Abstract
Instrumentation of the airways in critical patients (endotracheal tube or tracheostomy cannula) prevents them from performing their function of humidify and heating the inhaled gas. In addition, the administration of cold and dry medical gases and the high flows that patients experience during invasive and non-invasive mechanical ventilation generate an even worse condition. For this reason, a device for gas conditioning is needed, even in short-term treatments, to avoid potential damage to the structure and function of the respiratory epithelium. In the field of intensive therapy, the use of heat and moisture exchangers is common for this purpose, as is the use of active humidification systems. Acquiring knowledge about technical specifications and the advantages and disadvantages of each device is needed for proper use since the conditioning of inspired gases is a key intervention in patients with artificial airway and has become routine care. Incorrect selection or inappropriate configuration of a device can have a negative impact on clinical outcomes. The members of the Capítulo de Kinesiología Intensivista of the Sociedad Argentina de Terapia Intensiva conducted a narrative review aiming to show the available evidence regarding conditioning of inhaled gas in patients with artificial airways, going into detail on concepts related to the working principles of each one.
Keywords: Humidification systems, Mechanical ventilation, Airway management
INTRODUCTION
The conditioning of medical gases administered to patients has become a routine healthcare procedure. Under normal conditions, the upper airway and respiratory tract are responsible for humidify and heating inspired air, a process defined as conditioning of inhaled gas.(1,2) This process is critical for optimally conditioning the gas and avoiding potential damage to the structure and function of the respiratory epithelium.(3-6)
Instrumentation of the airways (endotracheal tube or tracheostomy cannula) prevents the conditioning of inspired gas. In addition, the administration of cold and dry medical gases and the high flows that patients experience with invasive (iMV) or non-invasive mechanical ventilation (NIV) lead to an even worse condition.(7) For this reason, the use of an external device for conditioning the delivered gases is required, even in short-term treatments.
METHODS
A literature search was performed by the Capítulo de Kinesiología Intensivista of the Sociedad Argentina de Terapia Intensiva (SATI) to develop the present narrative review. The search was performed using the following databases: LILACS, MEDLINE, Cochrane library and SciELO, and the following terms and combinations of words: "randomized controlled trial" OR "controlled clinical trial" OR "trial" OR "groups" AND "humidifiers" AND "heat and moisture exchangers" OR "heat and moisture exchangers filters" AND "heated humidifiers" OR "heated humidified" AND "mechanical ventilation" AND "noninvasive ventilation" AND "spontaneous breathing". The most relevant articles were chosen according to the authors' criteria.
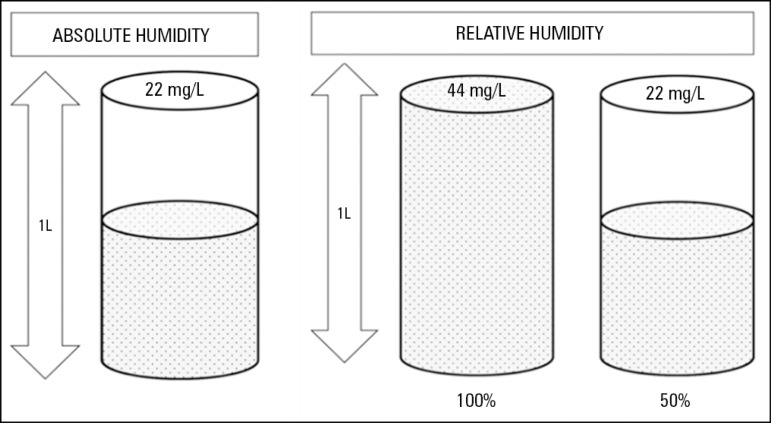
Concept of humidity
Humidity is the amount of water vapor contained in a gas and is, in general, characterized in terms of absolute or relative humidity.(8-10) The temperature of the gas is very important because its water vapor content depends on gas temperature. Relative humidity is the percentage (%) of water vapor contained in a gas relative to its maximum carrying capacity. Absolute humidity is the total amount of water vapor contained in a gas, expressed in milligrams of water suspended in liters of gas (mg/L). Absolute humidity is directly related to the gas temperature and is important in terms of humidification since at low temperatures, the relative humidity can be 100%, while the absolute humidity can be far below the recommended value(8,9) (Figure 1 and Table 1).
Figure 1.
Graphical description of absolute and relative humidity.
Table 1.
Relationships between the gas temperature, absolute humidity and water vapor pressure
| Gas temperature (ºC) |
Absolute humidity (mg/L) |
Water vapor pressure (mmHg) |
|---|---|---|
| 0 | 4.85 | 4.6 |
| 5 | 6.8 | 6.5 |
| 10 | 9.4 | 9.2 |
| 15 | 12.8 | 12.8 |
| 20 | 17.3 | 17.5 |
| 25 | 23.0 | 23.7 |
| 30 | 30.4 | 31.7 |
| 32 | 33.8 | 35.5 |
| 34 | 37.6 | 39.8 |
| 36 | 41.7 | 44.4 |
| 37 | 43.9 | 46.9* |
| 38 | 46.2 | 49.5 |
| 40 | 51.1 | 55.1 |
| 42 | 56.5 | 61.3 |
| 44 | 62.5 | 68.1 |
Ideal condition for gas conditioning, limit of isothermal saturation.
Physiology of the upper airway. Role in gas conditioning
The conditioning of inspired air is the process by which a gas is warmed and moisturized during its passage through the airways to reach the alveolar level under optimal conditions.(5)
Although the gas acquires temperature and humidity during its passage through the airway, the main area where the heating of inspired air occurs is the nose.(5,11-13) The temperature of nasal mucosa is approximately 32ºC, and although the contact time between inspired air and nasal mucosa is short, this time is sufficient to transfer heat. In addition, the nose has a great potential to regulate blood perfusion and thus counterbalance the loss of heat during inspiration. Moreover, the air circulates through a narrow conduit generating turbulent flow that allows optimizations in heating, humidification and filtering.(12,13) During expiration, the humidity of exhaled air is partially preserved by condensation on the mucosa due to differences in temperature. Approximately 25% of the heat and humidity is recovered during exhalation.(11)
Since the temperature of the inspired air increases during its passage through the airway, at the level of the alveolar-capillary interface, it is at body temperature (37ºC), with 100% relative humidity and 44mg/L absolute humidity. The point where the gas acquires these conditions is known as the isothermal saturation limit; this limit is usually close to the 4th or 5th bronchial generation. It is critical to reach the isothermal saturation limit to avoid damage to the mucosa and the ciliary epithelium.(7)
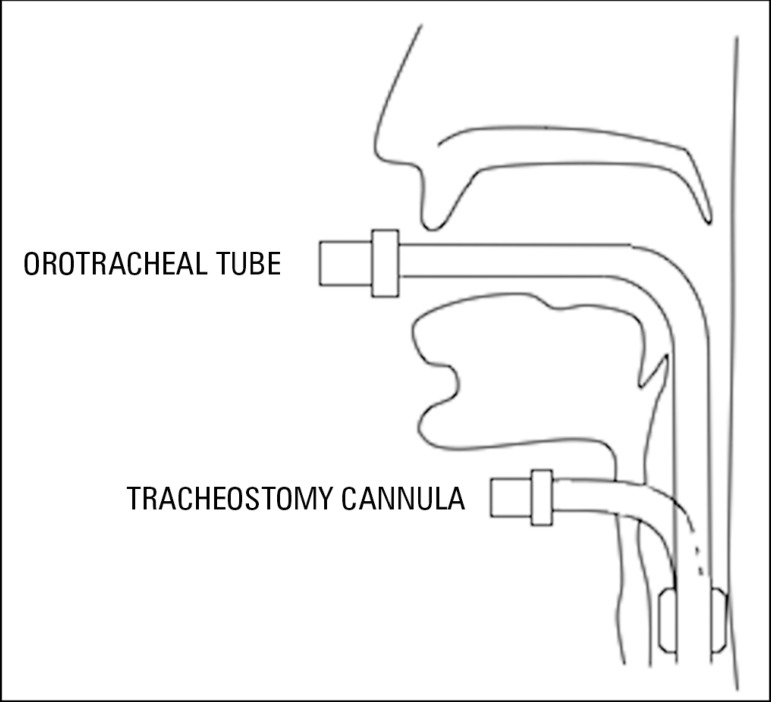
The presence of an artificial airway prevents inspired air from contacting the mucosa of the upper airway affecting gas conditioning (Figure 2). Moreover, if medical gases are administered, there is a risk of generating alterations in clearance and mucosa(5,8) because these medical gases are cold and dry.(14)
Figure 2.
