to ICB status. Whereas the ventral striatum is associated with anticipation of future rewards and reward-related drug reinforcement, the dorsal striatum maintains compulsive habitual responding to reward-based behaviors (O'Doherty et al., 2004; Everitt and Robbins, 2005). Indeed, dorsal striatal dopamine release is necessary to maintain habit-based learning in addiction paradigms (Yin et al., 2004; Vanderschuren et al., 2005), where reductions in dorsal D2/3 receptor BPND occur after an action becomes habitual (Nader et al., 2006; Dalley et al., 2007). Dorsal striatal reductions in D2/3 receptors are observed in patients with long-term cocaine, methamphetamine, alcohol, nicotine, and opiate abuse (Trifilieff and Martinez, 2014). In this manner, an impulsive behavior becomes compulsive, as dopaminergic abnormalities that initially occur in the ventral striatum, extend dorsally via the feedforward striato–nigro–striatal loop (Haber and Knutson, 2010). At the receptor level, low ventral striatal D2/3 receptors (associated with reward-related impulsivity) cause signaling changes that over time evolve into dorsal D2/3 reductions (linked to compulsive reward driven behavior). Together, we interpret reduced [18F]fallypride binding in both ventral and dorsal striatum of ICB patients as a neurobiological manifestation of both impulsive, and compulsive behaviors, paralleling previous findings in substance abuse disorders.
The midbrain and impulsive-compulsive behavioral symptoms
Although differences in mean ventral midbrain D2/3 BPND in ICB have not been reported by the current or a previous study (Ray et al., 2012) a positive relationship was observed in the current study between midbrain [18F]fallypride BPND and the severity of reward seeking behaviors (QUIP-RS), in ICB+ but not ICB− patients. This parallels a past [11C]-(+)-PHNO PET study that described a similar relationship between pathological gambling severity and midbrain binding (Boileau et al., 2013). In healthy humans, impulsivity has been positively correlated with anteroventral striatal dopamine release and negatively correlated with ventral midbrain D2/3 (Buckholtz et al., 2010). Similarly, PD patients with DAgonist-induced pathological gambling demonstrated increased ventral striatal dopamine release during performance on a gambling task relative to those without this side-effect (Steeves et al., 2009); in addition, increased ventral striatal dopamine release has also been reported following presentation of reward-related visual cues associated with individual ICBs in ICB+ patients (O'Sullivan et al., 2011; Wu et al., 2015). Combined, these studies suggest that state impulsivity in younger healthy subjects and ICBs in PD bear a common association with increased ventral striatal dopamine release.
Given that ventral midbrain D2/3 receptors function as inhibitory autoreceptors at both axonal and somatodendritic areas, and the negative correlation between midbrain D2/3 BPND and state impulsivity seen in healthy subjects (Mercuri et al., 1992; Khan et al., 1998; Buckholtz et al., 2010), the positive correlation between ventral midbrain D2/3 BPND and QUIP-RS scores would therefore appear to be unexpected. However, the total level of ventral midbrain D2/3 receptors includes those expressed on axons innervating the dorsal as well as the ventral striatum, in addition to other brain structures. Although postmortem studies of early to middle stage PD have shown that dopaminergic projections to the motor striatum are more severely affected by denervation (Gibb and Lees, 1991), the fraction of D2/3 receptors expressed on neurons projecting to the ventral striatum likely still represents a small minority of the total ventral midbrain D2/3 content. The lack of difference in total level of ventral midbrain D2/3 receptors may therefore not be informative as to the status of neurons projecting to the ventral striatum. If the number of D2/3 receptors on individual dopamine neurons projecting to the ventral striatum remains relatively constant between ICB+ and ICB− subjects, then the positive correlation seen in this study may reflect a relatively more intact dopaminergic innervation of the ventral striatum consistent with the increased ventral striatal dopamine release seen in previous studies.
