Abstract
Chimeric antigen receptor (CAR) T-cell therapy has been clinically proven to efficiently combat haematological malignancies. However, continuous efforts are required to increase the specificity of CAR T-cells against tumour versus normal tissues, and are essential to improve their antitumour activity in solid tumours. This review summarises the structure of major CAR designs, and strategies to overcome immunosuppressive tumour microenvironment, and reduce toxicities. Along with reviewing currently available techniques that allow the elimination of CAR T-cells after they fulfil their desired functions, using suicide genes, drug elimination strategies are also introduced. A better understanding of the strengths and pitfalls of CAR T-cell therapy will provide fundamental knowledge for the improvement of engineered T-cell therapy in the near future.
Keywords: chimeric antigen receptor, CAR T-cell therapy, haematological and solid tumors
Introduction
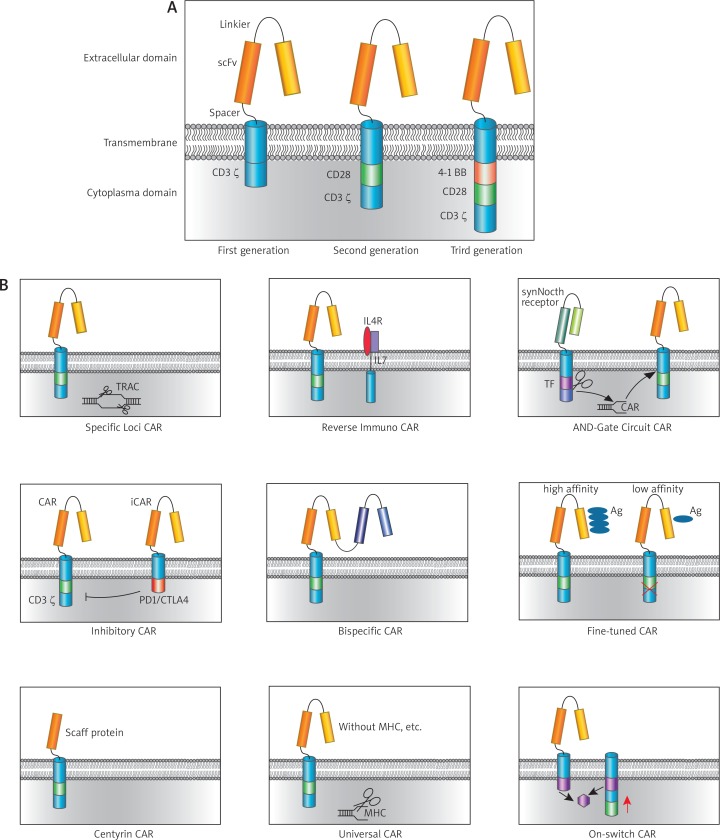
Chimeric antigen receptor (CAR) is one of the fast-developing techniques in immunotherapy, which directs CAR-expressing immune cells (usually T and natural killer cells) to recognise specific target antigens expressed by tumour cells [1–4]. The basic construct of CAR comprises of a signal peptide sequence, the binding moiety (i.e., single chain variable fragment, scFV), and a spacer region at the extracellular domain, a transmembrane domain, and an intracellular signalling domain (i.e., CD3ζ). The first-generation CAR is mainly the fusion of scFv with a CD3ζ cytoplasmic domain. The second- and third- generation CARs incorporate one or more costimulatory domains other than CD3ζ domain, such as CD28, 4-1BB or both, which contributes to prolonged T-cells activation and expansion [5–11]. The constructs of the first-, second- and third- generation CARs are listed in Fig. 1A. Engagement with antigen via scFV leads to the activation of CD3ζ-mediated activation signals and CD28, 4-1BB-mediated costimulatory cascades, which subsequently induce cytotoxic activity of the engineered immune cells.
Fig. 1.
Chimeric antigen receptor (CAR) structure and design. A) Three generations of CARs. CAR compromises 3 domains: extracellular domain; transmembrane domain; and cytoplasmic domain. First generation CAR only has CD3ζ domain; second-generation CAR incorporates CD28 or 4-1BB, while the third-generation CAR incorporates both or more. B) Primary CARs design and evolution
Adoptive T-cell therapy was first employed in 1988 by Rosenberg et al. using ex vivo expanded tumour-infiltrating T-cells (TILs) in melanoma patients [12]. Other researchers also used T-cells expanded from peripheral blood mononuclear cells in tumour immunotherapy [13, 14]. Adoptive transfer of T-cells engineered with scFV specifically targeting CD19 (named as CD19-CAR) made great success in anti-B-cell malignancy [15, 16]. CD19-CAR T-cell therapy was recently approved by the Food and Drug Administration (FDA) for immunotherapy in relapsed and refractory (r/r) B-cell acute lymphoblastic leukaemia (ALL) for paediatric and young adult patients, and for adult patients with r/r diffuse large B-cell lymphoma (DLBCL), who have failed two or more prior therapies. The high response rates in patients treated by CD19-CAR T-cells led to great efforts by researchers and oncologists to design novel CAR constructs based on current available T-cell engineering strategies along with the recently generally used CRISPR/Cas9 method. This review summarises the current progression in CAR T-cell design and its associated T-cell engineering strategies, and discusses the potential of next generation CAR T-cells for haematological tumours to solid tumours (Table 1).
Table 1.
