Key Points
Question
Is protein intake greater than the recommended dietary allowance needed to maintain lean body mass in older adults?
Findings
In this randomized clinical trial of 92 men with physical functional limitations, changes in lean body mass, muscle strength and power, and physical function did not differ between men who consumed controlled diets containing the recommended dietary allowance and men who consumed a higher amount of protein (1.3 g/kg/d) for 6 months.
Meaning
The recommended dietary allowance for protein is sufficient to maintain lean body mass; protein intake exceeding the recommended dietary allowance does not increase lean body mass in functionally limited older men who are eating less than the recommended dietary allowance.
Abstract
Importance
The Institute of Medicine set the recommended dietary allowance (RDA) for protein at 0.8 g/kg/d for the entire adult population. It remains controversial whether protein intake greater than the RDA is needed to maintain protein anabolism in older adults.
Objective
To investigate whether increasing protein intake to 1.3 g/kg/d in older adults with physical function limitations and usual protein intake within the RDA improves lean body mass (LBM), muscle performance, physical function, fatigue, and well-being and augments LBM response to a muscle anabolic drug.
Design, Setting, and Participants
This randomized clinical trial with a 2 × 2 factorial design was conducted in a research center. A modified intent-to-treat analytic strategy was used. Participants were 92 functionally limited men 65 years or older with usual protein intake less thanor equal to 0.83 g/kg/d within the RDA. The first participant was randomized on September 21, 2011, and the last participant completed the study on January 19, 2017.
Interventions
Participants were randomized for 6 months to controlled diets with 0.8 g/kg/d of protein plus placebo, 1.3 g/kg/d of protein plus placebo, 0.8 g/kg/d of protein plus testosterone enanthate (100 mg weekly), or 1.3 g/kg/d of protein plus testosterone. Prespecified energy and protein contents were provided through custom-prepared meals and supplements.
Main Outcomes and Measures
The primary outcome was change in LBM. Secondary outcomes were muscle strength, power, physical function, health-related quality of life, fatigue, affect balance, and well-being.
Results
Among 92 men (mean [SD] age, 73.0 [5.8] years), the 4 study groups did not differ in baseline characteristics. Changes from baseline in LBM (0.31 kg; 95% CI, −0.46 to 1.08 kg; P = .43) and appendicular (0.04 kg; 95% CI, −0.48 to 0.55 kg; P = .89) and trunk (0.24 kg; 95% CI, −0.17 to 0.66 kg; P = .24) lean mass, as well as muscle strength and power, walking speed and stair-climbing power, health-related quality of life, fatigue, and well-being, did not differ between men assigned to 0.8 vs 1.3 g/kg/d of protein regardless of whether they received testosterone or placebo. Fat mass decreased in participants given higher protein but did not change in those given the RDA: between-group differences were significant (difference, −1.12 kg; 95% CI, −2.04 to −0.21; P = .02).
Conclusions and Relevance
Protein intake exceeding the RDA did not increase LBM, muscle performance, physical function, or well-being measures or augment anabolic response to testosterone in older men with physical function limitations whose usual protein intakes were within the RDA. The RDA for protein is sufficient to maintain LBM, and protein intake exceeding the RDA does not promote LBM accretion or augment anabolic response to testosterone.
Trial Registration
clinicaltrials.gov Identifier: NCT01275365
This randomized clinical trial investigates whether greater than the recommended dietary allowance of protein is needed to maintain lean body mass in older adults.
Introduction
The recommended dietary allowance (RDA) for protein, set by the Institute of Medicine, is 0.8 g/kg/d for the entire adult population, including young and old and male and female. Many experts have questioned whether the protein RDA is adequate to preserve lean body mass (LBM) and physical function in older adults. There is some evidence that anabolic response of skeletal muscle to dietary protein is attenuated in older individuals. Epidemiologic studies of older persons have reported an association of dietary protein intake with LBM change over time, although this association has not been observed in weight-stable persons. Controlled feeding studies of 10 to 12 weeks’ duration in older adults have shown that protein intakes at or below the RDA result in loss of LBM. In short-term studies, protein intakes exceeding the RDA were reported to promote apparent nitrogen retention and stimulate leucine kinetics. However, studies of older adults fed protein greater than the RDA have shown inconsistent improvements in LBM and physical function. Many studies did not control energy intake; some added a protein supplement to the usual diet, resulting in variable total protein intake and compliance. Most studies recruited healthy older adults without functional limitations and did not select individuals with usual protein intakes less than the RDA. Despite methodological limitations of short-term studies and inconsistent results of protein intervention trials, many national organizations and experts recommend dietary protein intakes greater than the RDA to maintain and promote protein anabolism in older adults. Therefore, our primary aim was to investigate whether increasing protein intake in older adults who usually consume amounts at or below the RDA to 1.3 g/kg/d would increase LBM, muscle performance, physical function, and well-being measures compared with older men who consume protein at the RDA level.
Results of studies in athletes and older adults suggest that protein intake substantially greater than the RDA may be required to optimize adaptations to exercise training. A number of muscle anabolic drugs, such as androgens and myostatin antagonists, are being developed to treat sarcopenia. Therefore, it is important to know whether protein intake exceeding the RDA is needed for achieving optimal anabolic response to muscle anabolic drugs. Our second aim was to investigate whether higher protein intake in excess of the RDA is needed in older adults with physical function limitations to optimize the anabolic response to testosterone, a drug known to increase muscle mass and strength. In older individuals whose usual protein intake is within the RDA, we hypothesized that increasing their protein intake to 1.3 g/kg/d without changing the daily energy intake would not result in greater improvements in LBM, muscle strength, and physical function than providing the RDA but that the higher protein intake would augment anabolic response to testosterone.
Methods
Study Design
The design of the trial has been published previously. The Optimizing Protein Intake in Older Men (OPTIMen) Trial was a randomized, placebo-controlled, double-blind, parallel-group trial with a 2 × 2 factorial design (Supplement 1). Institutional review boards at Brigham and Women’s Hospital and Boston Medical Center approved the study. Participants provided written informed consent. An independent data and safety monitoring board oversaw the progress and safety of the study. The first participant was randomized on September 21, 2011, and the last participant completed the study on January 19, 2017.
Participants
Participants were community-dwelling men 65 years or older with moderate physical function limitation (Short Physical Performance Battery summary score range, 3-10) whose average daily protein intake was less than or equal to 0.83 g/kg/d. This value was selected as the 97.5th percentile for dietary protein allowance from a meta-analysis of nitrogen balance studies. We excluded men with prostate cancer, severe lower urinary tract symptoms, untreated sleep apnea, heart failure, myocardial infarction, or stroke within 6 months, as well as those having glycated hemoglobin levels exceeding 8% or those with erythrocytosis.
Participant Recruitment
After a brief telephone screening, participants underwent medical history, physical examination, blood cell counts, serum chemistries, prostate-specific antigen screening, and Short Physical Performance Battery testing. Average daily energy and protein intakes were ascertained from 24-hour food recalls on 3 days, including one weekend day.
Participants who met eligibility criteria entered a run-in period during which they were asked to eat a custom diet containing 0.8 g/kg/d of protein for 10 to 16 days. Participants who consumed less than 75% of provided meals or supplements were excluded.
