Abstract
Acute lymphoblastic leukemia is the most prevalent cancer in children. Novel components to help struggle aggressive malignancies and overcome some side effects of conventional treatments could be a promising strategy. Epigallocatechingallate (EGCG), have attracted the attention of scientists for prevention or treatment of some cancers. Jurkat cells were incubated with the different concentrations of EGCG (30–100 µm) for 24, 48, and 72 h and cell viability was investigated using MTS test. Apoptosis and the level of caspase 3 alterations were evaluated using flowcytometry and expression of Fas by Real Time PCR. EGCG decreased viability of cells with an inhibition concentration (IC50) of 82.8 ± 3.1, 68.8 ± 4 and 59.7 ± 4.8 μM in 24,48 and 72 h. 50, 70 and 100 µM concentrations of EGCG induced apoptosis in about 31, 40 and 71% of the cells, respectively. The mean value of caspase 3 positive cells in the presence of 50, 70 and 100 µm concentrations of EGCG was 19.3 ± 2.9, 29.5 ± 3.1 and 61.2 ± 3.4 respectively compared to 7.8 ± 1.1 in control with a significant difference at 100 µm concentration. Treatment with EGCG for 48 h enhanced the expression of Fas reaching to a significant level at 100 µM concentration. EGCG is effective in decrease cell viability, apoptosis induction and enhancement of caspase 3 and Fas expression level in jurkat cells. A comprehensive understanding of molecular events and pharmacokinetics of the component and experiments in animal models are required for dose determination and its interaction with other components of combination chemotherapy.
Keywords: EGCG, Jurkat cell line, Apoptosis, Caspase 3, Fas
Introduction
Cancer is one of the most prevalent causes of death and is expected to increase from 14.1 million new cases in 2012 to 24 million in 2035 and the most rises will be in developing countries [1]. Acute lymphoblastic leukemia is the most prevalent cancer in children with different incidence according to ethnic and race reaching to about 40 per million in whites [2]. Acute leukemia is an aggressive disease and there is a serious need for novel components to help struggle these malignancies. A promising strategy for cancer prevention is introducing drugs that block the development of cancer. Natural compounds and their derivatives have influenced blood cells and components and have been considered for the treatment of different diseases including cancer [3, 4]. Some extracts of medicinal plants have been used to overcome multidrug resistance [5]. Epigallocatechin-3-gallate (EGCG), a polyphenolic compound, is the most important catechin derived from green tea with anticancer properties against many cancer cell lines [6]. EGCG has been found to comprise about 30% of anti-oxidant capacity of green tea and effectively diminishes cellular injury by reducing free radicals causing oxidative damage [7, 8]. Many studies have demonstrated the anti-oxidant activity of polyphenols in different cells and tissues. Studies have shown that EGCG induces in vitro apoptosis in some cell lines. It has also been demonstrated that EGCG incorporate into the lipid bilayer of the membrane and influence multiple signaling pathways [9]. A key regulator of apoptosis is Fas/Fas ligand system which is one of the major extrinsic apoptosis pathways for T cells. Many plant derivatives have shown their anti-cancer effects on T cell leukemia cell lines, as we have reported increasing apoptosis of this cell line with pterostilbene [10]. EGCG causes cell cycle arrest through regulation of expression of regulatory proteins and inhibition of NFκB activation [11]. Moreover EGCG increases IL23-related DNA repair and activate cytotoxic T cells in tumor. This polyphenolic compound has shown anti-proliferative effects on drug sensitive and resistance small cell lung carcinoma [12]. Differentiated promyelocytic cells have been resistant to EGCG, whereas HL-60 undifferentiated leukemia cells were sensitive in Okada et al. study which is a favorable chemo-therapeutic effect [13]. EGCG is effective on some of the biological pathways such as growth factor signaling, kinase dependent mitogen activated protein and ubiquitin/proteasome pathways [14]. In B cell chronic lymphocytic leukemia, EGCG has increased apoptosis accompanied by caspase-3 activation [15]. On the other hand it can inhibit angiogenesis in some tumors. In the present work, we reported the effect of EGCG on apoptosis through the Fas pathway on a T lymphoblastic leukemia cell line.
Materials and Methods
Cell Culture
Jurkat cells (Pasteur Institute, Iran) were grown in RPMI-1640 culture medium supplemented with 10% fetal calf serum, 0.3 mg/ml glutamine, 100 IU penicillin and 100 µg/ml streptomycin, and kept in a humidified atmosphere containing 5% CO2 at 37°. Cells in the exponential phase were used for all experiments. Cell count was performed by hemocytometer and tripane blue dye.