Bypass of the airway based on the type of artificial airway.
Two types of devices for conditioning inspired gases in the presence or absence of an artificial airway are available: heat and moisture exchangers (HME) and active humidifiers.(15)
Regardless of which device is chosen, it should infallibly meet the minimum requirements to replace the function of the upper airway, which, according the American Association for Respiratory Care, are:(9)
- 30mg/L absolute humidity, 34ºC and 100% relative humidity for HME.
- Between 33 and 44mg/L absolute humidity; between 34ºC and 41ºC; 100% relative humidity for active humidifiers.
PASSIVE HUMIDIFIERS
Classification
The working principle for these devices is based on their capacity to retain heat and humidity during expiration and to deliver at least 70% of them to the inhaled gas during subsequent inspiration. This "passive" function can be achieved by different mechanisms, and the classification of these devices is based on their mechanisms.(16-22)
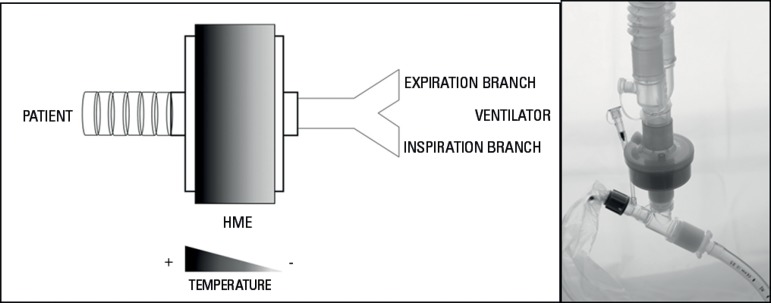
a. Heat and moisture exchangers
Heat and moisture exchangers are simple condensers constructed with elements made of disposable foam, synthetic fiber or paper, with a significant surface area that can generate an effective temperature gradient through the device delivering heat on each inspiration. From the field of filtration, hydrophobic HMEs were made to repel the humidity and to retain the heat of the expired gas, delivering it in the next inspiration (Figure 3).(8,16,23,24)
Figure 3.
Schematic description of the working principle of a heat and moisture exchanger and placement in the ventilator circuit.
b. Hygroscopic condenser humidifiers (HCHs) or hygroscopic heat and moisture exchangers (HHMEs)
In contrast with HMEs, HCHs or HHMEs are devices made with synthetic fiber coated by a hygroscopic chemical product (calcium chloride or lithium chloride), which absorbs expired water vapor and delivers it to the inspired gas, optimizing the delivery of humidity. The synthetic fiber also helps to decrease the accumulation of condensation in a device-dependent position.(8,17,18)
c. Heat and moisture exchangers with filter
These devices are made with materials needed for moisturizing and heating based on their working principle (hydrophobic or hygroscopic); in addition, they contain an electrostatic filter. Filters are flat layers of fiber material (modacrylic or propylene) that act as a barrier to the gas flow; at the same time, the filtration performance is optimized by applying material with electrostatic charge.(25)
The available types of filters are: heat and moisture exchanger filters (HMEFs), hygroscopic condenser humidifier filters (HCHFs) or hygroscopic heat and moisture exchanger filters (HHMEFs).(18)
d. Combined heat and moisture exchangers
Hygroscopic and hydrophobic elements are used combined to create a combined HME. The performance in terms of absolute humidity is better in HCHs than in HMEs. However, the performances are similar between HCHs and combined HMEs.(24,26)
PASSIVE HUMIDIFIERS - SPECIAL CONSIDERATIONS
Dead space
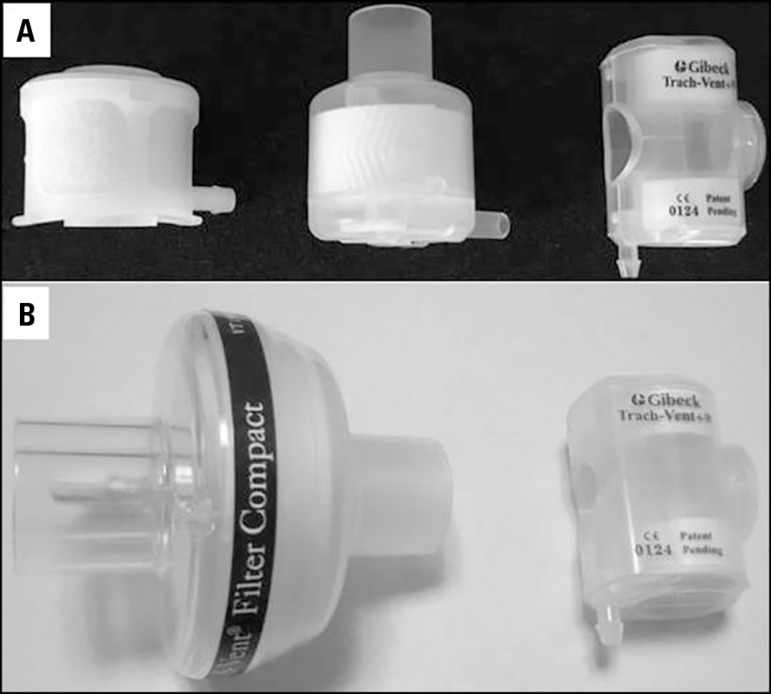
The working principle of passive humidifiers implies that a higher volume of condenser material will yield better device performance (Figure 4). For this reason, the 'ideal' dead space for a humidifier is approximately 50mL.(18)
Figure 4.
A) Heat and moisture exchangers for patients with artificial airways in spontaneous ventilation (particularly in tracheotomized patients). B) Graphic comparison between volumes of a conventional heat and moisture exchanger for use in patients with artificial airway in mechanical ventilation and one for use in tracheotomized patients with spontaneous ventilation.