Randomization
Participants were randomized using computer-generated randomization tables and randomly varying blocks of 4 and 8 to the following: (1) 0.8 g/kg/d of protein plus placebo injections intramuscularly weekly, (2) 1.3 g/kg/d of protein plus placebo, (3) 0.8 g/kg/d of protein plus testosterone enanthate (100 mg weekly), or (4) 1.3 g/kg/d of protein plus testosterone. Randomization was stratified by diabetes status.
Interventions
Testosterone and placebo injections were administered in the Men’s Health Research Unit. Details of the dietary intervention have been previously published. Energy and protein contents of each participant’s individualized diet were standardized by providing packaged meals and supplements (eTable 1 in Supplement 2). Daily energy requirement was calculated using the dietary reference intake equation plus an activity factor. Participants received 1260 mg of calcium, 1000 IU of vitamin D3, and a multivitamin daily.
Daily energy and protein intakes were apportioned between prepackaged meals, protein or carbohydrate (placebo) supplements, and discretionary food allowances (eTable 1 in Supplement 2). Packaged meals with individualized protein and energy contents were supplied by Personal Chef to Go, Mechanicsville, Virginia, and provided 0.7 g/kg/d of protein and 80% of daily energy requirements. Discretionary foods (fruits/vegetables, coffee/tea, alcoholic beverages, and other foods) provided an additional 0.1 g/kg/d of protein and 15% of energy. The difference between the prescribed protein and energy intakes and protein and energy contents of packaged meals was made up by protein or carbohydrate supplements. Participants received their daily protein allotment through packaged meals (0.7 g/kg/d), supplement (0 g/kg/d for control and 0.5 g/kg/d for the higher protein group), and discretionary foods (0.1 g/kg/d). Participants in the group receiving 1.3 g/kg/d of protein received a supplement containing 0.5 g/kg/d of casein and whey protein mix, bringing their protein intake to 1.3 g/kg/d; the control group received a supplement containing 0.5 g/kg/d of carbohydrate powder.
Twenty percent of daily energy intake was provided as breakfast, 40% as lunch, and 40% as dinner. A 7-day supply of packaged food was picked up by participants or was home delivered.
A laboratory in Arden Hills, Minnesota (rtech laboratories from Land O’Lakes) performed quality control tests of each supplement batch. In addition, they periodically checked protein and energy contents of packaged meals.
Compliance
Every week, a nutritionist (M.S. or K.S.) reviewed either 24-hour food recalls or dietary compliance checklists to reinforce dietary instructions. For dietary compliance checklists, participants checked off food items, discretionary food, and portions consumed.
Exercise
Participants were asked to maintain their usual physical activity and exercise level. They were instructed to avoid vigorous resistance and endurance exercise.
Masking
Participants and study staff were masked to randomization: group assignment was known only to investigational pharmacy personnel, an unmasked statistician, and an unmasked nutritionist (T.G.T.) who prepared the supplement. The randomization was communicated to unmasked personnel via an automated email from the data management system. The data and safety and monitoring board was provided masked data, with treatment arms differentiated by alphanumeric codes.
Outcomes
The primary outcome was change in LBM, measured by dual-energy x-ray absorptiometry calibrated using a soft-tissue phantom. Lean body mass is an integrated marker of protein anabolism that can be measured precisely and is responsive to anabolic interventions. Secondary outcomes included appendicular and trunk lean tissue mass, maximal voluntary leg press and chest press strength, and leg power (eMethods in Supplement 2). Physical function measures included 6-minute walking distance, stair-climbing power with and without carrying a load of 20% body mass, and 50-m walk carrying a load equaling 20% body mass (eMethods in Supplement 2).
Health-related quality of life (HRQOL) and self-reported physical function were assessed using the 36-Item Short Form Health Survey, well-being by the Psychological General Well-Being Index, fatigue by the Functional Assessment of Chronic Illness Therapy 1 Scale, and positive and negative affect by the Derogatis Affects Balance Scale. Adverse events, blood cell counts and serum chemistries, prostate-specific antigen, International Prostate Symptom Score, lipids, lipoproteins, serum urea nitrogen and creatinine, and 24-hour urinary calcium and urea nitrogen excretion were monitored.
Statistical Analysis
The primary hypotheses concerned the effect of protein level on LBM and the differential effect of testosterone in the groups receiving 0.8 vs 1.3 g/kg/d of protein. We used a modified intent-to-treat analytic strategy. All randomized participants who had at least one postrandomization assessment were included in analyses. A mixed-effects regression model was used to assess 3-month and 6-month outcomes simultaneously, controlling for baseline LBM and diabetes status (a stratification factor) and allowing for unstructured correlation between participants’ serial measurements. The mean between-group differences in postrandomization change in outcomes were estimated (eg, between the groups receiving 0.8 vs 1.3 g/kg/d of protein) using treatment contrasts and associated 95% CIs. Associations between changes in protein intake and changes in outcome measures were also estimated using mixed-effects regression. The analytic plan assumed additivity of protein and testosterone effects, such that the former was estimated by comparing all individuals who received the enhanced protein intake with those who did not (ie, the main effect of protein), controlling for testosterone administration.
Adherence of results to this assumption was investigated in sensitivity analyses using statistical interaction terms. Additional sensitivity analyses examined the effect of interventions on end-of-treatment outcome measures using analysis of covariance and considered the potential for secular trends by comparing estimated effects in the first half of the randomized participants with those in the second half. Type I error for 2-sided Wald-type hypothesis tests was set at 0.05. Because analyses were prespecified, no adjustment was made for multiplicity. The analyses used SAS version 9.3 (SAS Institute Inc) and R version 3.2.5 (R Foundation).
The sample size was based on the assumption that 76 participants across all 4 groups would provide 80% power to detect a standardized treatment difference of 0.65 between those receiving 0.8 g/kg/d of protein and those receiving 1.3 g/kg/d of protein. This difference was deemed clinically meaningful because it was shown to be associated with improvements in muscle strength and physical function in other functionally limited populations. We assumed that the SD of change in LBM in the treatment arms would range between 2.5 and 4.0 kg. This assumption was met in the trial: the SD of change in each of the 4 groups was substantially less than that assumed.
Anticipating a maximum of 15% cumulative missingness and loss to follow-up, we enrolled 92 participants. This was calculated by dividing 76 by 0.85.
Results
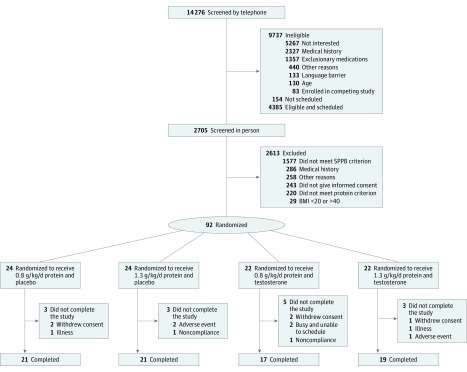
In total, 14 276 individuals underwent telephone screening, 2705 underwent in-person screening, 154 met eligibility criteria and entered a trial diet run-in period, 95 met dietary compliance requirements, 3 participants withdrew before randomization, 92 were randomized, 81 completed 3 months of intervention, and 78 completed 6 months of intervention. These results are shown in Figure 1.
Figure 1. CONSORT Diagram Showing the Flow of Participants in the OPTIMen Trial by Receipt of Protein, Placebo, and Testosterone Enanthate (100 mg Weekly).