Analysis of Cell Viability
MTS was used to evaluate cell viability according to Thabrew method [16]. Briefly, Cells at 1 × 104 cells/ml were cultured in a 96-well tissue culture plate and incubated for 24 h. The cells then were treated with different concentrations of EGCG (0–100 µM) for 24, 48 and 72 h in above culture media. MTS was added to each well and cells were incubated for 3 h more at 37 °C in a dark place. The optical density (OD) against the background (culture medium with DMSO) at 490 nm was assessed using ELISA reader (stat fax-2100 awarenes). Each independent experiment was repeated at least three times and the concentration required for a 50% inhibition of growth (IC50) was determined. The OD is relative to the total number of living cells. Normal PBMC was tested along with cell line at the same experimental conditions.
Flowcytometric Analysis of Apoptosis
Apoptosis was detected by flow cytometry with the FITC Annexin V Apoptosis Detection Kit (BD Pharmingen). Briefly, jurkat cells were seeded in a 6 well plate in complete media for 24 h. The cells then treated with different concentrations of EGCG for 48 h, were afterward harvested and washed in PBS twice. 106 cells were re-suspended in 1 ml 1× binding buffer. 105 cells were incubated with 5 µl of FITC-labeled annexin V and PI (propidium iodide) at room temperature in darkness for 20 min, then 400 µl of 1× binding buffer were added. The tube was mixed gently, and kept on ice and analyzed by flow cytometry (PARTEC, Germany). FITC positive cells are apoptotic and could be at first or in final stage of apoptosis. Both populations were recorded as apoptotic cells. Untreated sample was considered as negative control for comparison.
Real Time PCR for Fas Expression
Cells were treated with different concentrations of EGCG or left untreated for 48 h, then harvested. Total RNA was extracted using RNA extraction Biozol method (Bioflux, Japan). Total RNA concentration was determined using Thermo Scientific nanodrop 2000, USA. The extracted RNA was re-suspended in DEPS water and stored at −70 °C for future use. cDNA was synthesized using random hexamers and oligo dt primers according to the manufacturer recommendation (Revert Aid first cDNA synthesis Kit, Thermo Scientific, Finland). An aliquot of the resulting DNA was used for PCR amplification according to previously described method using specific primers to achieve optimal thermal and concentration conditions (Thermocycler ASTEC, PC818, Japan). The amplified PCR products was then analyzed by polyacrylamide gel electrophoresis. Fas and β-actin primers were designed using the Gene Works Sofware Program. Thermal cycling conditions are summarized in Table 1. To evaluate the expression of Fas, quantitative PCR was performed and optimized to an amplification efficiency of more than 95%, Rotor Gene RG 3000 Corbet Research, Australia. The primer sets amplified Fas and β-actin to 174 and 118 bp respectively. Table 2 demonstrates the primers and TaqMan probe sequences. The system generates a real time amplification plot based on the normalized fluorescence signal. The comparative cycle (ct) value of target gene was normalized by subtracting the ct value of β-actin (∆ct). The ∆ct value was used to calculate the relative expression level of Fas to β-actin [17].
Table 1.
Thermal cycling condition of Fas/β-actin
| 95 °C for 10 min |
| 45 cycle of 95 °C for 15 s, 60 °C for 60 s |
Table 2.
Primer and probe sequences
| Gene | Primer and probe sequences | Product size (bp) |
|---|---|---|
| β-Actin | F 5′ AGCCTCGCCTTTGCCGA 3′ | 147 |
| R 5′ CTGGTGCCTGGGGCG 3′ | ||
| Probe FAM CCGCCGCCCGTCCACACCCGCC TAMRA | ||
| Fas | F 5′ TGAAGGACATGGCTTAGAAGTG 3′ | 118 |
| R 5′ GGTGCAAGGGTCACAGTGTT 3′ | ||
| Probe FAM AAACTGCACCCGGACCCAGAATACC TAMRA |
Detection of Caspase 3 Positive Cells
Cells were incubated with different concentrations of EGCG and activated-caspase 3 positive cells were identified using intracellular staining and flowcytometry according to the described method (BD). Briefly, the cells were cultured in a 6-well plate at a concentration of 200,000 cells/well in 2 ml complete media and treated with different concentrations of EGCG for 48 h. The cells were washed and re-suspended in cytofix/cytoperm solution and incubated for 20 min on ice. The cells were washed again with perm/wash buffer and incubated with PE conjugated anti-caspase 3 in a perm/wash buffer suspension at room temperature for 30 min in darkness. After the final wash, the cells were re-suspended in perm/wash buffer and prepared for flowcytometric analysis.
Statistical Analysis
Data were presented as mean ± SD and analyzed by SPSS, version 18, using Kruskal–Wallis and Dunn’s Multiple comparison test. The difference between control and each concentration considered significant if p value <0.05. All experiments were repeated at least 3 independent times. Probit analysis was used for IC50 calculation and GraphPad prizm for Graphs.
