Abstract
Objectives
To assess the effect of sex and spouse condition on symptoms of anxiety, depression and posttraumatic stress symptoms in patients and their spouses.
Methods
A prospective study conducted in a 22-bed adult mixed intensive care unit in a tertiary hospital in São Paulo, Brazil. Patients and their spouses were enrolled 2 days after intensive care unit admission. They were interviewed while in the intensive care unit using the Hospital Anxiety and Depression Scale. At 30 and 90 days after intensive care unit discharge, they completed the Impact of Event Scale and Hospital Anxiety and Depression Scale by phone.
Results
From March 2011 to March 2013, we analyzed 118 patients and their spouses. We observed that female sex was associated with higher scores than male sex was in terms of the anxiety Hospital Anxiety and Depression Scale - subscale (p = 0.032) and depression (p = 0.034). There was no association between sex and posttraumatic stress disorder symptoms. However, spouses had higher Impact of Event Scale points compared with patients (p = 0.001).
Conclusions
Female sex was associated with anxiety and depression, and spouses were more vulnerable to post-traumatic stress symptoms than the patients were. Increasing age and a later time of assessment were also associated with lower scores on the Impact of Event Scale.
Keywords: Anxiety; Depression; Spouses; Stress disorders, post-traumatic; Intensive care units; Female
INTRODUCTION
Admission to an intensive care unit (ICU) exposes the patient to serious stressors, such as distress related to the disease, being in pain, having tubes in the nose and/or mouth, loss of control, sleep deprivation, physical limitation, and not being able to communicate.(1-3) Furthermore, patients and family members commonly experience high rates of anxiety and depression symptoms as well as posttraumatic stress disorder (PTSD) both during and after ICU discharge.(4-8) Previous studies highlighted that family members of ICU-admitted patients, particularly their spouses, suffer relevant psychological distress, occasionally even more than their beloved ones; therefore, the family members need support both during the ICU stay and during the follow-up period.(8) Importantly, follow-up studies have suggested that patients and their family members may experience different levels of anxiety, depression and post-traumatic distress in various ICU recovery periods.(9,10)
Some factors may contribute to increased incidence of these symptoms, including female sex, spouses, young age, need for mechanical ventilation, and severity of disease.(6-10) Although the literature has identified some risk factors for anxiety, depression and PTSD in critically ill patients and their family members, few studies have assessed the effect of female gender on the development of these symptoms in a specific population, such as patients admitted to an intensive care unit and their spouses. Girard et al. observed that high levels of PTSD symptoms after critical illness requiring mechanical ventilation were most likely to occur in female patients. According to the authors, it is of the utmost importance to understand the risk factors that may facilitate preventive strategies and to direct screening for symptoms of PTSD after critical illness.(11)
The aim of this study was to assess the effect of sex and spouse conditions on the symptoms of anxiety, depression and posttraumatic stress symptoms in patients and their spouses during ICU stays and at 30 and 90 days following ICU discharge.
METHODS
This is a secondary analysis of a prospective study conducted in a tertiary private teaching hospital, Hospital Sírio-Libanês, in São Paulo, Brazil.(8) The institutional review board (IRB), called the "Comitê de Ética em Pesquisa da Sociedade Beneficente de Senhoras do Hospital Sírio Libanês", reviewed and approved this study (HSL - protocol number 2010/44). All patients with more than 48 hours of ICU stay and their spouses were invited to participate and sign written informed consent. The study was conducted in a medical-surgical unit that contains 22 private rooms. A family member can stay with the patient 24 hours per day in their private room (for one patient only) and rotate with another visitor at any time during the day or night. They are allowed to sleep in the patient's room (which contains a sofa bed or a comfortable armchair, bathroom and TV). In addition, the ICU has two visitation periods, in which up to two visitors are allowed in the patient's room at the same time. During invasive procedures (intubation, catheterization), family members are invited to remain outside the room.
