This cohort study assesses the efficacy of exome-targeted capture sequencing to detect mutations in genes broadly linked to cerebellar ataxia and investigates their prevalence in a large cohort of undiagnosed patients with various phenotypic presentations.
Key Points
Questions
Is exome-targeted capture sequencing able to detect mutations in genes broadly linked to ataxia, and what is the prevalence of such mutations in a large cohort of undiagnosed patients with various phenotypic presentations?
Findings
This cohort study of 319 patients with undiagnosed cerebellar ataxia used a sequencing approach that allowed the identification of genetically relevant variants in known genes in 91 (28.5%). This approach had the highest success rate for patients with spastic ataxia or a cerebellar ataxia with oculomotor apraxia–like phenotype; SPG7, SACS, SETX, SYNE1, and CACNA1A were the most frequently mutated genes.
Meaning
Mutations were identified in a broad range of genes implicated in ataxia and related neurologic diseases, even in cohorts that underwent previous extensive screening.
Abstract
Importance
Molecular diagnosis is difficult to achieve in disease groups with a highly heterogeneous genetic background, such as cerebellar ataxia (CA). In many patients, candidate gene sequencing or focused resequencing arrays do not allow investigators to reach a genetic conclusion.
Objectives
To assess the efficacy of exome-targeted capture sequencing to detect mutations in genes broadly linked to CA in a large cohort of undiagnosed patients and to investigate their prevalence.
Design, Setting, and Participants
Three hundred nineteen index patients with CA and without a history of dominant transmission were included in the this cohort study by the Spastic Paraplegia and Ataxia Network. Centralized storage was in the DNA and cell bank of the Brain and Spine Institute, Salpetriere Hospital, Paris, France. Patients were classified into 6 clinical groups, with the largest being those with spastic ataxia (ie, CA with pyramidal signs [n = 100]). Sequencing was performed from January 1, 2014, through December 31, 2016. Detected variants were classified as very probably or definitely causative, possibly causative, or of unknown significance based on genetic evidence and genotype-phenotype considerations.
Main Outcomes and Measures
Identification of variants in genes broadly linked to CA, classified in pathogenicity groups.
Results
The 319 included patients had equal sex distribution (160 female [50.2%] and 159 male patients [49.8%]; mean [SD] age at onset, 27.9 [18.6] years). The age at onset was younger than 25 years for 131 of 298 patients (44.0%) with complete clinical information. Consanguinity was present in 101 of 298 (33.9%). Very probable or definite diagnoses were achieved for 72 patients (22.6%), with an additional 19 (6.0%) harboring possibly pathogenic variants. The most frequently mutated genes were SPG7 (n = 14), SACS (n = 8), SETX (n = 7), SYNE1 (n = 6), and CACNA1A (n = 6). The highest diagnostic rate was obtained for patients with an autosomal recessive CA with oculomotor apraxia–like phenotype (6 of 17 [35.3%]) or spastic ataxia (35 of 100 [35.0%]) and patients with onset before 25 years of age (41 of 131 [31.3%]). Peculiar phenotypes were reported for patients carrying KCND3 or ERCC5 variants.
Conclusions and Relevance
Exome capture followed by targeted analysis allows the molecular diagnosis in patients with highly heterogeneous mendelian disorders, such as CA, without prior assumption of the inheritance mode or causative gene. Being commonly available without specific design need, this procedure allows testing of a broader range of genes, consequently describing less classic phenotype-genotype correlations, and post hoc reanalysis of data as new genes are implicated in the disease.