Results
EGCG Decreased Cell Viability in a Time- and Dose-Dependent Behavior
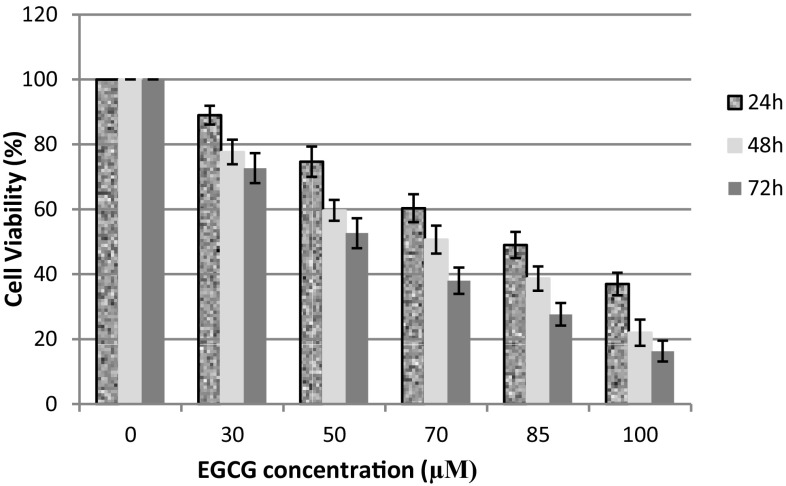
Jurkat cells and PBMC were incubated with various concentrations of EGCG for 24, 48 and 72 h. Decrease of cell viability was observed after incubation time in a dose- and time-dependent behavior (Fig. 1). Jurkat cell viability was about 91, 76, 71%, at a concentration of 30 μM after 24, 48 and 72 h respectively, however viability declined to 37, 22 and 16% at a concentration of 100 μM after above incubation periods. Inhibition concentration (IC50) was 82.82 ± 3.12 μM in 24 h, 68.84 ± 4.03 μM in 48 h and 59.7 ± 4.85 μM in 72 h. Cell viability of normal PBMC did not reach to IC50 as at the highest used concentration, 100 µM, it was still about 65% after 48 h incubation time.
Fig. 1.
Effect of different concentrations of EGCG on viability of Jurkat cell line after 24, 48, and 72 h. Decreased cell viability is time and dose dependent
EGCG Increased Apoptosis of Lymphoblastic Leukemia Cells
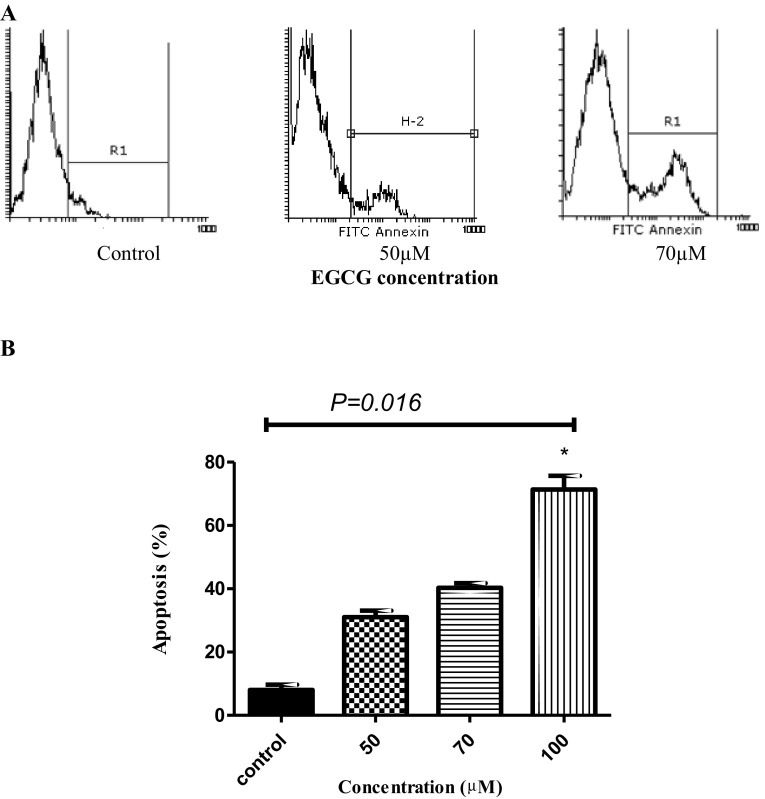
The apoptosis was determined by a double staining method with Annexin V-FITC/PI. Jurkat cells were incubated with various concentrations (0, 50, 70, 100 µM) of EGCG for 48 h. Apoptosis was increased after treatment with different concentrations of the drug compared to control group. Figure 2a shows an example of the apoptosis in the presence of 50 and 70 µM concentration of ECGC. Figure 2b demonstrates the values of 3 independent experiments. 50, 70 and 100 µM concentrations of EGCG induced apoptosis in about 31, 40 and 71% of the cells, respectively.
Fig. 2.