List of CAR targets in haematological and solid tumor
| I. Haematological tumor CAR targets | ||
|---|---|---|
| Target | Gene | Description |
| BCMA | TNFRSF17 | TNF receptor superfamily member 17\B-cell maturation protein |
| CD123 | IL3RA | interleukin 3 receptor subunit α\CD123 antigen |
| CD138 | SDC1 | syndecan 1 |
| CD19 | CD19 | CD19 molecule |
| CD20 | MS4A1 | membrane spanning 4-domains A1 |
| CD22 | CD22 | SIGLEC2 |
| CD38 | CD38 | CD38 molecule |
| CD5 | CD5 | lymphocyte antigen T1/Leu-1 |
| Ig κ chain | IgK | immunoglobulin κ locus |
| LeY | FUT3 | fucosyltransferase 3 (Lewis Blood Group) |
| NKG2D ligand | NKG2D | killer cell lectin like receptor K1/CD314 |
| ROR1 | ROR1 | receptor tyrosine kinase like orphan receptor 1 |
| WT1 | WT1 | Wilms’ tumour antigen 1 |
| II. Solid tumour CAR targets | ||
| Target | Gene | Description |
| C-Met | MET | MET proto-oncogene |
| CAIX | CA9 | carbonic anhydrase 9 |
| CD133 | PROM1 | prominin 1 |
| CD171 | L1CAM | L1 cell adhesion molecule |
| CD70 | CD70 | tumour necrosis factor ligand superfamily member 7 |
| CEA | CEACAM5 | carcinoembryonic antigen related cell adhesion molecule 5 |
| EGFR | EGFR | epidermal growth factor receptor |
| EGFR vIII | EGFRVIII | epidermal growth factor receptor variant 3 |
| Ep-CAM | EPCAM | epithelial cell adhesion molecule |
| EphA2 | EPHA2 | EPH receptor A2 |
| FAP | FAP | fibroblast activation protein α |
| GD2 | disialoganglioside | |
| GPC3 | GPC3 | glypican 3 |
| HER2 | ERBB2 | Erb-B2 receptor tyrosine kinase 2 |
| HPV16-E6 | HPV E6 | human papillomavirus E6 protein |
| IL13Ra2 | IL13RA2 | interleukin 13 receptor subunit α2 |
| LeY | FUT3 | fucosyltransferase 3 (Lewis Blood Group) |
| MAGEA3 | MAGEA3 | MAGE family member A3 |
| MAGEA4 | MAGEA4 | MAGE family member A4 |
| MART1 | MLANA | melan-A |
| Mesothlin | MSLN | mesothelin |
| MUC1 | MUC1 | mucin 1, cell surface associated |
| MUC16 | MUC16 | mucin 16, cell surface associated |
| NY-ESO-1 | CTAG1B | cancer/testis antigen 1B |
| PD-L1 | CD274 | CD274 molecule |
| PSCA | PSCA | prostate stem cell antigen |
| PSMA | FOLH1 | folate hydrolase 1 |
| ROR1 | ROR1 | receptor tyrosine kinase like orphan receptor 1 |
| VEGFR2 | KDR | kinase insert domain receptor/vascular endothelial growth factor receptor 2 |
First generation of CAR
Kuwana and Eshaar first demonstrated that synthetic CARs, fusion of scFv against hapten with a CD3ζ cytoplasmic domain, can overcome MHC restriction and TCR low affinity, leading to more efficient recognition of tumour targets [1, 6]. This is called the first-generation CARs, which included the zeta-chain of the CD3 complex (CD3ζ) that facilitates TCR signal and activates T-cells with modest toxicity. This kind of CARs lack co-stimulatory signals, which limits the proliferating capabilities of T-cell upon exposure to repeated antigens. T-cells with first-generation CARs are easily arrested at the G-G1 phase of the cell cycle, similar to T-cells activated with anti-CD3 alone ex vivo [17].
Second- and third-generation CARs
The introduction of co-stimulatory CD28 or 4-1BB into the signalling domain of CARs led to impressive clinical benefits, especially in B-cell malignancies [8–11]. It is well understood that coupling of CD28 and CD3ζ signals augments TCR signalling, increases cytokine production, promotes proliferation and anti-apoptosis, and affects the epigenetic structure and metabolism of T-cells [8–10]. These functions are mediated by phosphoinositide 3-kinase (PI3K)-AKT pathway and activated following the phosphorylation of the cytoplasmic tails of CD3ζ and CD28. Thus, incorporation of CD28 signals into the second-generation CAR promotes the proliferation and persistence of engineered CAR T-cells in vivo [8–10, 18, 19].
Another strategy is the addition of 4-1BB into the second-generation CAR. 4-1BB can be induced transiently by TCR and CD28 signalling via ERK and JNK signalling pathways. Researchers have found that 4-1BB supports T-cell survival, with effects more evident and durable in CD8+ T-cells than CD4+ T-cells [20–22]. The most important function of 4-1BB signalling is to facilitate memory T-cell formation and robust expansion upon antigen re-stimulation [23, 24]. When comparing CD28 and 4-1BB CARs, Sadelain et al. found that both two second-generation CARs demonstrated similar anti-tumour effect, while 4-1BB CARs persisted longer in vivo even after the tumour had been eradicated [7, 19, 25].
In addition to CD28 and 4-1BB, other co-stimulatory molecules were also introduced into CARs signalling domains, including CD27, OX-40, ICOS, CD40L, CD137, LAP10, etc. [19, 26–28]. When more than two co-stimulatory signalling are incorporated in addition to CD3ζ in CARs, they are named the third-generation CARs. The effects of different constructs are still under investigation due to limited data. The paragraphs below will introduce different designs CARs currently under investigation (Fig. 1B).
wTarget CARs to specific loci
Current CARs vectors are delivered into T-cells via mammalian plasmid transfection, mRNA transfection, viral transduction, or transposon/transposase [29–36]. The random integration of CAR into the host genome may cause severe harmful results, such as clonal expansion, oncogenic transformation, unpredicted transgene expression, and gene silencing. To avoid the above-mentioned uncontrolled events, Sadelain et al. used the CRISPR/Cas9 method to guide the integration of CD19-CAR into a specific TCRα constant (TRAC) locus [37]. In a mouse model of acute lymphoblastic leukaemia, they showed that the TRAC-CAR T-cells induced greater responses and more prolonged survival than randomly transduced CARs. In addition, T-cells with engineered TRAC-CAR presented more memory characteristics and less exhausted phenotype. The locus-targeted CAR demonstrated optimal expression of CARs on the T-cell surface. The TRAC-CAR dynamic expression seems to be regulated by the TCR enhancer/promotor in response to repeated stimulation by antigen, mimicking a natural procedure of TCR regulation [37]. This study is an example of a successful T-cell genome editing by CRISPR/Cas9. However, similar strategies have not been extrapolated in clinical settings and the associated side effects are unclear.