Introduction
Hereditary cerebellar ataxias (CAs) are clinically and genetically heterogeneous. All transmission modes have been described. The cardinal cerebellar syndrome is frequently part of a complex clinical spectrum with additional neurologic and/or extraneurologic symptoms.1
The most frequent autosomal recessive (AR) CAs are Friedreich ataxia, caused by GAA repeat expansions in intron 1 of FXN (OMIM 606829),2 and ataxia-telangiectasia, caused by loss-of-function mutations in ATM (OMIM 607585).3 Nonclassic clinical pictures have been described for both.4,5 Autosomal dominant (AD) CAs are most often caused by CAG repeat expansions in ATXN1 (OMIM 601556), ATXN2 (OMIM 601517), ATXN3 (OMIM 607047), CACNA1A (OMIM 601011), ATXN7 (OMIM 607640), TBP (OMIM 600075), or ATN1 (OMIM 607462).6 Overall, mutations in more than 140 genes have been described, involving pathways such as mitochondrial functions, DNA repair, transcription and translation, ciliary structure, and lipid biosynthesis.1,7
Sanger sequencing of candidate genes or panel approaches8 often fails to lead to a diagnosis.1 We aimed to evaluate the efficacy of exome-capture sequencing followed by targeted analysis of genes broadly linked to CA9,10,11,12 to identify mutations in 319 patients with undiagnosed CA and without an AD transmission history. To our knowledge, this CA cohort is the largest studied.
Methods
Patient Recruitment and Clinical Evaluation
Three hundred nineteen index cases of CA were recruited by the Spastic Paraplegia and Ataxia (SPATAX) network (https://spatax.wordpress.com/) and examined using a standardized form (https://spatax.files.wordpress.com/2013/09/fichecliniquespatax-eurospa-2011.pdf). The sexes were equally distributed. For the 210 patients with available information, the national origin was mostly France (112 [53.3%]) and continental Europe (39 [18.6%]). We classified the 298 cases with full phenotypic information into the following 6 clinical groups: (1) pure ataxic phenotype (n = 62), (2) additional spastic component (spastic ataxia) (n = 100), (3) complex late-onset clinical picture with extrapyramidal signs (n = 30), (4) metabolic presentation with mitochondrial features (sensorineural hearing loss, ptosis, ophthalmoplegia, optic atrophy, axonal neuropathy, cardiomyopathy, short stature, and/or diabetes type 1) or white matter changes (n = 70), (5) sensory ataxia (n = 19), or (6) a CA with oculomotor apraxia (AOA)–like presentation (n = 17) (Table). The remaining 21 patients were unclassified. The patients’ familial anamneses included no evidence of AD transmission. Recessive inheritance was considered to be plausible based on consanguinity (101 of 298 [33.9%]) or family history consisting of at least 2 affected siblings (59 of 298 [19.8%]) with no case in other generations. According to a classic nonsystematic clinical approach, expansions of FXN (80 patients) or ADCA genes (132 patients, including ATXN1 in 129, ATXN2 in 129, ATXN3 in 130, CACNA1A in 126, ATXN7 in 110, TBP in 47, and ATN1 in 102) and mutations in various genes (eg, APTX [OMIM 606350], SETX [OMIM 608465], SPG7 [OMIM 602783], SACS [OMIM 604490], and POLG [OMIM 174763]) were ruled out when the phenotype was suggested by means of clinical presumption or biological workup (ie, measurement of albumin, cholesterol, or α-fetoprotein level). This study was approved by the Paris Necker ethics committee. Written informed consent was obtained in accordance with French ethics regulations.
Table. Clinical Subgroups Among the Cohort.
| Clinical Group | No. of Index Patients | No. (%) of Patients | ||||||
|---|---|---|---|---|---|---|---|---|
| Age at Onset <25 y | Age at Onset >40 y | Consanguinity | Very Probable or Definite Diagnosis | Very Probable or Definite Diagnosis When Age at Onset <25 y | Very Probable or Definite Diagnosis When Age at Onset >40 y | Possible Diagnosis | ||
| AOA-like phenotype (increased α-fetoprotein level, low albumin level, ocular apraxia) | 17 | 15 (88.2) | 1 (5.9) | 7 (41.2) | 6 (35.3) | 6 (35.3) | 0 | 2 (11.8) |
| Late complex (MSA-like, parkinsonism, not pyramidal) | 30 | 0 | 20 (66.7) | 7 (23.3) | 3 (10.0) | 0 | 0 | 1 (3.3) |
| Metabolic (mitochondrial features, white matter changes) | 70 | 45 (64.3) | 6 (8.6) | 24 (34.3) | 16 (22.9) | 10 (14.3) | 0 | 2 (2.9) |
| Pure (only cerebellar signs, slow progression) | 62 | 20 (32.3) | 13 (21.0) | 19 (30.6) | 9 (14.5) | 5 (8.1) | 0 | 6 (9.7) |
| Sensory ataxia (FRDA/PolG-like) | 19 | 9 (47.4) | 8 (42.1) | 8 (42.1) | 2 (10.5) | 2 (10.5) | 0 | 2 (10.5) |
| Spastic ataxia (cerebellar and pyramidal signs) | 100 | 42 (42.0) | 15 (15.0) | 36 (36.0) | 35 (35.0) | 18 (18.0) | 4 (4.0) | 6 (6.0) |
| Alla | 298 | 131 (44.0) | 63 (21.1) | 101 (33.9) | 72 (22.6)b | 41 (31.3) | 4 (6.4) | 19 (5.9) |
Abbreviations: AOA, cerebellar ataxia with oculomotor apraxia; FRDA, Friedreich ataxia; MSA, multisystemic atrophy; PolG, polymerase gamma.