The professional-to-bed ratios in the ICU are as follows: nurse 1:4; nurse-assistant 1:2; physician 1:6 (dayshift) and 1:10 (night shift). This ICU has a 24-hour visitation policy, and family members remain with the patient for an average of 12 hours per day.(8)
The inclusion criteria for patients were age over 18 years and more than 48 hours of ICU stay. The exclusion criteria for patients were psychiatric disorders, severe neurologic disease, illness too severe to answer at the first assessment or any difficulty with follow-up due to physical impairment or limitations (such as hearing, incapacity to speak, language barriers, or being too old to participate, e.g., if advanced age causes limitation in reading, understanding or speaking on the phone). We also invited their spouses (wife, husband or their partners) if they were involved with the patient's care (visiting the patient at least two days). The exclusion criteria for spouses included psychiatric disorders. For patients and spouses, psychiatric disorders included anxiety and depression under drug treatment at ICU admission. After 48 hours of ICU stay, both patient and their spouse were approached. If the patient was unable to participate at first assessment because of clinical conditions (e.g., mechanical ventilation, delirium), they were excluded. During the ICU stay, when patients were able to participate, they were assessed and interviewed. At 30 and 90 days, only those who participated in the ICU period were followed up.
Patients and their spouses were interviewed while in the ICU using the Hospital Anxiety and Depression Scale (HADS). At 30 and 90 days after ICU discharge, they were also interviewed by phone to complete the Impact of Event Scale (IES) and HADS. The HADS score for each subscale (anxiety and depression) ranges from 0 - 21, and a cut-off of > 10 was used to depict each condition. The scores for the entire scale (emotional distress) range from 0 - 42, with higher scores indicating more distress. The IES score has been used for many years and seems reliable across a broad range of traumatic events, and it can be easily applied during a telephone interview. The IES is not a tool for diagnosing PTSD, but it does detect symptoms indicating a risk of PTSD. It includes 15 items, seven of which measure intrusive symptoms (for example, intrusive thoughts, nightmares, intrusive feelings and imagery) and eight of which measure avoidance symptoms (numbing of responsiveness, avoidance of feelings, situations, and ideas). Respondents are asked to rate the items according to how often each has occurred in the past 7 days. The IES score ranges from 0 - 75 points, with higher scores indicating more severe post-traumatic stress symptoms. Patients were classified as having low or high IES scores, using 30 as the cutoff, in agreement with previous reports that higher than 30 points indicates post-traumatic stress reaction with a significant risk of PTSD. To ensure optimal quality of the data, all interviews were conducted by the same person, a psychologist with ICU interview experience. Both scales were previously validated in Brazil.(12,13)
For each patient, the following information was collected: age, sex, level of education, cause of ICU admission, cancer disease, Simplified Acute Physiology Score (SAPS) 3, Glasgow Coma Scale, Sequential Organ Failure Assessment (SOFA), ICU length of stay, need of mechanical ventilation, renal replacement therapy in the ICU, delirium (positive Confusion Assessment Method for the Intensive Care Unit - CAM-ICU), and final outcome in the ICU. The following information was supplied by the spouse: sex, age, level of education, religious belief, previous ICU experience and how much time per day is spent with the patient in the ICU.
Statistical analysis
We performed descriptive analysis of continuous variables using the mean and standard deviation or median and interquartile range and frequencies for categorical variables. To compare the HADS anxiety and depression scores at three assessments according to age, sex and patient or spousal condition, we performed generalized estimating equations with a first-order autoregressive correlation matrix between assessments, assuming a normal marginal distribution and identity link function. To compare IES scores at 30 and 90 days, we performed generalized estimating equations with a first-order autoregressive correlation matrix between assessments, assuming a Poisson marginal distribution and log link function. Generalized estimating equations are a powerful and modern methods for repeated measures, allowing the fit of continuous, categorical and count outcomes. Based on the literature, there was an expected natural trend to improvement over time in HADS and IES. To be correctly modelled, we used an autoregressive correlation matrix, assuming that the measures that were taken closer were more correlated than were those taken over far distances. Therefore, due to their flexibility and features, allowing correct model specification and taking account of all measures, we used generalized estimating equations instead of ANOVA.(14)
We tested interactions among sex, condition and time of assessment. Multiple comparisons were adjusted for multiplicity using Bonferroni's method. A p value of < 0.05 was considered significant.