Reverse immunosuppressive CAR
Tumours can employ an immune suppressive microenvironment to evade host immune cells cytotoxicity. Tumours and their surrounding matrix produce inhibitory cytokines, including interleukin-4 (IL-4), IL-10, TGF-β, and leukaemia inhibiting factor (LIF), which promote tumour growth and protect the tumour from immune destruction [38, 39]. One of the obstructs that limit CARs function in solid tumour is the inhibitory tumour microenvironment. In order to reverse the suppressive situation, Mohammed, et al. re-engineered their prostate stem cell antigen (PSCA-) CAR by expression of IL-4 receptor on the T-cell surface with cytoplasmic domain replaced by IL-7 (4/7 ICR T-cells). In the presence of IL-4 and OKT3 (both of which mimic tumour inhibitory factors and tumour antigen), they found that CAR T-cells not only proliferated but also expanded in the absence of IL-2. In an in vivo study, the 4/7 ICR PSCA-CAR T-cells showed more effective memory features, superior antitumour activity, and increased expansion, compared to CAR without 4/7 ICR. Thus, the inhibitory effects of tumour derived IL-4 inverted into T-cell proliferation and enhanced the PSCA-CARs antitumour activity [40]. Another advantage of this strategy is to limit the off-target effects of CAR T-cells to tumour antigens expressed at low level in normal tissues that are not enriched with inhibitory factors (IL-4). These results suggest that a combination of costimulatory molecules with anti-inhibitory signals in the CAR-signalling domain may further improve the clinical benefits of CAR T-cell therapy. However, this strategy does not work in second-generation CARs with CD3ζ and CD28 due to unidentified mechanisms.
Pressor et al. replaced PD-1 signalling domain with CD28 counterpart on CTLs; when PD-L1 on tumour cells engaged with the altered PD-1 on CTLs, enhanced CTL cytotoxicity was confirmed [41]. In a similar vein, the PD1/CD28 signalling domain swap has successfully transferred to CAR engineering, and PD1/CD28 PSCA-CARs outperformed the conventional PSCA-CAR alone or PD1 antibodies [42]. Several groups also reported enhanced cytotoxicity by the depletion or knockdown of PD1 in CAR T-cells in solid tumour models [43, 44]. Therefore, transgenic expression of two factors may increase CARs specificity, and invert more inhibitory factors simultaneously in solid tumours.
Combinational antigen recognition: dual CAR AND-Gate
Determination of tumour-specific surface antigens is the most critical step for CAR specificity. Very rare tumour surface antigens express exclusively in tumour tissues; and even tiny amounts of some “so-called” tumour-specific antigens in normal tissues or organs will cause severe side effects or even lethal results upon infusion of large quantities of CARs T-cells. Distinct strategies have been used to develop CARs, referred to as dual CAR AND-gate, that simultaneously recognises two or more tumour-specific antigens [45, 46]. This type of CAR T-cells mediates more specific killing of target cells that bear both antigens, with low efficacy in tissues that express either antigen alone, thus reducing the undesirable side effects. A more recent strategy in the dual CAR AND-gate used a synthetic Notch (synNotch) receptor carrying the binding moiety for one antigen, whose activation can subsequently induce the expression of a second CAR. Upon engagement with the first antigen, the synNotch receptor automatically clips its cytoplasmic domain and gains transcription factor function. This process in turn induces the second CAR expression in 4 hours [47]. The method showed high efficiency to clear the tumour cells expressing both antigens, and left the normal tissues unattacked. Such methods open the possibility that tumours could be targeted based on multiple antigens. Furthermore, synNotch receptor could also be used to induce effective molecules and downstream genes to tumours sites [47–50].
Inhibitory CARs (iCAR): brake of CARs
Inhibitory CAR (iCAR) is normally delivered together with conventional CAR into T-cells. iCAR recognises a distinct antigen from conventional CAR, and its scFV is fused to PD-1 or CTLA-4 cytoplasmic domain. When the targeT-cells express CAR-specific antigen, CARs are activated and execute cytotoxicity; when targeT-cells express both antigens, iCARs are activated and transmit negative signals that dampens the function of the CARs [51]. iCAR is used to reduce the bystander killing by targeting proteins that are expressed on healthy tissues, but reduced in tumours.
Bispecific CARs
Tumour antigens often evolve during tumourigenesis due to somatic mutations and epigenetic modifications. For example, patients treated with CD19-CARs relapse due to CD19 loss. Therefore, another tumour antigen is required to enhance CARs efficacy. A number of researchers designed a bispecific CARs that fused two scFv, which can recognise dual antigens. CD19-CD20-CAR T-cells were able to control both wild-type B-cell lymphoma and CD19-mutants with equal efficiency in vivo [52]. Another group constructed a CD19-HER2-CAR, which simultaneously targets the CD19 and the human epidermal growth factor receptor 2 (HER2). The efficacy of CD19-HER2-CAR was determined in a mouse model of B-cell lymphoma, which induces distinct T-cell reactivity against each antigen, and synergistic enhancement of effector functions when both antigens were presented [53]. The bispecific CARs help to overcome the inefficiency of adoptive cell therapy due to the loss of tumour antigens.
Affinity-tuned CARs
Based on antibody-antigen affinity, one can screen antibodies that discriminate antigens expressed at different density in normal tissue versus tumour. The CAR with low-affinity scFv selectively targets cells overexpressing EGFR, but shows no effects on cells with lower levels of EGFR [54]. Through such a strategy, the application of affinity-tuned scFvs in CARs offers a wider range of choices against antigens that are physiologically present in normal tissues but are remarkably upregulated in tumours.