Includes the 298 patients for whom complete clinical information was available.
Includes 1 patient with known SPG7 mutations lacking sufficient clinical information for classification.
Sequencing and Bioinformatics
Exome-enriched libraries were prepared with the rapid-capture expanded exome kit (Nextera; Illumina) and sequenced on the manufacturer’s system (HiSeq 2000; Illumina) (2 × 100–base pair paired-end reads). Sequence alignment and variant calling were performed following the Broad Institute’s Genome Analysis Toolkit (GATK)13,14,15 version 3 best practices. Sequence reads were aligned against the reference human genome (UCSC hg19) using the Burrows-Wheeler Alignment tool.16 The Picard software toolset (http://broadinstitute.github.io/picard/) was used to calculate summary alignment metrics and mark duplicate reads. Local realignments near indels, base-score recalibration, variant calling, joint genotyping, and variant quality score recalibration were performed using GATK.
Variants were annotated with Annovar17 (http://annovar.openbioinformatics.org/) and sorted with SnpSift18 (http://snpeff.sourceforge.net/SnpSift.html) based on (1) quality (GATK filter pass, quality >30), (2) effect on the coding sequence of a protein-coding gene (exonic nonsynonymous single-nucleotide variant or splice variant), (3) frequency in public databases of no greater than 1% (Exome Variant Server [http://evs.gs.washington.edu/EVS/] and Exome Aggregation Consortium [http://exac.broadinstitute.org/, https://www.biorxiv.org/content/early/2016/05/10/030338]), and (4) internal frequency (allele count ≤30; ie, ≤4.7%). IntersectBed (http://bedtools.readthedocs.io/en/latest/) allowed filtering variants affecting known CA or hereditary spastic paraplegia genes, because both overlap clinically, based on curation of PubMed performed in February 2015 and in-house lists (209 genes) (eTable 1 in the Supplement). Variants in other genes were not examined.
Variants Processing
Biallelic (homozygous or compound heterozygous) variants were first sought because of the likelihood of AR inheritance. Very rare (≤0.1% frequency in the aforementioned databases) heterozygous variants were also considered in ADCA genes (eTable 1 in the Supplement and Figure 1). The plausibility of genotype-phenotype correlations was evaluated for all flagged variants.
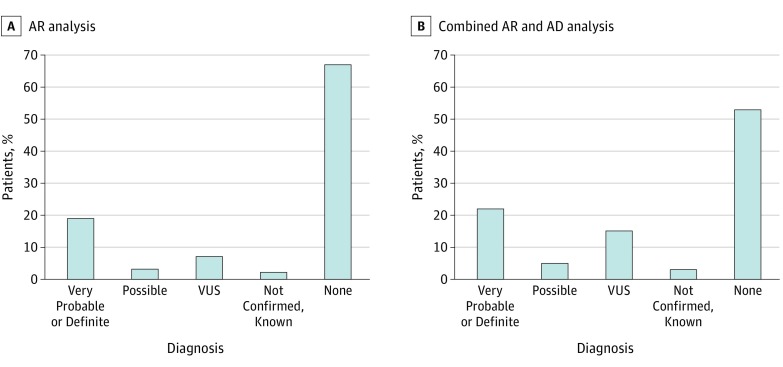
Figure 1. General Study Results.
