Abstract
This cross-sectional analysis of Medicare data determined the specialty of physicians providing mechanical thrombectomy to patients with ischemic stroke.
Optimal stroke management requires sufficient availability of physicians qualified to perform mechanical thrombectomy. Little is known about the US workforce for this recently established, evidence-based procedure.1
Methods
We performed a cross-sectional study using a data set from the US Centers for Medicare and Medicaid Services containing claims for care provided between January 1, 2009, and September 30, 2015, to a nationally representative 5% sample of Medicare beneficiaries. The institutional review board at Weill Cornell Medical College approved this study. The institutional review board waived the requirement for informed consent for this minimal-risk research.
We included beneficiaries 65 years or older who had been enrolled in fee-for-service Medicare for 1 year or longer within the 6-year timeframe of the data set, or until death, without concurrent Medicare Advantage enrollment. We analyzed the claims submitted during hospitalizations for acute ischemic stroke, defined by validated International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes.2,3 We defined mechanical thrombectomy as a claim with Current Procedural Terminology code 37184 combined with an ICD-9-CM code for cerebrovascular disease (430-438).
We classified specialties using codes that reflect the self-designated specialty of clinicians at the time of enrollment in Medicare. Python software was used to look up the physician name and specialty associated with the National Provider Identifier (NPI) numbers that appeared on claims. Investigators blinded to the specialty designations used these names and NPI numbers to search public online records (via Google) regarding the residency and fellowship training of each clinician.
In sensitivity analyses, we redefined thrombectomy as a physician claim with an isolated Current Procedural Terminology code of 37184 plus an ischemic stroke ICD-9-CM diagnosis code as the sole indication. We also limited the sample to ICD-9-CM code 434.11 for embolic stroke.
We used descriptive statistics with 95% CIs, κ statistics, and χ2 tests with 2-tailed α = .05. Analyses were performed using Python version 3.6.1 (Python Software Foundation) and Stata/MP version 14 (StataCorp).
Results
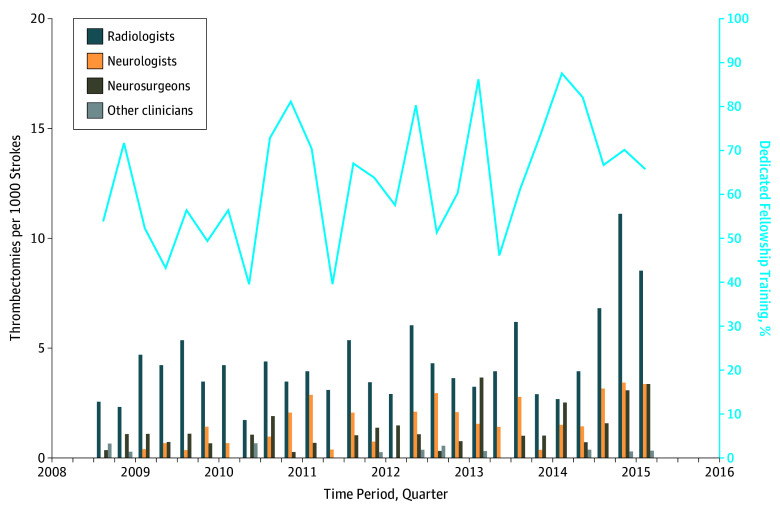
Of the 555 thrombectomies performed during 77 774 stroke hospitalizations in the data set, 341 (61.4%; 95% CI, 57.2%-65.5%) were performed by radiologists, 110 (19.8%; 95% CI, 16.6%-23.4%) by neurologists, 91 (16.4%; 95% CI, 13.4%-19.7%) by neurosurgeons, and 13 (2.4%; 95% CI, 1.3%-4.0%) by other physicians; 367 (66.1%; 95% CI, 62.0%-70.1%) were performed by physicians with dedicated neurointerventional fellowship training. The specialty codes present in the data from the US Centers for Medicare and Medicaid Services had excellent agreement with NPI numbers (agreement rate, 89.0%; κ, 0.81) and Google search results (agreement rate, 91.5%; κ, 0.85). The distribution of specialties was similar regardless of how they were designated (Table). Clinician characteristics did not change significantly after December 17, 2014, when the first trial to show a clinical benefit for thrombectomy was published (Figure).1 The findings were similar in sensitivity analyses.