This dead space does not represent a disadvantage for patients with iMV because the dead space can be compensated for in the programming of the ventilator. However, in patients with artificial airways, without the requirement of iMV, the increase in the ventilatory minute volume as a compensatory mechanism for the dead space could generate a hard-to-tolerate load in patients with low ventilatory reserve. Therefore, passive humidifiers with 'small volume' were developed (Figure 4). Although they can be more 'tolerable', they have low humidification capacity that worsens when the tidal volume (VT) increases and with supplementary O2.(27-30)
The instrumental dead space added by the passives humidifiers during iMV becomes relevant when the pathology requires strategies for lung protection (low VT). Studies conducted by Prat(31) and Hinkson(32) account for this, demonstrating significant changes in arterial carbon dioxide partial pressure (PaCO2) (and in pH) under these circumstances.
Resistance
Although the resistance of an unused device could be considered negligible (5cmH2O/L/sec assessed as 'dry": International Standards Organization Draft International Standard 9360-2),(33) resistance can vary under changes in the conditions (presence of condensation, impaction due to secretions, changes in ventilatory parameters, increases in the VT and the flow). Although some studies(18,34,35) have shown that the presence of 'humidity' in a device does not lead to significant changes in resistance, excessive condensation or impaction (due to secretions or blood) can alter it.
PASSIVE HUMIDIFIERS
Implementation and monitoring
Due to the working principle of a passive humidifier, it should always be placed before the 'Y' part of the circuit, allowing the device to contact the inspired and expired air during each ventilation cycle (Figure 3), which makes the passive humidifier part of the instrumental dead space.(19)
Volume of the heat and moisture exchanger and its relation to the humidification capacity
Several factors affect the delivery of humidity to the patient: internal volume and absolute humidity provided are 2 significant variables to consider.
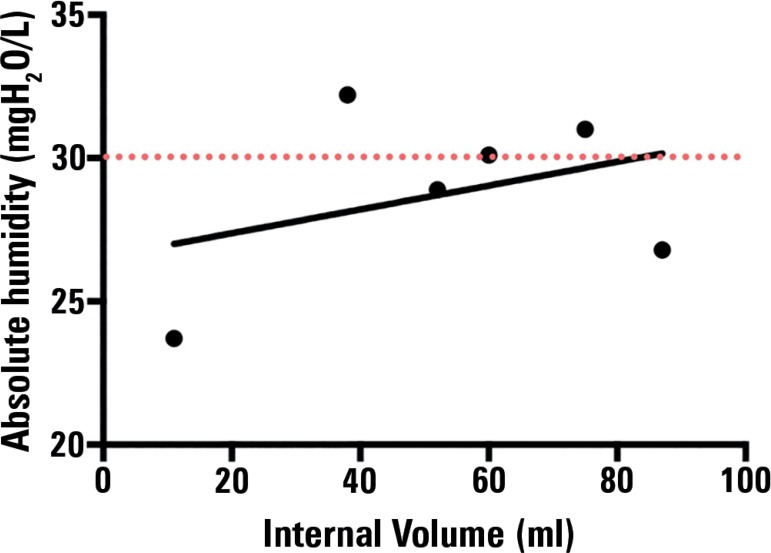
In a bench study, Eckerbom et al.(16) related the dead space of HME with the absolute humidity delivered, reporting a poor correlation between both variables. However, only 6 devices were assessed; some of them were bacterial filters, so the results should be considered with caution. To analyze the results provided by this study in more detail, we drafted a scatter plot (Figure 5) with the abovementioned variables. This plot shows a poor correlation between these variables (r = 0.36; p = 0.47).
Figure 5.
Correlation between internal volume and humidity delivered in Eckerbom's study. The programming of the ventilator corresponds to "Setting II" of the study (tidal volume of 500 -mL, respiratory frequency of 20 breaths per minute). Pearson's correlation coefficient was used for the statistical analysis.
Source: Based on data from the study: Eckerbom B, Lindholm CE. Performance evaluation of six heat and moisture exchangers according to the Draft International Standard (ISO/DIS 9360). Acta Anaesthesiol Scand. 1990;34(5):404-9.(16)
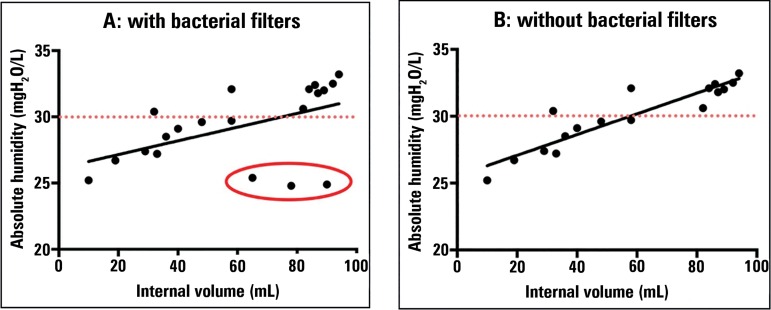
Branson et al.(18) tried to replicate the abovementioned study, with the same ISO standards but with more devices. Branson et al.(18) showed that as the dead space increases, the delivered absolute humidity also increases. To further explore these results, we drafted correlation graphs using data provided by Branson et al.(18) (Figure 6). Figure 6A shows poor correlation (r = 0.5; p = 0.01) between the 2 variables. However, when analyzing the devices used in detail, we found that 3 bacterial filters were included (marked with a red circle). When the analysis was repeated but excluding the results related to these 3 devices, we found an excellent correlation (Figure 6B; r = 0.91; p < 0.0001).
Figure 6.
Correlation between the internal volume of the heat and moisture exchanger and the absolute humidity delivered. The programming of the ventilator corresponds to "Setting I" (tidal volume of 500mL, respiratory frequency of 20 breaths per minute). In "B", the same analysis as in "A" was conducted, but excluding the 3 bacterial filters (Pall, Intertech HEPA, Intersurgical). Pearson's correlation coefficient was used for the statistical analysis.
Source: Based on data from the study: Branson R, Davis K Jr. Evaluation of 21 passive humidifiers according to the ISO 9360 standard: moisture output, dead space, and flow resistance. Respir Care. 1996;41:736-43.(18)
The ratio between the delivered absolute humidity and the dead space in mL is an efficacy measure described in the literature.(18) Devices with a higher ratio are considered more effective, that is, they provide better delivery of absolute humidity per unit of internal volume. Humidifiers reaching the recommended limit of 30 mg/L9 had a dead space of approximately 60mL (Figure 6A and 6B).
Therefore, we can assume that the device volume influences its performance and that the volume should be taken into account when selecting an HME.
Minute volume and performance of heat and moisture exchangers
The humidification performance of an HME decreases when minute volume increases.(8,16,18-21) Some studies found that the absolute humidity delivered decreased as the VT increased,(8,16) whereas only Unal et al.(21) found that the flow was a variable influencing the performance. The inconsistencies found between studies could be due to the use of different laboratory models (hygrometric or gravimetric methods). However, in 2014, Lellouche et al.(36) investigated the impact of minute ventilation (10 versus 20L/minute) and the room temperature on the new generation of HMEs, reporting no significant effects on the performance of these devices [absolute humidity delivered with a minute volume > 10L/minute was 30.9mg/L]. For this reason, these authors recommend not taking into account the minute ventilation as a limitation of the new generation of humidifiers. Since the minute volume is composed of the respiratory frequency and the VT, it might be worth investigating this issue thoroughly. The increase of the VT in the study was a modest 150mL (500 to 650mL, which means 30%), whereas the increase in respiratory frequency was greater, from 20 to 30 resp/minute (50%). The question becomes one of which of these 2 components of the minute volume [VT or respiratory frequency] has a greater effect on a humidifier performance.