Variants were sorted based on classic criteria (detailed in the Variant Analysis subsection of the Results section), then analyzed assuming an autosomal recessive (AR) transmission mode (including homozygous and heterozygous compound variants), which allowed identifying possibly to definitely causative variants in 74 patients (23.2%). Combining this analysis with one based on presumed autosomal dominant (AD) transmission (including heterozygous varients and a frequency ≤0.1%) improved this number to 91 patients (28.5%) for AD and AR inheritance modes, with 10 additional patients carrying very probable to definite pathogenic mutations. VUS indicates variant of unknown significance.
Sanger sequencing was performed if (1) the variant read depth was below 10 × , (2) informative family members were available for segregation (other affected members [n = 13] or healthy relatives without biallelic mutations [n = 6]), or (3) it allowed determining the cis- or trans-localization of compound heterozygous variants (n = 7). All Sanger resequenced variants and segregation results are reported in eTable 2 in the Supplement.
Results
The 319 included patients had equal sex distribution (160 female [50.2%] and 159 male [49.8%] patients). Mean (SD) age at onset was 27.9 (18.6) years; the age at onset was younger than 25 years for 131 of 298 patients (44.0%) with complete clinical data.
Sequencing
Approximately 8 gigabases of alignable sequence data were generated per sample. On average, 95% of exome capture baits had at least a 10 × depth and 70% at least a 30 × depth. A total of 488 393 single-nucleotide polymorphisms and 69 480 indels were included. We deliberately retained patients with low coverage to avoid distorting the percentage of positive findings.
Variant Analysis
The aforementioned analysis (Figure 1) provided 0 to 4 (AR) or 0 to 2 (AD) candidate genes per patient. We defined the following 4 pathogenicity groups: (1) probable or definitive causative variant(s), including a known or a recurrent variant, 3 or 4 concordant pathogenicity predictions by sorting intolerant from tolerant (SIFT), polymorphism phenotyping 2 (PolyPhen2) HumDiv, LRT, and Mutation Taster and Genomic Evolutionary Rate Profiling (GERP++) score of greater than 3 and plausible genotype-phenotype association, or compatible biomarker values (such as hexaminidase levels); (2) possibly causative variant(s), including most of the above but at least 1 criterion missing, or a slightly discordant phenotype for the gene spectrum; (3) variant(s) of clinically unknown significance (VUS); and (4) no diagnosis, including no variant in a known gene or a variant in known genes without convincing genetics arguments to match the clinical phenotype or the adequate inheritance mode.
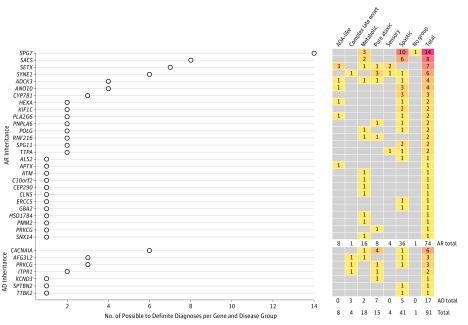
We obtained very probable or definite diagnoses for 72 patients (22.6%; including 62 with AR and 10 with AD inheritance) (Figure 1). We identified possibly causative variants for an additional 19 patients (6.0%; 12 with AR and 7 with AD inheritance). The most frequently encountered recessive mutations were in SPG7 (n = 14), followed by SACS (n = 8), SETX (n = 7), and SYNE1 (OMIM 608441) (n = 6) (Figure 2). Dominant mutations were most numerous in CACNA1A (n = 6), followed by PRKCG (OMIM 176980) (n = 3). Possible to definite variants are listed in eTable 2 in the Supplement, with arguments for their classification; VUS are available in eTable 3 in the Supplement.
Figure 2. Number of Possible to Definite Diagnoses per Gene and Disease Group.