One prior study of DAgonist-induced pathological gambling has also observed distinctions in the ventral midbrain, where performance of a gambling task produced greater apparent dopamine release in ICB− compared with ICB+ subjects (Ray et al., 2012). The authors concluded that this apparent decreased DA release reflected altered D2/3 autoreceptor function leading to the previously reported increase in ventral striatal dopamine release. However, this PET [11C]FLB-457 study was performed following pramipexole administration, which has been shown to produce significant changes in ventral midbrain dopamine D2/3 BPND that were not present in the ventral striatum (Ray et al., 2012; Deutschländer et al., 2016). Combined with the finding that dopamine release within the midbrain is crucial in producing therapeutic psychostimulant effects in related psychiatric phenotypes, such as attention deficit/hyperactivity disorder (del Campo et al., 2013) it is likely that individual differences in both midbrain D2/3 survival and drug sensitivity are involved in the manifestation of ICB. As a result, the interaction between pramipexole binding and changes in autoreceptor function requires further study. The positive correlation of midbrain D2/3 receptor levels with dopamine agonist induced altered reward behaviors in PD seen in the current study suggests the possibility that ICB+ PD subjects may have relatively greater preservation of ventral striatal dopaminergic innervation than ICB− subjects.
Relationships between dopamine receptors in the midbrain and other reward related-regions
Correlations between midbrain D2/3 BPND and the caudate, putamen, globus pallidus, and amygdala significantly differ between groups. Using [18F]fallypride, significant positive BPND correlations between midbrain, striatum, and amygdala (Zald et al., 2010) are evident in healthy humans. A positive correlation across multiple regions may reflect similar types of D2/3 receptors (e.g., autoreceptors), concerted influence of nigrostriatal and mesolimbic dopamine release or DAgonist effects on D2/3 expression (Itokawa et al., 1996; Haber and Knutson, 2010), or the relative integrity of midbrain-based dopaminergic networks. Although the comparison of interregional correlations is cautiously interpreted given the older age of our subjects (Zald et al., 2010), ICB+ patients appear more similar to healthy controls. The ventral midbrain is known to contain several heterogeneous subpopulations, with unique patterns of anatomical projection, pharmacological and cellular properties, and relevance to behavior (Lammel et al., 2008; Haber and Knutson, 2010). Furthermore, past evidence using presynaptic biomarkers such as FDOPA indicates that dopaminergic projections undergo differential rates of PD-related degeneration, where the loss of dorsal striatal innervation is known to precede the same process in the ventral striatum (Gibb and Lees, 1991; Kumakura et al., 2010). Consequently, denervation that uniquely spares cells that regulate dopamine release to the dorsal striatum, globus pallidus, or amygdala could also be involved in producing ICBs. This result could also be affected by similar expression, but altered dynamic function of D2/3 in ICB+ patients. Chronic DAgonist administration can induce midbrain D2 autoreceptor desensitization in rodents (Chernoloz et al., 2009), and differences in this response, or PD-related changes to receptor functionality could also play a role. Regardless of the mechanism, ICB appears to be associated with greater functional preservation of midbrain dopaminergic terminal fields in ICB+ compared with ICB− subjects. Increased integrity of midbrain dopamine neuron subpopulations and the extended reward network, in combination with decreased ventral striatal and putamen dopamine D2/3 receptor levels, may result in a DAgonist “overdose” of the reward circuit that drives the development of compulsive reward-driven behaviors with impaired inhibitory behavioral control.
Limitations and future directions
Interpretation of the present work relies on the assumption that BPND differences are manifestations of ICB-related distinctions in D2/3 receptor expression. Changes in apparent [18F]fallypride BPNDs can also be produced by differences in extracellular dopamine levels, which compete with [18F]fallypride in binding to D2/3 receptors. However, previous studies examining the relationship between shifts in striatal extracellular dopamine levels and changes in [11C]raclopride binding have indicated a 44:1 ratio, where a 44% increase in extracellular dopamine produces a 1% decrease in BPND (Breier et al., 1997). In the current study, ICB+ patients have ventral striatal D2/3 receptor levels 17.1% lower than those seen in ICB− patients, adjusted for covariates; such a difference in [18F]fallypride BPND would require an ∼750% higher extracellular dopamine level. Therefore, it is unlikely that the entire difference in ventral striatal [18F]fallypride BPND is due to increased extracellular dopamine levels. Although some studies have expressed differences in stimuli-induced acute dopamine release in ICB+ subjects (Steeves et al., 2009; Ray et al., 2012), no reports have described synaptic dopamine concentrations at rest. Therefore, the topics of ICB-related dopamine release and reward-circuit preservation demand further exploration by other experimental modalities, such as [18F]fallypride with concurrent pharmacological challenge. Animal models are needed to test mechanistic hypotheses relating to medication use and altered ventral striatal D2/3 receptor levels. In addition, whereas the cohort included in the present study was composed mostly of ICB+ subjects defined by hypersexuality and compulsive eating, some previous studies have exclusively examined pathological gamblers (Steeves et al., 2009; Ray et al., 2012); although similarities are apparent between the two samples (including reduced ventral striatal BPND, as well as a relationship between midbrain BPND and impulsivity) differences are also present (such as the lack of cortical findings in the present work). Overall, these findings emphasize a distinct association between medication-induced reward-driven-behaviors and altered expression of D2/3 receptors in key striatal and midbrain components of reward networks in PD patients. Further validation of this relationship could eventually lead to the use of [18F]fallypride as a screening measure for personalization of treatment regimens, and a better understanding of which individuals respond best to the long-term prescription of DAgonist medication.