Table. Clinician Specialty Among Cases of Mechanical Thrombectomy for Ischemic Stroke in a 5% Sample of Medicare Beneficiaries.
| Clinician Specialty | No. (%) | ||
|---|---|---|---|
| CMSa | NPIb | Googlec | |
| Radiology | 341 (61.4) | 328 (59.2) | 316 (56.9) |
| Neurosurgery | 91 (16.4) | 99 (17.9) | 95 (17.1) |
| Neurology | 110 (19.8) | 108 (19.5) | 131 (23.6) |
| Other | 13 (2.4) | 20 (3.4) | 13 (2.4) |
Abbreviations: CMS, Centers for Medicare and Medicaid Services; NPI, National Provider Identifier.
Provider specialty as self-designated at the time of enrollment in Medicare.
Provider specialty as self-designated on the NPI application.
Provider specialty as ascertained from review of publicly available online records.
Figure. Temporal Changes in Stroke-Related Mechanical Thrombectomy Rates and Backgrounds of Performing Physicians.
The publication date of the Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands trial,1 which was the first trial to show a clinical benefit for thrombectomy, was December 17, 2014.
Discussion
In a nationally representative cohort of elderly patients with stroke, most mechanical thrombectomies were performed by radiologists, neurologists, and neurosurgeons. Other specialists performed fewer than 1 in 30 procedures.
Our study has limitations. First, the data set included only patients 65 years or older; however, such patients account for most strokes in the United States. Second, interventionalists who treat patients with Medicare Advantage plans may differ from those who treat fee-for-service Medicare beneficiaries. However, more than 70% of Medicare beneficiaries are in fee-for-service Medicare. Third, although we used all publicly available data to assess the training of physicians, the sparse regulation of neurointerventional fellowships meant that we could not make definite statements on the type or quality of the fellowship training that these clinicians received.
It has been argued that a workforce shortage exists that could be filled by non-neuroscience clinicians with expertise in catheter-based procedures.4 Neurointerventionalists have countered that they are available to most US patients,5 but vascular neurologists have nevertheless raised concerns about a shortage.6 It has remained unclear to what extent thrombectomies are being performed by specialists outside of radiology and clinical neuroscience specialties. Small case series7 have reported stroke-related mechanical thrombectomies performed by cardiologists in specific hospitals, but, to our knowledge, nationally representative data have been lacking. By filling this knowledge gap, this study may help shed light on the current standard of care for mechanical thrombectomy and inform plans for optimizing systems of acute stroke care across the United States.
References
- 1.Berkhemer OA, Fransen PS, Beumer D, et al. ; MR CLEAN Investigators . A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20. [DOI] [PubMed] [Google Scholar]
- 2.Tirschwell DL, Longstreth WT Jr. Validating administrative data in stroke research. Stroke. 2002;33(10):2465-2470. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . International Classification of Diseases, Ninth Revision (ICD-9). Geneva, Switzerland: World Health Organization; 1977. [Google Scholar]
- 4.Hopkins LN, Holmes DR Jr. Public health urgency created by the success of mechanical thrombectomy studies in stroke. Circulation. 2017;135(13):1188-1190. [DOI] [PubMed] [Google Scholar]
- 5.Suzuki S, Saver JL, Scott P, et al. Access to intra-arterial therapies for acute ischemic stroke: an analysis of the US population. AJNR Am J Neuroradiol. 2004;25(10):1802-1806. [PMC free article] [PubMed] [Google Scholar]
- 6.Grotta JC, Lyden P, Brott T. Rethinking training and distribution of vascular neurology interventionists in the era of thrombectomy. Stroke. 2017;48(8):2313-2317. [DOI] [PubMed] [Google Scholar]
- 7.DeVries JT, White CJ, Collins TJ, et al. Acute stroke intervention by interventional cardiologists. Catheter Cardiovasc Interv. 2009;73(5):692-698. [DOI] [PubMed] [Google Scholar]