BMI indicates body mass index (calculated as weight in kilograms divided by height in meters squared); CONSORT, Consolidated Standards of Reporting Trials; OPTIMen, Optimizing Protein Intake in Older Men; and SPPB, Short Physical Performance Battery.
Baseline Characteristics
The mean (SD) values for baseline characteristics of participants were as follows: age of 73.0 (5.8) years, body mass index (calculated as weight in kilograms divided by height in meters squared) of 30.3 (4.9), Short Physical Performance Battery summary score of 8.1 (1.3), and LBM of 55.0 (7.3) kg. Fifteen percent (n = 14) of participants had diabetes. The groups were not different in their baseline characteristics (Table). Baseline intake of protein, energy, and macronutrients did not differ among groups.
Table. Baseline Characteristics of Participants by Receipt of Protein, Placebo, and Testosterone Enanthate (100 mg Weekly).
| Variable | 0.8 g/kg/d Protein Plus Placebo (n = 24) |
1.3 g/kg/d Protein Plus Placebo (n = 24) |
0.8 g/kg/d Protein Plus Testosterone (n = 22) |
1.3 g/kg/d Protein Plus Testosterone (n = 22) |
All (N = 92) |
|---|---|---|---|---|---|
| Demographics | |||||
| Age, mean (SD), y | 71.3 (4.2) | 73.5 (5.7) | 71.0 (3.6) | 76.0 (7.9) | 73.0 (5.8) |
| Body weight, mean (SD), kg | 95.3 (12.5) | 90.2 (15.8) | 94.4 (17.6) | 87.2 (18.3) | 91.8 (16.2) |
| Height, mean (SD), cm | 175.3 (6.9) | 174.2 (7.0) | 173.2 (7.5) | 173.0 (9.4) | 174.0 (7.7) |
| BMI, mean (SD) | 31.1 (4.2) | 29.6 (4.6) | 31.4 (5.5) | 29.0 (5.0) | 30.3 (4.9) |
| Diabetes, No. (%) | 4 (17) | 4 (17) | 3 (14) | 3 (14) | 14 (15) |
| SPPB summary score, mean (SD) | 8.0 (1.4) | 7.8 (1.4) | 8.4 (1.1) | 8.2 (1.4) | 8.1 (1.3) |
| Protein intake, mean (SD), g/kg/d | 0.69 (0.15) | 0.72 (0.11) | 0.72 (0.19) | 0.70 (0.14) | 0.71 (0.15) |
| Dual-Energy X-Ray Absorptiometry Measurements, Mean (SD) | |||||
| Whole-body lean mass, kg | 56.3 (5.5) | 54.3 (7.2) | 56.1 (8.6) | 53.3 (7.9) | 55.0 (7.3) |
| Appendicular lean soft-tissue mass, kg | 25.7 (5.0) | 25.8 (5.4) | 26.5 (5.6) | 25.1 (5.2) | 25.8 (5.2) |
| Trunk lean mass, kg | 28.3 (2.7) | 26.8 (3.7) | 27.8 (4.3) | 26.5 (4.4) | 27.4 (3.8) |
| Whole-body fat mass, kg | 33.6 (9.0) | 30.5 (9.5) | 33.4 (9.3) | 28.9 (9.7) | 31.6 (9.4) |
| Appendicular fat mass, kg | 13.0 (3.9) | 11.9 (3.6) | 12.7 (3.8) | 11.4 (4.2) | 12.3 (3.9) |
| Trunk fat mass, kg | 19.4 (5.7) | 17.5 (6.3) | 19.5 (5.8) | 16.4 (5.8) | 18.2 (6.0) |
| Percentage lean mass, % | 61.0 (1.1) | 62.3 (1.1) | 61.1 (1.0) | 63.3 (1.3) | 61.9 (5.5) |
| Muscle Performance Measures, Mean (SD) | |||||
| Leg press strength, N | 2128.5 (490.3) | 2154.1 (359.2) | 2137.4 (465.8) | 1909.0 (420.8) | 2088.2 (415.0) |
| Chest press strength, N | 458.8 (117.5) | 450.0 (103.0) | 430.6 (76.8) | 414.8 (108.0) | 437.7 (101.9) |
| Leg press power, W | 582.5 (161.2) | 559.1 (121.5) | 560.4 (131.6) | 480.3 (141.5) | 549.6 (142.3) |
| Physical Function Measures, Mean (SD) | |||||
| 6-min Walking distance, m | 428.2 (108.3) | 442.2 (77.3) | 451.5 (84.5) | 470.6 (88.8) | 448.7 (90.3) |
| Unloaded stair-climbing power, W | 377.3 (85.6) | 356.5 (91.7) | 400.5 (138.5) | 317.5 (85.6) | 362.9 (113.7) |
| Loaded stair-climbing power, W | 407.2 (162.4) | 393.1 (132.9) | 466.1 (156.7) | 345.9 (95.8) | 383.7 (128.8) |
| Loaded walking speed, m/s | 1.6 (0.4) | 1.6 (0.4) | 1.6 (0.4) | 1.5 (0.2) | 1.6 (0.3) |
| 36-Item Short Form Health Survey, Mean (SD) | |||||
| Physical functioning score | 75.4 (22.4) | 81.7 (17.0) | 78.6 (15.7) | 82.0 (17.6) | 79.4 (18.3) |
| Total score | 77.0 (11.1) | 80.1 (13.6) | 80.7 (14.9) | 78.8 (13.0) | 79.1 (13.0) |
| Psychological General Well-Being Index, Mean (SD) | |||||
| Global score | 79.0 (8.7) | 81.7 (12.6) | 81.0 (12.9) | 78.1 (15.0) | 80.0 (12.3) |
| Functional Assessment of Chronic Illness Therapy 1 Scale, Mean (SD) | |||||
| Fatigue score | 42.1 (6.6) | 42.4 (7.8) | 43.0 (7.6) | 41.8 (6.2) | 42.3 (7.0) |
| Derogatis Affects Balance Scale Score, Mean (SD) | |||||
| Joy | 13.3 (2.0) | 14.6 (2.5) | 13.8 (1.9) | 13.6 (3.5) | 13.8 (2.6) |
| Contentment | 14.0 (2.4) | 14.6 (2.6) | 14.9 (1.9) | 14.6 (2.6) | 14.5 (2.4) |
| Vigor | 11.7 (2.3) | 13.1 (3.0) | 13.7 (2.7) | 12.5 (4.1) | 12.8 (3.1) |
| Affection | 12.6 (2.7) | 13.9 (3.4) | 14.5 (2.4) | 14.2 (2.7) | 13.8 (2.9) |
| Anxiety | 4.3 (2.6) | 5.7 (3.2) | 5.8 (2.7) | 6.0 (4.2) | 5.4 (3.2) |
| Depression | 2.6 (2.3) | 3.0 (2.8) | 3.5 (2.9) | 4.6 (3.9) | 3.4 (3.1) |
| Hostility | 3.8 (2.9) | 4.6 (2.6) | 4.4 (3.0) | 4.6 (3.6) | 4.4 (3.0) |
| Guilt | 2.9 (2.8) | 4.0 (2.7) | 3.2 (2.2) | 4.3 (3.4) | 3.6 (2.8) |
| Laboratory Data, Mean (SD) | |||||
| Glucose, mg/dL | 104.3 (25.5) | 100.0 (20.0) | 106.1 (25.8) | 100.3 (13.6) | 102.6 (21.6) |
| Serum urea nitrogen, mg/dL | 17.8 (4.9) | 16.4 (5.5) | 16.6 (3.0) | 15.4 (4.6) | 16.6 (4.7) |
| Calcium, mg/dL | 9.34 (0.33) | 9.41 (0.34) | 9.40 (0.28) | 9.40 (0.31) | 9.38 (0.31) |
| AST, U/L | 22.2 (9.0) | 21.4 (5.1) | 20.7 (5.1) | 22.0 (9.7) | 21.6 (7.5) |
| ALT, U/L | 23.0 (11.5) | 21.1 (6.9) | 19.6 (7.7) | 19.9 (13.0) | 21.0 (10.0) |
