Key Points
Questions
What are the issues with health care access and affordability for cancer survivors compared with non–cancer-affected control respondents, and how did the proportion of survivors reporting these issues change over time?
Findings
In this population-based study of 30 364 participants using 2010 to 2016 data from the National Health Interview Survey, cancer survivors were more likely than control respondents to report delayed or forgone health care, and inability to afford medications and health care services. The proportion of cancer survivors reporting delayed or forgone care and inability to afford health care services significantly decreased during implementation of the Affordable Care Act (2010-2016).
Meaning
Despite recent improvements, cancer survivors continue to experience difficulties accessing and affording health care.
This population-based study analyzes cancer survivors’ ability to access and afford health care during implementation of the US Affordable Care Act using data from the 2010 to 2016 National Health Interview Survey.
Abstract
Importance
Cancer survivors face ongoing health issues and need access to affordable health care, yet studies examining health care access and affordability in this population are lacking.
Objectives
To evaluate health care access and affordability in a national sample of cancer survivors compared with adults without cancer and to evaluate temporal trends during implementation of the Affordable Care Act.
Design, Setting, and Participants
We used data from the National Health Interview Survey from 2010 through 2016 to conduct a population-based study of 30 364 participants aged 18 years or older. We grouped participants as cancer survivors (n = 15 182) and those with no reported history of cancer, whom we refer to as control respondents (n = 15 182), matched on age. We excluded individuals reporting a cancer diagnosis prior to age 18 years and those with nonmelanoma skin cancers.
Main Outcomes and Measures
We compared issues with health care access (eg, delayed or forgone care) and affordability (eg, unable to afford medications or health care services) between cancer survivors and control respondents. We also explored trends over time in the proportion of cancer survivors reporting these difficulties.
Results
Of the 30 364 participants, 18 356 (57.4%) were women. The mean (SD) age was 63.5 (23.5) years. Cancer survivors were more likely to be insured (14 412 [94.8%] vs 13 978 [92.2%], P < .001) and to have government-sponsored insurance (7266 [44.3%] vs 6513 [38.8%], P < .001) compared with control respondents. In multivariable models, cancer survivors were more likely than control respondents to report delayed care (odds ratio [OR], 1.38; 95% CI, 1.16-1.63), forgone medical care (OR, 1.76; 95% CI, 1.45-2.12), and/or inability to afford medications (OR, 1.77; 95% CI, 1.46-2.14) and health care services (OR, 1.46; 95% CI, 1.27-1.68) (P < .001 for all). From 2010 to 2016, the proportion of survivors reporting delayed medical care decreased each year (B = 0.47; P = .047), and the proportion of those needing and not getting medical care also decreased each year (B = 0.35; P = .04). In addition, the proportion of cancer survivors who reported being unable to afford prescription medication decreased each year (B=0.66; P = .004) and the proportion of those unable to afford at least 1 of 6 services decreased each year (B = 0.51; P = .01).
Conclusions and Relevance
Despite higher rates of insurance coverage, cancer survivors reported greater difficulties accessing and affording health care compared with adults without cancer. Importantly, the proportion of survivors reporting these issues continued a downward trend throughout our observation period in the years following the implementation of the Affordable Care Act. Our findings suggest incremental improvement in health care access and affordability after recent health care reform and provide an important benchmark as additional changes are likely to occur in the coming years.
Introduction
The number of cancer survivors continues to rise, with recent estimates reporting over 15 million Americans with a medical history of cancer alive today.1 Cancer survivors often require management of treatment-related late-effects, monitoring for subsequent malignant disease, and treatment of comorbid medical conditions.2,3,4,5,6,7 In addition, cancer survivors are more likely to experience physical and mental health issues compared with those without a medical history of cancer, often necessitating referral to multiple physician specialists.7,8,9,10,11 Thus, cancer survivors have unique, long-term health care needs and access to timely and affordable care is essential for these individuals.
