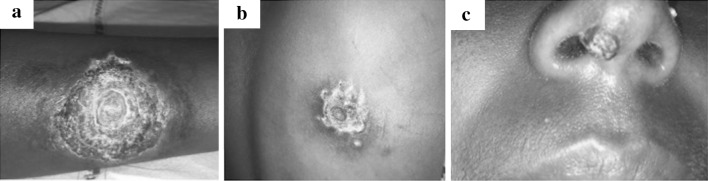
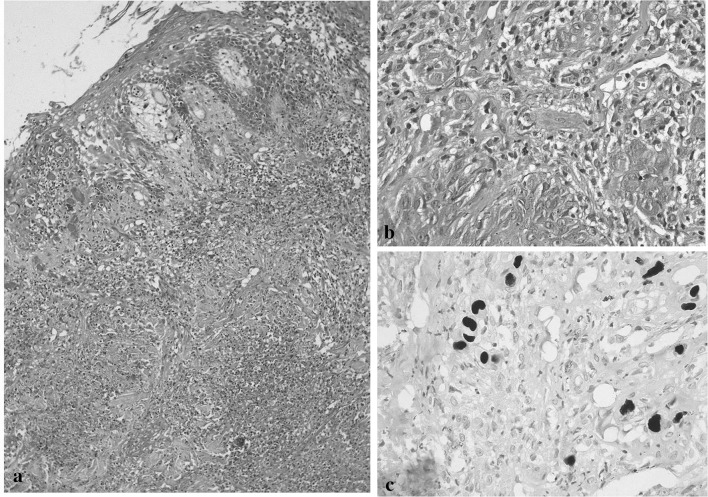
A 15 year-old-girl, known case of Pro T cell acute lymphoblastic leukemia on maintenance chemotherapy (vincristine, methotrexate and 6-mercaptopurine) presented with multiple skin lesions for 3 weeks duration. She had applied antibiotic cream (mupirocin) and taken oral cloxacillin with no relief. She was afebrile and had well-defined proliferating, necrotic, warty lesion with overlying ‘whorled’ crusts on ventral aspect of left forearm measuring 5 × 5 cm with infiltrated and erythematous surrounding skin (Fig. 1a). Similar lesions were also noted on right infra scapular area (4 × 4 cm) (Fig. 1b) and columella of nose (1 × 1 cm) (Fig. 1c). A few satellite lesions were noted (Fig. 1b). She had hemoglobin of 120 g/L, WBC 2.2 × 109/L, platelet 370 × 109/L with normal peripheral blood smear. Possibility of atypical mycobacterial, fungal or viral skin infection was considered. Biopsy from the margin of the left forearm ulcer showed cytoplasmic inclusion bodies with typical ‘owl eye’ appearance suggestive of CMV infection (Fig. 2a), which was confirmed by CMV immunostain (Fig. 2b). CMV DNA PCR was planned but couldn’t be done due to financial constraints. Her chemotherapy was withheld and she received oral valganciclovir 900 mg twice daily. After 3 weeks, she had significantly improved skin lesion.
Fig. 1.
Clinical photograph showing a well-defined proliferating, necrotic, warty lesion with overlying ‘whorled’ crusts on ventral aspect of left forearm with infiltrated and erythematous surrounding skin (a). Similar lesions are also seen on right infra scapular area (b) with few satellite lesions and columella of nose (c)
Fig. 2.
Photomicrographs showing: an ulcerated epidermis with neutrophilic debris in dermis (a) (H&E, ×100); cytomegaly and nuclemegaly with prominent eosinophilc intranuclear inclusions (b) (H&E, ×400); immunostain for CMV highlighting CMV inclusions (c) (CMV immunostain, ×400)
Infection remains an important cause of morbidity and mortality in cases of acute lymphoblastic leukemia in resource constraints settings [1]. Cytomegalovirus belongs to herpesvirus group of DNA viruses. The prevalence of CMV infection is estimated to be 80–90%, however in immunocompetent individuals it remains dormant. In immunocompromised individuals the virus gets reactivated under the influence of high TNF alfa [2] and presents with meningo-encephalitis, retinitis, esophagitis, GI ulcers, pneumonia or skin ulcers. The skin manifestation may be in the form of vesicles, papules, nodules, licheniform lesions, scarlatiform lesions, urticarial lesions or ulcers. CMV infection with skin lesions is rare and difficult to diagnose early due to varied presentation [3]. Timely diagnosis and therapy is also important, as skin manifestation historically has been associated with 80% mortality at 6 months [4]. Due to the high prevalence, serology is usually not helpful in diagnosis or confirmation of CMV disease or reactivation. Characteristic inclusion bodies on histopathological examination are highly suggestive of CMV infection, which can be confirmed by immunohistochemical stains [5]. Valganciclovir 900 mg twice daily for 3 weeks is sufficient to control the viremia and also serves as convenient alternative in carefully selected cases of CMV disease [6]. Its absorption, efficacy and side effect profile is similar to conventionally used intravenous ganciclovir.
Our case is a rare case of CMV infection of the skin due to the unique ‘whorled’ appearance of the lesions. The index case emphasizes the need to think early and think smart when immunocompromised patients present with non-healing skin lesions. Lastly, valganciclovir has simplified the therapy of this bewildering infection and with timely management a favorable clinical outcome can be expected in such patients.
Compliance with Ethical Standards
Conflict of interest
There is no conflict of interest between the authors.
Informed Consent
Informed signed written consent was taken from the patient involved.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and Animals Rights
No animals were involved in the study.
References
- 1.Malhotra P, Varma S, Varma N, Kumari S, Das R, Jain S, Ahluwalia J, Mahi S, Sharma SC, Radhika S. Outcome of adult acute lymphoblastic leukemia with BFM protocol in a resource-constrained setting. Leuk Lymphoma. 2007;48(6):1173–1178. doi: 10.1080/10428190701343255. [DOI] [PubMed] [Google Scholar]
- 2.Malhotra P, Menon MC, Varma N, Mishra B, Saikia UN, Suri V, Varma S. Cytomegalovirus pneumonia in adult acute lymphoblastic leukemia. J Assoc Physicians India. 2008;56:541–542. [PubMed] [Google Scholar]
- 3.Park JH, Oh JJ, Lee ES. Two cases of cutaneous cytomegalovirus infection in immunocompromised patients. Ann Dermatol. 2004;16(2):67–70. doi: 10.5021/ad.2004.16.2.67. [DOI] [Google Scholar]
- 4.Lee JY. Cytomegalovirus infection involving the skin in immunocompromised hosts. A clinicopathologic study. Am J Clin Pathol. 1989;92(1):96–100. doi: 10.1093/ajcp/92.1.96. [DOI] [PubMed] [Google Scholar]
- 5.Fasanya AA, Pedersen FT, Alhassan S, Adjapong O, Thirumala R. Cytomegalovirus cutaneous infection in an immunocompromised patient. Cureus. 2016;8(5):e598. doi: 10.7759/cureus.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lambert EM, Strasswimmer J, Lazova R, Antaya RJ. Cytomegalovirus ulcer. Successful treatment with valganciclovir. Arch Dermatol. 2004;140(10):1199–1201. doi: 10.1001/archderm.140.10.1199. [DOI] [PubMed] [Google Scholar]