| PSA, ng/mL | 1.70 (0.94) | 1.55 (1.15) | 1.31 (0.82) | 1.31 (0.81) | 1.48 (0.94) |
| Hemoglobin, g/dL | 14.1 (1.2) | 14.4 (1.3) | 14.0 (0.9) | 14.2 (1.0) | 14.2 (1.1) |
| Hematocrit, % | 42.9 (3.5) | 43.1 (3.8) | 42.4 (2.8) | 42.5 (2.6) | 42.7 (3.2) |
| Creatinine, mg/dL | 0.97 (0.18) | 0.99 (0.19) | 0.98 (0.18) | 1.07 (0.26) | 1.00 (0.21) |
| Total protein, g/dL | 7.00 (0.37) | 6.98 (0.44) | 7.01 (0.42) | 7.03 (0.47) | 7.01 (0.42) |
| Albumin, g/dL | 4.36 (0.28) | 4.32 (0.24) | 4.40 (0.30) | 4.40 (0.26) | 4.37 (0.27) |
| Globulin, g/dL | 2.64 (0.43) | 2.66 (0.35) | 2.61 (0.28) | 2.64 (0.37) | 2.64 (0.36) |
| Total cholesterol, mg/dL | 173.6 (29.3) | 165.4 (40.0) | 162.1 (29.5) | 173.8 (36.8) | 168.9 (34.1) |
| HDL cholesterol, mg/dL | 49.2 (20.0) | 46.2 (10.9) | 44.6 (11.3) | 47.6 (15.3) | 47.0 (14.8) |
| LDL cholesterol, mg/dL | 96.3 (28.6) | 89.0 (32.7) | 90.5 (19.5) | 101.5 (32.9) | 94.3 (29.0) |
| Triglycerides, mg/dL | 149.7 (97.4) | 151.1 (78.6) | 134.7 (67.4) | 123.4 (64.4) | 140.3 (78.4) |
| Total testosterone, ng/dL | 323.0 (164.7) | 406.3 (241.2) | 426.0 (221.8) | 484.6 (247.7) | 407.8 (224.7) |
| Free testosterone, ng/dL | 7.2 (4.3) | 10.1 (7.7) | 11.6 (7.3) | 12.0 (8.0) | 10.1 (7.1) |
| 24-h Urinary calcium, mg/24 h | 135.3 (87.9) | 114.9 (72.2) | 116.6 (95.3) | 120.8 (72.2) | 122.1 (81.3) |
| 24-h Urinary urea nitrogen, g/24 h | 9.9 (3.1) | 9.7 (3.8) | 11.1 (3.4) | 8.4 (2.1) | 9.8 (3.3) |
Abbreviations: ALT, alanine aminotransferase; AST; aspartate aminotransferase; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HDL, high-density lipoprotein; LDL, low-density lipoprotein; PSA, prostate-specific antigen; SPPB, Short Physical Performance Battery.
SI conversion factors: To convert albumin level to grams per liter, multiply by 10; ALT and AST levels to microkatals per liter, multiply by 0.0167; calcium level to millimoles per liter, multiply by 0.25; cholesterol level to millimoles per liter, multiply by 0.0259; creatinine level to micromoles per liter, multiply by 88.4; free and total testosterone levels to nanomoles per liter, multiply by 0.0347; glucose level to millimoles per liter, multiply by 0.0555; hematocrit to proportion of 1.0, multiply by 0.01; hemoglobin level to grams per liter, multiply by 10.0; PSA level to micrograms per liter, multiply by 1.0; serum urea nitrogen level to millimoles per liter, multiply by 0.357; total protein level to grams per liter, multiply by 10.0; and triglyceride level to millimoles per liter, multiply by 0.0113.
Compliance With Dietary Prescription and Study Procedures
During the first 3 months, compliance with packaged meals averaged 81% to 86%, and compliance with supplements averaged 90% to 94%. Compliance was similarly high during months 4 through 6 (eTable 2 in Supplement 2). Participants received greater than 99% of testosterone or placebo injections.
Energy intake was not different among groups. The men assigned to receive 1.3 g/kg/d of protein consumed a higher amount of protein than those assigned to receive 0.8 g/kg/d, as indicated by food recalls (eTable 3 in Supplement 2) and higher serum urea nitrogen and urinary urea nitrogen excretion (eTable 4 in Supplement 2).
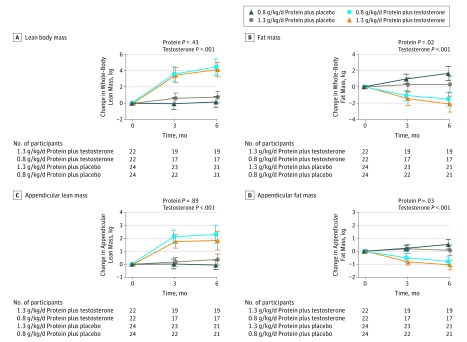
Lean Body Mass
There was no significant effect of protein level on LBM over 6 months. The changes in LBM did not differ among men assigned to 0.8 vs 1.3 g/kg/d of protein (effect size, 0.31 kg; 95% CI, −0.46 to 1.08 kg; P = .43) regardless of whether they received testosterone or placebo (Figure 2 and eTable 5 in Supplement 2). The increase in protein intake above baseline was not significantly associated with change in LBM. Men randomized to testosterone gained significantly more LBM than those randomized to placebo (3.54 kg; 95% CI, 2.88-4.20 kg; P < .001) regardless of protein intake.
Figure 2. Changes in Body Composition Measures.
A through D, Change in whole-body and regional lean and adipose tissue mass in kilograms from baseline was assessed using dual-energy x-ray absorptiometry. The number of randomized participants in each of the 4 intervention groups who contributed the data at each time point is shown at the bottom of the graphs. The P values, derived from the mixed-effects regression model framework, for the protein-level effect (0.8 vs 1.3 g/kg/d) and testosterone effect (testosterone vs placebo) are also shown. The months represent the time points (0, 3, and 6 months) at which the measurements were performed. Error bars indicate 95% CIs.
Changes in appendicular (0.04 kg; 95% CI, −0.48 to 0.55 kg; P = .89) and trunk (0.24 kg; 95% CI, −0.17 to 0.66 kg; P = .24) lean mass did not differ among men randomized to 0.8 vs 1.3 g/kg/d of protein regardless of whether they received testosterone or placebo (Figure 2 and eTable 5 in Supplement 2). Testosterone administration was associated with greater gains in trunk (1.70 kg; 95% CI, 1.34-2.06 kg; P < .001) and appendicular (1.86 kg; 95% CI, 1.48-2.23 kg; P < .001) lean mass than placebo.
