Abstract
The comorbidity between depression and substance use problems is well-documented, yet little research has investigated how stigma associated with one’s depression might relate to alcohol and drug use. The current study examined the association between depression-related stigma and substance use coping and considered the role of emotion dysregulation (i.e., difficulty in monitoring, evaluating, and modulating one’s emotional reactions) as a mechanism underlying this association. A sample of individuals who self-identified as having current or remitted depression (N=218) completed self-report measures of depression-related stigma, emotion dysregulation, and tendency to rely on alcohol or drugs to cope with psychological distress. Depression-related stigma was positively associated with emotion dysregulation, which was in turn associated with a greater tendency to engage in substance use coping. These findings provide initial support for the role of stigma as a contributor to maladaptive coping responses, such as substance use, among people living with depression. Further, they underscored the potential utility of targeting emotion dysregulation in stigma coping and substance abuse prevention intervention efforts.
Keywords: Depression, stigma, emotion regulation, substance use, coping
Affecting approximately 16.1 million adults each year, depression represents one of the most prevalent yet under-treated mental health conditions in the United States (National Institute of Mental Health, 2016). One major barrier to recovery faced by people with depression is the stigma associated with their psychiatric diagnosis (Corrigan, Druss, & Perlick, 2014). Across numerous studies among people with various mental illnesses, stigma has been shown to undermine self-esteem (Link, Streuening, Neese-Todd, Asmussen, & Phelan, 2001), increase social isolation (Perlick et al., 2001), and deter individuals from seeking mental health treatment (Vogel, Wade, & Haake, 2006). More specifically, depressed individuals are often stereotyped as weak and emotionally unstable (Ben-Porath, 2002), and many express concerns about the adverse impact of depression-related stigma on employment and friendships (Roeloffs et al., 2003). Little research, however, has examined how stigma might relate to alcohol and drug use. This limitation is noteworthy given the well-documented comorbidity between depression and substance use problems (Conway, Compton, Stinson, & Grant, 2006; Swendsen et al., 2010). Indeed, individuals with depression might be particularly inclined to engage in substance use as a coping strategy to alleviate their intense, pervasive psychological distress (Cooper, Frone, Russell, & Mudar, 1995; Hides et al., 2008). To this end, the present research examined the association between mental illness stigma and substance use coping by utilizing a sample of community participants who self-identified as having depression. Additionally, we explored the role of emotion dysregulation (i.e., difficulty in monitoring, evaluating, and modulating one’s emotional reactions; Thompson, Lewis, & Calkins, 2008) as a mechanism underlying this relationship.
Although little research has examined the links among stigma, emotion dysregulation, and substance use among people with mental illnesses, existing work on other stigmatized groups provides support for these associations. Specifically, an emerging body of literature highlights the role of emotion dysregulation as an important mechanism through which stigma operates to adversely impact mental and behavioral health. As explained by Hatzenbuehler (2009), chronic exposure to stigma-related stress can deplete self-regulatory resources, thereby undermining individuals’ ability to understand and manage their emotions. A daily diary study, for example, showed that stigma-related stressors can drive the use of maladaptive emotion regulation strategies (e.g., rumination, suppression) among both sexual and racial/ethnic minority participants (Hatzenbuehler, Nolen-Hoeksema, & Dovidio, 2009). In other cross-sectional and longitudinal studies, chronic exposure to stigma has also been prospectively and concurrently linked to various emotion regulation difficulties among gay and bisexual men, including lower emotional awareness and acceptance, limited access to various emotion regulation strategies, and difficulty with engaging in goal-directed behaviors when experiencing negative emotions (Pachankis et al., 2015; Rendina et al., 2017).
In addition to its ability to interfere with effective emotion regulation, stigma can also prompt escapist coping strategies such as substance use. For instance, among racial/ethnic and sexual minorities, experiences of prejudice and discrimination both concurrently and prospectively predicted alcohol and recreational drug use (Clark, 2014; Gibbons, Gerrard, Cleveland, Wills, & Brody, 2004; McLaughlin, Hatzenbuehler, & Keyes, 2010; Whitbeck, Hoyt, McMorris, Chen, & Stubben, 2001). Although no research, to our knowledge, has directly examined the role of emotion dysregulation as a mechanism underlying the association between stigma and substance use, existing evidence suggests that it might play an important role. In particular, Gibbons et al. (2012)) found that self-control (i.e., a set of related abilities that includes focusing and shifting attention, delaying gratification, and inhibiting impulsive behaviors) mediated the association between stigma-related experiences and substance use among African American adolescents. Further, emotion dysregulation is increasingly recognized as a predictor of risky behaviors such as substance use (Weiss, Sullivan, & Tull, 2015). In particular, individuals who experience greater emotion regulation difficulties tend to be more inclined to engage in substance use as a means to avoid negative emotional states that they are unable to tolerate or accept (Bonn-Miller, Vujanovic, & Zvolensky, 2008; Dvorak et al., 2014; Paulus et al., 2016). A prospective study involving individuals seeking treatment for alcohol dependence also identified emotion regulation deficits as a key predictor of alcohol use both during and after treatment (Berking et al., 2011).