Synthetic binding proteins CARs
Over the last two decades, great progress has been achieved in technologies involving synthetic binding proteins. Several platforms have been reported in generating proteins to diverse targets with high affinity and specificity, which are superior to antibodies in terms of smaller size and freedom from disulphide bond formation. Centyrin is one type of scaffold molecules being engineered to bind to target proteins with an interface of similar size to those used by antibodies. Janssen Biotech has developed a number of Centyrin libraries that are used for in vitro selection of Centyrin molecules that bind to targets with high affinity and specificity [55]. Recently, Janssen Biotech has authorised Poseida to develop Centyrin-based CARs, a B-cell maturation antigen (BCMA)-specific Centyrin has been developed to replace scFv part in the CAR construct. So far, little information about Centyrin CARs has been disclosed publicly, but our laboratory cooperating with Poseida has found that BCMA-specific Centyrin-based CAR treat has demonstrated similar effects to conventional CAR in treating multiple myeloma. In addition to Centyrin, there are also other well-established synthetic binding protein platforms, such as Monobodies, Anticalin, Affibody, and DARPin [56]. They all have the potential to be applied in biomedical fields that traditionally use antibodies.
Universal CARs
Conventional CARs are engineered and generated from autologous T-cells, and they are relatively safe in comparison to allogeneic cell transplantation, which commonly induce graft-versus-host-disease (GVHD). On the other hand, adoptively transferred T-cells also express major histocompatibility complex (MHC) class I, which can be attacked by allogeneic host T-cells to mount host-versus-graft disease (HVGD) [57]. However, the generation of autologous CAR T-cells is time-consuming and expensive, and depends heavily on the availability of patient-derived T-cells. To circumvent this problem, researchers explored ways to eliminate TCRs and MHC-related molecules on CAR T-cells, which can help to minimise GVHD and HVGH when infused into allogeneic recipients. Based on this idea, Cooper et al. knocked out TCR α/β chains by Sleeping Beauty transposon/transposase system. As expected, the allogeneic TCR-CD19-CAR T-cells are deficient in TCR signalling, but retained the capability to respond to CD19-expressing tumour [58]. Later, they completely disrupted HLA-I molecules in CAR T-cells and human embryonic stem cells by zinc finger nucleases assay, which allows the application of allogeneic CAR T-cells from a single donor into multiple recipients [29]. The CRISPR/Cas9 system greatly facilitated T-cell engineering as a simple and highly efficient way for multi genomic loci editing [59, 60]. Recent studies reported that CRISPR/Cas9 can be used to eliminate TCR, β-2 m, and PD-1 triple loci simultaneously in CAR T-cells [61], which demonstrated significantly reduced allogeneic reactivity and enhanced anti-tumour function [62].
Side effects of CAR T-cell therapy
Due to the limited data for other CARs, we will focus our discussion on CD19-CARs in this section. The major side effects of CD10-CARs in the clinic include cytokine release syndrome (CRS), neurological toxicity, and anaphylaxis. Toxicity control has become a critical step in CAR T-cell therapy.
Cytokine release syndrome (CRS): Corticosteroids could rapidly reverse CRS without compromising the desired antitumour effects. However, prolonged exposure to high-dose corticosteroids will result in severe side effects. IL-6 receptor-neutralising antibody, tocilizumab, has also been approved by FDA to reduce CRS [15, 63]. In addition, one dose of methylprednisolone is used to directly block T-cell activation and stop CAR T-cell therapy, when tocilizumab fails to control CRS [63].
Neurologic symptoms: The causative pathophysiology of neurologic side effects remains unknown. It is hypothesised that elevated cytokines leads to neurological toxicity. No direct CAR T-cell-mediated toxicity has been observed in the central nervous system. In most cases, the neurological side effects are often self-limiting without treatment [64].
B-cell aplasia: CD19-CAR T-cells kill not only tumour cells expressing CD19, but also normal CD19+ B cells. Therefore, patients who receive CD19 CAR T-cells therapy will develop B-cell aplasia, leading to hypogammaglobulinaemia. To prevent secondary infections caused by B-cell aplasia, IV immunoglobulin infusion is administered monthly to patients as long as aplasia persists [65].
Immunogenicity-related toxicity is another issue that requires attention. A case report showed that human anti-mouse IgG antibody (target mouse original scFV) responses were elicited following infusion of CAR T-cells [30]. It was the same group that found that CAR T-cell infusion can also induce anaphylaxis and cardiac arrest, which is probably due to IgE antibodies specific to the CAR [32].
Control systems in CARs
Despite of the above-mentioned strategies to control CAR-associated over activation, selective depletion of engineered CARs is an alternative strategy under massive investigation.
Suicide genes: To quickly remove infused CAR T-cells to avoid T-cells over activation, suicide genes are introduced in the construct of CARs. Fas and human inducible caspase 9 (iCasp9) are two suicide genes that have been investigated, which can be triggered by small molecules to cause T-cell apoptosis. Previous studies demonstrated an iCasp9 dimerising agent (AP1903) could eliminate 90% of iCasp9-engineered T-cells within 30 minutes following administration of a single dose [66-68].
Elimination genes: Another strategy to eliminate T-cells is to engineer a targetable moiety in genetically modified T-cells. For example, CAR T-cells can be enforced to overexpress CD20 and which can be targeted by rituximab. The CD20-expressing CAR T-cells will be eliminated through antibody-dependent T-cellular cytotoxicity (ADCC), upon infusion of rituximab. Such a strategy is also used by EGFR, which can be targeted by cetuximab, an FDA-approved mAb. Marin et al. reported that iCasp9 and CD20 are the most efficient controlling molecules that can induce rapid cell-death with sound safety and superior efficacy [69, 70].