Whole-Body and Regional Fat Mass
Fat mass did not change in men randomized to receive 0.8 g/kg/d of protein but decreased in men receiving 1.3 g/kg/d of protein: the between-group difference was statistically significant (difference, −1.12 kg; 95% CI, −2.04 to −0.21 kg; P = .02) (Figure 2 and eTable 5 in Supplement 2), controlling for testosterone administration. Testosterone use was associated with a significantly greater loss of fat mass than placebo (−2.01 kg; 95% CI, −2.69 to −1.33 kg; P < .001), controlling for protein level.
Similarly, appendicular and trunk fat mass did not change in the group receiving 0.8 g/kg/d of protein but decreased in the group receiving 1.3 g/kg/d of protein: between-group differences were significant for appendicular (−0.40 kg; 95% CI, −0.75 to −0.05 kg; P = .03) and trunk (−0.69 kg; 95% CI, −1.33 to −0.04 kg; P = .04) fat mass. Testosterone administration was associated with significantly greater loss of appendicular (−0.95 kg; 95% CI, −1.22 to −0.68 kg; P < .001) and trunk (−1.15 kg; 95% CI, −1.62 to −0.67 kg; P < .001) fat mass than placebo.
Changes in body mass did not differ between the groups receiving 0.8 vs 1.3 g/kg/d of protein, controlling for testosterone administration (between-group difference, −0.78 kg; 95% CI, −1.92 to 0.37 kg; P = .18). These results are shown in eFigure 1 in Supplement 2.
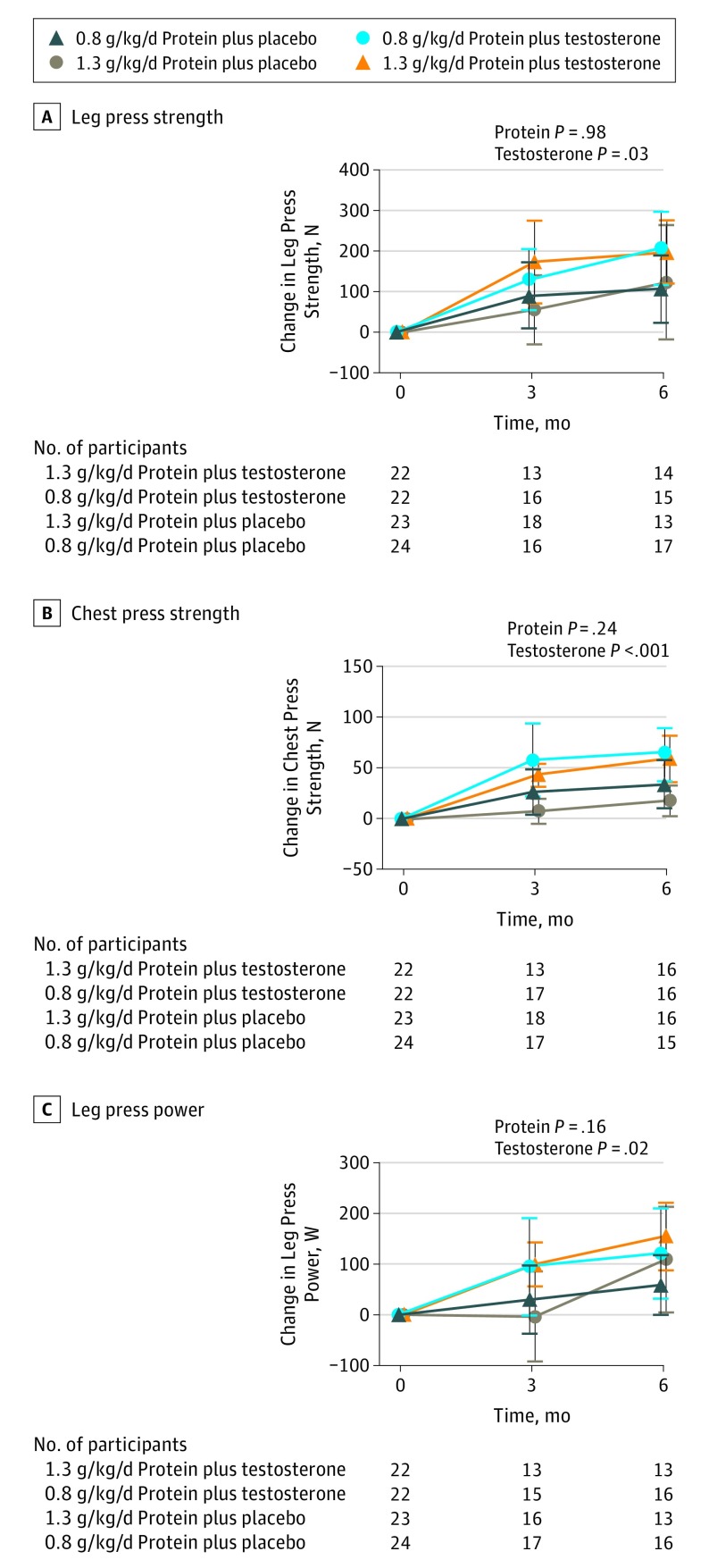
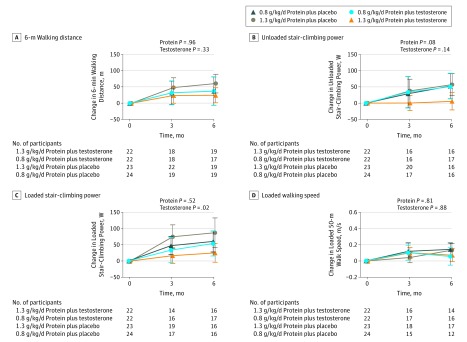
Muscle Performance and Physical Function
Changes in leg press strength, chest press strength, and leg press power did not differ significantly between the 2 protein levels (Figure 3 and eTable 5 in Supplement 2). Similarly, there was no significant difference between the 2 protein levels in the change in 6-minute walking distance, loaded or unloaded stair-climbing power, or loaded walking speed regardless of whether the participants were receiving testosterone or placebo (Figure 4). Testosterone administration was associated with greater improvements in leg press strength (84.1 N; 95% CI, 7.5-160.8 N; P = .03), chest press strength (37.0 N, 95% CI, 18.8 to 55.1 N; P < .001), and leg press power (38.2 W; 95% CI, 5.3-71.1 W; P = .02) than placebo.
Figure 3. Changes in Measures of Skeletal Muscle Performance.
A through C, Maximal voluntary strength measured as 1-repetition maximum in the leg press and chest press exercises and leg press power was assessed using the Keiser chest press and leg press machines (Keiser Sports). The number of randomized participants in each of the 4 intervention groups who contributed the data at each time point is shown at the bottom of the graphs. The P values, derived from the mixed-effects regression model framework, for the protein-level effect (0.8 vs 1.3 g/kg/d) and testosterone effect (testosterone vs placebo) are also shown. The months represent the time points (0, 3, and 6 months) at which the measurements were performed. Error bars indicate 95% CIs.
Figure 4. Changes in Performance-Based Measures of Physical Function.