Despite cancer survivors’ need for long-term access to high-quality and affordable health care, this population is at particularly high risk for experiencing financial burden related to the high costs of their care, which may negatively influence their ability to receive necessary survivorship care. Growing evidence demonstrates that patients with cancer experience substantial economic hardship related to their care, yet barriers to accessing and affording care experienced by cancer survivors remain understudied.12,13,14,15,16 Prior work has shown that patients with a cancer history experience issues related to disability, loss of work, and trouble obtaining affordable health insurance.7,17,18,19 In addition, survivors often require ongoing medical care for years after their initial cancer treatment, and the high out-of-pocket costs associated with their care can add to their financial struggles.20,21 Thus, cancer survivors are at risk for experiencing loss of income and financial burden related to their medical issues, which can last for years after their cancer diagnosis.21,22,23 Moreover, the financial barriers to care experienced by these individuals can negatively impact their health outcomes, including poorer quality of life, increased symptom burden, and potentially higher mortality.14,16,24
Previous research suggests that financial concerns represent a barrier to accessing medical services among cancer survivors.25,26,27,28,29 However, these studies were conducted prior to recent health care reform, which was designed to improve access to affordable health care, particularly for medically vulnerable individuals.30,31 In addition, health care costs have risen in recent years, with concomitant increases in the out-of-pocket medical expenditures incurred by patients.32,33,34 Therefore, we sought to conduct an updated analysis of cancer survivors’ ability to access and afford health care using data from the 2010 to 2016 National Health Interview Survey (NHIS). Specifically, we aimed to compare difficulties accessing and affording medical care in a national sample of cancer survivors and a group of control respondents with no medical history of cancer. We hypothesized that cancer survivors would report more difficulties accessing and affording health care compared with controls. In addition, we sought to explore whether issues related to health care access and affordability had changed over time, given the health care reform efforts in recent years. Although the Affordable Care Act (ACA) was signed into law in 2010, the provisions were rolled out over the following years, and many of the changes affecting the availability and terms of insurance became effective in January 2014.35 Importantly, studies examining whether ACA provisions effectively address the financial burden of cancer survivors are lacking.36 This provides an opportunity to evaluate both the financial burden and barriers to care experienced by the growing population of cancer survivors in the United States to examine the impact of recent health care reform efforts as policy debates over access and coverage continue.
Methods
Study Design and Participant Sample
We conducted a population-based study using cross-sectional data from serial samples of the National Health Interview Survey (NHIS) from 2010 through 2016, a nationally representative sample of nonmilitary and noninstitutionalized individuals living in the United States.37 The National Center for Health Statistics uses computer-assisted personal interviewing to administer the NHIS survey annually and collect health-related information from participants. We used data from the adult interview and the household survey. The NHIS asks participants if they had ever been told by a physician or health professional that they had cancer or a malignant abnormality of any kind, and if yes, the type of cancer and age of diagnosis. We compared 2 groups of adults: adult cancer survivors and adults with no reported history of cancer, whom we refer to as control respondents. We categorized any individual who reported receiving a cancer diagnosis after age 18 years as a cancer survivor. Owing to the important confounding potential of participant age on issues related to health care access and affordability,27,28,38 we chose to match control respondents based on age at the time of the survey within 1 year. We excluded individuals reporting a cancer diagnosis prior to age 18 years. In addition, we excluded individuals with nonmelanoma skin cancers, consistent with other studies involving cancer survivors.17,22,39
Measures
Sociodemographics
The NHIS includes sociodemographic data regarding participants’ age at the time of the survey, geographic region, sex, race/ethnicity, marital status, whether individuals had access to paid sick leave (at their current job or, if not currently working, on the job they previously held the longest), household income, whether the individual worked for pay, and educational status. The survey also contains information about whether the individual has health insurance, and for those who do, asks if they have any coverage by government-sponsored insurance (including Medicaid and Medicare) and/or any coverage by private insurance. The Partners institutional review board considered this study exempt from review.
Health Care Access
To examine issues regarding health care access, we used questions asking participants to report if their medical care had been delayed in the past 12 months because of worry about the cost (yes/no). We also used data asking participants if there was any time during the past 12 months when they needed medical care but did not get it because they could not afford it (yes/no).