ON-switch CAR
ON-switch CAR comprises two physically separate constructs, one containing the conventional CAR but with the CD3ζ activation domain is replaced by an inducible binding domain, and the other one contains the CD3ζ domain but lacks the antigen recognition scFC portion. The activity of ON-switch CAR is triggered by orally-administered small molecules on a dose-dependent manner. When a small molecule is administered, the split constructs form heterodimer, which subsequently activates T-cells [71]. ON-switch CAR yields antigen-specific and titratable killing of target T-cells depending on the dose of small molecules. Such a strategy can allow physicians to control CAR responses feasibly.
Challenges in solid tumour
CAR T-cells therapy has demonstrated remarkable success in haematological malignancies, but has limited effects in solid tumours. First, identification of antigens uniquely expressed in solid tumours remains as the critical challenge. Ideal tumour antigens should be expressed exclusively in tumours but not in normal tissues, or at least much more robust in tumour than in normal tissues. So far, nearly 30 antigens for solid tumours are currently under investigation as targets for CAR T-cell therapy [19, 28, 48, 72]. Second, tumour microenvironment in solids presents more complex suppressive factors than haematological malignancies, which impairs the trafficking and infiltration of CAR T-cells through mechanisms involving oxidative stress, nutrient starvation, low pH, and hypoxia [38, 73]. Third, inhibitory soluble proteins, including adenosine, Prostaglandin E2 (PEG2), TGF-β, and IL-10, secreted by tumour and tumour stromal cells suppress the function of CAR T-cells [38, 73]. Fourth, suppressive immune cells within solid tumour microenvironment, including Tregs, myeloid-derived suppressor cells, and tumour-associated macrophages/neutrophils are known to present as a barrier against CAR T-cell function. Thus, CAR T-cell design should combine strategies to overcome these negative factors, or should use strategies in combination with immune checkpoint blockade or other approaches [19, 26, 38, 48, 73, 74].
Perspectives
The CD19 CAR T-cell therapy is a revolutionary treatment in haematological malignancies [16, 75–77], as shown by the unprecedented response rate. The success of CAR T-cells in clinics has inspired tremendous interests of physicians, translational researchers, as well as industries to identify new targets for tumour immunotherapy. A range of versatile CAR constructs targeting a variety of novel tumour antigens have been reported and some of them are tested in phase I/II clinical trials. However, more optimised designs of CARs are required to reduced toxicity, multiply targeting, and increase cost-benefit efficiency, etc. With advanced technologies, such as CRISPR/Cas9, universal CAR T-cells with improved efficacy could be developed and applied in the near future.
Footnotes
The authors declare no conflict of interest.
References
- 1.Kuwana Y, Asakura Y, Utsunomiya N, Nakanishi M, Arata Y, Itoh S, Nagase F, Kurosawa Y. Expression of chimeric receptor composed of immunoglobulin-derived V resions and T-cell receptor-derived C regions. Biochem Biophys Res Commun. 1987;149:960–68. doi: 10.1016/0006-291x(87)90502-x. [DOI] [PubMed] [Google Scholar]
- 2.Gross G, Waks T, Eshhar Z. Expression of immunoglobulin-T-cell receptor chimeric molecules as functional receptors with antibody-type specificity. Proceedings of the National Academy of Sciences. 1989;86:10024–8. doi: 10.1073/pnas.86.24.10024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uherek C, Tonn T, Uherek B, Becker S, Schnierle B, Klingemann HG, Wels W. Retargeting of natural killer–cell cytolytic activity to ErbB2-expressing cancer cells results in efficient and selective tumour cell destruction. Blood. 2002;100:1265–73. [PubMed] [Google Scholar]
- 4.Imai C, Iwamoto S, Campana D. Genetic modification of primary natural killer cells overcomes inhibitory signals and induces specific killing of leukemic cells. Blood. 2005;106:376–83. doi: 10.1182/blood-2004-12-4797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brocker T, Peter A, Traunecker A, Karjalainen K. New simplified molecular design for functional T cell receptor. Eur J Immunol. 1993;23:1435–9. doi: 10.1002/eji.1830230705. [DOI] [PubMed] [Google Scholar]
- 6.Eshhar Z, Waks T, Gross G, Schindler DG. Specific activation and targeting of cytotoxic lymphocytes through chimeric single chains consisting of antibody-binding domains and the gamma or zeta subunits of the immunoglobulin and T-cell receptors. Proc Natl Acad Sci U S A. 1993;90:720–4. doi: 10.1073/pnas.90.2.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sadelain M, Brentjens R, Riviere I. The promise and potential pitfalls of chimeric antigen receptors. Curr Opin Immunol. 2009;21:215–23. doi: 10.1016/j.coi.2009.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krause A, Guo HF, Latouche JB, Tan C, Cheung NK, Sadelain M. Antigen-dependent CD28 Signaling Selectively Enhances Survival and Proliferation in Genetically Modified Activated Human Primary T Lymphocytes. J Exp Med. 1998;188:619–26. doi: 10.1084/jem.188.4.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hombach A, Wieczarkowiecz A, Marquardt T, Heuser C, Usai L, Pohl C, Seliger B, Abken H. Tumour-Specific T Cell Activation by Recombinant Immunoreceptors: CD3ζ Signaling and CD28 Costimulation Are Simultaneously Required for Efficient IL-2 Secretion and Can Be Integrated Into One Combined CD28/CD3ζ Signaling Receptor Molecule. J Immunol. 2001;167:6123–31. doi: 10.4049/jimmunol.167.11.6123. [DOI] [PubMed] [Google Scholar]