RESULTS
From March 2011 to March 2013, 1125 patients were admitted to the ICU ≥ 48 hours. After the inclusion and exclusion criteria were applied (588 exclusion criteria and 154 refused to participate), we analyzed 118 patients and their spouses.
Ninety-six (81.4%) patients were male. The mean age was 58.8 ± 12.6 years for patients and 54.8 ± 12.6 for spouses. The spouses were, on average, 4.0 years younger than the patients (95% confidence interval - 95%CI: 2.7 to 5.4 years; p < 0.001). There was no significant difference in the proportion of patients and spouses aged over 60 years. Among spouses, we observed a significantly lower proportion with college education (p < 0.001) (Table 1).
Table 1.
Characteristics of patients and their spouses
| Variables | Values |
|---|---|
| Patients (n = 118) | |
| Age | 58.8 ± 12 (30 - 84) |
| Sex (male) | 96 (81.4) |
| College education | 102 (86.4) |
| Moderate-severe pain at ICU | 60 (50.8) |
| SOFA score | 1.5 [0 - 5] |
| SAPS 3 (points) | 46.5 [36 - 61] |
| Cancer | 67 (56.8) |
| Activity of daily lives - eigh dependence | 10 (8.5) |
| Vasopressors | 43 (36.4) |
| Mechanical ventilation > 24 hours | 28 (23.7) |
| Renal replacement therapy | 19 (16.1) |
| Clinical ICU admission | 66 (55.9) |
| ICU length of stay (days) | 5.63 ± 5.92 (2 - 47) |
| Spouses (n = 118) | |
| Age | 54.8 ± 12 (24 - 81) |
| Sex (male) | 22 (18.6) |
| College education | 84 (71.2) |
| Catholic religion | 86 (72.9) |
| No previous family experience with ICU | 28 (23.7) |
| Family staying time in ICU (hours/day) | 16.00 [12 - 24] |
| ICU satisfaction score (points) | 13 [12 - 14] |
ICU - intensive care unit; SOFA - Sequential Organ Failure Assessment; SAPS - Simplified Acute Physiology Score. The results are expressed as mean ± standard deviation, n (%) or median [IQR].
We observed that 60 (50.8%) patients had severe pain during the ICU stay, 67 (56.8%) had a cancer diagnosis and 66 (55.9%) were receiving clinical treatments (Table 1). During the ICU stay, we observed that ten (8.5%) patients were very dependent in terms of their activities of daily living, 28 (23.7%) needed mechanical ventilation, 43 (36.4%) used vasoactive drugs and 19 (16.1%) needed renal replacement therapy. The median SOFA score was 1.5, and the median SAPS 3 score was 46.5 points, with a range of 21 - 93 (Table 1).
After 30 days, we followed-up 88 (74.6%) patients and 103 (87.3%) spouses, and at 90 days, we followed-up 77 (65.2%) patients and 94 (79.7%) spouses. The reasons for missing data were deaths (11 at 30 days and 4 at 90 days); being in no condition to participate (seven patients at 30 and 90 days); two patients refusing to participate at 30 days; and lost to follow-up (10 at 30 days and nine at 90 days).
The scores of anxiety, depression and PTSD symptoms are displayed in table 2. We observed that both patients and their spouses had higher anxiety- and depression-HADS scores as well as total HADS scores at baseline during their ICU stay compared with the scores after 30 and 90 days. Twenty-two (18.6%; 95%CI: 12.1% to 26.9%) patients had symptoms of anxiety, and eight (6.8%; 95% CI: 3.0% to 12.9%) had symptoms of depression at baseline. After 30 and 90 days, no patients had symptoms of anxiety, and few patients had symptoms of depression (1.1% [95%CI: 0.3% to 6.2%] and 1.3% [95%CI: 0.3% to 7.0%], respectively).