A through D, Loaded walking speed plus unloaded and loaded stair-climbing (per Muscle Performance subsection on page 5 and Figure 4) power were assessed. The number of randomized participants in each of the 4 intervention groups who contributed the data at each time point is shown at the bottom of the graphs. The P values, derived from the mixed-effects regression model framework, for the protein-level effect (0.8 vs 1.3 g/kg/d) and testosterone effect (testosterone vs placebo) are also shown. The months represent the time points (0, 3, and 6 months) at which the measurements were performed. Error bars indicate 95% CIs.
HRQOL, Well-Being, Affect Balance, and Fatigue
There was no significant effect of protein level or testosterone on overall HRQOL or physical component score, well-being, affect balance, or fatigue. These results are shown in eFigure 2 in Supplement 2.
Sensitivity Analyses
We observed little evidence of interaction of protein and testosterone effects on outcomes, so the design assumption of additivity of effects was consistent with observed results. Analysis of covariance models restricted to end-of-treatment outcome measures provided results that were similar to the primary analysis described above in the Lean Body Mass subsection. Comparison of effects in the first half of the enrolled participants with those in the second half did not suggest secular trends in results.
Serum Chemistries and Safety Measures
Adverse events and serious adverse events (eTable 6 in Supplement 2) did not differ among groups. Compared with 0.8 g/kg/d of protein, higher protein intake was associated with greater 24-hour urinary urea nitrogen excretion (1.91 g/24 hours; 95% CI, 0.23-3.58 g/24 hours; P = .03) and higher serum urea nitrogen (4.43 mg/dL; 95% CI, 2.64-6.21 mg/dL; P < .001) (eTable 4 in Supplement 2). Serum creatinine, aspartate aminotransferase, alanine aminotransferase, calcium, and 24-hour urinary calcium excretion did not differ among the groups.
In men randomized to testosterone, the mean (SD) total and free testosterone levels, measured 1 week after injections and averaged across months 3 and 6, increased from 456 (36) to 620 (41) ng/dL (total) and from 11.8 (1.2) to 19.3 (1.4) ng/dL (free) (to convert testosterone levels to nanomoles per liter, multiply by 0.0347). Testosterone administration increased hematocrit and levels of hemoglobin, serum creatinine, and prostate-specific antigen more than placebo (eTable 4 in Supplement 2).
Discussion
Compared with a daily intake of 0.8 g/kg/d of protein, a daily intake higher than the RDA (1.3 g/kg/d of protein) did not increase LBM, muscle strength or power, physical function, HRQOL, well-being, affect balance, or fatigue in functionally limited older men whose baseline protein intake was within the RDA. Furthermore, protein intake exceeding the RDA did not augment LBM or muscle strength gains induced by testosterone administration. Changes in LBM were not related to changes in protein intake. Our findings indicate that the RDA was sufficient to maintain LBM and do not support the hypothesis that protein intakes exceeding the RDA promote lean mass accretion or augment response to a muscle anabolic drug, such as testosterone. These data support a call by many experts for reevaluation of the current RDA estimate, which was derived from short-term nitrogen balance studies that included a small number of participants and even fewer older adults. These pioneering studies did not use integrated measures of anabolism, such as LBM, nor did they assess muscle performance and physical function.
The higher protein intake attenuated the gains in whole-body, appendicular, and trunk fat mass relative to 0.8 g/kg/d of protein. The mechanisms by which increased protein intake attenuates fat mass gains are incompletely understood but may include increased energy expenditure due to the thermic effect of protein and changes in gut hormones, such as glucagon and glucagon-like peptide 1, or other regulators of thermogenesis, such as sarcoplipin. Increased protein intake was associated with greater loss of fat mass in settings of exercise training or energy-restricted diets. In a cross-sectional study of older adults, protein intake equal to the RDA was associated with lower fat mass than protein intake less than the RDA.
Protein intervention was safe and was associated with a low frequency of adverse events. There were no significant changes in liver enzymes, serum creatinine, or urinary calcium excretion.
The study had a good trial design, including block randomization, parallel groups, and masking. The 2 × 2 factorial design enabled us to investigate the effects of protein level and testosterone separately and together. Our primary outcome of LBM, in contrast to urinary nitrogen balance or markers of protein kinetics, is an integrated measure of whole-body anabolism that can be measured precisely in older adults. We also included multiple measures of muscle performance, physical function, and patient-reported outcomes. We recruited men with physical function limitations whose protein intake was at or below the RDA, a group most likely to benefit from higher protein intake. The custom-designed meals included multiple animal and plant sources of high-quality protein. To our knowledge, this is the longest and largest randomized, controlled feeding study of protein intervention conducted in older adults.
To control variability in energy intake, we provided prepackaged meals and supplements designed to maintain energy balance. Food recalls and dietary compliance checklists confirmed that energy intake was not different among groups. We used several measures to enhance compliance, including provision of custom-prepared, portion-controlled meals. Dietary compliance checklists and 24-hour food recalls were used to assess compliance and to reinforce dietary instructions each week. Nutrient composition of packaged meals and supplements was verified periodically by chemical analyses.
An important challenge in dietary intervention studies is that participants given nutritional supplements may reduce their intake of other foods. Several lines of evidence indicate that the participants randomized herein to the higher protein groups increased their protein intake above baseline. The estimates of higher protein intake in men randomized to 1.3 g/kg/d of protein by food recalls and dietary compliance checklists were confirmed by increases in serum urea nitrogen and 24-hour urinary urea nitrogen excretion. Although these methods provide only approximate estimates of protein intake (food recalls tend to underestimate protein intakes), all 3 methods confirmed that the participants randomized to 1.3 g/kg/d of protein consumed a higher amount of protein than at baseline and higher than the group randomized to 0.8 g/kg/d of protein.
Limitations
The study has some limitations. Because the study included older men with mild to moderate physical dysfunction, we do not know whether our findings apply to women or to frail elderly older persons. Older adults, especially those with frailty, may have multiple comorbid conditions that may affect LBM. Our controlled feeding study in a research center was conducted in carefully selected, medically stable participants using packaged meals, close supervision, and frequent reinforcement of dietary instructions, which facilitated a high level of compliance. This level of compliance is difficult to achieve in clinical practice. The mean body mass index of the participants was approximately 30, which is typical for men of this age. Therefore, a significant proportion of the participants herein were obese. For this study, protein intakes were investigated using each participant’s measured body mass. Additional research is needed to assess whether the RDA for protein should be based on ideal body mass. However, prescribing protein intake based on ideal body mass would reduce total protein intake among older adults who are overweight or obese; this is not currently recommended. The participants herein were not hypogonadal, and there was no clinical indication for testosterone therapy in these men. A testosterone group was included to investigate if protein supplementation enhanced the effects of testosterone.
The sample size of 92 participants was intended to achieve 80% power to detect robust and clinically meaningful effects, but it provided less assurance of the detection of more subtle differences. The effect of the testosterone intervention on total and regional LBM was of the expected magnitude and statistically significant. The much smaller effects of the higher protein level on whole-body and appendicular fat mass were also detectable. By contrast, the observed differences in LBM between the groups receiving 0.8 vs 1.3 g/kg/d of protein were small and far smaller than those hypothesized. These observations suggest that it is the lack of a meaningful effect of the enhanced protein intervention, rather than a lack of statistical power, that drove this null finding.