Two studies compared(16,18) the performance in terms of humidification of the HMEs using methods and test conditions based on the ISO 9360:1992 standard. In both studies, a more significant effect on performance was observed when changing the VT from 500mL to 1000mL (increase of 100%) compared with changing the respiratory frequency from 10 to 20 resp/minute (increase of 100%), which suggests that VT has a primary effect.(16,18) Nevertheless, due to the unusual use of a VT of 1000 mL, the results should be considered with caution.
Time of contact with the air
Eckerbom et al.(16) assessed the time of contact of the inspired gas, and the authors did not find significant differences in delivered absolute humidity when comparing 1 second versus 2 seconds. Branson et al.(18) suggested that the expiratory flow could be a variable to consider since as the expiratory flow increases, the time of contact between the gas and the HME decreases along with the absolute humidity delivered.
PASSIVE HUMIDIFIERS - CHANGE
Although manufacturers provide general specifications for the changing of these devices, we could consider an 'ideal' recommendation that the change is performed:
ACTIVE HUMIDIFIERS (HEATED HUMIDIFIERS)
Active humidifiers are devices composed of an electric heater on which is placed a plastic casing with a metallic base in which sterile water is stored. When the base is warmed, the water temperature increases by convection. Some active humidifiers are self-regulated by a mechanism consisting of a heating wire (heated-wire breathing circuit) that keeps the gas temperature constant during its passage through the circuit and a wire with two temperature sensors connected to the exit of the heater (distal) and to a part of the circuit (close to the patient) to control the system temperature.
It should be taken into account that while heated-wire breathing circuit keep the temperature stable throughout its route and decrease the condensation, the lack of control exposes the patient to risks such as a higher incidence of occlusion of the artificial airway.(40)
TYPES OF ACTIVE HUMIDIFIERS
Bubble humidifiers
The flow of entering air is forced to pass through a tube that leads it to the lower part of the casing. The gas exiting from the distal end of the tube (under the water surface) form bubbles that gain humidity and temperature as they rise to the water surface. The amount of water in the container and the flow rate are factors affecting the humidity content of the gas. Simply expressed, if the water column in the container is taller, the gas-water interface will increase. Inversely, as the circulating flow increases, the device performance drops. These types of devices are no longer used.(41)
Pass-over humidifiers
The air flow passes over the water surface, which is hot, and the circulating gas gains heat and humidity from the gas-water interface formed.(41) In comparison with the previously described device, pass-over humidifiers have lower resistance. It is important to consider that the water temperature in the enclosure will be a determining factor for humidity.(42,43)
A variant of the pass-over humidifier is the 'wick' humidifier, in which a porous membrane that absorbs humidity (such as blotting paper) is dipped into water surrounded by the heating element, keeping the membrane constantly saturated with water vapor. The dry gas enters the chamber, makes contact with the wick and is loaded with more water vapor than in the basic system because the gas-liquid interface is larger.
Another variant is the hydrophobic membrane humidifier, where dry gas passes through the membrane, and, due to the membrane properties, only water vapor passes through. The dry gas is loaded with water vapor and exits the chamber.
ACTIVE HUMIDIFIERS - IMPLEMENTATION AND MONITORING
Assembly
Active humidifiers are placed in-line in the inspiration branch of the respirator. The circuit exiting the inspiration valve is connected with the entry hole of the plastic casing, which should be always filled to the level indicated by the manufacturer. Subsequently, a second section of the circuit (of standard length) is connected with the exit hole of the casing and to the "Y" of the circuit responsible for delivering gases to the patient.
With this type of humidification device, it is necessary to use water traps, reservoirs with unidirectional circulation systems that allow the deposition of surplus condensation without leaking air. Among other problems, the excessive accumulation of water in the circuit can lead to auto-triggering, misreading of the ventilator monitoring or even draining of contaminated material into the patient's airway.
Precautions and monitoring
- Observe that the tubing drains the water downwards and not toward the artificial airway or the ventilator.
- Place the water traps correctly to receive drained water.
- Frequently monitor the active humidifier device (water level, temperature level, check the presence of condensation).
- Never fill above the recommended level.
- Do not drain the condensation toward the humidifier chamber.
- Comply with the manufacturer's specifications.
SPECIAL HUMIDIFIERS
Humidifiers for aerosol therapy
The HME for aerosol therapy Gibeck Humid-Flo® is an HME that has the property of remaining in-line during the application of aerosols in mechanical ventilation, avoiding the opening of the circuit and potentially reducing the contamination of tubing and the exposure of healthcare staff to contaminated gases.
This type of humidifier has 2 modes: "HME and AEROSOL", which can be selected by rotating the central axis of the device. By choosing HME, the device acts as a conventional passive humidifier. In AEROSOL mode, the humidifier part is skipped; therefore, the aerosol goes directly to the patient without coming into contact with the humidifier material. However, the absolute humidity delivered with this device is at least questionable since it delivers 30.4mg/L, but with a VT of 1000mL.
Recently, in a bench study, Ari et al.(44) assessed the performance of several HMEs to be used in combination with aerosol therapy. Those authors did not find significant differences in drug (albuterol) deposition in the artificial lung without HME (control) versus with HME, using a moisturized circuit (simulating the actual gas exhalation of a patient). Although the study was only laboratory-based, the HME modified for aerosol therapy seemed to not interfere with drug deposition.
Heat and moisture exchanger-Booster
The HME-Booster® is a type of hybrid active humidifier consisting of a passive humidification system and a 'T' connector containing a self-regulated heater and a small-volume chamber for continuous infusion of distilled water (consuming approximately 250mL every 3 days). The upper part of the device has a hydrophobic membrane that only allows the passage of water when it has evaporated toward the tubing. Therefore, the humidity from the water evaporated on the membrane is aggregated during inspiration, improving the gas conditions by approximately 3 - 4mg/L (depending on the VT, I:E ratio and the type of HME used).(45) During the expiratory phase, heat and humidity are retained by the passive properties of the humidification system. The dead space of the device is approximately 9mL.
Advantages: easy to use, eliminates excessive condensation in the tubing, could be useful for hypothermic patients and has a bacterial filter (active humidifiers do not have a bacterial filter).
Disadvantages: it does not include temperature monitoring, increases resistance and requires a source of electrical energy (potential risk of burns and/or electric shocks).(46)
Active hygroscopic heat and moisture exchangers
This device consists of an HHME in a heated casing in the shape of a cone with a radiator and an electronic controller. There is a line between the device and the water source, another line between the radiator and the controller and a third heating line between the device and the controller. The casing contains a paper element that provides a surface for humidity transfer to the gas. A water source drips continuously on the paper element, and the casing heat makes the liquid evaporate, increasing the humidity of the inhaled gas. The device is electronically controlled through a water and temperature control unit used to program the volume per minute of the patient.(47)
Some of the proposed advantages are eliminating condensation from the inspiration branch and avoiding the use of water traps. In addition, if the water source is depleted, this device continues working like an HHME (providing approximately 28 - 31mg/L absolute humidity). The active HHME provides temperatures of 36 - 38ºC and 90 - 95% relative humidity. The absolute humidity provided by the device is similar to the HME or active humidifiers but with lower water use and less condensation. The dead space of the device is 73mL, and the resistance is 1.7cmH2O/L/s.(47)
The disadvantages of this product are the possibility of skin burns and greater dead space compared with a heated humidifier or only an HHME.