Table 2.
Anxiety, depression and post-traumatic stress disorder symptoms among patients and their spouses
| HADS total Score* | HADS Subscale Anxiety score* | HADS Subscale Depression score* | IES score† | |
|---|---|---|---|---|
| Patients | ||||
| At ICU (n = 118) | 9.9 ± 7.2 | 6.7 ± 4.4 | 3.2 ± 3.6 | - |
| 30-day (n = 88) | 3.4 ± 4.6 | 1.8 ± 2.3 | 1.6 ± 2.6 | 0.0 [0.0 - 6.0] |
| 90-day (n = 77) | 1.9 ± 3.7 | 1.0 ± 1.8 | 0.9 ± 2.2 | 0.0 [0.0 - 0.0] |
| Spouses | ||||
| At ICU (n = 118) | 10.8 ± 7.2 | 7.7 ± 4.4 | 3.1 ± 3.7 | |
| 30-day (n = 103) | 7.1 ± 7.8 | 4.1 ± 4.2 | 3.1 ± 4.1 | 5.0 [0.0 - 10.0] |
| 90-day (n = 94) | 5.4 ± 7.6 | 3.1 ± 4.1 | 2.2 ± 3.8 | 0.0 [0.0 - 1.0] |
HADS - Hospital Anxiety and Depression Scale; IES - Impact of Event Scale; ICU - intensive care unit.
Mean ± standard deviation;
Median [CI].
Among the spouses, twenty-seven (22.9%; 95%CI: 15.6% to 31.5%) had symptoms of anxiety, and eight (6.8%; 95%CI: 3.0% to 12.9%) had symptoms of depression at baseline. After 30 days, 11 (10.7%; 95%CI: 5.4% to 18.3%) had symptoms of anxiety and six (5.8%; 95%CI: 2.2% to 12.2%) had symptoms of depression. These symptoms decreased after 90 days: seven (7.4%; 95%CI: 3.0% to 14.7%) had symptoms of anxiety, and five (5.3%; 95%CI: 1,7% to 12.0%) had symptoms of depression.
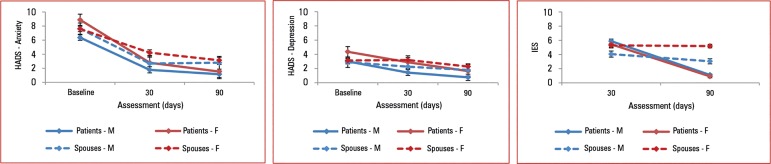
Overall, female sex was associated with higher scores, than were males in the anxiety HADS subscale, after adjusting for age, time of evaluation and whether they were patients or spouses (average +1.00 point [95%CI: 0.09 to 1.91]; p = 0.03). There was no significant difference between patients and spouses for anxiety (p = 0.098). We also observed that for each year older, both patients and spouses had an average reduction of 0.05 points (95%CI: -0.08 to -0.03; p < 0.001) on the HADS score for anxiety (Table 3). On average, these symptoms decreased over time, without an interaction of sex and condition. The score of anxiety was 4.23 (95%CI: -4.86 to -3.61; p < 0.001) and 5.05 (95%CI: -5.76 to -4.33; p < 0.001) points lower in the evaluation performed 30 and 90 days after ICU compared to baseline, respectively (Table 3). For depression, female sex was the only variable that was statistically associated with high scores (0.96 [95%CI: 0.07 to 1.85]; p = 0.034), whereas the level of depression decreased over time (Table 3). The outputs from the models for the HADS scores are depicted in figure 1.
Table 3.