In light of these findings, the present research extended previous work by examining how depression-related stigma might relate to individuals’ ability to engage in effective emotion regulation as well as their tendency to use substances as a coping mechanism. We focused on substance use coping as our outcome of interest given that individuals who use substances to cope with their negative emotions might be more prone to develop substance use problems than those who use substances for social reasons (Cooper, Russell, & George, 1988). Indeed, among a sample of African American adolescents, perceived racial discrimination was associated with increases in substance use only among those who endorsed substance use as a coping mechanism (Gerrard et al., 2012). Moreover, previous research suggests that emotion dysregulation tends to uniquely predict substance use behaviors that aim to reduce aversive psychological states (Bonn-Miller et al., 2008). As such, we believe that substance use coping might be of particular relevance in the context of the present research.
Recognizing that stigma can influence the lives of people with depression in a number of ways, we operationalized stigma as a multifaceted construct in the current study. Specifically, we measured stigma salience (i.e., the extent to which individuals think about their depression diagnosis; Quinn & Chaudoir, 2009), stigma consciousness (i.e., the extent to which individuals anticipate to be stereotyped by others based on their depression diagnosis; Pinel, 1999), and perceived stigma (i.e., perceptions of other people’s beliefs about individuals with depression; Link, 1987). We hypothesized that stigma would be associated with emotion dysregulation, which would in turn relate to substance use coping. Additionally, we hypothesized that emotion dysregulation would partially account for the association between stigma and substance use coping, as indicated by a significant indirect effect of stigma on substance use coping through emotion dysregulation. According to the modified labeling theory (Link, Struening, Cullen, Shrout, & Dohrenwend, 1989), mental illness stigma and its cognitive, affective, and behavioral sequelae largely stem from the label of having a psychiatric disorder rather than the experience of psychiatric symptoms. As such, we expected that our proposed model would hold for both individuals with ongoing or remitted symptoms, as both groups are marked by mental illness stigma. Further, given that mental illness stigma has been shown to adversely impact health above and beyond psychopathology symptoms (Link et al., 2001; Perlick et al., 2001), we expected that the hypothesized associations among stigma, emotion dysregulation, and substance use coping would remain significant when we include depressive symptoms as a covariate.
Method
Participants
Data for the current study were taken from a larger survey examining the experiences of individuals with a wide range of stigmatized identities. A total of 1,123 U.S. residents participated in the study via Amazon’s Mechanical Turk (MTurk), an Internet-based platform that permits members of the general public to complete tasks anonymously in exchange for monetary compensation. All participants were asked to select the stigmas that they possessed from a list of 93 stigmatized identities, conditions, or characteristics created in a separate study (masked for peer review). This list of stigmas contained two possible entries that are of relevance to the present research: depression (symptomatic) and depression (remitted). Participants ranked order each stigma in terms of its personal impact (i.e., the extent to which it influences one’s life and/or is considered personally significant). Participants then completed measures about their stigma-related experiences pertaining to their two most impactful stigmas, coping behaviors, and general physical and mental health. Individuals who did not complete all demographic variables or at least 50% of remaining variables (n = 115) as well as those who provided improbable responses (n = 2) were omitted from the dataset, resulting in a sample of 1,025 individuals. Of these remaining individuals, 218 indicated having depression as their most personally impactful stigma. This subset of participants (n = 218) was thus used as the analytic sample for the current study. All study materials and procedures were approved by the institutional review board of the authors’ institution.
Participants ranged in ages from 21 to 72 (M = 36.40, SD = 10.02). More than half of the participants were male (58.3%); most were White (89.9%) and did not identify as Hispanic (95.4%). The majority of the sample reported having at least some college education (82.6%), being either fulltime (51.4%) or part-time (35.7%) employed, and approximately half identified as single (44%). Most of the participants identified as having current, rather than remitted, depression (73.9%).