Analysis of apoptosis by flowcytometry. Jurkat cells were treated with EGCG for 48 h and compared to control. a The level of apoptosis was 8.2, 26 and 34% in control, 50 and 70 μM concentrations of EGCG respectively. b The mean value of apoptosis of 3 independent experiments. The effect of different concentrations of EGCG on Jurkat cell apoptosis after 48 h incubation compared to control group. A significant difference was observed in the level of apoptosis between control and the cells treated with 100 μM concentration of EGCG (*a significant difference)
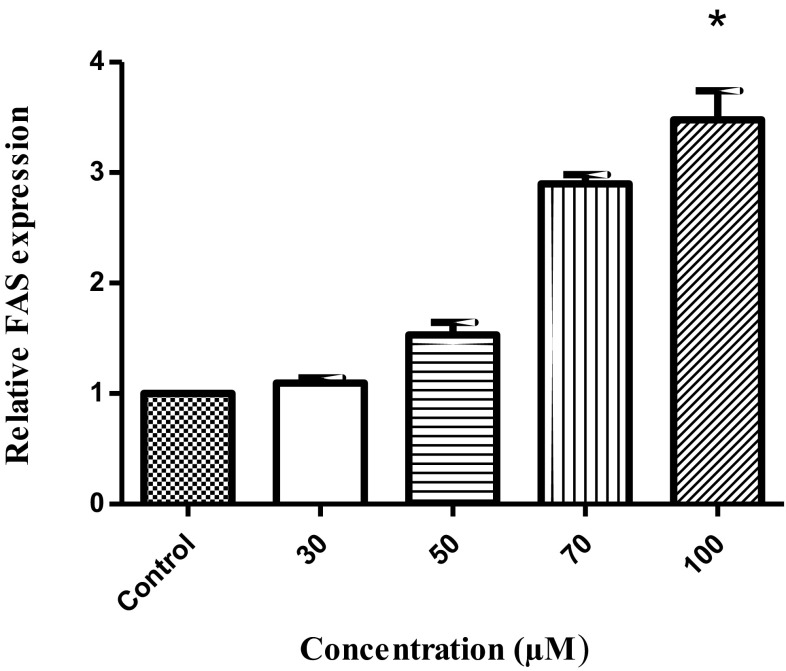
EGCG Enhanced Fas Expression in Jurkat Cells
Cells treated with different concentrations of EGCG. Standard curve in this reaction was established with 5 concentration solutions. Expression levels of β-actin in each solution were analyzed and the expression level of Fas was also detected in the same reaction system. All experiments were performed by three repeats. Fas was expressed at baseline level in untreated cells. Treatment with EGCG enhanced the expression of Fas reaching to a significant level at 100 µM concentration of EGCG. The expression was about 3 times at 70 µM and more than 3 times at 100 µM concentration of EGCG. Treatment with concentrations of more than 100 µM did not exhibit profound Fas expression as there was a massive cell death at higher concentrations. No significant difference was observed among different concentrations (Fig. 3).
Fig. 3.
Effect of EGCG on Fas expression. Jurkat cells were treated with different concentrations of EGCG or left untreated. The Fas expression was more than control at all used concentrations, but the difference was only significant between control and 100 μM concentration
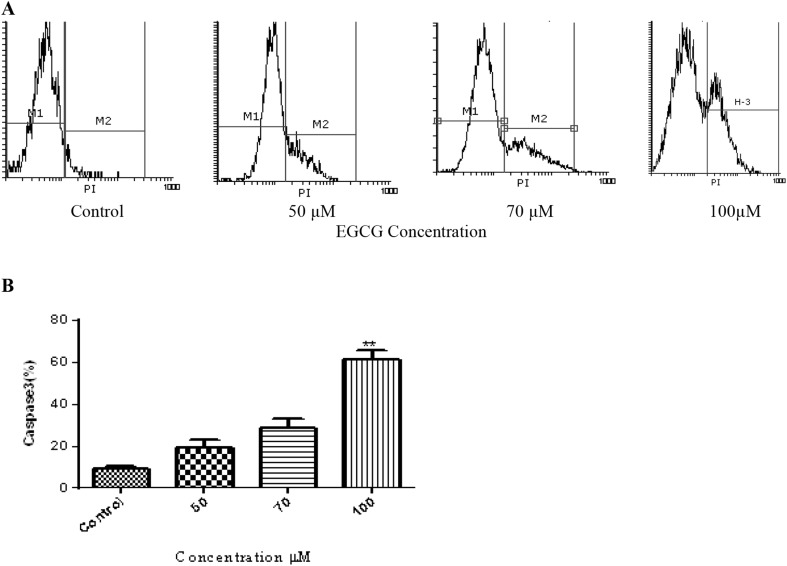
EGCG Increased Caspase 3 Positive Cells
Caspase 3 positive cells were detected by intracellular staining and flowcytometry after the cells were permeablized, fixed and incubated with anti-caspase 3 PE-conjugated monoclonal antibody. The percentage of positive cells was detected by flowcytometry after 48 h incubation with different concentration of EGCG. Figure 4a demonstrates an example of flowcytometric analysis of caspase-3. The mean value of positive cells in three independent experiments in the presence of 50, 70 and 100 µm concentrations of EGCG were compared to control. As shown in Fig. 4b, the mean was 19.3 ± 2.9, 29.5 ± 3.1 and 61.2 ± 3.4 respectively compared to 7.8 ± 1.1 in control. The ratio of positive cells increased in all used concentrations compared to control, but the difference was only significant at 100 µm concentration (Fig. 4b).