The left part of the Figure plots the number of patients identified with possible to definite mutations for each gene listed. The right part shows the repartition of these patients among the 6 disease subgroups. Disease groups are described in the Patient Recruitment and Clinical Evaluation subsection of the Methods section. AD indicates autosomal dominant; AR, autosomal recessive; AOA, cerebellar ataxia with oculomotor apraxia.
Diagnostic Yield per Clinical Group
The best diagnositic yields were found for AOA-like presentations with positive biological biomarkers (6 of 17 [35.3%]) and spastic ataxias (35 of 100 [35.0%]) as very probable or definite and 2 of 17 (11.8%) and 6 of 100 (6%), respectively, as possible (Table). Patients with late complex CA then were the least frequently diagnosed, with 3 of 30 (10.0%) as very probable or definite and 1 of 30 (3.3%) as possible. Early disease onset and consanguinity were associated with better chances of diagnoses (41 of 131 [31.3%] with very probable or definite with onset before 25 years vs 4 of 63 [6.4%] after 40 years; 31 [30.7%] with consanguinity vs 41 [18.8%] without).
The predefined clinical group was generally concordant with the genetic diagnosis (Figure 2), with some exceptions. One patient with an AOA-like presentation (AAR-211-3) had elevated α-fetoprotein levels, no variant in the APTX gene, and pathogenic mutations in the ANO10 gene (NM_018075.4:c.132dupA:p.D45fs;c.1537T>C:p.C513R). Patients with ANO10 mutations usually develop cerebellar symptoms in adulthood (aged 17-43 years19), whereas patients with AOA show earlier onset. Onset at 24 years of age in this patient was coherent with ANO10 mutations. We classified the diagnosis as possible because the clinical presentation was slightly unusual. Other patients with biallelic loss-of-function ANO10 variants had classic spastic ataxia.
One patient (AFT-76-10) with epilepsy, thus classified in the metabolic group, carried a CACNA1A frameshift (NM_001127222.1:c.2493dupC:p.N832fs). Autosomal recessive inheritance was first assumed because of a consanguineous pedigree, but a dominant history later appeared, with ataxic signs in the daughter of a cousin, for whom no DNA was available for testing.
One patient with spastic ataxia (SAL-399-573) harboured 2 nonsense variants in SYNE1 (NM_182961.3:c.14273T>G:p.L4758X;c.23346G>A:p.W7782X). Pyramidal signs were classically limited in the SYNE1 spectrum, but recent results have established that spasticity is part of the phenotype.20
Reports of Peculiar Phenotypes
We classified a previously reported PDYN variant (NM_001190898.2:c.616C>T:p.R206C21) as VUS. Its frequency in the Exome Aggregation Consortium (0.026%, or 16 heterozygous individuals), the lack of an effect on prodynorphin processing to dynorphin A and B,21 and the discordant phenotype of this French patient (AAR-287-4 with childhood-onset ataxia, intellectual disability, and behavioral abnormalities) relative to the previously reported late-onset spastic ataxia cast its pathogenicity in doubt.
We found a possibly causative KCND3 variant (NM_004980.4:c.641A>G:p.K214R) in a patient with an unusual episodic gait disorder. The onset of relapsing limb paraesthesia at 30 years of age first evoked multiple sclerosis. Vertigo and episodic occurrences of gait disorder appeared thereafter without interictal ataxia. Increased reflexes, the Hoffmann sign, unilateral extensor plantar reflexes, and saccadic ocular pursuit were observed. Magnetic resonance imaging showed superior cerebellar vermis atrophy. The unaffected mother carried the variant, suggesting incomplete penetrance. This finding might be in accordance with its prevalence in public databases (28 of 119 072 alleles; ie, 28 heterozygous among 59 536 individuals [0.05%]).
One patient (AAR-180-11) harbored a previously reported homozygous frameshift variant of ANO10 (NM_018075.4:c.132dupA:p.D45fs).19 This specific variant was always found in compound heterozygosity with others and assumed to be too severe when homozygous. The onset at 22 years in this homozygous patient and a mild spastic ataxic phenotype (stage 1 disability with no functional handicap) after 5 years of disease evolution is in accordance with previous reports for ANO10 showing it to not be more severe.