Health Care Affordability
To assess issues related to health care affordability, we used questions asking participants to report if they could afford different types of care and services in the previous 12 months (yes/no), specifically: prescription medications, mental health care, dental care, eyeglasses, specialist care, and follow-up care. We used this information to compute a dichotomous affordability variable that indicated whether the participant reported that they were unable to afford at least 1 of these 6 services in the previous 12 months (yes/no).
Statistical Analyses
We used descriptive statistics to examine the frequencies and means of the study variables. We compared participant sociodemographics between cancer survivors and control respondents using unadjusted binary logistic regression. To determine differences between survivors and control respondents with regard to care access and affordability, we used logistic regression, adjusted for prespecified potential confounders such as age, sex, race, ethnicity, marital status, survey year, region, education, employment, paid sick leave status, household income, and insurance type. Specifically, our models tested these 4 binary outcomes: (1) medical care delayed in the previous 12 months; (2) needed, but did not get medical care in the previous 12 months; (3) unable to afford prescription medication in the previous 12 months; and (4) unable to afford any of 6 services (medications, follow-up care, specialist care, mental health care, dental care, eyeglasses). We chose these outcome variables because we felt they best represented issues of health care access and affordability, were consistently asked from years 2010 to 2016, and are consistent with prior research.25,26,27,28 To address multiple comparisons, we applied a Bonferroni correction to the 4 outcomes assessed in the multivariable models using a corrected significance threshold of P = .01. To explore trends in the proportion of cancer survivors reporting issues with health care access and affordability over time, we used univariate generalized linear models with the weighted proportion of cancer survivors reporting each outcome as the dependent variable and year as the independent variable. We used NHIS weighting in all models, as per guidelines,40 and performed analyses using SAS statistical software (version 9.4, SAS Institute Inc).
Results
Participant Sample
The age-matched sample of adult respondents aged 18 years or older (n = 30 364) included 15 182 cancer survivors and 15 182 control respondents (eTable 1 in the Supplement). Cancer survivors were more likely to be insured (94.8% vs 92.2%, P < .001) and to have government-sponsored insurance (44.3% vs 38.8%, P < .001) compared with control respondents. In addition, cancer survivors were more likely to have paid sick leave (59.4% vs 57.1%, P = .002). Cancer survivors were less likely to be working for pay (31.4% vs 38.3%, P < .001) and to have less than a high school education (13.6% vs 16.6%, P < .001).
Health Care Access
Cancer survivors reported more problems related to health care access compared with control respondents. On multivariable logistic regression, survivors were more likely to report delayed medical care (odds ratio [OR], 1.38; 95% CI, 1.16-1.63; P < .001) and needing but not getting medical care (OR, 1.76; 95% CI, 1.45-2.12; P < .001) compared with control respondents (Table). Within the entire sample, being unmarried, having no paid sick leave, lower income, and not having government-sponsored or private health insurance were associated with health care access issues on multivariable analysis.
Table. Health Care Accessibility and Affordability Issues in the Previous 12 Months for Cancer Survivors and Control Respondents.
| Multivariable Models of Cancer Survivors vs Control Respondentsa | Odds Ratio (95% CI)b |
|---|---|
| Health care accessibility issues in the previous 12 months | |
| Medical care delayed | 1.38 (1.16-1.63) |
| Needed but did not get medical care | 1.76 (1.45-2.12) |
| Health care affordability issues in the previous 12 months | |
| Unable to afford prescription medication | 1.77 (1.46-2.14) |
| Unable to afford at least 1 of 6 servicesc | 1.46 (1.27-1.68) |
Models adjusted for age, sex, race, ethnicity, marital status, survey year, region, education, employment, paid sick leave status, household income, and insurance type.
P < .001 for all.
Unable to afford at least 1 of the following: medications, follow-up care, specialist care, mental health care, dental care, eyeglasses.