Generalized estimating equations with first order autoregressive correlation matrix comparing Hospital Anxiety and Depression Scale anxiety and depression and Impact of Event Scale scores over time, according to patient or spouse condition, gender and age
| Parameters | Anxiety | Depression | PTSD |
|---|---|---|---|
| Coefficient ± SD [95%CI]; p value |
Coefficient ± SD [95%CI]; p value |
Coefficient ± SD [95%CI]; p value |
|
| Female versus male | 1.00 ± 0.46, [0.09 - 1.91]; 0.032 |
0.96 ± 0.45, [ 0.07 - 1.85]; 0.034 |
-0.08 ± 0.11, [ -0.29 - 0.13]; 0.472 |
| Spouse versus patient | 0.77 ± 0.46, [- 0.14 - 1.68]; 0.098 |
-0.04 ± 0.45, [-0.93 - 0.85]; 0.930 |
-0.37 ± 0.12, [-0.60 - -0.14]; 0.001 |
| Age (per unit increase) | - 0.05 ± 0.01, [-0.08 - -0.03]; < 0.001 |
-0.02 ± 0.01, [-0.05 - 0.00]; 0.079 |
-0.04 ± 0.00, [ -0.04 - -0.03]; < 0.001 |
| 30-days versus baseline | -4.23 ± 0.32, [-4.86 - -3.61]; < 0.001 |
-1.44 ± 0.32, [ -2.07 - -0.80]; 0.001 |
- |
| 90-days versus baseline* | -5.05 ± 0.37, [-5.76 - -4.33]; < 0.001 |
-0.67 ± 0.27, [ -1.20 - -0.14]; 0.013 |
-1.66 ± 0.19, [ -1.88 - -1.45]; < 0.001 |
PTSD - posttraumatic stress disorder; SD - standard deviation; 95%CI - 95% confidence interval.
For posttraumatic stress disorder, the reference was the assessment at 30 days.
Figure 1.
Hospital Anxiety and Depression Scale anxiety and depression subscales and Impact of Event Scale scores of posttraumatic stress disorder symptoms according to gender and spouse condition.
HADS - Hospital Anxiety and Depression Scale; IES - Impact of Event Scale.
There was no association between sex and PTSD symptoms. However, spouses had higher IES scores than patients did (Table 3). Additionally, we found an interaction among sex, condition and time of assessment (Figure 1). Increasing age and later time of assessment were also associated with lower IES scores (Table 3).
DISCUSSION
This study aimed to evaluate the association between sex and spouse conditions for symptoms of anxiety, depression and posttraumatic stress traumatic during ICU admission and at the 30- and 90-day follow-ups after ICU discharge. We observed that females had, on average, higher levels of anxiety and depression than males did, but there was no association with PTSD. By contrast, being a spouse or patient had no association with anxiety and depression, although spouses were associated with PTSD symptoms.
Several studies have demonstrated a high prevalence of anxiety and depression in critical ill patients and their family members. However, few data can address the sex differences regarding these conditions. Our results are in accordance with recent studies, where female sex was associated with symptoms of anxiety, depression and post-traumatic distress.(4-9,11) In addition, their closest relatives suffered more from symptoms of post-traumatic stress, occasionally more so than the patients did.(8,15) Research on the causes of psychological distress in females in midlife has focused on the current adversity and hormonal changes associated with menopause.(16) However, psychosocial and unmeasured factors should also have an impact. We thus emphasize the need for the proper monitoring of anxiety, depression and PTSD, with greater attention paid to females, who are facing a critical illness during an ICU stay.