Measures
Stigma salience
To assess stigma salience, we asked participants to indicate the extent to which they generally think about their depression by selecting from one of the seven response options: almost never, several times a year, once a month, once a week, a few times a week, once a day, and many times each day (Quinn & Chaudoir, 2009). Following the procedure used by Quinn and Chaudoir (2009), we converted responses into a continuous measure representing the number of stigma-related thoughts per day (i.e., 0; 3/365; 12/365; 52/365; 4 × 52/365; 1; 5, respectively). Stigma salience has been associated with elevated psychological distress among individuals with a wide range of concealable stigmatized identities, including depression (Quinn & Chaudoir, 2009).
Stigma consciousness
The Stigma Consciousness Questionnaire (Pinel, 1999) assesses the extent to which stigmatized individuals expect to be stereotyped by others. Participants rated 10 items (e.g., “When interacting with others, I feel like they interpret all my behaviors in terms of my depression”) on a scale from 1 (strongly disagree) to 7 (strongly agree). The Stigma Consciousness Questionnaire has been adapted and validated across numerous stigmatized populations, including those with mental illnesses (Link, Wells, Phelan, & Yang, 2015; Pinel, 1999). In the current sample, Cronbach’s α was .82.
Perceived stigma
We assessed participants’ perception of most other people’s beliefs about depression using the six-item Devaluation subscale of the Perceived Devaluation-Discrimination Scale (e.g., “Most people think less of a person like you”; Link, 1987). Participants rated each item on a four-point scale, ranging from 1 (disagree strongly) to 4 (agree strongly). The Perceived Devaluation-Discrimination Scale was specifically developed to assess stigma associated with serious mental illnesses and has been linked to a wide range of adverse outcomes, including low self-esteem and increased social isolation (Link et al., 2001; Perlick et al., 2001). Consistent with the goals of the larger study, we included only the Devaluation sub-scale because it contains items whose wording can be easily adapted to assess the perceived stigma associated with multiple identities, conditions, or characteristics (see Meyer, Schwartz, & Frost, 2008). Cronbach’s α in the current sample was .84.
Emotion dysregulation
The 36-item Difficulties with Emotion Regulation Scale (Gratz & Roemer, 2004) assesses general problems with regulating emotions across six specific domains of dysregulation: non-acceptance of emotional responses (e.g., “When I’m upset, I become embarrassed for feeling that way”), difficulties engaging in goal-directed behavior (e.g., “When I’m upset, I have difficulty focusing on other things”), impulse control difficulties (e.g., “When I’m upset, I have difficulty controlling my behaviors”), lack of emotional awareness (e.g., “I am attentive to my feelings”; reverse-coded), limited access to emotion regulation strategies (e.g., “When I’m upset, I believe that I will remain that way for a long time”), and lack of emotional clarity (e.g., “I am confused about how I feel”). Participants rated the extent to which each item applies to themselves on a five-point scale, ranging from 1 (almost never [0–10%]) to 5 (almost always [91–100%]). The full scale score has been associated with a wide range of adverse mental and behavioral health outcomes, including depression, anxiety, self-injurious behaviors, and intimate partner violence (Gratz & Roemer, 2004). Cronbach’s α was .94 in the current sample.
Substance use coping
Substance use coping was assessed using the Brief COPE-Substance Use subscale (Carver, 1997). This scale includes two items: “I have been using alcohol or drugs to help me feel better” and “I have been using alcohol or drugs to help me get through stressful times.” Participants responded to each item using options ranging from 1 (I haven’t been doing this at all) to 4 (I have been doing this a lot). These items have been used in previous research to assess substance use coping (Gerrard et al., 2012; Nolen-Hoeksema & Harrell, 2002) and were strongly correlated in the current sample, r = .97.
Depressive symptoms
Depressive symptoms were measured using the 20-item Center for Epidemiological Studies–Depression Scale (CES-D; Radloff, 1977), a self-report symptom rating scale with an emphasis on the affective, depressed mood component of depression. Participants indicated the frequency of each symptom over the past week on a 4-point scale, ranging from 0 (rarely or none of the time [less than 1 day]) to 3 (most or all of the time [5–7 days]). Sample items include “I felt like everything I did was an effort” and “I felt hopeful about the future” (reverse-coded). Participant scores were summed across all items (in this sample, α = .92).