Footnotes
This work was supported by the National Institutes of Health/National Institute of Neurological Disorders and Stroke (R01NS097783, K23NS080988), the American Heart Association (14GRNT20150004), and CTSA Award UL1TR000445 from the National Center for Advancing Translational Sciences. We thank the patients for taking part in this study, and Kristen Kanoff, Charis Spears, and Carlos Faraco for their roles in data collection.
The authors declare no competing financial interests.
References
- American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders: DSM-IV-TR, Ed 4, text revision. Washington, DC: American Psychiatric Association. [Google Scholar]
- Anzalone A, Lizardi-Ortiz JE, Ramos M, De Mei C, Hopf FW, Iaccarino C, Halbout B, Jacobsen J, Kinoshita C, Welter M, Caron MG, Bonci A, Sulzer D, Borrelli E (2012) Dual control of dopamine synthesis and release by presynaptic and postsynaptic dopamine D2 receptors. J Neurosci 32:9023–9034. 10.1523/JNEUROSCI.0918-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boileau I, Payer D, Chugani B, Lobo D, Behzadi A, Rusjan PM, Houle S, Wilson AA, Warsh J, Kish SJ, Zack M (2013) The D2/3 dopamine receptor in pathological gambling: a positron emission tomography study with [11C]-(+)-propyl-hexahydro-naphtho-oxazin and [11C]raclopride. Addiction 108:953–963. 10.1111/add.12066 [DOI] [PubMed] [Google Scholar]
- Breier A, Su TP, Saunders R, Carson RE, Kolachana BS, de Bartolomeis A, Weinberger DR, Weisenfeld N, Malhotra AK, Eckelman WC, Pickar D (1997) Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc Natl Acad Sci U S A 94:2569–2574. 10.1073/pnas.94.6.2569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckholtz JW, Treadway MT, Cowan RL, Woodward ND, Li R, Ansari MS, Baldwin RM, Schwartzman AN, Shelby ES, Smith CE, Kessler RM, Zald DH (2010) Dopaminergic network differences in human impulsivity. Science 329:532. 10.1126/science.1185778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caine SB, Koob GF (1994) Effects of mesolimbic dopamine depletion on responding maintained by cocaine and food. J Exp Anal Behav 61:213–221. 10.1901/jeab.1994.61-213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camps M, Cortés R, Gueye B, Probst A, Palacios JM (1989) Dopamine receptors in human brain: autoradiographic distribution of D2 sites. Neuroscience 28:275–290. 10.1016/0306-4522(89)90179-6 [DOI] [PubMed] [Google Scholar]
- Chernoloz O, El Mansari M, Blier P (2009) Sustained administration of pramipexole modifies the spontaneous firing of dopamine, norepinephrine, and serotonin neurons in the rat brain. Neuropsychopharmacology 34:651–661. 10.1038/npp.2008.114 [DOI] [PubMed] [Google Scholar]
- Claassen DO, Kanoff K, Wylie SA (2013) Dopamine agonists and impulse control disorders in Parkinson's disease. US Neurol 9:13–16. 10.17925/USN.2013.09.01.13 [DOI] [Google Scholar]
- Cropley VL, Fujita M, Bara-Jimenez W, Brown AK, Zhang XY, Sangare J, Herscovitch P, Pike VW, Hallett M, Nathan PJ, Innis RB (2008) Pre- and post-synaptic dopamine imaging and its relation with frontostriatal cognitive function in parkinson disease: PET studies with [11C]NNC 112 and [18F]FDOPA. Psychiatry Res 163:171–182. 10.1016/j.pscychresns.2007.11.003 [DOI] [PubMed] [Google Scholar]