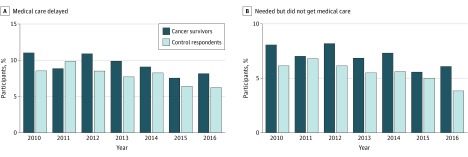
Figure 1 displays the proportion of cancer survivors and control respondents reporting problems related to health care access from 2010 to 2016. The proportion of survivors reporting delayed medical care decreased by 0.47 percentage points per year (B = 0.47; P = .047), and the proportion of those needing and not getting medical care decreased by 0.35 percentage points each year (B = 0.35; P = .04).
Figure 1. Proportion of Cancer Survivors and Control Respondents Reporting Issues With Health Care Access in the Previous 12 Months by Survey Year.
Health Care Affordability
Cancer survivors reported more difficulties with health care affordability compared with control respondents. Multivariable analyses demonstrated that survivors were more likely to report being unable to afford prescription medication (OR, 1.77; 95% CI, 1.46-2.14; P < .001) and being unable to afford at least 1 of 6 services (OR, 1.46; 95% CI, 1.27-1.68; P < .001) compared with control respondents (Table). Multivariable models of the entire sample demonstrated that female sex, being unmarried, having no paid sick leave, lower income, and not having government-sponsored or private health insurance were all associated with being more likely to report health care affordability issues. As a sensitivity analysis, we compared the proportion of survivors and control respondents who could afford all 6 services, and found that cancer survivors had lower odds of being able to afford all 6 services (OR, 0.68; 95% CI, 0.60-0.79; P < .001).
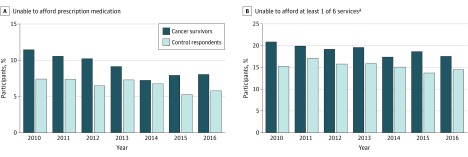
Figure 2 displays the proportion of cancer survivors and control respondents reporting problems related to health care affordability from 2010 through 2016. The proportion of cancer survivors who reported being unable to afford prescription medication decreased each year (B = 0.66; P = .004) and the proportion of those unable to afford at least 1 of 6 services decreased each year (B = 0.51; P = .01).
Figure 2. Proportion of Cancer Survivors and Control Respondents Reporting Issues With Health Care Affordability in the Previous 12 Months by Survey Year.
aUnable to afford at least 1 of the following: medications, follow-up care, specialist care, mental health care, dental care, eyeglasses.
Discussion
We examined health care access and affordability issues using a national sample of cancer survivors and demonstrated that survivors, despite higher rates of insurance coverage and more education, were more likely to report difficulties accessing and affording medical care owing to costs than individuals with no medical history of cancer. Compared with control respondents, we found that cancer survivors were more likely to report delaying and forgoing medical care as well as an inability to afford prescription medications and trouble affording certain health care services. Notably, we also found a decreasing trend in the proportion of cancer survivors reporting health care access and affordability concerns in more recent years. Collectively, these findings underscore the ongoing financial burden experienced by cancer survivors, despite potential improvements in recent years.
Importantly, our results suggest that problems with health care access and affordability may have been ameliorated during our observation period. This is a critical finding, considering that the survey data tracked information during the years surrounding implementation of the ACA.30,31 Specifically, we found decreasing trends in the proportion of survivors reporting delayed and forgone medical care as well as the inability to afford medications and health care services. Prior research suggests that the ACA could potentially increase the availability of insurance and expand coverage to additional services important for cancer survivors, and thereby reduce the financial burden experienced by these individuals.36,41,42 Of note, although the ACA was signed into law in 2010, many of the changes affecting the availability and terms of insurance became effective in 2014, yet our findings suggest a steady decrease in issues related to health care access and affordability from 2010 to 2016. This fact, in addition to our lack of data prior to 2010, limit our ability to definitively state that the ACA alone caused the decreasing trends in health care access and affordability issues. Furthermore, although the absolute reduction in the percentage of cancer survivors reporting health care access and affordability issues over time appeared to be somewhat modest in our study, it is noteworthy that these improvements occurred in the context of increasing drug prices for cancer and many other indications.43,44 By demonstrating that issues related to health care access and affordability appear to have decreased in recent years, our results have key implications for future policy discussions surrounding health care reform and should serve as a current benchmark.