Data analysis
Preliminary analyses indicated that, among all of the demographic variables, age was negatively associated with substance use coping. Thus, we included age as a covariate in our subsequent analyses. To test our hypothesized associations among stigma, emotion dysregulation, and substance use coping, we utilized structural equation modeling (SEM) via AMOS 7.0 (Arbuckle, 2006), in which we specified stigma as a latent variable consisting of stigma consciousness, stigma salience, and perceived stigma; both emotion dysregulation and substance use coping were treated as manifest. As recommended by Hayes (2013), bootstrapping was used to test for indirect effects. To examine whether our proposed model would apply to individuals with remitted versus ongoing symptoms, we tested model invariance across these two subgroups. Specifically, we conducted a chi-square difference test between the fit of an unstructured model in which parameters were permitted to differ between the two groups and another in which the parameters were constrained to be equivalent between the two groups. Lastly, to account for the role that depressive symptoms might play in the associations among stigma, emotion dysregulation, and substance use coping, we reran the model while including depressive symptoms as a covariate.
Results
Zero-order correlations among all variables of interest are displayed in Table 1. The three stigma variables were positively correlated with one another and were also positively correlated with emotion dysregulation; emotion dysregulation was positively correlated with substance use coping. Depressive symptoms were positively correlated with both stigma and emotion dysregulation, though not with substance use coping. Age was negatively correlated with both emotion dysregulation and substance use coping, such that older participants reported fewer emotion regulation difficulties and were less likely to use alcohol or drugs as a coping strategy. Participants with ongoing depression symptoms reported greater levels of stigma and higher levels of emotion dysregulation than participants with remitted symptoms.
Table 1.
Zero-order correlations and group comparisons of variables in models.
| Stigma Salience | Stigma Consc. | Perceived Stigma | Substance Coping | Emotion Dysreg. | Age | |
|---|---|---|---|---|---|---|
| Stigma Consc. | .483*** | — | — | — | — | — |
| Perceived Stigma | .299*** | .575*** | — | — | — | — |
| Substance Coping | .074 | .143* | .184** | — | — | — |
| Emotion Dysreg. | .393*** | .314*** | .357*** | .244*** | — | — |
| Age | −.046 | −.068 | .002 | −.141* | −.186** | — |
| Diagnostic Status† | −7.06*** | −4.56*** | −2.40** | .312 | −3.51** | .199 |
| CES-D Score | .500*** | .375*** | .331*** | .113 | .651*** | −.033 |
p < .05.
p < .01.
p < .001.
Diagnostic Status estimates are t-values from independent t-test assuming equal variances.
Our proposed model, as depicted in Figure 1, demonstrated adequate fit, RMSEA = .07, CFI = .94, GFI = .97, χ2 = 23.75, p = .022. As hypothesized, stigma was positively associated with emotion dysregulation, β = .43, p = .006, 95% CI: [.26, .60]. Furthermore, emotion dysregulation was positively associated with substance use coping, β = .16, p = .018, 95% CI: [.02, .36]. Consistent with our expectation that emotion dysregulation would partially account for the association between stigma and substance use coping, the indirect effect of stigma on substance use coping through emotion dysregulation was significant, β = .07, p = .012, 95% CI: [.01, .17]. The direct effect of stigma on substance use coping was not significant, β = .18, p = .12, 95% CI: [−.01, .33]. Emotion dysregulation accounted for 26.9% of the total effect (β = .23, p = .005, 95% CI: [.10, .38]) of stigma on substance use coping. Nested models comparing individuals with ongoing versus remitted symptoms indicated that this mediation model did not significantly differ across groups, p = .57. The same pattern of results was obtained when we reran this model after entering depressive symptoms as a covariate, with the indirect effect of stigma on substance use coping through emotion dysregulation remaining significant, β = .04, p = .034, 95% CI: [.02, .12].1
Figure 1.
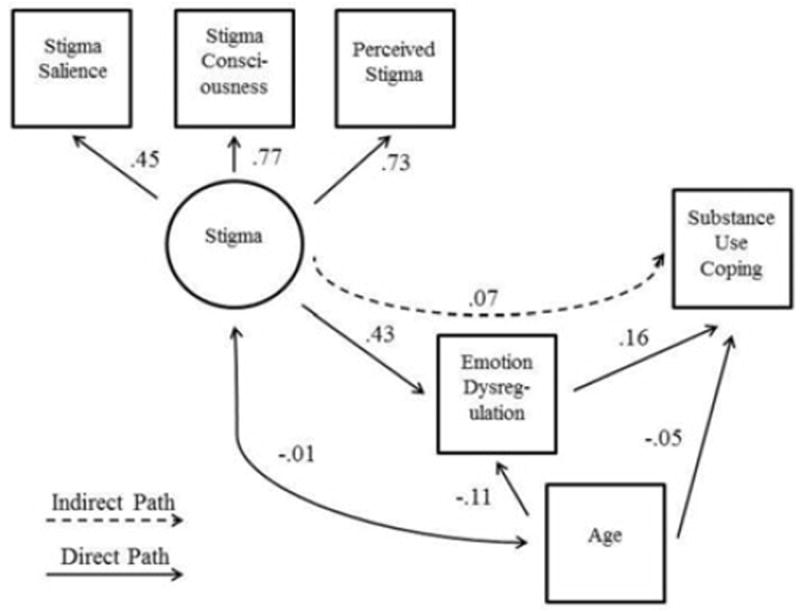
Hypothesized model with regression weights.