PASSIVE AND ACTIVE HUMIDIFIERS
Advantages and disadvantages
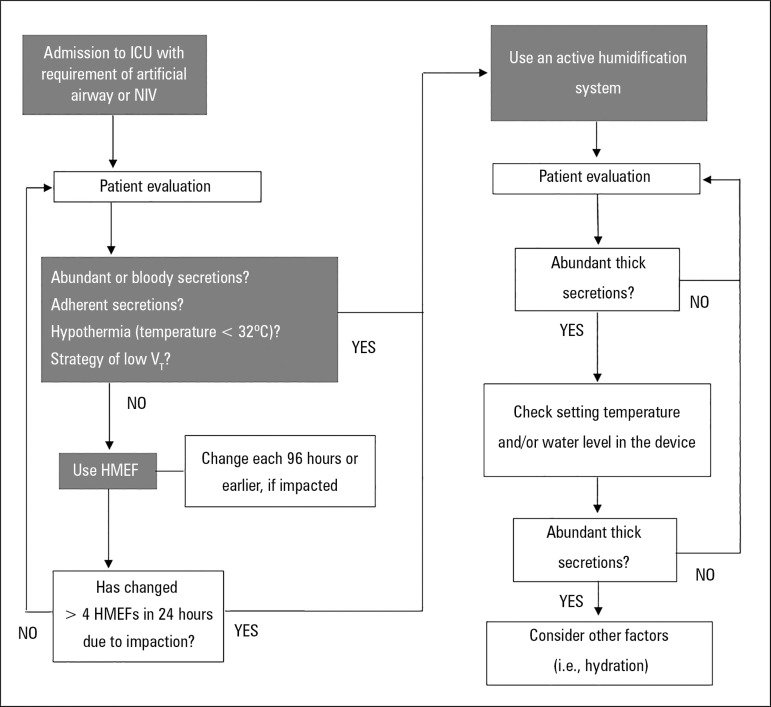
Taking into account the humidification capacity and the advantages and disadvantages, both passive and active humidifiers are suitable for the conditioning of inhaled gas (Table 2).(48,49) Although there are some data that favor the use of HMEF (or HCHF) over active humidifiers for the prevention of pneumonia associated with mechanical ventilation, the choice of the device should not be based only on infection control.(9) An algorithm for the selection of the humidification device is proposed in figure 7.
Table 2.
Advantages and disadvantages of active and passive humidification systems
| Advantages | Disadvantages | |
| Active humidifiers | They do not have contraindications. As they are placed in the inspiratory branch, they do not add instrumental dead space. If used correctly, they do not increase the resistance. They have alarm systems. They are more efficient and can deliver accurate temperatures. |
Possibility of electrocution of the patient and the
operator. They expose the airway lesion to excessive temperature. The presence of water in the circuit can limit the airflow. Condensation generates changes in the airway pressure and can lead to asynchronies. Colonization of the circuit. They require more monitoring to ensure correct performance. |
| Advantages | Disadvantages | |
| Passive humidifiers | Their use is simple. They do not have risks related to the treatment equipment. They are light in weight. They are cheaper. They are easily available in the intensive care unit. |
They are contraindicated in some pathologies or
clinical conditions. Because they are placed before the 'Y' in the circuit, they increase the instrumental dead space. They increase the resistance (negligible in most cases). They have lower performance or efficiency compared with an active humidifier. They should be retired to be able to apply aerosol therapy (except Gibeck Humid-Flo HME®). |
Figure 7.
Algorithm for the selection of the humidification device.
ICU - intensive care unit; AA - artificial airway; NIV - non-invasive mechanical ventilation; VT - tidal volume; HMEF - heat and moisture exchanger with filter.
Source: Adapted from: Branson RD. Humidification for patients with artificial airways. Respir Care. 1999;44(6):630-41.(50)
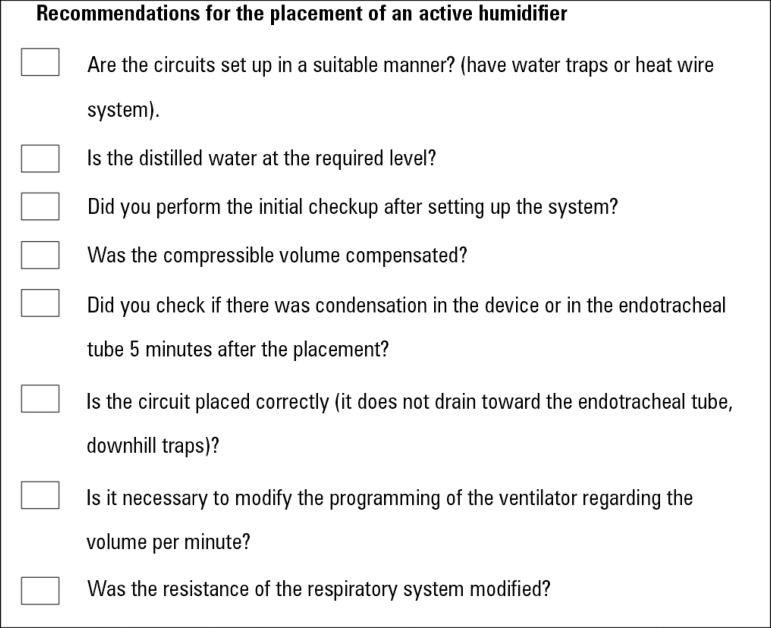
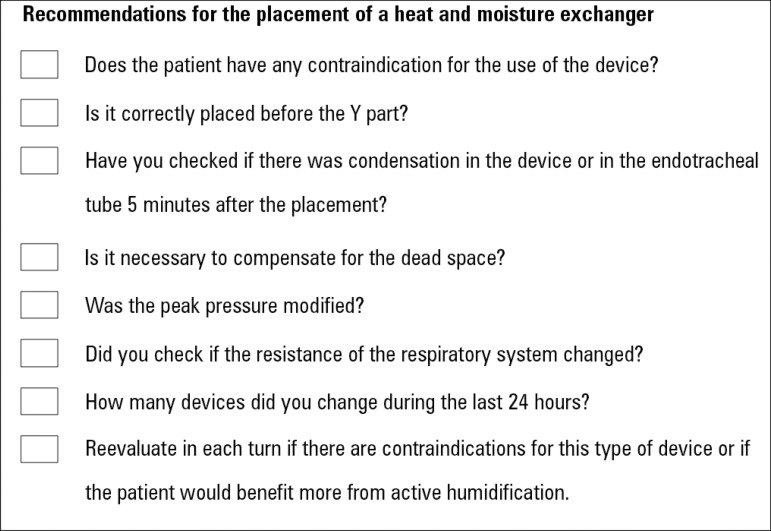
To simplify the checks that should be performed when choosing a humidification system, we have provided this short list containing the main points to be considered (Figures 8 and 9).
Figure 8.
Recommendations to take into account for placement of an active humidifier.
Figure 9.
Recommendations to take into account for the placement of a heat and moisture exchanger.
When deciding which humidification system should be used, one should take into account the different clinical scenarios since each device features particular properties that can affect the clinical situation of the patient (Table 3).(9,27-29,31,32,42,43,51-61) Given below are some clinical situations that should be considered:
Table 3.