Posttraumatic stress occurs when a person experienced, witnessed, or was confronted with an event involving death or threat. It involves fear, helplessness or even intense terror. The ICU environment is so threatening that the prevalence of these symptoms was compared to that felt by people who experienced a natural disaster or even rape.(9) We found that spouses were more vulnerable to post-traumatic stress symptoms than patients were. Interestingly, these symptoms in patients lessened significantly after three months, whereas they persisted over time in their spouses. However, although spouses spent many hours per day visiting the patients, we did not find an association between being a spouse and both anxiety and depression. Interestingly, the correlation of anxiety and depression symptoms between patients and family members in a positive direction was observed in a previous study by our group.(8) In addition, anxiety, depression and post-traumatic stress symptoms in patients lessened significantly after three months, whereas in family members, they may persist over time.(8)
Although psychological distresses have been given considerable attention in recent years, few studies have addressed the symptoms of anxiety, depression and post-traumatic distress by comparing patients and their spouses or exploring the effects of sex and spouse conditions, including the ICU stay and 30 and 90 days after ICU discharge.(17,18)
Our study has some strengths, such as the assessment of patients and their respective spouses at three time points (during the ICU stay and at 30 and 90 days after ICU discharge) and the evaluation of exact patient-spouse pairs. However, it has some limitations. First, it was a single-center study that was performed in an open-visit private ICU; therefore, it was not representative of Brazilian ICUs.(19) Second, we excluded several patients (mainly due to severity and barriers to completing the interview), although we could analyze a considerable number of pairs (patient/spouse). Third, we had a very low incidence of anxiety and depression symptoms compared with the literature. Part of this could be attributed to our open-visit policy, but we cannot rule out selection bias by excluding more severe patients.
CONCLUSIONS
In our study setting, we found that female sex had an important association with anxiety and depression, whereas spouses were associated with post-traumatic stress symptoms, which persisted over time. We recommend a proactive intervention during intensive care unit stays to reduce patient-spouse distresses.
Authors' contributions
Conception or design of the work: RR Fumis and HS Oliveira; Acquisition of data: RR Fumis; Statistical Analysis: RR Fumis; Interpretation of data: RR Fumis and HS Oliveira; Drafting the manuscript: RR Fumis and HS Oliveira; Final approval of the version to be published: RR Fumis and HS Oliveira.
ACKNOWLEDGEMENTS
We are deeply indebted to Andréia de Fátima Nascimento, for the contribution she made sharing her expertise with statistical methods to improve our manuscript.
Funding Statement
Este estudo foi realizado com suporte financeiro da Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), processo 11/05672-1, e do Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), processo 159573/2015-7.
Footnotes
Conflicts of interest: None.
This study is supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) - process 11/05672-1 and supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) - process 159573/2015-7.
Responsible editor: Márcio Soares
REFERENCES
- 1.Biancofiore G, Bindi ML, Romanelli AM, Urbani L, Mosca F, Filipponi F. Stress-inducing factors in ICUs: what liver transplant recipients experience and what caregivers perceive. Liver Transpl. 2005;11(8):967–972. doi: 10.1002/lt.20515. [DOI] [PubMed] [Google Scholar]
- 2.Novaes MA, Knobel E, Bork AM, Pavão OF, Nogueira-Martins LA, Ferraz MB. Stressors in ICU: perception of the patient, relatives and health care team. Intensive Care Med. 1999;25(12):1421–1426. doi: 10.1007/s001340051091. [DOI] [PubMed] [Google Scholar]
- 3.Skalski CA, DiGerolamo L, Gigliotti E. Stressors in five client populations: Neuman systems model-based literature review. J Adv Nurs. 2006;56(1):69–78. doi: 10.1111/j.1365-2648.2006.03981.x. [DOI] [PubMed] [Google Scholar]