Discussion
In the past decade, emotion dysregulation has received increasing empirical attention as an important mechanism underlying the adverse impact of stigma on mental and behavioral health. However, most of the existing research in this area has focused on sexual and racial/ethnic minorities (e.g., Hatzenbuehler et al., 2009; Pachankis et al., 2015). The current investigation extended previous research by examining the associations among stigma-related experiences, emotion dysregulation, and substance use coping among a sample of individuals who self-identified as having depression. Consistent with our hypotheses, we found that stigma was positively associated with emotion dysregulation, which in turn related to individuals’ tendency to engage in substance use coping. Furthermore, there was a significant indirect effect of stigma on substance use coping through emotion dysregulation, supporting the role of emotion dysregulation as a mechanism mediating the association between stigma and substance use coping. It is worth noting that, consistent with the modified labeling theory (Link et al., 1989), these results were applicable to individuals with either ongoing or remitted symptoms; furthermore, they remained significant after controlling for depressive symptom severity. Taken together, these findings suggested that mental illness stigma can drive adverse outcomes across time and intensity of psychiatric symptoms.
The present findings have important theoretical and practical implications. Despite the well-documented comorbidity between depression and substance use problems (Conway et al., 2006; Swendsen et al., 2010) and the strong evidence supporting the association between stigma and substance use among other marginalized groups (Gibbons et al., 2004; McLaughlin et al., 2010), little research has considered the role of stigma as a contributor to comorbid depression and substance use problems. Our findings provide preliminary support for the idea that stigma-related experiences surrounding one’s depression can potentially prompt substance use coping by interfering with effective emotion regulation. They also highlight the potential value of addressing emotion regulation difficulties as a promising treatment target for interventions that promote adaptive coping and empowerment among individuals living with depression. Indeed, while psychotherapies targeting emotion regulation have been linked to improved substance use outcomes (Linehan et al., 1999), individuals might gain further benefit from interventions that specifically address emotion regulation deficits stemming from the stigma associated with their depression diagnosis. Consistent with this possibility, interventions that focus on strengthening emotion regulation skills (e.g., cognitive restructuring, mindfulness) have demonstrated preliminary efficacy in reducing stigma-related stress among people with various mental illnesses (e.g., Knight, Wykes, & Hayward, 2006; Luoma, Kohlenberg, Hayes, Bunting, & Rye, 2009; see Mittal, Sullivan, Chekuri, Allee, & Corrigan, 2012, for a review). Future research is needed to assess the potential efficacy of these strategies in reducing problematic substance use among people with depression. To minimize treatment burden for those who already receive psychotherapy, researchers could also explore the feasibility of incorporating stigma coping exercises into standard cognitive behavioral therapy.
The current study has several limitations. First, the cross-sectional nature of our data precludes drawing predictive, causal conclusions. In particular, whereas our conceptualization of emotion dysregulation as a mechanism underlying the association between stigma and substance use coping is well-grounded in the theoretical literature (e.g., Gibbons et al., 2012; Weiss et al., 2015), it is possible that substance use coping mediates the association between stigma and emotion dysregulation, such that individuals who rely on alcohol or drugs to cope with stress tend to experience greater emotion regulation difficulties. Further, our conclusions are subject to bias from known confounds between self-reported stress exposure and health status, such that individuals who experience poorer health outcomes (e.g., emotion dysregulation and maladaptive coping) might perceive more stigma-related experiences because of those outcomes (Contrada et al., 2000; Dohrenwend, Dohrenwend, Dodson, & Shrout, 1984). Consequently, future research using longitudinal or experimental designs is needed to clarify the relationships among mental illness stigma, emotion dysregulation, and substance use coping. For example, prospective designs that include measures of these constructs at repeated assessment points over time could help elucidate the long-term and causal effects of mental illness stigma on emotion dysregulation and substance use coping.