Our work adds to a growing body of literature identifying the financial concerns experienced by patients with cancer. Based on our findings, we believe that future efforts should seek to assess and address the adverse consequences of the financial burden experienced by survivors of cancer. Such efforts will be instrumental in: (1) understanding how health care costs can influence patients’ approach to their medical care and decision making, (2) identifying patients with cancer who may be more likely to experience problems accessing and affording needed medical care, and (3) providing tailored counseling or financial support services that meet the unique needs of these patients. In addition, an improved understanding of the financial barriers to care encountered by cancer survivors may help clinicians anticipate care accessibility and affordability issues to better meet the needs of these individuals.45,46,47 Notably, cancer survivors have an ongoing and increased need for posttreatment care coordination, including proper monitoring for cancer recurrence, late-effects of treatment, and guidance on a healthy lifestyle, which necessitate continued access to efficient and high-value care.36,48 Thus, our study successfully demonstrates that cancer survivors encounter barriers to affordable and accessible health care, and our findings should motivate future efforts to better support this population and improve their survivorship care.
Our findings expand on previous work demonstrating that cancer survivors often experience issues with health care affordability and access.25,26,27,28,29 Consistent with prior research, our findings suggest that survivors may be more likely to have health insurance compared with those without a medical history of cancer, and their insurance was more likely to be government-sponsored insurance.25 Despite this fact, and our data suggesting the positive effects of having either private or government-sponsored insurance, cancer survivors still had greater odds of experiencing problems with health care access and affordability. These findings highlight the limits of evaluating health insurance coverage alone as a surrogate for access to affordable, high-quality care and are particularly important as national debates over health care center on questions of both the affordability (premiums and subsidies) and the content (regulation of covered services) of health insurance. Also aligning with prior studies, we found that being unmarried, having a lower income, and the absence of paid sick leave at work were all associated with reporting difficulties with health care affordability and access.39,49,50,51 Notably, cancer survivors were more likely than controls to have paid sick leave at work, which may suggest that survivors are aware of and seek employment that provides this benefit. Thus, our findings provide valuable insights highlighting that cancer survivors experience considerable barriers to accessing affordable health care, while also identifying those at greater risk for experiencing adverse consequences of the high costs of health care. Although screening for financial burden may benefit all patients with cancer, clinicians caring for cancer survivors in primary care and other settings should be alert to the need for increased attention to financial barriers to care among this population.
Limitations
Several limitations of our study are worth noting. First, this was a cross-sectional analysis of annual surveys over repeated years, and we cannot determine the directionality of the associations we observed. Also, because the same participants are not included in each year's survey, we could not evaluate changes within participants across years. Second, we relied on self-reported questionnaires, and thus participants’ responses may be limited by their ability to accurately recall the issues they experienced regarding health care access and affordability. In addition, cancer survivors may be more likely than control respondents to report problems with health care access and affordability, given their likelihood of having greater medical needs and their understanding of the importance of having access to affordable health care.25,26,27 However, we lack information about respondents’ perception of the need for health care services. Third, our results may not generalize to cancer survivors with more advanced cancers, those with shorter survival, or those with poorer health because the NHIS does not include institutionalized individuals and we lack information about those who were too sick to complete the survey.52 We also lack information about cancer stage, grade, and treatment received for the survivors in our sample, and thus we cannot comment on the influence of these important factors. Moreover, we cannot distinguish the type of government-sponsored insurance, and data suggest that patients with Medicaid may have worse outcomes than other patients.53 Lastly, we cannot determine the long-term consequences of the care affordability and access issues reported by those in our study, but future work should seek to investigate how these reported issues with access and affordability impact cancer survivors’ use of health care services, their quality of life, and the quality of their survivorship care.