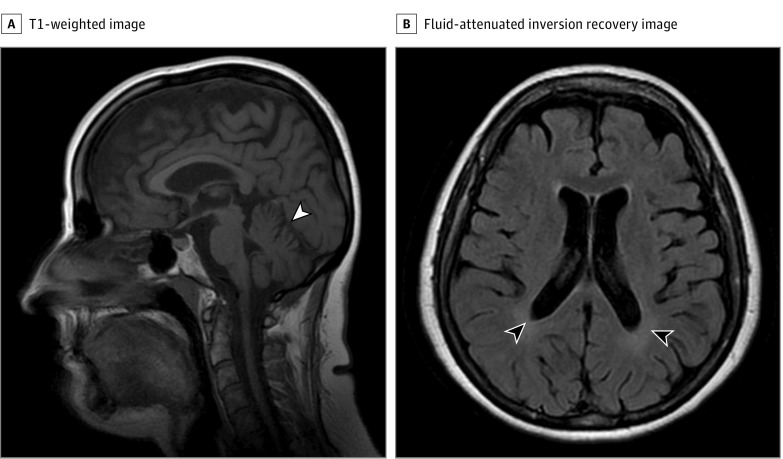
Finally, 2 siblings (AAR-73-3 and AAR-73-4) with spastic ataxia from a consanguineous pedigree carried a causative homozygous nonsense ERCC5 variant (NM_000123.3:c.3004C>T:p.Q1002X). The index patient (AAR-73-4) presented with spastic paraparesis, proximal and distal weakness, and severe sensory-motor demyelinating neuropathy at 24 years of age. She used a walking aid at 48 years of age, was wheelchair bound at 52 years of age, and had limited upward gaze and cognitive impairment at 54 years of age. The Scale for the Assessment and Rating of Ataxia score (18 of 40 at 46 years of age and 29 of 40 at 54 years of age) denoted clear progressivity. Magnetic resonance imaging of the brain showed slight cerebellar atrophy and white matter anomalies (Figure 3). Her brother (AAR-73-3) started to show signs of the disease at 15 years of age, used a walking aid at 39 years of age, and was bedridden and died at 51 years of age. The ERCC5 gene belongs to a DNA repair pathway; biallelic mutations have been associated with xeroderma pigmentosum, Cockayne syndrome, and combined xeroderma pigmentosum–Cockayne syndrome phenotypes.22,23 Major characteristics from classic xeroderma pigmentosum–Cockayne syndrome presentations (increased photosensitivity, skin pigmentation abnormalities, enophthalmos, progressive microcephaly, deafness, or retinitis) were absent. Our finding is nevertheless consistent with the ataxic gait of some patients with ERCC5 mutations.24
Figure 3. Magnetic Resonance Image of the Brain in a Patient.
A woman in her 40s harbored homozygous nonsense mutations in ERCC5 (p. Q1002X). After 22 years of disease evolution, the sagittal section of a T1-weighted image (A) showed mild atrophy of the upper cerebellar vermis (white arrowhead), and the axial fluid-attenuated inversion recovery section (B) showed slight white matter blurring (black arrowheads).
Discussion
We used exome-targeted capture sequencing followed by targeted analysis of genes broadly linked to CA to study 319 patients with undiagnosed CA, the largest such cohort to date, to assess the possibility of detecting mutations with this approach and their prevalence. Previously reported cohorts included no more than 76 patients.9
Our diagnostic yield was 22.6% (72 of 319 patients), with 5.9% (19 of 319) possible additional diagnoses (Figure 1). This rate might be lower because our cohort, recruited through a specialized university-based network of reference centers for rare diseases, has undergone extensive screening previously. However, these findings are similar to those of previous reports using targeted gene panels (18%8) or exome sequencing (21%-46%8,9,10,11,12,25) and other mendelian diseases (34% diagnoses in heterogeneous patients26; 33% in hereditary spastic paraplegia27).
The diagnostic yield was highly variable among clinical subgroups, being the highest for AOA-like phenotypes and spastic ataxias and the lowest for late-onset complex cases. It was also lower in patients with onset after 40 years of age (6.4%), in accordance with other observations.8,25 This finding may be explained by less extensive knowledge of genes implicated in late-onset ataxias or by the more frequent involvement of nongenetic causes.