- Dalley JW, Fryer TD, Brichard L, Robinson ES, Theobald DE, Lääne K, Peña Y, Murphy ER, Shah Y, Probst K, Abakumova I, Aigbirhio FI, Richards HK, Hong Y, Baron JC, Everitt BJ, Robbins TW (2007) Nucleus accumbens D2/3 receptors predict trait impulsivity and cocaine reinforcement. Science 315:1267–1270. 10.1126/science.1137073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Campo N, Fryer TD, Hong YT, Smith R, Brichard L, Acosta-Cabronero J, Chamberlain SR, Tait R, Izquierdo D, Regenthal R, Dowson J, Suckling J, Baron JC, Aigbirhio FI, Robbins TW, Sahakian BJ, Müller U (2013) A positron emission tomography study of nigro-striatal dopaminergic mechanisms underlying attention: implications for ADHD and its treatment. Brain 136:3252–3270. 10.1093/brain/awt263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deutschländer A, la Fougère C, Boetzel K, Albert NL, Gildehaus FJ, Bartenstein P, Xiong G, Cumming P (2016) Occupancy of pramipexole (Sifrol) at cerebral dopamine D2/3 receptors in Parkinson's disease patients. Neuroimage Clin 12:41–46. 10.1016/j.nicl.2016.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egerton A, Hirani E, Ahmad R, Turton DR, Brickute D, Rosso L, Howes OD, Luthra SK, Grasby PM (2010) Further evaluation of the carbon11-labeled D2/3 agonist PET radiotracer PHNO: reproducibility in tracer characteristics and characterization of extrastriatal binding. Synapse 64:301–312. 10.1002/syn.20718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engber TM, Marin C, Susel Z, Chase TN (1993) Differential effects of chronic dopamine D1 and D2 receptor agonists on rotational behavior and dopamine receptor binding. Eur J Pharmacol 236:385–393. 10.1016/0014-2999(93)90476-X [DOI] [PubMed] [Google Scholar]
- Everitt BJ, Robbins TW (2005) Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci 8:1481–1489. 10.1038/nn1579 [DOI] [PubMed] [Google Scholar]
- Fabbrini G, Juncos J, Mouradian MM, Serrati C, Chase TN (1987) Levodopa pharmacokinetic mechanisms and motor fluctuations in Parkinson's disease. Ann Neurol 21:370–376. 10.1002/ana.410210409 [DOI] [PubMed] [Google Scholar]
- Farde L, Suhara T, Nyberg S, Karlsson P, Nakashima Y, Hietala J, Halldin C (1997) A PET-study of [11C]FLB 457 binding to extrastriatal D2-dopamine receptors in healthy subjects and antipsychotic drug-treated patients. Psychopharmacology (Berl) 133:396–404. 10.1007/s002130050420 [DOI] [PubMed] [Google Scholar]
- Gibb WR, Lees AJ (1991) Anatomy, pigmentation, ventral and dorsal subpopulations of the substantia nigra, and differential cell death in Parkinson's disease. J Neurol Neurosurg Psychiatry 54:388–396. 10.1136/jnnp.54.5.388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, Dubois B, Holloway R, Jankovic J, Kulisevsky J, Lang AE, Lees A, Leurgans S, LeWitt PA, Nyenhuis D, Olanow CW, et al. (2008) Movement disorder society-sponsored revision of the unified Parkinson's disease rating scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 23:2129–2170. 10.1002/mds.22340 [DOI] [PubMed] [Google Scholar]
- Grober E, Sliwinski M (1991) Development and validation of a model for estimating premorbid verbal intelligence in the elderly. J Clin Exp Neuropsychol 13:933–949. 10.1080/01688639108405109 [DOI] [PubMed] [Google Scholar]
- Gunn RN, Lammertsma AA, Hume SP, Cunningham VJ (1997) Parametric imaging of ligand-receptor binding in PET using a simplified reference region model. Neuroimage 6:279–287. 10.1006/nimg.1997.0303 [DOI] [PubMed] [Google Scholar]
- Haber SN, Knutson B (2010) The reward circuit: linking primate anatomy and human imaging. Neuropsychopharmacology 35:4–26. 10.1038/npp.2009.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall H, Ogren SO, Köhler C, Magnusson O (1989) Animal pharmacology of raclopride, a selective dopamine D2 antagonist. Psychopharmacol Ser 7:123–130. [DOI] [PubMed] [Google Scholar]