- 10.Maher J, Brentjens RJ, Gunset G, Rivière I, Sadelain M. Human T-lymphocyte cytotoxicity and proliferation directed by a single chimeric TCR[zeta]/CD28 receptor. Nat Biotech. 2002;20:70–5. doi: 10.1038/nbt0102-70. [DOI] [PubMed] [Google Scholar]
- 11.Imai C, Mihara K, Andreansky M, Nicholson IC, Pui CH, Geiger TL, Campana D. Chimeric receptors with 4-1BB signaling capacity provoke potent cytotoxicity against acute lymphoblastic leukemia. Leukemia. 2004;18:676–84. doi: 10.1038/sj.leu.2403302. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberg SA, Packard BS, Aebersold PM, et al. Use of tumour-infiltrating lymphocytes and interleukin-2 in the immunotherapy of patients with metastatic melanoma. N Engl J Med. 1988;319:1676–80. doi: 10.1056/NEJM198812223192527. [DOI] [PubMed] [Google Scholar]
- 13.Hunder NN, Wallen H, Cao J, et al. Treatment of Metastatic Melanoma with Autologous CD4+ T Cells against NY-ESO-1. N Engl J Med. 2008;358:2698–703. doi: 10.1056/NEJMoa0800251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lizée G, Overwijk WW, Radvanyi L, Gao J, Sharma P, Hwu P. Harnessing the Power of the Immune System to Target Cancer. Annu Rev Med. 2013;64:71–90. doi: 10.1146/annurev-med-112311-083918. [DOI] [PubMed] [Google Scholar]
- 15.Davila ML, Riviere I, Wang X, Dey P, Selvaraj P. Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci Trans Med. 2014;6:224ra225–224ra225. doi: 10.1126/scitranslmed.3008226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maude SL, Frey N, Shaw PA, et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med. 2014;371:1507–17. doi: 10.1056/NEJMoa1407222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jenkins MK, Burrell E, Ashwell JD. Antigen presentation by resting B cells. Effectiveness at inducing T cell proliferation is determined by costimulatory signals, not T cell receptor occupancy. J Immunol. 1990;144:1585–90. [PubMed] [Google Scholar]
- 18.Boomer JS, Green JM. An Enigmatic Tail of CD28 Signaling. Cold Spring Harbor Perspectives in Biology. 2010:2. doi: 10.1101/cshperspect.a002436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van der Stegen SJC, Hamieh M, Sadelain M. The pharmacology of second-generation chimeric antigen receptors. Nat Rev Drug Discov. 2015;14:499–509. doi: 10.1038/nrd4597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Takahashi C, Mittler RS, Vella AT. Cutting Edge: 4-1BB Is a Bona Fide CD8 T Cell Survival Signal. J Immunol. 1999;162:5037–40. [PubMed] [Google Scholar]
- 21.Dawicki W, Bertram EM, Sharpe AH, Watts TH. 4-1BB and OX40 Act independently to facilitate robust CD8 and CD4 recall responses. J Immunol. 2004;173:5944–51. doi: 10.4049/jimmunol.173.10.5944. [DOI] [PubMed] [Google Scholar]
- 22.Lee SW, Park Y, Song A, Cheroutre H, Kwon BS, Croft M. Functional dichotomy between OX40 and 4-1BB in modulating effector CD8 T cell responses. J Immunol. 2006;177:4464–72. doi: 10.4049/jimmunol.177.7.4464. [DOI] [PubMed] [Google Scholar]
- 23.Shuford WW, Klussman K, Tritchler DD, et al. 4-1BB Costimulatory signals preferentially induce CD8+/T cell proliferation and lead to the amplification in vivo of cytotoxic T cell responses. J Exp Med. 1997;186:47–55. doi: 10.1084/jem.186.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hendriks J, Xiao Y, Rossen JWA, van der Sluijs KF, Sugamura K, Ishii N, Borst J. During viral infection of the respiratory tract, CD27, 4-1BB, and OX40 collectively determine formation of CD8+ memory T cells and their capacity for secondary expansion. J Immunol. 2005;175:1665–76. doi: 10.4049/jimmunol.175.3.1665. [DOI] [PubMed] [Google Scholar]
- 25.Carpenito C, Milone MC, Hassan R, et al. Control of large, established tumour xenografts with genetically retargeted human T cells containing CD28 and CD137 domains. Proc Natl Acad Sci U S A. 2009;106:3360–5. doi: 10.1073/pnas.0813101106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hinrichs CS, Restifo NP. Reassessing target antigens for adoptive T-cell therapy. Nat Biotech. 2013;31:999–1008. doi: 10.1038/nbt.2725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morello A, Sadelain M, Adusumilli PS. Mesothelin-Targeted CARs: Driving T Cells to Solid Tumours. Cancer Discovery. 2016;6:133–46. doi: 10.1158/2159-8290.CD-15-0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sadelain M, Riviere I, Riddell S. Therapeutic T cell engineering. Nature. 2017;545:423–31. doi: 10.1038/nature22395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Torikai H, Reik A, Soldner F, et al. Toward eliminating HLA class I expression to generate universal cells from allogeneic donors. Blood. 2013;122:1341–9. doi: 10.1182/blood-2013-03-478255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beatty GL, Haas AR, Maus MV, et al. Mesothelin-Specific Chimeric Antigen Receptor mRNA-Engineered T Cells Induce Antitumour Activity in Solid Malignancies. Cancer Immunol Res. 2014;2:112–20. doi: 10.1158/2326-6066.CIR-13-0170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGarrity GJ, Hoyah G, Winemiller A, et al. Patient monitoring and follow-up in lentiviral clinical trials. J Gene Med. 2013;15:78–82. doi: 10.1002/jgm.2691. [DOI] [PubMed] [Google Scholar]