Second, we acknowledge that the substance use coping measure used in the current study was relatively limited in scope. Although the measure was taken from the well-validated Brief COPE questionnaire (Carver, 1997), it only contains two items and does not directly capture substance use behaviors. Given that individuals who use substances to cope with negative emotions are particularly prone to developing substance use problems (Cooper et al., 1988; Gerrard et al., 2012), we believe that focusing on substance use coping as our outcome of interest serves as a good initial step in exploring the relationship between mental illness stigma and substance use. Future research could productively examine how mental illness stigma might influence daily alcohol and drug use, which can be measured using timeline follow-back (Sobell & Sobell, 1992) or ecological momentary assessment (Shiffman, 2009) methods.
Third, given that depression has been identified as one of the most prevalent mental health conditions in the U.S. population (National Institute of Mental Health, 2016), our decision to focus on individuals with depression in the current research represents an important contribution to the mental illness stigma literature. Nonetheless, we acknowledge that people with depression tend to experience less stigmatization compared to those with other serious mental illnesses, such as schizophrenia and bipolar disorder (Angermeyer, Beck, Dietrich, & Holzinger, 2004). Future research should therefore expand the scope of the current investigation by examining the generalizability of our findings to individuals with other psychiatric disorders. Lastly, because participants for the current study were recruited on-line via Amazon’s Mechanical Turk, our sample was relatively homogeneous, with most of the participants being White and well-educated. Future research should carefully examine the generalizability of our findings using more heterogeneous, representative samples.
Deficits in emotion regulation have been implicated in the development of problematic substance use as a means to cope with psychological distress (Weiss et al., 2015). Furthermore, a small yet growing body of research has demonstrated the importance of considering emotion dysregulation in understanding maladaptive responding to stigma-related stress (e.g., Hatzenbuehler, 2009; Pachankis et al., 2015; Perez & Soto, 2011; Wang, Weiss, Pachankis, & Link, 2016). The present research contributes to the existing literature by providing initial support for the role of emotion dysregulation as a mechanism underlying the association between mental illness stigma and substance use coping among people living with depression. Further, findings underscored the potential utility of targeting emotion dysregulation in stigma coping and substance abuse prevention intervention efforts.
Acknowledgments
Preparation of this manuscript was supported by National Institutes of Health grants R01MH109413-01S1 to Katie Wang and John E. Pachankis and T32MH020031 to Charles L. Burton. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to acknowledge the contributions of Hannah Mogul-Adlin and Adam Eldahan in data collection and preparation.
Footnotes
Given that the Difficulties in Emotion Regulation Scale (DERS) consists of six subscales, we also conducted exploratory analyses to examine each of the individual subscales of the DERS as potential mediators underlying the association between stigma and substance use coping. We found significant indirect effects through the following two DERS subscales: Emotional non-acceptance (β = .10, p = .012, CI: .03, .19) and Limited Access to Emotion Regulation Strategies (β = .07, p = .044, CI: .003, .17).
References
- Angermeyer MC, Beck M, Dietrich S, Holzinger A. The stigma of mental illness: Patients’ anticipations and experiences. International Journal of Social Psychiatry. 2004;50:153–162. doi: 10.1177/0020764004043115. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL. Amos (Version 7.0) [Computer Program] Chicago: SPSS; 2006. [Google Scholar]
- Ben-Porath DD. Stigmatization of individuals who receive psychotherapy: An interaction between help-seeking behavior and the presence of depression. Journal of Social and Clinical Psychology. 2002;21:400–413. doi: 10.1521/jscp.21.4.400.22594. [DOI] [Google Scholar]
- Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, Junghanns K. Deficits in emotion-regulation skills predict alcohol use during and after cognitive behavioral therapy for alcohol dependence. Journal of Consulting and Clinical Psychology. 2011;79:307–318. doi: 10.1037/a0023421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Zvolensky MJ. Emotional dysregulation: Association with coping-oriented marijuana use motives among current marijuana users. Substance Use and Misuse. 2008;43:1653–1665. doi: 10.1080/10826080802241292. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Clark TT. Perceived discrimination, depressive symptoms, and substance use in young adulthood. Addictive Behaviors. 2014;39:1021–1025. doi: 10.1016/j.addbeh.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contrada RJ, Ashmore RD, Gary ML, Coups E, Egeth JD, Sewell A, Chasse V. Ethnicity-related sources of stress and their effects on well-being. Current Directions in Psychological Science. 