Conclusions
We demonstrated that cancer survivors are more likely to experience problems accessing and affording needed health care compared with adults without a medical history of cancer. In addition, we found that survivors were more likely than control respondents to report delayed and forgone medical care and having an inability to afford prescriptions and other health care services, despite being more likely to have health insurance, higher education, and paid sick leave at work. Notably, our findings suggest that survivors’ struggles to access and afford medical care decreased during our observation period, coincident with implementation and expanding coverage under the ACA, although we cannot attribute this to any specific ACA provision. Moreover, our study spans a time of important national initiatives, such as the Choosing Wisely campaign, which focus on changing the discussion in health care regarding efficient and high-value care, which could have altered survivors’ demand for health care.54,55,56 Thus, our results provide important evidence during this time of change as debate over health care reform continues. With the growing number of cancer survivors and the rising costs of health care in the United States, future efforts to enhance access to affordable health care should build on our findings and focus on improving our understanding of specific financial barriers, consequences of these barriers, and opportunities to screen for and address patients’ financial burden and barriers to care.
eTable 1. Participant Characteristics
eTable 2. Health Care Accessibility Issues in the Previous 12 Months for Cancer Survivors and Control Respondents
eTable 3. Health Care Affordability Issues in the Previous 12 Months for Cancer Survivors and Control Respondents
eTable 4. Ability to Afford All Six Health Care Services in the Previous 12 Months for Cancer Survivors and Control Respondents
eTable 5. Questions Related to Health Care Access and Affordability from the National Health Interview Survey (NHIS)
References
- 1.Miller KD, Siegel RL, Lin CC, et al. . Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271-289. [DOI] [PubMed] [Google Scholar]
- 2.Friedman DL, Whitton J, Leisenring W, et al. . Subsequent neoplasms in 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. J Natl Cancer Inst. 2010;102(14):1083-1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reulen RC, Frobisher C, Winter DL, et al. ; British Childhood Cancer Survivor Study Steering Group . Long-term risks of subsequent primary neoplasms among survivors of childhood cancer. JAMA. 2011;305(22):2311-2319. [DOI] [PubMed] [Google Scholar]
- 4.Ness KK, Krull KR, Jones KE, et al. . Physiologic frailty as a sign of accelerated aging among adult survivors of childhood cancer: a report from the St Jude Lifetime cohort study. J Clin Oncol. 2013;31(36):4496-4503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edwards BK, Noone AM, Mariotto AB, et al. . Annual Report to the Nation on the status of cancer, 1975-2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2014;120(9):1290-1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robison LL, Hudson MM. Survivors of childhood and adolescent cancer: life-long risks and responsibilities. Nat Rev Cancer. 2014;14(1):61-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: age, health, and disability. J Gerontol A Biol Sci Med Sci. 2003;58(1):82-91. [DOI] [PubMed] [Google Scholar]
- 8.Vuotto SC, Krull KR, Li C, et al. . Impact of chronic disease on emotional distress in adult survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer. 2017;123(3):521-528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell AJ, Ferguson DW, Gill J, Paul J, Symonds P. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol. 2017;14(8):721-732. [DOI] [PubMed] [Google Scholar]
- 10.Hawkins NA, Soman A, Buchanan Lunsford N, Leadbetter S, Rodriguez JL. Use of medications for treating anxiety and depression in cancer survivors in the United States. J Clin Oncol. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prasad PK, Hardy KK, Zhang N, et al. . Psychosocial and neurocognitive outcomes in adult survivors of adolescent and early young adult cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2015;33(23):2545-2552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ubel PA, Abernethy AP, Zafar SY. Full disclosure--out-of-pocket costs as side effects. N Engl J Med. 2013;369(16):1484-1486. [DOI] [PubMed] [Google Scholar]