- 32.Maus MV, Haas AR, Beatty GL, Albelda SM, Levine BL, Liu X, Zhao Y, Kalos M, June CH. T Cells Expressing Chimeric Antigen Receptors Can Cause Anaphylaxis in Humans. Cancer Immunol Res. 2013;1:26–31. doi: 10.1158/2326-6066.CIR-13-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nakazawa Y, Huye LE, Salsman VS, et al. PiggyBac-mediated cancer immunotherapy using EBV-specific cytotoxic T-cells expressing HER2-specific chimeric antigen receptor. Mol Ther. 2011;19:2133–43. doi: 10.1038/mt.2011.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raja Manuri PV, Wilson MH, Maiti SN, et al. piggyBac Transposon/Transposase System to Generate CD19-Specific T Cells for the Treatment of B-Lineage Malignancies. Hum Gene Ther. 2010;21:427–37. doi: 10.1089/hum.2009.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yoon SH, Lee JM, Cho HI, Kim EK, Kim HS, Park MY, Kim TG. Adoptive immunotherapy using human peripheral blood lymphocytes transferred with RNA encoding Her-2/neu-specific chimeric immune receptor in ovarian cancer xenograft model. Cancer Gene Ther. 2008;16:489–497. doi: 10.1038/cgt.2008.98. [DOI] [PubMed] [Google Scholar]
- 36.Boissel L, Betancur M, Wels WS, Tuncer H, Klingemann H. Transfection with mRNA for CD19 specific chimeric antigen receptor restores NK cell mediated killing of CLL cells. Leuk Res. 2009;33:1255–9. doi: 10.1016/j.leukres.2008.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eyquem J, Mansilla-Soto J, Giavridis T, et al. Targeting a CAR to the TRAC locus with CRISPR/Cas9 enhances tumour rejection. Nature. 2017;543:113–7. doi: 10.1038/nature21405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rabinovich GA, Gabrilovich D, Sotomayor EM. Immunosuppressive strategies that are mediated by tumour cells. Ann Rev Immunol. 2007;25:267–96. doi: 10.1146/annurev.immunol.25.022106.141609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leen AM, Sukumaran S, Watanabe N, et al. Reversal of tumour immune inhibition using a chimeric cytokine receptor. Mol Ther. 2014;22:1211–20. doi: 10.1038/mt.2014.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mohammed S, Sukumaran S, Bajgain P, et al. Improving Chimeric Antigen Receptor-Modified T Cell Function by Reversing the Immunosuppressive Tumour Microenvironment of Pancreatic Cancer. Mol Ther. 2017;25:249–58. doi: 10.1016/j.ymthe.2016.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prosser ME, Brown CE, Shami AF, Forman SJ, Jensen MC. Tumour PD-L1 co-stimulates primary human CD8+ cytotoxic T cells modified to express a PD1:CD28 chimeric receptor. Mol Immunol. 2012;51:263–72. doi: 10.1016/j.molimm.2012.03.023. [DOI] [PubMed] [Google Scholar]
- 42.Liu X, Ranganathan R, Jiang S, et al. A Chimeric Switch-Receptor Targeting PD1 Augments the Efficacy of Second-Generation CAR T Cells in Advanced Solid Tumours. Cancer Res. 2016;76:1578–1590. doi: 10.1158/0008-5472.CAN-15-2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen N, Morello A, Tano Z, Adusumilli PS. CAR T-cell intrinsic PD-1 checkpoint blockade: A two-in-one approach for solid tumour immunotherapy. OncoImmunology. 2017;6:e1273302. doi: 10.1080/2162402X.2016.1273302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scarfo I, Maus MV. Current approaches to increase CAR T cell potency in solid tumours: targeting the tumour microenvironment. J Immunother Cancer. 2017;5:28. doi: 10.1186/s40425-017-0230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kloss CC, Condomines M, Cartellieri M, Bachmann M, Sadelain M. Combinatorial antigen recognition with balanced signaling promotes selective tumour eradication by engineered T cells. Nat Biotechnol. 2013;31:71–5. doi: 10.1038/nbt.2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lanitis E, Poussin M, Klattenhoff AW, Song D, Sandaltzopoulos R, June CH, Powell DJ. Chimeric antigen receptor T Cells with dissociated signaling domains exhibit focused antitumour activity with reduced potential for toxicity in vivo. Cancer Immunol Res. 2013;1:43–53. doi: 10.1158/2326-6066.CIR-13-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morsut L, Roybal KT, Xiong X, Gordley RM, Coyle SM, Thomson M, Lim WA. Engineering Customized Cell Sensing and Response Behaviors Using Synthetic Notch Receptors. Cell. 2016;164:780–91. doi: 10.1016/j.cell.2016.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lim WA, June CH. The Principles of Engineering Immune Cells to Treat Cancer. Cell. 2017;168:724–40. doi: 10.1016/j.cell.2017.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roybal KT, Rupp LJ, Morsut L, Walker WJ, McNally KA, Park JS, Lim WA. Precision Tumour Recognition by T Cells With Combinatorial Antigen-Sensing Circuits. Cell. 2016;164:770–9. doi: 10.1016/j.cell.2016.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roybal KT, Williams JZ, Morsut L, et al. Engineering T-cells with customized therapeutic response programs using synthetic Notch receptors. Cell. 2016;167:419–432.e416. doi: 10.1016/j.cell.2016.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fedorov VD, Themeli M, Sadelain M. PD-1- and CTLA-4-Based Inhibitory Chimeric Antigen Receptors (iCARs) Divert Off-Target Immunotherapy Responses. Sci Trans Med. 2013;5:215ra172–215ra172. doi: 10.1126/scitranslmed.3006597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zah E, Lin M-Y, Silva-Benedict A, Jensen MC, Chen YY. T Cells Expressing CD19/CD20 Bispecific Chimeric Antigen Receptors Prevent Antigen Escape by Malignant B Cells. Cancer Immunol Res. 2016;4:498–508. doi: 10.1158/2326-6066.CIR-15-0231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grada Z, Hegde M, Byrd T, et al. TanCAR: A Novel Bispecific Chimeric Antigen Receptor for Cancer Immunotherapy. Mol Ther Nucl Acids. 2013:2. doi: 10.1038/mtna.2013.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Caruso HG, Hurton LV, Najjar A, et al. Tuning Sensitivity of CAR to EGFR Density Limits Recognition of Normal Tissue While Maintaining Potent Antitumour Activity. Cancer Res. 2015;75:3505–3518. doi: 10.1158/0008-5472.CAN-15-0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Diem MD, Hyun L, Yi F, et al. Selection of high-affinity Centyrin FN3 domains from a simple library diversified at a combination of strand and loop positions. Protein Eng Des Sel. 2014;27:419–429. doi: 10.1093/protein/gzu016. [DOI] [PubMed] [Google Scholar]