Nevertheless, the findings of our study should be interrogated in larger confirmatory studies. Our analyses did not find evidence of interaction between interventions, although the statistical power to detect interactions was limited. The recruitment plans of future trials should consider the OPTIMen Trial screening experience, which randomized 1 participant per 30 men screened in person and 155 men screened on the telephone.
Conclusions
Protein intake equal to the RDA was sufficient to maintain LBM, muscle strength, and physical function in functionally limited older men. Our findings do not support the recommendation that protein intakes higher than the RDA promote LBM accretion or augment anabolic response to a muscle anabolic drug, such as testosterone. Our data highlight the need for reevaluation of the protein RDA in older adults, especially those with frailty and chronic diseases.
Trial Protocol
eTable 1. Energy and Protein Distribution in 0.8-g/kg/d and 1.3-g/kg/d Groups
eTable 2. Dietary Adherence With Packaged Meals and Supplements During Months 1 to 3 and Months 4 to 6
eTable 3. Estimated Protein and Energy Intake From 24-Hour Food Recalls
eTable 4. Model-Based Estimates of Mean Change in Laboratory Variables by Intervention Groups, With Estimated Differences Attributable to the 2 Interventions
eTable 5. Model-Based Estimates of Mean Change in Outcomes by Intervention Groups, With Estimated Differences Attributable to the 2 Interventions
eTable 6. Adverse Event and Serious Adverse Event Profile by Randomized Group and Physiologic System
eMethods. Supplemental Methods
eFigure 1. Total Body Mass
eFigure 2. Patient-Reported Outcomes
References
- 1.Institute of Medicine Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 2.Rennie MJ. Anabolic resistance: the effects of aging, sexual dimorphism, and immobilization on human muscle protein turnover. Appl Physiol Nutr Metab. 2009;34(3):377-381. [DOI] [PubMed] [Google Scholar]
- 3.Cuthbertson D, Smith K, Babraj J, et al. Anabolic signaling deficits underlie amino acid resistance of wasting, aging muscle. FASEB J. 2005;19(3):422-424. [DOI] [PubMed] [Google Scholar]
- 4.Houston DK, Nicklas BJ, Ding J, et al. ; Health ABC Study . Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr. 2008;87(1):150-155. [DOI] [PubMed] [Google Scholar]
- 5.Geirsdottir OG, Arnarson A, Ramel A, Jonsson PV, Thorsdottir I. Dietary protein intake is associated with lean body mass in community-dwelling older adults. Nutr Res. 2013;33(8):608-612. [DOI] [PubMed] [Google Scholar]
- 6.Gregorio L, Brindisi J, Kleppinger A, et al. Adequate dietary protein is associated with better physical performance among post-menopausal women 60-90 years. J Nutr Health Aging. 2014;18(2):155-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Isanejad M, Mursu J, Sirola J, et al. Association of protein intake with the change of lean mass among elderly women: The OSTPRE Fracture Prevention Study (OSTPRE-FPS). J Nutr Sci. 2015;4:e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McDonald CK, Ankarfeldt MZ, Capra S, Bauer J, Raymond K, Heitmann BL. Lean body mass change over 6 years is associated with dietary leucine intake in an older Danish population. Br J Nutr. 2016;115(9):1556-1562. [DOI] [PubMed] [Google Scholar]
- 9.Sahni S, Mangano KM, Hannan MT, Kiel DP, McLean RR. Higher protein intake is associated with higher lean mass and quadriceps muscle strength in adult men and women. J Nutr. 2015;145(7):1569-1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campbell WW, Trappe TA, Wolfe RR, Evans WJ. The recommended dietary allowance for protein may not be adequate for older people to maintain skeletal muscle. J Gerontol A Biol Sci Med Sci. 2001;56(6):M373-M380. [DOI] [PubMed] [Google Scholar]
- 11.Castaneda C, Charnley JM, Evans WJ, Crim MC. Elderly women accommodate to a low-protein diet with losses of body cell mass, muscle function, and immune response. Am J Clin Nutr. 1995;62(1):30-39. [DOI] [PubMed] [Google Scholar]
- 12.Campbell WW, Crim MC, Dallal GE, Young VR, Evans WJ. Increased protein requirements in elderly people: new data and retrospective reassessments. Am J Clin Nutr. 1994;60(4):501-509. [DOI] [PubMed] [Google Scholar]
- 13.Koopman R, Verdijk L, Manders RJ, et al. Co-ingestion of protein and leucine stimulates muscle protein synthesis rates to the same extent in young and elderly lean men. Am J Clin Nutr. 2006;84(3):623-632. [DOI] [PubMed] [Google Scholar]
- 14.Holm L, Olesen JL, Matsumoto K, et al. Protein-containing nutrient supplementation following strength training enhances the effect on muscle mass, strength, and bone formation in postmenopausal women. J Appl Physiol (1985). 2008;105(1):274-281. [DOI] [PubMed] [Google Scholar]
- 15.Fiatarone MA, O’Neill EF, Ryan ND, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med. 1994;330(25):1769-1775. [DOI] [PubMed] [Google Scholar]
- 16.Iglay HB, Apolzan JW, Gerrard DE, Eash JK, Anderson JC, Campbell WW. Moderately increased protein intake predominately from egg sources does not influence whole body, regional, or muscle composition responses to resistance training in older people. J Nutr Health Aging. 2009;13(2):108-114. [DOI] [PubMed] [Google Scholar]
- 17.Campbell WW, Crim MC, Young VR, Joseph LJ, Evans WJ. Effects of resistance training and dietary protein intake on protein metabolism in older adults. Am J Physiol. 1995;268(6, pt 1):E1143-E1153. [DOI] [PubMed] [Google Scholar]
- 18.Meredith CN, Frontera WR, O’Reilly KP, Evans WJ. Body composition in elderly men: effect of dietary modification during strength training. J Am Geriatr Soc. 1992;40(2):155-162. [DOI] [PubMed] [Google Scholar]
- 19.Tieland M, van de Rest O, Dirks ML, et al. Protein supplementation improves physical performance in frail elderly people: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc. 2012;13(8):720-726. [DOI] [PubMed] [Google Scholar]
- 20.Xu ZR, Tan ZJ, Zhang Q, Gui QF, Yang YM. Clinical effectiveness of protein and amino acid supplementation on building muscle mass in elderly people: a meta-analysis. PLoS One. 2014;9(9):e109141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bauer JM, Verlaan S, Bautmans I, et al. Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc. 2015;16(9):740-747. [DOI] [PubMed] [Google Scholar]
- 22.Fukagawa NK. Protein requirements: methodologic controversy amid a call for change. Am J Clin Nutr. 2014;99(4):761-762. [DOI] [PubMed] [Google Scholar]
- 23.National Health and Medical Research Council Recommended Dietary Intakes for Use in Australia. Canberra: Australian Government Publishing Service; 1991. [Google Scholar]
- 24.Bauer J, Biolo G, Cederholm T, et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc. 2013;14(8):542-559. [DOI] [PubMed] [Google Scholar]
- 25.Deutz NE, Bauer JM, Barazzoni R, et al. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr. 2014;33(6):929-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wolfe RR, Miller SL, Miller KB. Optimal protein intake in the elderly. Clin Nutr. 2008;27(5):675-684. [DOI] [PubMed] [Google Scholar]