Fig. 4.
Effect of EGCG on the level of caspase 3 positive cells. Jurkat cells were incubated with EGCG for 48 h and caspase 3 positive cells were detected by intracellular staining and flowcytometry. a An example of flowcytometric analysis of caspase 3 positive cells. The level of positive cells increased with increasing concentration. b The mean value of positive cells in the presence of 50, 70 and 100 μM concentration of EGCG compared to control. The difference reached to a significant level at 100 μM concentration of EGCG (**). The demonstrated values are the mean of 3 independent experiments
Discussion
The treatment of cancer including leukemia has encountered considerable changes in recent years. New cytotoxic drugs improved the outcome of the patients, but side effects are still the main concern. Polyphenolic compounds of green tea have attracted wide range of researches in recent years and some studies have reported improve of prognosis of some cancers including low grade B cell lymphoma with green tea [18]. Anti-proliferative effect of EGCG through induction of apoptosis has been already reported in some cell lines [19] with variable IC50 based on the cell types. While it has been a potent anti-proliferative agent with an IC50 as low as 4.9 µM in SPC-A-1 human lung carcinoma cell line at 48 h incubation time, others reported moderate effects on proliferation of human retinal pigment epithelial cells [20, 21]. The anti-proliferative effect of EGCG has also been demonstrated on mice spleen cells at concentrations of 2.5–10 µM [22]. In the latter study Li W et al. found cell cycle arrest at G0/G1 rather than increased apoptosis. In hepatocellular carcinoma cell lines cell growth has been inhibited at concentration of 50–100 µM [23]. Since T-ALL has been known as a poor prognosis leukemia we focused of a T lymphoblastic leukemia. Here we demonstrated the decrease of jurkat cell viability with a time and dose dependent manner in the presence of EGCG as we had an IC50 about 70 µM at 48 h and about 60 at 72 h. At a specific time point, the viability decreased parallel to increasing the concentration. Meanwhile we demonstrated less toxic effects on normal PBMC upon EGCG treatment.
The dose dependency is in agreement with Rao and Pagidas in human ovarian cancer cells [24]. Our data showed decrease of cell viability in 24 h as well, starting at 20 µM concentration which is different than that found in pancreatic cell line with 20 and 40 µM concentrations [25]. This finding confirms the difference between different cancer cells and possibly different experimental conditions.
Induction of apoptosis is one of the main approaches in anti-cancer therapy. The present study shows the enhancement of apoptosis in a T cell line with a dose dependent behavior. A concentration of the drug which was associated with more apoptosis also caused more proliferation inhibition in cell viability assay. Green tea catechins are susceptible to autoxidation and accumulates as H2O2 and may influence apoptosis [26]. EGCG has inhibited cycxloxigenase-2 expression in 10–100 µM concentrations in androgen sensitive and insensitive prostatic carcinoma cell lines [14]. Berletch et al. studied the effect of EGCG on MCF-7 breast cancer and HL-60 leukemia cell lines. They found the apoptosis rate at day 9 two times of the control in HL-60 treated cells, however it was more than 11 times in MCF-7 cells. They also found the difference in down regulation of hTERT mRNA between these two cell types [27]. Different sensitivity of the cells to apoptosis may indicate that different mechanisms can be involved in different cell lines. It seems that the diminution of viability in the presence of EGCG in the present work was dependent on the level of apoptosis (vs. necrosis), which is an advantage of anti-cancer treatments.
Fas is a chief extrinsic pathway of apoptosis in T cells. Alteration of some signaling pathways have already been reported and some researchers believe that EGCG by non-specific binds causes protein precipitation [28]. While some studies have indicated the anti-oxidant activity of green tea, others have noticed the hydrogen peroxide production as the main cause of cytotoxic effects. Catalase addition to cell culture has shown to reverse that anti-proliferative effect [29]. EGCG has reported to inhibit proteasome activity in some cancer cells and control the growth of tumor by causing cell cycle arrest at G1. Human normal fibroblasts are not sensitive to this effect [30]. We found enhancement of apoptosis and Fas expression in this T cell leukemia line in the presence of EGCG. This effect has already been found in some other cancer cell lines. Irimie et al. [31] have found the activation of Fas expression in oral carcinoma cells and Wang et al. [32] have revealed the up regulation of Fas and BAX and down regulation of Bcl2. The similar results for the Fas expression have been reported in head and neck squamous cell carcinoma and human breast cancer cells [33, 34]. All of the above findings suggest the Fas/Fas ligand pathway as a mechanism for apoptosis with EGCG. Our findings showed dose-dependency of Fas expression as we had more expression with higher concentrations. The data of caspase-3 detection as the nearly the end-point of this pathway also showed enhancement in the presence of EGCG.