- 13.Zafar SY, Peppercorn JM, Schrag D, et al. . The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lathan CS, Cronin A, Tucker-Seeley R, Zafar SY, Ayanian JZ, Schrag D. Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J Clin Oncol. 2016;34(15):1732-1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramsey S, Blough D, Kirchhoff A, et al. . Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood). 2013;32(6):1143-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramsey SD, Bansal A, Fedorenko CR, et al. . Financial Insolvency as a Risk Factor for Early Mortality Among Patients With Cancer. J Clin Oncol. 2016;34(9):980-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yabroff KR, Lawrence WF, Clauser S, Davis WW, Brown ML. Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst. 2004;96(17):1322-1330. [DOI] [PubMed] [Google Scholar]
- 18.Kirchhoff AC, Kuhlthau K, Pajolek H, et al. . Employer-sponsored health insurance coverage limitations: results from the Childhood Cancer Survivor Study. Support Care Cancer. 2013;21(2):377-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Boer AG, Taskila T, Ojajärvi A, van Dijk FJ, Verbeek JH. Cancer survivors and unemployment: a meta-analysis and meta-regression. JAMA. 2009;301(7):753-762. [DOI] [PubMed] [Google Scholar]
- 20.Narang AK, Nicholas LH. Out-of-pocket spending and financial burden among Medicare beneficiaries with cancer. JAMA Oncol. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nipp RD, Kirchhoff AC, Fair D, et al. . Financial burden in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2017;35(30):3474-3481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guy GP Jr, Ekwueme DU, Yabroff KR, et al. . Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;31(30):3749-3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zajacova A, Dowd JB, Schoeni RF, Wallace RB. Employment and income losses among cancer survivors: Estimates from a national longitudinal survey of American families. Cancer. 2015;121(24):4425-4432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kale HP, Carroll NV. Self-reported financial burden of cancer care and its effect on physical and mental health-related quality of life among US cancer survivors. Cancer. 2016;122(8):283-289. [DOI] [PubMed] [Google Scholar]
- 25.Sabatino SA, Coates RJ, Uhler RJ, Alley LG, Pollack LA. Health insurance coverage and cost barriers to needed medical care among U.S. adult cancer survivors age<65 years. Cancer. 2006;106(11):2466-2475. [DOI] [PubMed] [Google Scholar]
- 26.Weaver KE, Rowland JH, Bellizzi KM, Aziz NM. Forgoing medical care because of cost: assessing disparities in healthcare access among cancer survivors living in the United States. Cancer. 2010;116(14):3493-3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kent EE, Forsythe LP, Yabroff KR, et al. . Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer. 2013;119(20):3710-3717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zheng Z, Han X, Guy GP Jr, et al. . Do cancer survivors change their prescription drug use for financial reasons? findings from a nationally representative sample in the United States. Cancer. 2017;123(8):1453-1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gonzales F, Zheng Z, Yabroff KR. Trends in financial access to prescription drugs among cancer survivors. J Natl Cancer Inst. 2018;110(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wharam JF, Ross-Degnan D, Rosenthal MB. The ACA and high-deductible insurance—strategies for sharpening a blunt instrument. N Engl J Med. 2013;369(16):1481-1484. [DOI] [PubMed] [Google Scholar]
- 31.Public Law 111-148, Patient Protection and Affordable Care Act, March 23, 2010.
- 32.Adrion ER, Ryan AM, Seltzer AC, Chen LM, Ayanian JZ, Nallamothu BK. Out-of-Pocket Spending for Hospitalizations Among Nonelderly Adults. JAMA Intern Med. 2016;176(9):1325-1332. [DOI] [PubMed] [Google Scholar]
- 33.Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Warren JL, Yabroff KR, Meekins A, Topor M, Lamont EB, Brown ML. Evaluation of trends in the cost of initial cancer treatment. J Natl Cancer Inst. 2008;100(12):888-897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Obama B. United States Health Care Reform: Progress to Date and Next Steps. JAMA. 2016;316(5):525-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leopold C, Park ER, Nekhlyudov L. The impact of the Affordable Care Act on cancer survivorship. Cancer J. 2017;23(3):181-189. [DOI] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention National Health Interview Survey (NHIS). Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2010-2013. http://www.cdc.gov/nchs/nhis.htm. Accessed June 30, 2015.
- 38.Banthin JS, Bernard DM. Changes in financial burdens for health care: national estimates for the population younger than 65 years, 1996 to 2003. JAMA. 2006;296(22):2712-2719. [DOI] [PubMed] [Google Scholar]
- 39.Yabroff KR, Dowling EC, Guy GP Jr, et al. . Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34(3):259-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention Variance Estimation Guidance, NHIS 2016. https://www.cdc.gov/nchs/data/nhis/2016var.pdf. Accessed December 6, 2017.