- 27.Volpi E, Nazemi R, Fujita S. Muscle tissue changes with aging. Curr Opin Clin Nutr Metab Care. 2004;7(4):405-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gersovitz M, Motil K, Munro HN, Scrimshaw NS, Young VR. Human protein requirements: assessment of the adequacy of the current Recommended Dietary Allowance for dietary protein in elderly men and women. Am J Clin Nutr. 1982;35(1):6-14. [DOI] [PubMed] [Google Scholar]
- 29.Lemon PW, Tarnopolsky MA, MacDougall JD, Atkinson SA. Protein requirements and muscle mass/strength changes during intensive training in novice bodybuilders. J Appl Physiol (1985). 1992;73(2):767-775. [DOI] [PubMed] [Google Scholar]
- 30.Tarnopolsky MA, Atkinson SA, MacDougall JD, Chesley A, Phillips S, Schwarcz HP. Evaluation of protein requirements for trained strength athletes. J Appl Physiol (1985). 1992;73(5):1986-1995. [DOI] [PubMed] [Google Scholar]
- 31.Bhasin S, Apovian CM, Travison TG, et al. Design of a randomized trial to determine the optimum protein intake to preserve lean body mass and to optimize response to a promyogenic anabolic agent in older men with physical functional limitation. Contemp Clin Trials. 2017;58:86-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rand WM, Pellett PL, Young VR. Meta-analysis of nitrogen balance studies for estimating protein requirements in healthy adults. Am J Clin Nutr. 2003;77(1):109-127. [DOI] [PubMed] [Google Scholar]
- 33.Bhasin S, Cunningham GR, Hayes FJ, et al. ; Task Force, Endocrine Society . Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536-2559. [DOI] [PubMed] [Google Scholar]
- 34.Apovian CM, Singer MR, Campbell WW, et al. Development of a novel six-month nutrition intervention for a randomized trial in older men with mobility limitations. J Nutr Health Aging. 2017;21(10):1081-1088. [DOI] [PubMed] [Google Scholar]
- 35.Wheeler ML. Nutrient database for the 2003 exchange lists for meal planning. J Am Diet Assoc. 2003;103(7):894-920. [DOI] [PubMed] [Google Scholar]
- 36.Bhasin S, Woodhouse L, Casaburi R, et al. Older men are as responsive as young men to the anabolic effects of graded doses of testosterone on the skeletal muscle. J Clin Endocrinol Metab. 2005;90(2):678-688. [DOI] [PubMed] [Google Scholar]
- 37.Bhasin S, Storer TW, Javanbakht M, et al. Testosterone replacement and resistance exercise in HIV-infected men with weight loss and low testosterone levels. JAMA. 2000;283(6):763-770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.LeBrasseur NK, Bhasin S, Miciek R, Storer TW. Tests of muscle strength and physical function: reliability and discrimination of performance in younger and older men and older men with mobility limitations. J Am Geriatr Soc. 2008;56(11):2118-2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ware J, Kosinski M. SF-36 Physical and Mental Health Summary Scales: A Manual for Users of Version 1.2. Lincoln, RI: Quality Metric; 2005. [Google Scholar]
- 40.Revicki DA, Leidy NK, Howland L. Evaluating the psychometric characteristics of the Psychological General Well-Being Index with a new response scale. Qual Life Res. 1996;5(4):419-425. [DOI] [PubMed] [Google Scholar]
- 41.Cella D, Eton DT, Lai JS, Peterman AH, Merkel DE. Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J Pain Symptom Manage. 2002;24(6):547-561. [DOI] [PubMed] [Google Scholar]
- 42.Derogatis LR. Derogatis Affects Balance Scale (DABS): Preliminary Scoring, Procedures & Administration Manual. Baltimore, MD: Clinical Psychometric Research; 1996. [Google Scholar]
- 43.Fiatarone MA, Marks EC, Ryan ND, Meredith CN, Lipsitz LA, Evans WJ. High-intensity strength training in nonagenarians: effects on skeletal muscle. JAMA. 1990;263(22):3029-3034. [PubMed] [Google Scholar]
- 44.Glickman N, Mitchell HH, Lambert EH, Keeton RW. The total specific dynamic action of high-protein and high-carbohydrate diets on human subjects. J Nutr. 1948;36(1):41-57. [DOI] [PubMed] [Google Scholar]
- 45.Hutchison AT, Piscitelli D, Horowitz M, et al. Acute load-dependent effects of oral whey protein on gastric emptying, gut hormone release, glycemia, appetite, and energy intake in healthy men. Am J Clin Nutr. 2015;102(6):1574-1584. [DOI] [PubMed] [Google Scholar]
- 46.Maurya SK, Bal NC, Sopariwala DH, et al. Sarcolipin is a key determinant of the basal metabolic rate, and its overexpression enhances energy expenditure and resistance against diet-induced obesity. J Biol Chem. 2015;290(17):10840-10849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Campbell WW, Kim JE, Amankwaah AF, Gordon SL, Weinheimer-Haus EM. Higher total protein intake and change in total protein intake affect body composition but not metabolic syndrome indexes in middle-aged overweight and obese adults who perform resistance and aerobic exercise for 36 weeks. J Nutr. 2015;145(9):2076-2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim JE, O’Connor LE, Sands LP, Slebodnik MB, Campbell WW. Effects of dietary protein intake on body composition changes after weight loss in older adults: a systematic review and meta-analysis. Nutr Rev. 2016;74(3):210-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Longland TM, Oikawa SY, Mitchell CJ, Devries MC, Phillips SM. Higher compared with lower dietary protein during an energy deficit combined with intense exercise promotes greater lean mass gain and fat mass loss: a randomized trial. Am J Clin Nutr. 2016;103(3):738-746. [DOI] [PubMed] [Google Scholar]
- 50.Beasley JM, Deierlein AL, Morland KB, Granieri EC, Spark A. Is meeting the recommended dietary allowance (RDA) for protein related to body composition among older adults? results from the Cardiovascular Health of Seniors and Built Environment Study. J Nutr Health Aging. 2016;20(8):790-796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Snyder PJ, Bhasin S, Cunningham GR, et al. ; Testosterone Trials Investigators . Effects of testosterone treatment in older men. N Engl J Med. 2016;374(7):611-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Berner LA, Becker G, Wise M, Doi J. Characterization of dietary protein among older adults in the United States: amount, animal sources, and meal patterns. J Acad Nutr Diet. 2013;113(6):809-815. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable 1. Energy and Protein Distribution in 0.8-g/kg/d and 1.3-g/kg/d Groups
eTable 2. Dietary Adherence With Packaged Meals and Supplements During Months 1 to 3 and Months 4 to 6
eTable 3. Estimated Protein and Energy Intake From 24-Hour Food Recalls
eTable 4. Model-Based Estimates of Mean Change in Laboratory Variables by Intervention Groups, With Estimated Differences Attributable to the 2 Interventions
eTable 5. Model-Based Estimates of Mean Change in Outcomes by Intervention Groups, With Estimated Differences Attributable to the 2 Interventions
eTable 6. Adverse Event and Serious Adverse Event Profile by Randomized Group and Physiologic System
eMethods. Supplemental Methods
eFigure 1. Total Body Mass
eFigure 2. Patient-Reported Outcomes