Caspase 3 positive cells were increased in all used concentrations and reached to a significant level at 100 µM concentration of EGCG which is consistent with our data of Fas expression. This finding is in agreement with some other reported cell lines. In rat hepatocytes, caspase 3 activity has been reported to increase in cell lysate after exposure to EGCG in Kucera et al. study [25]. A derivative of EGCG, EGCG-MP, increased the expression of caspase-3 in K562, a promyelocytic leukemia cell line which is in agreement with our data in jurkat cells [35]. The similar results have also been reported in pancreatic and nasopharyngeal cell lines [25, 36].
Overall, we represented that EGCG induces apoptotic effects on a T-cell lymphoblastic line based on the concentration of the drug. This effect is apparently through the apoptosis, but the exact mechanism of EGCG induced apoptosis or cell death is still in question. Since EGCG had minimal toxic effect on normal cells in vitro, it could be considered as a part of combination therapy for ALL to enhance the anti-cancer effect of chemotherapy after in vivo approval in experimental models. More over such a component may allow reducing the dose of chemotherapy agents to exert less cytotoxicity and side effects as we have recently reported the synergistic effect of thymoquinone in combination with doxorubicin (DoX) on T-cell lymphoblastic leukemia cells (jurkat) [37].
Conclusion
In the present work, we provided evidence of the induction of apoptosis through the Fas/Fas ligand activation, however other apoptosis mechanisms may be involved upon EGCG treatment in T cell line which need to be investigated. As EGCG had inhibitory effect on T cell growth, autoimmune diseases can also be a target for future studies. The understanding of molecular events will provide more insights to the development of new therapeutic agents. However more in-depth in vitro experiments are needed with the lymphoblasts of ALL patients and then in vivo studies in animal models. A comprehensive understanding of pharmacokinetics of the component is required for dose determination and its interaction with other components of combination chemotherapy.
Acknowledgements
The authors would like to thank the Deputy of Research and Technology of the Shahrekord University of Medical Sciences for financial support of the project with the Grant No. 1317.
References
- 1.Stewart BW, Bray F, Forman D, Ohgaki H, Straif K, Ullrich A, et al. Cancer prevention as part of precision medicine: ‘plenty to be done’. Carcinogenesis. 2016;37(1):2–9. doi: 10.1093/carcin/bgv166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hunger SP, Mullighan CG. Acute lymphoblastic leukemia in children. N Engl J Med. 2015;373(16):1541–1552. doi: 10.1056/NEJMra1400972. [DOI] [PubMed] [Google Scholar]
- 3.Arreola R, Quintero-Fabian S, Lopez-Roa RI, Flores-Gutierrez EO, Reyes-Grajeda JP, Carrera-Quintanar L, et al. Immunomodulation and anti-inflammatory effects of garlic compounds. J Immunol Res. 2015;2015:401630. doi: 10.1155/2015/401630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shirzad H, Taji F, Pourgheysari B, Raisi S, Rafieian KM (2012) Comparison of antitumour activities of heated and raw garlic extracts on fibrosarcoma in mice. J Babol Univ Med Sci 14(6):77–83
- 5.Senthilkumar R, Chen BA, Cai XH, Fu R. Anticancer and multidrug-resistance reversing potential of traditional medicinal plants and their bioactive compounds in leukemia cell lines. Chin J Nat Med. 2014;12(12):881–894. doi: 10.1016/S1875-5364(14)60131-X. [DOI] [PubMed] [Google Scholar]
- 6.Khan N, Afaq F, Saleem M, Ahmad N, Mukhtar H. Targeting multiple signaling pathways by green tea polyphenol (−)-epigallocatechin-3-gallate. Cancer Res. 2006;66(5):2500–2505. doi: 10.1158/0008-5472.CAN-05-3636. [DOI] [PubMed] [Google Scholar]
- 7.Butt MS, Sultan MT. Green tea: nature’s defense against malignancies. Crit Rev Food Sci Nutr. 2009;49(5):463–473. doi: 10.1080/10408390802145310. [DOI] [PubMed] [Google Scholar]