2000;9:136–139. doi: 10.1111/1467-8721.00078. [DOI] [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry. 2006;67:247–257. doi: 10.4088/JCP.v67n0211. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037/0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, George WH. Coping, expectancies, and alcohol abuse: A test of social learning formulations. Journal of Abnormal Psychology. 1988;97:218–230. doi: 10.1037/0021-843X.97.2. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychological Science in the Public Interest. 2014;15:37–70. doi: 10.1177/1529100614531398. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BS, Dohrenwend BP, Dodson M, Shrout PE. Symptoms, hassles, social supports, and life events: Problem of confounded measures. Journal of Abnormal Psychology. 1984;93:222–230. doi: 10.1037/0021-843X.93.2.222. [DOI] [PubMed] [Google Scholar]
- Dvorak RD, Sargent EM, Kilwein TM, Stevenson BL, Kuvaas NJ, Williams TJ. Alcohol use and alcohol-related consequences: Associations with emotion regulation difficulties. American Journal of Drug and Alcohol Abuse. 2014;40:125–130. doi: 10.3109/00952990.2013.877920. [DOI] [PubMed] [Google Scholar]
- Gerrard M, Stock ML, Roberts ME, Gibbons FX, O’Hara RE, Weng CY, Wills TA. Coping with racial discrimination: The role of substance use. Psychology of Addictive Behaviors. 2012;26:550–560. doi: 10.1037/a0027711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M, Cleveland MJ, Wills TA, Brody G. Perceived discrimination and substance use in African American parents and their children: A panel study. Journal of Personality and Social Psychology. 2004;86:517–529. doi: 10.1037/0022-3514.86.4.517. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, O’Hara RE, Stock ML, Gerrard M, Weng CY, Wills TA. The erosive effects of racism: Reduced self-control mediates the relation between perceived racial discrimination and substance use in African American adolescents. Journal of Personality and Social Psychology. 2012;102:1089–1104. doi: 10.1037/a0027404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz K, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediational framework. Psychological Bulletin. 2009;135:707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Nolen-Hoeksema S, Dovidio JF. How does stigma “get under the skin”?: The mediating role of emotion regulation. Psychological Science. 2009;20:1282–1289. doi: 10.1111/j.1467-9280.2009.02441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hides L, Lubman DI, Cosgrave EM, Buckby JA, Killackey E, Yung AR. Motives for substance use among young people seeking mental health treatment. Early Intervention in Psychiatry. 2008;2:188–194. doi: 10.1111/j.1751-7893.2008.00076.x. [DOI] [PubMed] [Google Scholar]
- Knight MTD, Wykes T, Hayward P. Group treatment of perceived stigma and self-esteem in schizophrenia: A waiting list trial of efficacy. Behavioral and Cognitive Therapy. 2006;34:305–318. doi: 10.1017/S1352465805002705. [DOI] [Google Scholar]
- Linehan MM, Schmidt H, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. American Journal of Addiction. 1999;8:279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Link BG. Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations of rejection. American Sociological Review. 1987;52:96–112. doi: 10.2307/2095395. [DOI] [Google Scholar]
- Link BG, Struening E, Cullen FT, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders—An empirical assessment. American Sociological Review. 1989;54:400–423. doi: 10.2307/2095613. [DOI] [Google Scholar]
- Link BG, Streuening EL, Neese-Todd S, Asmussen S, Phelan JC. Stigma as a barrier to recovery: The consequences of stigma for the self-esteem of people with mental illnesses. Psychiatric Services. 2001;52:1621–1626. doi: 10.1176/appi.ps.52.12.1621. [DOI] [PubMed] [Google Scholar]
- Link BG, Wells J, Phelan JC, Yang L. Understanding the importance of “symbolic interaction stigma”: How expectations about the reactions of others adds to the burden of mental illness stigma. Psychiatric Rehabilitation Journal. 2015;38:117–124. doi: 10.1037/prj0000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoma JB, Kohlenberg BS, Hayes SC, Bunting K, Rye AK. Reducing self-stigma in substance abuse through acceptance and commitment therapy: Model, manual development, and pilot outcomes. Addiction Research & Theory. 2009;16:149–165. doi: 10.1080/16066350701850295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Keyes KM. Responses to discrimination and psychiatric disorders among Black, Hispanic, female, and lesbian, gay, and bisexual individuals. American Journal of Public Health. 2010;100:1477–1484. doi: 10.2105/ajph.2009.181586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Schwartz S, Frost DM. Social patterning of stress and coping: Does disadvantaged social statuses confer more stress and fewer coping resources? Social Science and Medicine. 2008;67:368–379. doi: 10.1016/j.socscimed.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal D, Sullivan G, Chekuri L, Allee E, Corrigan PW. Empirical studies of self-stigma reduction strategies: A critical review of the literature. Psychiatric Services. 2012;63:974–981. doi: 10.1176/appi.ps.201100459. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. Major depression among adults. 2016 Retrieved from https://www.nimh.nih.gov/health/statistics/prevalence/major-depression-among-adults.shtml.