- Harrison MB, Wylie SA, Frysinger RC, Patrie JT, Huss DS, Currie LJ, Wooten GF (2009) UPDRS activity of daily living score as a marker of Parkinson's disease progression. Mov Disord 24:224–230. 10.1002/mds.22335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itokawa M, Toru M, Ito K, Tsuga H, Kameyama K, Haga T, Arinami T, Hamaguchi H (1996) Sequestration of the short and long isoforms of dopamine D2 receptors expressed in chinese hamster ovary cells. Mol Pharmacol 49:560–566. [PubMed] [Google Scholar]
- Joyce JN, Janowsky A, Neve KA (1991) Characterization and distribution of [125I]epidepride binding to dopamine D2 receptors in basal ganglia and cortex of human brain. J Pharmacol Exp Ther 257:1253–1263. [PubMed] [Google Scholar]
- Kaasinen V, Någren K, Hietala J, Oikonen V, Vilkman H, Farde L, Halldin C, Rinne JO (2000) Extrastriatal dopamine D2 and D3 receptors in early and advanced Parkinson's disease. Neurology 54:1482–1487. 10.1212/WNL.54.7.1482 [DOI] [PubMed] [Google Scholar]
- Kenny PJ, Voren G, Johnson PM (2013) Dopamine D2 receptors and striatopallidal transmission in addiction and obesity. Curr Opin Neurobiol 23:535–538. 10.1016/j.conb.2013.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RM, Woodward ND, Riccardi P, Li R, Ansari MS, Anderson S, Dawant B, Zald D, Meltzer HY (2009) Dopamine D2 receptor levels in striatum, thalamus, substantia nigra, limbic regions, and cortex in schizophrenic subjects. Biol Psychiatry 65:1024–1031. 10.1016/j.biopsych.2008.12.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Mason N, Jones C, Ansari M, Manning R, Price R (2000) N-allyl-5-fluoropropylepidepride (fallypride): radiation dosimetry, quantification of striatal and extrastriatal dopamine receptors in man. Neuroimage 11:S32. [Google Scholar]
- Khan ZU, Mrzljak L, Gutierrez A, de la Calle A, Goldman-Rakic PS (1998) Prominence of the dopamine D2 short isoform in dopaminergic pathways. Proc Natl Acad Sci U S A 95:7731–7736. 10.1073/pnas.95.13.7731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumakura Y, Danielsen EH, Gjedde A, Vernaleken I, Buchholz HG, Heinz A, Gründer G, Bartenstein P, Cumming P (2010) Elevated [18F]FDOPA utilization in the periaqueductal gray and medial nucleus accumbens of patients with early Parkinson's disease. Neuroimage 49:2933–2939. 10.1016/j.neuroimage.2009.11.035 [DOI] [PubMed] [Google Scholar]
- Lammel S, Hetzel A, Häckel O, Jones I, Liss B, Roeper J (2008) Unique properties of mesoprefrontal neurons within a dual mesocorticolimbic dopamine system. Neuron 57:760–773. 10.1016/j.neuron.2008.01.022 [DOI] [PubMed] [Google Scholar]
- Lammertsma AA, Bench CJ, Hume SP, Osman S, Gunn K, Brooks DJ, Frackowiak RS (1996) Comparison of methods for analysis of clinical [11C] raclopride studies. J Cerebl Blood Flow Metab 16:42–52. 10.1097/00004647-199601000-00005 [DOI] [PubMed] [Google Scholar]
- Mawlawi O, Martinez D, Slifstein M, Broft A, Chatterjee R, Hwang DR, Huang Y, Simpson N, Ngo K, Van Heertum R, Laruelle M (2001) Imaging human mesolimbic dopamine transmission with positron emission tomography: I. accuracy and precision of D2 receptor parameter measurements in ventral striatum. J Cereb Blood Flow Metab 21:1034–1057. 10.1097/00004647-200109000-00002 [DOI] [PubMed] [Google Scholar]
- Mercuri NB, Calabresi P, Bernardi G (1992) The electrophysiological actions of dopamine and dopaminergic drugs on neurons of the substantia nigra pars compacta and ventral tegmental area. Life Sci 51:711–718. 10.1016/0024-3205(92)90479-9 [DOI] [PubMed] [Google Scholar]