- 8.Stewart AJ, Mullen W, Crozier A. On-line high-performance liquid chromatography analysis of the antioxidant activity of phenolic compounds in green and black tea. Mol Nutr Food Res. 2005;49(1):52–60. doi: 10.1002/mnfr.200400064. [DOI] [PubMed] [Google Scholar]
- 9.Adachi S, Nagao T, Ingolfsson HI, Maxfield FR, Andersen OS, Kopelovich L, et al. The inhibitory effect of (−)-epigallocatechin gallate on activation of the epidermal growth factor receptor is associated with altered lipid order in HT29 colon cancer cells. Cancer Res. 2007;67(13):6493–6501. doi: 10.1158/0008-5472.CAN-07-0411. [DOI] [PubMed] [Google Scholar]
- 10.Rahimnejad T, Beshkar P, Shirzad H, Rafieiankopaei M, Safdari V, Asgarian Dehkordi N, et al. Effect of pterostilbene on cellular proliferation inhibition and induction of apoptosis in lymphoblastic leukemia cell line. J Babol Univ Med Sci. 2014;16(12):32–38. [Google Scholar]
- 11.Aggarwal BB, Shishodia S. Molecular targets of dietary agents for prevention and therapy of cancer. Biochem Pharmacol. 2006;71(10):1397–1421. doi: 10.1016/j.bcp.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 12.Sadava D, Whitlock E, Kane SE. The green tea polyphenol, epigallocatechin-3-gallate inhibits telomerase and induces apoptosis in drug-resistant lung cancer cells. Biochem Biophys Res Commun. 2007;360(1):233–237. doi: 10.1016/j.bbrc.2007.06.030. [DOI] [PubMed] [Google Scholar]
- 13.Okada N, Tanabe H, Tazoe H, Ishigami Y, Fukutomi R, Yasui K, et al. Differentiation-associated alteration in sensitivity to apoptosis induced by (−)-epigallocatechin-3-O-gallate in HL-60 cells. Biomed Res. 2009;30(4):201–206. doi: 10.2220/biomedres.30.201. [DOI] [PubMed] [Google Scholar]
- 14.Khan N, Mukhtar H. Multitargeted therapy of cancer by green tea polyphenols. Cancer Lett. 2008;269(2):269–280. doi: 10.1016/j.canlet.2008.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee YK, Bone ND, Strege AK, Shanafelt TD, Jelinek DF, Kay NE. VEGF receptor phosphorylation status and apoptosis is modulated by a green tea component, epigallocatechin-3-gallate (EGCG), in B-cell chronic lymphocytic leukemia. Blood. 2004;104(3):788–794. doi: 10.1182/blood-2003-08-2763. [DOI] [PubMed] [Google Scholar]
- 16.Thabrew MI, Hughes RD, McFarlane IG. Screening of hepatoprotective plant components using a HepG2 cell cytotoxicity assay. J Pharm Pharmacol. 1997;49(11):1132–1135. doi: 10.1111/j.2042-7158.1997.tb06055.x. [DOI] [PubMed] [Google Scholar]
- 17.Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc. 2008;3(6):1101–1108. doi: 10.1038/nprot.2008.73. [DOI] [PubMed] [Google Scholar]
- 18.Shanafelt TD, Lee YK, Call TG, Nowakowski GS, Dingli D, Zent CS, et al. Clinical effects of oral green tea extracts in four patients with low grade B-cell malignancies. Leuk Res. 2006;30(6):707–712. doi: 10.1016/j.leukres.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 19.Singh BN, Shankar S, Srivastava RK. Green tea catechin, epigallocatechin-3-gallate (EGCG): mechanisms, perspectives and clinical applications. Biochem Pharmacol. 2011;82(12):1807–1821. doi: 10.1016/j.bcp.2011.07.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alex AF, Spitznas M, Tittel AP, Kurts C, Eter N. Inhibitory effect of epigallocatechin gallate (EGCG), resveratrol, and curcumin on proliferation of human retinal pigment epithelial cells in vitro. Curr Eye Res. 2010;35(11):1021–1033. doi: 10.3109/02713683.2010.506970. [DOI] [PubMed] [Google Scholar]
- 21.Li W, Wu JX, Tu YY. Synergistic effects of tea polyphenols and ascorbic acid on human lung adenocarcinoma SPC-A-1 cells. J Zhejiang Univ Sci B. 2010;11(6):458–464. doi: 10.1631/jzus.B0900355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu D, Guo Z, Ren Z, Guo W, Meydani SN. Green tea EGCG suppresses T cell proliferation through impairment of IL-2/IL-2 receptor signaling. Free Radic Biol Med. 2009;47(5):636–643. doi: 10.1016/j.freeradbiomed.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Nishikawa T, Nakajima T, Moriguchi M, Jo M, Sekoguchi S, Ishii M, et al. A green tea polyphenol, epigallocatechin-3-gallate, induces apoptosis of human hepatocellular carcinoma, possibly through inhibition of Bcl-2 family proteins. J Hepatol. 2006;44(6):1074–1082. doi: 10.1016/j.jhep.2005.11.045. [DOI] [PubMed] [Google Scholar]