Humidification systems: clinical considerations
| VAP | It is recommended not to select a humidification device based on its relationship with infection control |
| ARDS | The use of an active humidifier is suggested since it maintains its performance despite the ventilatory strategy used. It allows the optimization of the effective alveolar ventilation and decreases the VT and the instrumental dead space. |
| COPD | The use of an active humidifier is suggested since it does not increase the instrumental dead space or the ventilatory demand, without the risk of generating auto-PEEP. If using HME, change every 48 hours |
| Burned | The use of an active humidifier is suggested in patients with large body surfaces affected and inhalatory lesions due to its stable performance |
| Hypothermia | The use of an active humidifier is suggested in patients under a hypothermia strategy since they have demonstrated a better performance than HMEs and active HMEs |
| BPF | The use of an active humidifier is suggested in cases with an exhaled volume below 70% of the inhaled volume |
| NIV | Patients requiring ventilatory support for more than 1 hour are candidates for the use of a humidification device. The recommended device is an active humidifier with continuous flow ventilators with a one-branch circuit. In microprocessed ventilators with two-branch circuits, this recommendation is questionable. |
| Disconnection from MV | In patients with a problem in PaCO2 due their pathology or who present significant muscle weakness, the use of an active humidifier is recommended |
| Spontaneous ventilation | The use of a humidifier bottles as a conditioning system for the inhaled gases of a patient with artificial airways is discouraged |
VAP - ventilator-associated pneumonia; ARDS - acute respiratory distress syndrome; VT - tidal volume; COPD - chronic obstructive pulmonary disease; PEEP - positive end expiratory pressure; HME - heat and moisture exchanger; BPF - bronchopleural fistula; NIV - non-invasive mechanical ventilation; MV - mechanical ventilation; PaCO2 - carbon dioxide partial pressure.
- Acute Respiratory Distress Syndrome: The ventilatory strategy of lung protection uses low VT (4 to 6mL/kg predicted body weight), which implies the risk of generating hypercapnia due to hypoventilation. It becomes rational to decrease the instrumental dead space as much as possible to counteract this adverse effect. An easy strategy to implement is the use of active humidifiers in these situations.(31,32,53,54)
- Ventilator associated-pneumonia (VAP): Decreasing the VAP rate is achieved by the adoption of a series of measures; humidification systems are not part of these measures (CDC 2014). For this reason, it is recommended to not choose the humidification device based on infection control.(51,52)
- NIV: The high flows achieved by the devices and leaks predispose them to heat and moisture loss during the respiratory cycle. Humidification increases the chances of success in the application of NIV since it is related to the capacity of managing respiratory secretions and increases the feeling of comfort. The device of choice for gas conditioning in NIV would be the active humidifier, with continuous flow ventilators and a one-branch circuit. In microprocessor-controlled ventilators with a two-branch circuit, this recommendation could be debated.(60,61)
- Spontaneous ventilation and artificial airways: In patients with tracheostomy (without iMV), it is advised to use the corresponding HME (considering their limitations) as the first-line treatment. In case it is contraindicated, then active humidification systems with a water temperature in the casing not below 53ºC should be used.(42,43)
CONCLUSIONS
Knowledge of the technical specifications and the advantages and disadvantages of each of the humidification devices is essential for professionals who provide care to patients in the intensive care unit. The conditioning of inspired gases is a key intervention in patients with artificial airways and has become a routine care strategy. The incorrect selection of the device or an inappropriate configuration can negatively affect the clinical outcome by damaging the airway mucosa, increasing respiratory effort or prolonging invasive mechanical ventilation.
Footnotes
Conflicts of interest: None.
Responsible editor: Gilberto Friedman
REFERENCES
- 1.Lindemann J, Leiacker R, Rettinger G, Keck T. Nasal mucosal temperature during respiration. Clin Otolaryngol Allied Sci. 2002;27(3):135–139. doi: 10.1046/j.1365-2273.2002.00544.x. [DOI] [PubMed] [Google Scholar]
- 2.Keck T, Leiacker R, Riechelmann H, Rettinger G. Temperature profile in the nasal cavity. Laryngoscope. 2000;110(4):651–654. doi: 10.1097/00005537-200004000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Walker AK, Bethune DW. A comparative study of condenser humidifiers. Anaesthesia. 1976;31(8):1086–1093. doi: 10.1111/j.1365-2044.1976.tb11950.x. [DOI] [PubMed] [Google Scholar]
- 4.Mercke U. The influence of temperature on mucociliary activity. Temperature range 40 degrees C to 50 degrees C. Acta Otolaryngol. 1974;78(3-4):253–258. doi: 10.3109/00016487409126352. [DOI] [PubMed] [Google Scholar]
- 5.Burton JD. Effects of dry anaesthetic gases on the respiratory mucous membrane. Lancet. 1962;1(7223):235–238. doi: 10.1016/s0140-6736(62)91187-x. [DOI] [PubMed] [Google Scholar]
- 6.Rathgeber J, Kazmaier S, Penack O, Züchner K. Evaluation of heated humidifiers for use on intubated patients: a comparative study of humidifying efficiency, flow resistance, and alarm functions using a lung model. Intensive Care Med. 2002;28(6):731–739. doi: 10.1007/s00134-002-1275-9. [DOI] [PubMed] [Google Scholar]
- 7.Déry R. The evolution of heat and moisture in the respiratory tract during anaesthesia with a non-rebreathing system. Can Anaesth Soc J. 1973;20(3):296–309. doi: 10.1007/BF03027168. [DOI] [PubMed] [Google Scholar]
- 8.Lucato JJ, Adams AB, Souza R, Torquato JA, Carvalho CR, Marini JJ. Evaluating humidity recovery efficiency of currently available heat and moisture exchangers: a respiratory system model study. Clinics (Sao Paulo) 2009;64(6):585–590. doi: 10.1590/S1807-59322009000600015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Association for Respiratory Care. Restrepo RD, Walsh BK. Humidification during invasive and noninvasive mechanical ventilation: 2012. Respir Care. 2012;57(5):782–788. doi: 10.4187/respcare.01766. [DOI] [PubMed] [Google Scholar]