- Mestre TA, Strafella AP, Thomsen T, Voon V, Miyasaki J (2013) Diagnosis and treatment of impulse control disorders in patients with movement disorders. Ther Adv Neurol Disord 6:175–188. 10.1177/1756285613476127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee J, Christian BT, Dunigan KA, Shi B, Narayanan TK, Satter M, Mantil J (2002) Brain imaging of 18F-fallypride in normal volunteers: blood analysis, distribution, test–retest studies, and preliminary assessment of sensitivity to aging effects on dopamine D-2/D-3 receptors. Synapse 46:170–188. 10.1002/syn.10128 [DOI] [PubMed] [Google Scholar]
- Nader MA, Morgan D, Gage HD, Nader SH, Calhoun TL, Buchheimer N, Ehrenkaufer R, Mach RH (2006) PET imaging of dopamine D2 receptors during chronic cocaine self-administration in monkeys. Nat Neurosci 9:1050–1056. 10.1038/nn1737 [DOI] [PubMed] [Google Scholar]
- Nakanishi S, Hikida T, Yawata S (2014) Distinct dopaminergic control of the direct and indirect pathways in reward-based and avoidance learning behaviors. Neuroscience 282:49–59. 10.1016/j.neuroscience.2014.04.026 [DOI] [PubMed] [Google Scholar]
- Narendran R, Slifstein M, Guillin O, Hwang Y, Hwang DR, Scher E, Reeder S, Rabiner E, Laruelle M (2006) Dopamine (D2/3) receptor agonist positron emission tomography radiotracer [11C]-(+)-PHNO is a D3 receptor preferring agonist in vivo. Synapse 60:485–495. 10.1002/syn.20325 [DOI] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H (2005) The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53:695–699. 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- Nutt DJ, Lingford-Hughes A, Erritzoe D, Stokes PR (2015) The dopamine theory of addiction: 40 years of highs and lows. Nat Rev Neurosci 16:305–312. 10.1038/nrn3939 [DOI] [PubMed] [Google Scholar]
- O'Doherty J, Dayan P, Schultz J, Deichmann R, Friston K, Dolan RJ (2004) Dissociable roles of ventral and dorsal striatum in instrumental conditioning. Science 304:452–454. 10.1126/science.1094285 [DOI] [PubMed] [Google Scholar]
- O'Sullivan SS, Wu K, Politis M, Lawrence AD, Evans AH, Bose SK, Djamshidian A, Lees AJ, Piccini P (2011) Cue-induced striatal dopamine release in Parkinson's disease-associated impulsive-compulsive behaviours. Brain 134:969–978. 10.1093/brain/awr003 [DOI] [PubMed] [Google Scholar]
- Payer DE, Guttman M, Kish SJ, Tong J, Strafella A, Zack M, Adams JR, Rusjan P, Houle S, Furukawa Y, Wilson AA, Boileau I (2015) [11C]-(+)-PHNO PET imaging of dopamine D2/3 receptors in Parkinson's disease with impulse control disorders. Mov Disord 30:160–166. 10.1002/mds.26135 [DOI] [PubMed] [Google Scholar]
- Pettit HO, Ettenberg A, Bloom FE, Koob GF (1984) Destruction of dopamine in the nucleus accumbens selectively attenuates cocaine but not heroin self-administration in rats. Psychopharmacology (Berl) 84:167–173. 10.1007/BF00427441 [DOI] [PubMed] [Google Scholar]
- Piercey MF. (1998) Pharmacology of pramipexole, a dopamine D3-preferring agonist useful in treating Parkinson's disease. Clin Neuropharmacol 21:141–151. [PubMed] [Google Scholar]
- Radloff LS. (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Ray NJ, Miyasaki JM, Zurowski M, Ko JH, Cho SS, Pellecchia G, Antonelli F, Houle S, Lang AE, Strafella AP (2012) Extrastriatal dopaminergic abnormalities of DA homeostasis in Parkinson's patients with medication-induced pathological gambling: a [11C] FLB-457 and PET study. Neurobiol Dis 48:519–525. 10.1016/j.nbd.2012.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinne UK, Laihinen A, Rinne JO, Någren K, Bergman J, Ruotsalainen U (1990) Positron emission tomography demonstrates dopamine D2 receptor supersensitivity in the striatum of patients with early Parkinson's disease. Mov Disord 5:55–59. 10.1002/mds.870050114 [DOI] [PubMed] [Google Scholar]