- 24.Rao SD, Pagidas K. Epigallocatechin-3-gallate, a natural polyphenol, inhibits cell proliferation and induces apoptosis in human ovarian cancer cells. Anticancer Res. 2010;30(7):2519–2523. [PubMed] [Google Scholar]
- 25.Kostin SF, McDonald DE, McFadden DW. Inhibitory effects of (−)-epigallocatechin-3-gallate and pterostilbene on pancreatic cancer growth in vitro. J Surg Res. 2012;177(2):255–262. doi: 10.1016/j.jss.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 26.Hou Z, Sang S, You H, Lee MJ, Hong J, Chin KV, et al. Mechanism of action of (−)-epigallocatechin-3-gallate: auto-oxidation-dependent inactivation of epidermal growth factor receptor and direct effects on growth inhibition in human esophageal cancer KYSE 150 cells. Cancer Res. 2005;65(17):8049–8056. doi: 10.1158/0008-5472.CAN-05-0480. [DOI] [PubMed] [Google Scholar]
- 27.Berletch JB, Liu C, Love WK, Andrews LG, Katiyar SK, Tollefsbol TO. Epigenetic and genetic mechanisms contribute to telomerase inhibition by EGCG. J Cell Biochem. 2008;103(2):509–519. doi: 10.1002/jcb.21417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shim JH, Choi HS, Pugliese A, Lee SY, Chae JI, Choi BY, et al. (-)-Epigallocatechin gallate regulates CD3-mediated T cell receptor signaling in leukemia through the inhibition of ZAP-70 kinase. J Biol Chem. 2008;283(42):28370–28379. doi: 10.1074/jbc.M802200200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chai PC, Long LH, Halliwell B. Contribution of hydrogen peroxide to the cytotoxicity of green tea and red wines. Biochem Biophys Res Commun. 2003;304(4):650–654. doi: 10.1016/S0006-291X(03)00655-7. [DOI] [PubMed] [Google Scholar]
- 30.Nam S, Smith DM, Dou QP. Ester bond-containing tea polyphenols potently inhibit proteasome activity in vitro and in vivo. J Biol Chem. 2001;276(16):13322–13330. doi: 10.1074/jbc.M004209200. [DOI] [PubMed] [Google Scholar]
- 31.Irimie AI, Braicu C, Zanoaga O, Pileczki V, Gherman C, Berindan-Neagoe I, et al. Epigallocatechin-3-gallate suppresses cell proliferation and promotes apoptosis and autophagy in oral cancer SSC-4 cells. Onco Targets Ther. 2015;8:461–470. doi: 10.2147/OTT.S78358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang J, Xie Y, Feng Y, Zhang L, Huang X, Shen X, et al. (−)-Epigallocatechingallate induces apoptosis in B lymphoma cells via caspase-dependent pathway and Bcl-2 family protein modulation. Int J Oncol. 2015;46(4):1507–1515. doi: 10.3892/ijo.2015.2869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hsu YC, Liou YM. The anti-cancer effects of (−)-epigallocatechin-3-gallate on the signaling pathways associated with membrane receptors in MCF-7 cells. J Cell Physiol. 2011;226(10):2721–2730. doi: 10.1002/jcp.22623. [DOI] [PubMed] [Google Scholar]
- 34.Lin HY, Hou SC, Chen SC, Kao MC, Yu CC, Funayama S, et al. (−)-Epigallocatechin gallate induces Fas/CD95-mediated apoptosis through inhibiting constitutive and IL-6-induced JAK/STAT3 signaling in head and neck squamous cell carcinoma cells. J Agric Food Chem. 2012;60(10):2480–2489. doi: 10.1021/jf204362n. [DOI] [PubMed] [Google Scholar]
- 35.Jung JH, Yun M, Choo EJ, Kim SH, Jeong MS, Jung DB, et al. A derivative of epigallocatechin-3-gallate induces apoptosis via SHP-1-mediated suppression of BCR-ABL and STAT3 signalling in chronic myelogenous leukaemia. Br J Pharmacol. 2015;172(14):3565–3578. doi: 10.1111/bph.13146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fang CY, Wu CC, Hsu HY, Chuang HY, Huang SY, Tsai CH, et al. EGCG inhibits proliferation, invasiveness and tumor growth by up-regulation of adhesion molecules, suppression of gelatinases activity, and induction of apoptosis in nasopharyngeal carcinoma cells. Int J Mol Sci. 2015;16(2):2530–2558. doi: 10.3390/ijms16022530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Soltani A, Pourgheysari B, Shirzad H, Sourani Z (2016) Antiproliferative and apoptosis-inducing activities of thymoquinone in lymphoblastic leukemia cell line. Indian J Hematol Blood Transfus (Epub) [DOI] [PMC free article] [PubMed]