- 10.Branson RD, Campbell RS, Davis K, Porembka DT. Anaesthesia circuits, humidity output, and mucociliary structure and function. Anaesth Intensive Care. 1998;26(2):178–183. doi: 10.1177/0310057X9802600208. [DOI] [PubMed] [Google Scholar]
- 11.Forbes AR. Temperature, humidity and mucus flow in the intubated trachea. Br J Anaesth. 1974;46(1):29–34. doi: 10.1093/bja/46.1.29. [DOI] [PubMed] [Google Scholar]
- 12.Wiesmiller K, Keck T, Leiacker R, Lindemann J. Simultaneous in vivo measurements of intranasal air and mucosal temperature. Eur Arch Otorhinolaryngol. 2007;264(6):615–619. doi: 10.1007/s00405-006-0232-6. [DOI] [PubMed] [Google Scholar]
- 13.Keck T, Leiacker R, Heinrich A, Kühnemann S, Rettinger G. Humidity and temperature profile in the nasal cavity. Rhinology. 2000;38(4):167–171. [PubMed] [Google Scholar]
- 14.Pillow JJ, Hillman NH, Polglase GR, Moss TJ, Kallapur SG, Cheah FC, et al. Oxygen, temperature and humidity of inspired gases and their influences on airway and lung tissue in near-term lambs. Intensive Care Med. 2009;35(12):2157–2163. doi: 10.1007/s00134-009-1624-z. [DOI] [PubMed] [Google Scholar]
- 15.Uchiyama A, Yoshida T, Yamanaka H, Fujino Y. Estimation of tracheal pressure and imposed expiratory work of breathing by the endotracheal tube, heat and moisture exchanger, and ventilator during mechanical ventilation. Respir Care. 2013;58(7):1157–1169. doi: 10.4187/respcare.01698. [DOI] [PubMed] [Google Scholar]
- 16.Eckerbom B, Lindholm CE. Performance evaluation of six heat and moisture exchangers according to the Draft International Standard (ISO/DIS 9360) Acta Anaesthesiol Scand. 1990;34(5):404–409. doi: 10.1111/j.1399-6576.1990.tb03112.x. [DOI] [PubMed] [Google Scholar]
- 17.Cohen IL, Weinberg PF, Fein IA, Rowinski GS. Endotracheal tube occlusion associated with the use of heat and moisture exchangers in the intensive care unit. Crit Care Med. 1988;16(3):277–279. doi: 10.1097/00003246-198803000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Branson R, Davis Jr K. Evaluation of 21 passive humidifiers according to the ISO 9360 standard: moisture output, dead space, and flow resistance. Respir Care. 1996;41:736–743. [Google Scholar]
- 19.Martin C, Papazian L, Perrin G, Saux P, Gouin F. Preservation of humidity and heat of respiratory gases in patients with a minute ventilation greater than 10 L/min. Crit Care Med. 1994;22(11):1871–1876. [PubMed] [Google Scholar]
- 20.Martin C, Thomachot L, Quinio B, Viviand X, Albanese J. Comparing two heat and moisture exchangers with one vaporizing humidifier in patients with minute ventilation greater than 10 L/min. Chest. 1995;107(5):1411–1415. doi: 10.1378/chest.107.5.1411. [DOI] [PubMed] [Google Scholar]
- 21.Unal N, Kanhai JK, Buijk SL, Pompe JC, Holland WP, Gültuna I, et al. A novel method of evaluation of three heat-moisture exchangers in six different ventilator settings. Intensive Care Med. 1998;24(2):138–146. doi: 10.1007/s001340050535. [DOI] [PubMed] [Google Scholar]
- 22.Wilkes AR. Heat and moisture exchangers. Structure and function. Respir Care Clin N Am. 1998;4(2):261–279. [PubMed] [Google Scholar]
- 23.Lee MG, Ford JL, Hunt PB, Ireland DS, Swanson PW. Bacterial retention properties of heat and moisture exchange filters. Br J Anaesth. 1992;69(5):522–525. doi: 10.1093/bja/69.5.522. [DOI] [PubMed] [Google Scholar]
- 24.Boyer A, Thiéry G, Lasry S, Pigné E, Salah A, de Lassence A, et al. Long-term mechanical ventilation with hygroscopic heat and moisture exchangers used for 48 hours: a prospective clinical, hygrometric, and bacteriologic study. Crit Care Med. 2003;31(3):823–829. doi: 10.1097/01.CCM.0000055382.87129.DD. [DOI] [PubMed] [Google Scholar]
- 25.Turnbull D, Fisher PC, Mills GH, Morgan-Hughes NJ. Performance of breathing filters under wet conditions: a laboratory evaluation. Br J Anaesth. 2005;94(5):675–682. doi: 10.1093/bja/aei091. [DOI] [PubMed] [Google Scholar]
- 26.Davis Jr K, Evans SL, Campbell RS, Johannigman JA, Luchette FA, Porembka DT, et al. Prolonged use of heat and moisture exchangers does not affect device efficiency or frequency rate of nosocomial pneumonia. Crit Care Med. 2000;28(5):1412–1418. doi: 10.1097/00003246-200005000-00026. [DOI] [PubMed] [Google Scholar]
- 27.Le Bourdellès G, Mier L, Fiquet B, Djedaïni K, Saumon G, Coste F, et al. Comparison of the effects of heat and moisture exchangers and heated humidifiers on ventilation and gas exchange during weaning trials from mechanical ventilation. Chest. 1996;110(5):1294–1298. doi: 10.1378/chest.110.5.1294. [DOI] [PubMed] [Google Scholar]
- 28.Campbell RS, Davis Jr K, Johannigman JA, Branson RD. The effects of passive humidifier dead space on respiratory variables in paralyzed and spontaneously breathing patients. Respir Care. 2000;45(3):306–312. [PubMed] [Google Scholar]
- 29.Chikata Y, Oto J, Onodera M, Nishimura M. Humidification performance of humidifying devices for tracheostomized patients with spontaneous breathing: a bench study. Respir Care. 2013;58(9):1442–1448. doi: 10.4187/respcare.02093. [DOI] [PubMed] [Google Scholar]
- 30.Brusasco C, Corradi F, Vargas M, Bona M, Bruno F, Marsili M, et al. In vitro evaluation of heat and moisture exchangers designed for spontaneously breathing tracheostomized patients. Respir Care. 2013;58(11):1878–1885. doi: 10.4187/respcare.02405. [DOI] [PubMed] [Google Scholar]
- 31.Prat G, Renault A, Tonnelier JM, Goetghebeur D, Oger E, Boles JM, et al. Influence of the humidification device during acute respiratory distress syndrome. Intensive Care Med. 2003;29(12):2211–2215. doi: 10.1007/s00134-003-1926-5. [DOI] [PubMed] [Google Scholar]
- 32.Hinkson CR, Benson MS, Stephens LM, Deem S. The effects of apparatus dead space on P(aCO2) in patients receiving lung-protective ventilation. Respir Care. 2006;51(10):1140–1144. [PubMed] [Google Scholar]
- 33.International Standardization Organization (ISO) Anaesthetic and respiratory equipment - Heat and moisture exchangers (HMEs) for humidifying respired gases in humans - Part 2: HMEs for use with tracheostomized patients having minimum tidal volumes of 250 ml. EN ISO 9360-2:2009, ISO 9360-2:2001. Available from: https://www.iso.org/obp/ui/#iso:std:iso:9360:-2:ed-1:v1:en.