- Schaltenbrand G, Wahren W (1998) Atlas for stereotaxy of the human brain: with an accompanying guide (2nd ed. rev). Stuttgart, Germany: Thieme. [Google Scholar]
- Steeves TD, Miyasaki J, Zurowski M, Lang AE, Pellecchia G, Van Eimeren T, Rusjan P, Houle S, Strafella AP (2009) Increased striatal dopamine release in parkinsonian patients with pathological gambling: a [11C] raclopride PET study. Brain 132:1376–1385. 10.1093/brain/awp054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thanos PK, Michaelides M, Umegaki H, Volkow ND (2008) D2R DNA transfer into the nucleus accumbens attenuates cocaine self-administration in rats. Synapse 62:481–486. 10.1002/syn.20523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson's disease. Mov Disord 25:2649–2653. 10.1002/mds.23429 [DOI] [PubMed] [Google Scholar]
- Tompson D, Oliver-Willwong R (2009) Pharmacokinetic and pharmacodynamic comparison of ropinirole 24-hour prolonged release and ropinirole immediate release in patients with Parkinson's disease. Clin Neuropharmacol 32:140–148. 10.1097/WNF.0b013e318176c505 [DOI] [PubMed] [Google Scholar]
- Trifilieff P, Martinez D (2014) Imaging addiction: D2 receptors and dopamine signaling in the striatum as biomarkers for impulsivity. Neuropharmacology 76:498–509. 10.1016/j.neuropharm.2013.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trifilieff P, Feng B, Urizar E, Winiger V, Ward RD, Taylor KM, Martinez D, Moore H, Balsam PD, Simpson EH, Javitch JA (2013) Increasing dopamine D2 receptor expression in the adult nucleus accumbens enhances motivation. Mol Psychiatry 18:1025–1033. 10.1038/mp.2013.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tziortzi AC, Searle GE, Tzimopoulou S, Salinas C, Beaver JD, Jenkinson M, Laruelle M, Rabiner EA, Gunn RN (2011) Imaging dopamine receptors in humans with [11C]-(+)-PHNO: dissection of D3 signal and anatomy. Neuroimage 54:264–277. 10.1016/j.neuroimage.2010.06.044 [DOI] [PubMed] [Google Scholar]
- Vanderschuren LJ, Di Ciano P, Everitt BJ (2005) Involvement of the dorsal striatum in cue-controlled cocaine seeking. J Neurosci 25:8665–8670. 10.1523/JNEUROSCI.0925-05.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voon V, Potenza MN, Thomsen T (2007) Medication-related impulse control and repetitive behaviors in Parkinson's disease. Curr Opin Neurol 20:484–492. 10.1097/WCO.0b013e32826fbc8f [DOI] [PubMed] [Google Scholar]
- Voon V, Sohr M, Lang AE, Potenza MN, Siderowf AD, Whetteckey J, Weintraub D, Wunderlich GR, Stacy M (2011) Impulse control disorders in Parkinson disease: a multicenter case-control study. Ann Neurol 69:986–996. 10.1002/ana.22356 [DOI] [PubMed] [Google Scholar]
- Weintraub D, Hoops S, Shea JA, Lyons KE, Pahwa R, Driver-Dunckley ED, Adler CH, Potenza MN, Miyasaki J, Siderowf AD, Duda JE, Hurtig HI, Colcher A, Horn SS, Stern MB, Voon V (2009) Validation of the questionnaire for impulsive-compulsive disorders in Parkinson's disease. Mov Disord 24:1461–1467. 10.1002/mds.22571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weintraub D, Mamikonyan E, Papay K, Shea JA, Xie SX, Siderowf A (2012) Questionnaire for impulsive-compulsive disorders in Parkinson's disease-rating scale. Mov Disord 27:242–247. 10.1002/mds.24023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu K, Politis M, O'Sullivan SS, Lawrence AD, Warsi S, Bose S, Lees AJ, Piccini P (2015) Single versus multiple impulse control disorders in Parkinson's disease: an 11C-raclopride positron emission tomography study of reward cue-evoked striatal dopamine release. J Neurol 262:1504–1514. 10.1007/s00415-015-7722-7 [DOI] [PubMed] [Google Scholar]