- Nolen-Hoeksema S, Harrell ZA. Rumination, depression, and alcohol use: Tests of gender differences. Journal of Cognitive Psychotherapy. 2002;16:391–403. doi: 10.1891/jcop.16.4.391.52526. [DOI] [Google Scholar]
- Pachankis JE, Rendina HJ, Restar A, Ventuneac A, Grov C, Parsons JT. A minority stress–emotion regulation model of sexual compulsivity among highly sexually active gay and bisexual men. Health Psychology. 2015;34:829–840. doi: 10.1037/hea0000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus DJ, Bakhshaie J, Lemaire C, Garza M, Ochoa-Perez M, Valdivieso J, Zvolensky MJ. Negative affectivity and problematic alcohol use among Latinos in primary care: The role of emotion dysregulation. Journal of Dual Diagnoses. 2016;12:137–147. doi: 10.1080/15504263.2016.1172897. [DOI] [PubMed] [Google Scholar]
- Perez CR, Soto JA. Cognitive reappraisal in the context of oppression: Implications for psychological functioning. Emotion. 2011;11:675–680. doi: 10.1037/a0021254. [DOI] [PubMed] [Google Scholar]
- Perlick DA, Rosenheck RA, Clarkin JF, Sirey JA, Salahi J, Struening EL, Link BG. Stigma as a barrier to recovery: Adverse effects of perceived stigma on social adaptation of persons diagnosed with bipolar affective disorder. Psychiatric Services. 2001;52:1627–1632. doi: 10.1176/appi.ps.52.12.1627. [DOI] [PubMed] [Google Scholar]
- Pinel EC. Stigma consciousness: The psychological legacy of social stereotypes. Journal of Personality and Social Psychology. 1999;76:114–128. doi: 10.1037/0022-3514.76.1.114. [DOI] [PubMed] [Google Scholar]
- Quinn DM, Chaudoir SR. Living with a concealable stigmatized identity: The impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health. Journal of Personality and Social Psychology. 2009;97:634–651. doi: 10.1037/a0015815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Rendina HJ, Gamarel KE, Pachankis JE, Ventuneac A, Grov C, Parsons JT. Extending the minority stress model to incorporate HIV-positive gay and bisexual men’s experiences: A longitudinal examination of mental health and sexual risk behavior. Annals of Behavioral Medicine. 2017;51:147–158. doi: 10.1007/s12160-016-9822-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roeloffs C, Sherbourne C, Unutzer J, Fink A, Tang L, Wells KB. Stigma and depression among primary care patients. General Hospital Psychiatry. 2003;25:311–315. doi: 10.1016/S0163-8343(03)00066-5. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychological assessment. 2009;21:486–497. doi: 10.1037/a0017074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell L, Sobell M. Timeline Follow-Back. In: Litten R, Allen J, editors. Measuring Alcohol Consumption. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, Merikangas KR, Kessler RC. Mental disorders as risk factors for substance use, abuse and dependence: Results from the 10-year follow-up of the National Comorbidity Survey. Addiction. 2010;105:1117–1128. doi: 10.1111/j.1360-0443.2010.02902.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RA, Lewis MD, Calkins SD. Reassessing Emotion Regulation. Child Development Perspectives. 2008;2:124–131. doi: 10.1111/j.1750-8606.2008.00054.x. [DOI] [Google Scholar]
- Vogel DL, Wade NG, Haake S. Measuring the self-stigma associated with seeking psychological help. Journal of Counseling Psychology. 2006;53:325–337. doi: 10.1037/0022-0167.53.3.325. [DOI] [Google Scholar]
- Wang K, Weiss NH, Pachankis JE, Link BG. Emotional clarity as a buffer in the association between perceived mental illness stigma and suicide risk. Stigma and Health. 2016;1:252–262. doi: 10.1037/sah0000032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Sullivan TP, Tull MT. Explicating the role of emotion dysregulation in risky behaviors: A review and synthesis of the literature with directions for future research and clinical practice. Current Opinion in Psychology. 2015;3:22–29. doi: 10.1016/j.copsyc.2015.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitbeck LB, Hoyt DR, McMorris BJ, Chen X, Stubben JD. Perceived discrimination and early substance abuse among American Indian children. Journal of Health and Social Behavior. 2001;42:405–424. doi: 10.2307/3090187. [DOI] [PubMed] [Google Scholar]