- 41.Davidoff AJ, Hill SC, Bernard D, Yabroff KR. The Affordable Care Act and expanded insurance eligibility among nonelderly adult cancer survivors. J Natl Cancer Inst. 2015;107(9):djv181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Griffith K, Evans L, Bor J. The Affordable Care Act reduced socioeconomic disparities in health care access [published online July 26, 2017]. Health Aff (Millwood). 10.1377/hlthaff.2017.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Howard DH, Bach PB, Berndt ER, Conti RM. Pricing in the market for anticancer drugs. J Econ Perspect. 2015;29(1):139-162. [DOI] [PubMed] [Google Scholar]
- 44.Dusetzina SB. Drug pricing trends for orally administered anticancer medications reimbursed by commercial health plans, 2000-2014. JAMA Oncol. 2016;2(7):960-961. [DOI] [PubMed] [Google Scholar]
- 45.Schrag D, Hanger M. Medical oncologists’ views on communicating with patients about chemotherapy costs: a pilot survey. J Clin Oncol. 2007;25(2):233-237. [DOI] [PubMed] [Google Scholar]
- 46.Zafar SY, Chino F, Ubel PA, et al. . The utility of cost discussions between patients with cancer and oncologists. Am J Manag Care. 2015;21(9):607-615. [PubMed] [Google Scholar]
- 47.Kelly RJ, Forde PM, Elnahal SM, Forastiere AA, Rosner GL, Smith TJ. Patients and physicians can discuss costs of cancer treatment in the clinic. J Oncol Pract. 2015;11(4):308-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Denlinger CS, Ligibel JA, Are M, et al. . NCCN guidelines insights: survivorship, version 1.2016. J Natl Compr Canc Netw. 2016;14(6):715-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jagsi R, Pottow JA, Griffith KA, et al. . Long-term financial burden of breast cancer: experiences of a diverse cohort of survivors identified through population-based registries. J Clin Oncol. 2014;32(12):1269-1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nipp RD, Zullig LL, Samsa G, et al. . Identifying cancer patients who alter care or lifestyle due to treatment-related financial distress. Psychooncology. 2016;25(6):719-725. [DOI] [PubMed] [Google Scholar]
- 51.Veenstra CM, Regenbogen SE, Hawley ST, Abrahamse P, Banerjee M, Morris AM. Association of paid sick leave with job retention and financial burden among working patients with colorectal cancer. JAMA. 2015;314(24):2688-2690. [DOI] [PubMed] [Google Scholar]
- 52.Hewitt M, Breen N, Devesa S. Cancer prevalence and survivorship issues: analyses of the 1992 National Health Interview Survey. J Natl Cancer Inst. 1999;91(17):1480-1486. [DOI] [PubMed] [Google Scholar]
- 53.Ellis L, Canchola AJ, Spiegel D, Ladabaum U, Haile R, Gomez SL. Trends in cancer survival by health insurance status in California from 1997 to 2014 [published online November 30, 2017]. JAMA Oncol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hahn EE, Tang T, Lee JS, et al. . Use of posttreatment imaging and biomarkers in survivors of early-stage breast cancer: inappropriate surveillance or necessary care? Cancer. 2016;122(6):908-916. [DOI] [PubMed] [Google Scholar]
- 55.Morden NE, Colla CH, Sequist TD, Rosenthal MB. Choosing wisely—the politics and economics of labeling low-value services. N Engl J Med. 2014;370(7):589-592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rocque GB, Williams CP, Jackson BE, et al. . Choosing wisely: opportunities for improving value in cancer care delivery? J Oncol Pract. 2017;13(1):e11-e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Participant Characteristics
eTable 2. Health Care Accessibility Issues in the Previous 12 Months for Cancer Survivors and Control Respondents
eTable 3. Health Care Affordability Issues in the Previous 12 Months for Cancer Survivors and Control Respondents
eTable 4. Ability to Afford All Six Health Care Services in the Previous 12 Months for Cancer Survivors and Control Respondents
eTable 5. Questions Related to Health Care Access and Affordability from the National Health Interview Survey (NHIS)