- 34.Lucato JJ, Tucci MR, Schettino GP, Adams AB, Fu C, Forti Jr G, et al. Evaluation of resistance in 8 different heat-and-moisture exchangers: effects of saturation and flow rate/profile. Respir Care. 2005;50(5):636–643. [PubMed] [Google Scholar]
- 35.Chiaranda M, Verona L, Pinamonti O, Dominioni L, Minoja G, Conti G. Use of heat and moisture exchanging (HME) filters in mechanically ventilated ICU patients: influence on airway flow-resistance. Intensive Care Med. 1993;19(8):462–466. doi: 10.1007/BF01711088. [DOI] [PubMed] [Google Scholar]
- 36.Lellouche F, Qader S, Taillé S, Lyazidi A, Brochard L. Influence of ambient temperature and minute ventilation on passive and active heat and moisture exchangers. Respir Care. 2014;59(5):637–643. doi: 10.4187/respcare.02523. [DOI] [PubMed] [Google Scholar]
- 37.Thomachot L, Boisson C, Arnaud S, Michelet P, Cambon S, Martin C. Changing heat and moisture exchangers after 96 hours rather than after 24 hours: a clinical and microbiological evaluation. Crit Care Med. 2000;28(3):714–720. doi: 10.1097/00003246-200003000-00019. [DOI] [PubMed] [Google Scholar]
- 38.Ricard JD, Le Mière E, Markowicz P, Lasry S, Saumon G, Djedaïni K, et al. Efficiency and safety of mechanical ventilation with a heat and moisture exchanger changed only once a week. Am J Respir Crit Care Med. 2000;161(1):104–109. doi: 10.1164/ajrccm.161.1.9902062. [DOI] [PubMed] [Google Scholar]
- 39.Thomachot L, Leone M, Razzouk K, Antonini F, Vialet R, Martin C. Randomized clinical trial of extended use of a hydrophobic condenser humidifier: 1 vs. 7 days. Crit Care Med. 2002;30(1):232–237. doi: 10.1097/00003246-200201000-00033. [DOI] [PubMed] [Google Scholar]
- 40.Roustan JP, Kienlen J, Aubas P, Aubas S, du Cailar J. Comparison of hydrophobic heat and moisture exchangers with heated humidifier during prolonged mechanical ventilation. Intensive Care Med. 1992;18(2):97–100. doi: 10.1007/BF01705040. [DOI] [PubMed] [Google Scholar]
- 41.Oh TE, Lin ES, Bhatt S. Resistance of humidifiers, and inspiratory work imposed by a ventilator-humidifier circuit. Br J Anaesth. 1991;66(2):258–263. doi: 10.1093/bja/66.2.258. [DOI] [PubMed] [Google Scholar]
- 42.Roux NG, Plotnikow GA, Villalba DS, Gogniat E, Feld V, RiberoVairo N, et al. Evaluation of an active humidification system for inspired gas. Clin Exp Otorhinolaryngol. 2015;8(1):69–75. doi: 10.3342/ceo.2015.8.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roux NG, Feld V, Gogniat E, Villalba D, Plotnikow G, Ribero Vairo N, et al. El frasco humidificador como sistema de humidificación del gas inspirado no cumple con las recomendaciones. Evaluación y comparación de tres sistemas de humidificación. Estudio de laboratorio. Med Intensiva. 2010;27(3) [Google Scholar]
- 44.Ari A, Alwadeai KS, Fink JB. Effects of heat and moisture exchangers and exhaled humidity on aerosol deposition in a simulated ventilator-dependent adult lung model. Respir Care. 2017;62(5):538–543. doi: 10.4187/respcare.05015. [DOI] [PubMed] [Google Scholar]
- 45.Thomachot L, Viviand X, Boyadjiev I, Vialet R, Martin C. The combination of a heat and moisture exchanger and a Booster: a clinical and bacteriological evaluation over 96 h. Intensive Care Med. 2002;28(2):147–153. doi: 10.1007/s00134-001-1193-2. [DOI] [PubMed] [Google Scholar]
- 46.Pelosi P, Severgnini P, Selmo G, Corradini M, Chiaranda M, Novario R, et al. In vitro evaluation of an active heat-and-moisture exchanger: the Hygrovent Gold. Respir Care. 2010;55(4):460–466. [PubMed] [Google Scholar]
- 47.Branson RD, Campbell RS, Johannigman JA, Ottaway M, Davis Jr K, Luchette FA, et al. Comparison of conventional heated humidification with a new active hygroscopic heat and moisture exchanger in mechanically ventilated patients. Respir Care. 1999;44(8):912–917. [Google Scholar]
- 48.Siempos II, Vardakas KZ, Kopterides P, Falagas ME. Impact of passive humidification on clinical outcomes of mechanically ventilated patients: a meta-analysis of randomized controlled trials. Crit Care Med. 2007;35(12):2843–2851. doi: 10.1097/01.ccm.0000295302.67973.9a. [DOI] [PubMed] [Google Scholar]
- 49.Kelly M, Gillies D, Todd DA, Lockwood C. Heated humidification versus heat and moisture exchangers for ventilated adults and children. Cochrane Database Syst Rev. 2010;(4):CD004711–CD004711. doi: 10.1002/14651858.CD004711.pub2. [DOI] [PubMed] [Google Scholar]
- 50.Branson RD. Humidification for patients with artificial airways. Respir Care. 1999;44(6):630–641. [Google Scholar]
- 51.American Thoracic Society. Infectious Diseases Society of America Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 52.Klompas M, Branson R, Eichenwald EC, Greene LR, Howell MD, Lee G, et al. Strategies to prevent ventilator-associated pneumonia in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(Suppl 2):S133–S154. doi: 10.1017/s0899823x00193894. [DOI] [PubMed] [Google Scholar]
- 53.Prin S, Chergui K, Augarde R, Page B, Jardin F, Vieillard-Baron A. Ability and safety of a heated humidifier to control hypercapnic acidosis in severe ARDS. Intensive Care Med. 2002;28(12):1756–1760. doi: 10.1007/s00134-002-1520-2. [DOI] [PubMed] [Google Scholar]
- 54.Morán I, Bellapart J, Vari A, Mancebo J. Heat and moisture exchangers and heated humidifiers in acute lung injury/acute respiratory distress syndrome patients. Effects on respiratory mechanics and gas exchange. Intensive Care Med. 2006;32(4):524–531. doi: 10.1007/s00134-006-0073-1. [DOI] [PubMed] [Google Scholar]
- 55.Parrilla FJ, Morán I, Roche-Campo F, Mancebo J. Ventilatory strategies in obstructive lung disease. Semin Respir Crit Care Med. 2014;35(4):431–440. doi: 10.1055/s-0034-1382155. [DOI] [PubMed] [Google Scholar]
- 56.Iotti GA, Olivei MC, Braschi A. Mechanical effects of heat- moisture exchangers in ventilated patients. Crit Care. 1999;3(5):R77–R82. doi: 10.1186/cc361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Girault C, Breton L, Richard JC, Tamion F, Vandelet P, Aboab J, et al. Mechanical effects of airway humidification devices in difficult to wean patients. Crit Care Med. 2003;31(5):1306–1311. doi: 10.1097/01.CCM.0000063284.92122.0E. [DOI] [PubMed] [Google Scholar]
- 58.McCall JE, Cahill TJ. Respiratory care of the burn patient. J Burn Care Rehabil. 2005;26(3):200–206. [PubMed] [Google Scholar]
- 59.Lellouche F, Qader S, Taille S, Lyazidi A, Brochard L. Under-humification and over-humidification during moderate induced hypothermia with usual devices. Intensive Care Med. 2006;32(7):1014–1021. doi: 10.1007/s00134-006-0192-8. [DOI] [PubMed] [Google Scholar]
- 60.Oto J, Nakataki E, Okuda N, Onodera M, Imanaka H, Nishimura M. Hygrometric properties of inspired gas and oral dryness in patients with acute respiratory failure during noninvasive ventilation. Respir Care. 2014;59(1):39–45. doi: 10.4187/respcare.02351. [DOI] [PubMed] [Google Scholar]
- 61.Nava S, Navalesi P, Gregoretti C. Interfaces and humidification for noninvasive mechanical ventilation. Respir Care. 2009;54(1):71–84. [PubMed] [Google Scholar]