- Yin HH, Knowlton BJ, Balleine BW (2004) Lesions of dorsolateral striatum preserve outcome expectancy but disrupt habit formation in instrumental learning. Eur J Neurosci 19:181–189. 10.1111/j.1460-9568.2004.03095.x [DOI] [PubMed] [Google Scholar]
- Zald DH, Woodward ND, Cowan RL, Riccardi P, Ansari MS, Baldwin RM, Cowan RL, Smith CE, Hakyemez H, Li R, Kessler RM (2010) The interrelationship of dopamine D2-like receptor availability in striatal and extrastriatal brain regions in healthy humans: a principal component analysis of [18F]fallypride binding. Neuroimage 51:53–62. 10.1016/j.neuroimage.2010.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PET acquisition time parameters. Download Table 1-1, DOCX file (51.3KB, docx)
PET acquisition time parameters. Acquisition parameters related to DY period start times and break lengths for both groups. Download Table 1-2, DOCX file (52.1KB, docx)
Dopamine agonist medication distribution. The number of individuals prescribed pramipexole, ropinirole, or rotigotine is listed for each group. No other dopamine agonist medications were represented, and no individual was prescribed multiple medications concurrently. No significant differences were found in the distribution of dopamine agonist medications prescribed to the ICB+ and ICB- groups, indicating that treatment differences are unlikely to be a confounding factor. Download Table 1-3, DOCX file (53.5KB, docx)
Manual segmentation protocol for [18F]fallypride binding potential analysis. (A-G) Representative coronal and axial slices for a single subject show an example of the manual segmentation routine for four different structures, including (A) caudate, (B) amygdala, (C) putamen, (D) thalamus, (E) ventral striatum, (F) midbrain, and (G) globus pallidus. Download Figure 1-1, TIF file (15.8MB, tif)
Mean ROI volumes. Mean volumes are listed alongside standard deviations, in mm3. No significant differences were found in structure size between the ICB+ and ICB- groups, indicating that structural volume is unlikely to be a confounding factor. Download Figure 1-2, TIF file (1.5MB, tif)
Mean ROI BPND. Age and UPDRS-II corrected BPND is listed for each group alongside standard error of the mean. Significant differences were found in between the ICB+ and ICB- groups in the ventral striatum and putamen. Download Figure 1-3, DOCX file (68.5KB, docx)
QUIP-RS and BPND correlation coefficients. The results of partial Pearson's correlation tests, corrected for age and UPDRS-II. For each ROI, the correlation coefficient and significance value is listed, separating between the ICB+ and ICB- groups. A significant correlation between QUIP-RS and midbrain BPND was found exclusively in the ICB+ group. Download Figure 2-1, DOCX file (47.5KB, docx)
Midbrain [18F]fallypride binding potential vs. [18F]fallypride binding potential in other regions. (A-G) Scatterplots of midbrain BPND (x-axis) vs. BPND in regions where no significant group*BPND interaction was observed (y-axis) fit with a linear regression for the ICB+ and ICB- groups. No interaction effect was observed in the (A-B) ventral striatum (ICB+: r=0.499, P=0.058; ICB-: r=0.593 P=0.016) or (C-D) thalamus (ICB+: r=0.395, P=0.145; ICB-: r=0.380 P=0.146), indicating the lack of a divergent BPND relationship between the structures. Download Figure 3-1, DOCX file (48KB, docx)