- 56.Sha F, Salzman G, Gupta A, Koide S. Monobodies and other synthetic binding proteins for expanding protein science. Protein Sci. 2017;26:910–24. doi: 10.1002/pro.3148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ghosh A, Smith M, James SE, et al. Donor CD19 CAR T cells exert potent graft-versus-lymphoma activity with diminished graft-versus-host activity. Nat Med. 2017;23:242–9. doi: 10.1038/nm.4258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Torikai H, Reik A, Liu P-Q, et al. A foundation for universal T-cell based immunotherapy: T cells engineered to express a CD19-specific chimeric-antigen-receptor and eliminate expression of endogenous TCR. Blood. 2012;119:5697–705. doi: 10.1182/blood-2012-01-405365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wright AV, Nuñez JK, Doudna JA. Biology and Applications of CRISPR Systems: Harnessing Nature’s Toolbox for Genome Engineering. Cell. 2016;164:29–44. doi: 10.1016/j.cell.2015.12.035. [DOI] [PubMed] [Google Scholar]
- 60.Tsai SQ, Joung JK. Defining and improving the genome-wide specificities of CRISPR-Cas9 nucleases. Nat Rev Genet. 2016;17:300–12. doi: 10.1038/nrg.2016.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rupp LJ, Schumann K, Roybal KT, Gate RE, Ye CJ, Lim WA, Marson A. CRISPR/Cas9-mediated PD-1 disruption enhances anti-tumour efficacy of human chimeric antigen receptor T cells. Sci Rep. 2017;7:737. doi: 10.1038/s41598-017-00462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ren J, Liu X, Fang C, Jiang S, June CH, Zhao Y. Multiplex Genome Editing to Generate Universal CAR T Cells Resistant to PD1 Inhibition. Clin Cancer Res. 2017;23:2255–66. doi: 10.1158/1078-0432.CCR-16-1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee DW, Gardner R, Porter DL, Louis CU, Ahmed N, Jensen M, Grupp SA, Mackall CL. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124:188–95. doi: 10.1182/blood-2014-05-552729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Morgan RA, Chinnasamy N, Abate-Daga DD, et al. Cancer regression and neurologic toxicity following anti-MAGE-A3 TCR gene therapy. J Immunother. 2013;36:133–51. doi: 10.1097/CJI.0b013e3182829903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Davila ML, Kloss CC, Gunset G, Sadelain M. CD19 CAR-Targeted T Cells Induce Long-Term Remission and B Cell Aplasia in an Immunocompetent Mouse Model of B Cell Acute Lymphoblastic Leukemia. Plos One. 2013;8:e61338. doi: 10.1371/journal.pone.0061338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhou X, Dotti G, Krance RA, et al. Inducible caspase-9 suicide gene controls adverse effects from alloreplete T cells after haploidentical stem cell transplantation. Blood. 2015;125:4103–13. doi: 10.1182/blood-2015-02-628354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Paszkiewicz PJ, Fräßle SP, Srivastava S, et al. Targeted antibody-mediated depletion of murine CD19 CAR T cells permanently reverses B cell aplasia. J Clin Invest. 2016;126:4262–72. doi: 10.1172/JCI84813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Di Stasi A, Tey SK, Dotti G, et al. Inducible Apoptosis as a Safety Switch for Adoptive Cell Therapy. New Engl J Med. 2011;365:1673–1683. doi: 10.1056/NEJMoa1106152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Philip B, Kokalaki E, Mekkaoui L, et al. A highly compact epitope-based marker/suicide gene for easier and safer T-cell therapy. Blood. 2014;124:1277–87. doi: 10.1182/blood-2014-01-545020. [DOI] [PubMed] [Google Scholar]
- 70.Wang X, Chang WC, Wong CW, et al. A transgene-encoded cell surface polypeptide for selection, in vivo tracking, and ablation of engineered cells. Blood. 2011;118:1255–63. doi: 10.1182/blood-2011-02-337360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wu CY, Roybal KT, Puchner EM, Onuffer J, Lim WA. Remote control of therapeutic T cells through a small molecule-gated chimeric receptor. Science. 2015;350:aab4077. doi: 10.1126/science.aab4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jaspers JE, Brentjens RJ. Development of CAR T cells designed to improve antitumour efficacy and safety. Pharmacol Ther. 2017;178:83–91. doi: 10.1016/j.pharmthera.2017.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Newick K, O’Brien S, Moon E, Albelda SM. CAR T Cell Therapy for Solid Tumours. Annu Rev Med. 2017;68:139–52. doi: 10.1146/annurev-med-062315-120245. [DOI] [PubMed] [Google Scholar]
- 74.Fesnak AD, June CH, Levine BL. Engineered T cells: the promise and challenges of cancer immunotherapy. Nat Rev Cancer. 2016;16:566–81. doi: 10.1038/nrc.2016.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ramos CA, Heslop HE, Brenner MK. CAR-T Cell Therapy for lymphoma. Ann Rev Med. 2016;67:165–83. doi: 10.1146/annurev-med-051914-021702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Grupp SA, Kalos M, Barrett D, et al. Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. N Engl J Med. 2013;368:1509–18. doi: 10.1056/NEJMoa1215134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Porter DL, Levine BL, Kalos M, Bagg A, June CH. Chimeric antigen receptor-modified T cells in chronic lymphoid leukemia. N Engl J Med. 2011;365:725–33. doi: 10.1056/NEJMoa1103849. [DOI] [PMC free article] [PubMed] [Google Scholar]