- 4.Pochard F, Darmon M, Fassier T, Bollaert PE, Cheval C, Coloigner M, Merouani A, Moulront S, Pigne E, Pingat J, Zahar JR, Schlemmer B, Azoulay E, French FAMIREA study group Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. J Crit Care. 2005;20(1):90–96. doi: 10.1016/j.jcrc.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Myhren H, Ekeberg O, Tøien K, Karlsson S, Stokland O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Crit Care. 2010;14(1):R14–R14. doi: 10.1186/cc8870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fumis RR, Deheinzelin D. Family members of critically ill cancer patients: assessing the symptoms of anxiety and depression. Intensive Care Med. 2009;35(5):899–902. doi: 10.1007/s00134-009-1406-7. [DOI] [PubMed] [Google Scholar]
- 7.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, Fassier T, Galliot R, Garrouste-Orgeas M, Goulenok C, Goldgran-Toledano D, Hayon J, Jourdain M, Kaidomar M, Laplace C, Larché J, Liotier J, Papazian L, Poisson C, Reignier J, Saidi F, Schlemmer B, FAMIREA Study Group Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 8.Fumis RR, Ranzani OT, Martins PS, Schettino G. Emotional disorders in pairs of patients and their family members during and after ICU stay. PLoS One. 2015;10(1):e0115332. doi: 10.1371/journal.pone.0115332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson JC, Hart RP, Gordon SM, Hopkins RO, Girard TD, Ely EW. Post-traumatic stress disorder and post-traumatic stress symptoms following critical illness in medical intensive care unit patients: assessing the magnitude of the problem. Crit Care. 2007;11(1):R27–R27. doi: 10.1186/cc5707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paparrigopoulos T, Melissaki A, Tzavellas E, Karaiskos D, Ilias I, Kokras N. Increased co-morbidity of depression and post-traumatic stress disorder symptoms and common risk factors in intensive care unit survivors: a two-year follow-up study. Int J Psychiatry Clin Pract. 2014;18(1):25–31. doi: 10.3109/13651501.2013.855793. [DOI] [PubMed] [Google Scholar]
- 11.Girard TD, Shintani AK, Jackson JC, Gordon SM, Pun BT, Henderson MS, et al. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care. 2007;11(1):R28–R28. doi: 10.1186/cc5708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Botega NJ, Bio MR, Zomignani MA, Garcia Jr C, Pereira WA. Mood disorders among inpatients in ambulatory and validation of the anxiety and depression scale HAD. Rev Saude Publica. 1995;29(5):355–363. doi: 10.1590/s0034-89101995000500004. Portuguese. [DOI] [PubMed] [Google Scholar]
- 13.Oliveira e Silva AC, Nardi AE, Horowitz M. Brazilian version of the Impact of Event Scale (IES): translation and cross-cultural adaptation. Rev Psiquiatr Rio Grande Sul. 2010;32(3):86–93. [Google Scholar]
- 14.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 15.Dithole K, Thupayagale-Tshweneagae G, Mgutshini T. Posttraumatic stress disorder among spouses of patients discharged from the intensive care unit after six months. Issues Ment Health Nurs. 2013;34(1):30–35. doi: 10.3109/01612840.2012.715235. [DOI] [PubMed] [Google Scholar]
- 16.Kuh D, Hardy R, Rodgers B, Wadsworth ME. Lifetime risk factors for women's psychological distress in midlife. Soc Sci Med. 2002;55(11):1957–1973. doi: 10.1016/s0277-9536(01)00324-0. [DOI] [PubMed] [Google Scholar]
- 17.Rosendahl J, Brunkhorst FM, Jaenichen D, Strauss B. Physical and mental health in patients and spouses after intensive care of severe sepsis: a dyadic perspective on long-term sequelae testing the Actor-Partner Interdependence Model. Crit Care Med. 2013;41(1):69–75. doi: 10.1097/CCM.0b013e31826766b0. [DOI] [PubMed] [Google Scholar]
- 18.Young E, Eddleston J, Ingleby S, Streets J, McJanet L, Wang M, et al. Returning home after intensive care: a comparison of symptoms of anxiety and depression in ICU and elective cardiac surgery patients and their relatives. Intensive Care Med. 2005;31(1):86–91. doi: 10.1007/s00134-004-2495-y. [DOI] [PubMed] [Google Scholar]
- 19.Ramos FJ, Fumis RR, de Azevedo LC, Schettino G. Intensive care unit visitation policies in Brazil: a multicenter survey. Rev Bras Ter Intensiva. 2014;26(4):339–346. doi: 10.5935/0103-507X.20140052. [DOI] [PMC free article] [PubMed] [Google Scholar]