In 9 cases, the diagnosis was established during the study but not confirmed. Five patients carried disease-causing repeat expansions, which cannot be detected by short-read techniques owing to the limited read length. These 5 patients included 1 with a heterozygous ATXN7 polyglutamine expansion, 1 with a heterozygous and 1 with a homozygous ATXN3 polyglutamine expansion, and 2 with pathogenic expansions in FXN. In this predominantly AR-assumed population, CAG repeat expansions in ATXN1, ATXN2, ATXN3, CACNA1A, ATXN7, TBP, and ATN1 were sought based only on suggestive clinical elements on examination, as were GAA repeats in FXN. A sixth patient harboured a homozygous 31-kb deletion in ANO10 encompassing exon 12 that was not detected by our approach. Mutations in NDRG1 (OMIM 605262) were reported in another patient during the study process. This gene, mostly implicated in Charcot-Marie-Tooth disease type 4D, was not included in our list. Finally, 2 patients flagged by quality check metrics were diagnosed with APTX-linked and SPG7-linked CA, but low global coverage prohibited from detecting the variants.
Exome-targeted capture sequencing is widely available and has several advantages compared with other sequencing approaches. If targeted gene panel sequencing is a cost-effective alternative to focus on many genes in 1 run, it requires an additional design step and redesign as new genes are linked to CA. Conversely, exome capture allows post hoc reanalysis of data as other groups identify mutations in new (CA) genes. For example, 2 patients not included in the claimed diagnosed group carried mutations in CAPN128 and 2 others carried mutations in SLC25A46.29
This approach also allows a broader range of genes to be tested. When AR inheritance is the prime hypothesis, genes with AD-transmitted mutations might be overlooked. Even without a dominant transmission history, AD analysis yielded a significant amount of additional diagnoses (Figure 1 and Figure 2), including 3 in consanguineous pedigrees. Two diagnoses were pathogenic, including a previously reported PRKCG mutation and a CACNA1A frameshift, which is classic for this gene.30 Possible explanations include the de novo occurrence of the variant, incomplete penetrance, a censor effect owing to premature death, or paternity issues. Autosomal dominant analysis significantly raised the number of VUS because missense heterozygous variations are difficult to interpret. Our results confirm CACNA1A as a prominent gene in CA, which we also confirmed in an independent AD cohort.31 We often did not have access to DNA from relatives because patients were from an adult neurologic clinic and were enrolled during the course of several years. Access to DNA from relatives would have allowed the detection of de novo variants or confirmation of the localization of heterozygous compound mutations in trans. Whenever possible, sequencing a trio might prove to be more efficacious.
In general, next-generation approaches circumvent the issue of gene prioritization based on phenotypic presumptions, with the limitation of the aforementioned expansions. This nonsystematic, time-consuming, classic approach missed the diagnosis in the prescreened patients in the absence of pathognomonic signs. Most genes mutated in our cohort were implicated in only 1 or 2 patients (Figure 2). Furthermore, exome-targeted capture sequencing allows a broader range of genes to be tested, including genes associated with neurologic diseases but not typically with ataxia. We enlarged the clinical spectrum linked to genes for which the phenotype is not primarily CA, such as ERCC5, PLA2G6, or SPG7. Careful examination of clinical records revealed suggestive signs of these syndromes in most cases. However, they were not sufficiently suggestive to have been evoked at first glance. Moreover, mutations in a given gene can lead to divergent phenotypes spread over several clinical groups (≤4 for SYNE1, SETX, and ADCK3). Capturing the exome makes it possible to avoid prior assumptions about the causative gene.10
Spastic paraplegia genes are the most frequent example of phenotype broadening, with mutations in SPG7 and SACS as well as CYP7B1, SPG11, and PLA2G6 (Figure 2 and eTable 2 in the Supplement). SPG7 mutations were recently recognized to be a major cause of CA32; most patients, however, develop pyramidal signs along with disease progression. In our cohort, 9 of 14 patients with SPG7 mutations had a spastic phenotype (64.3%) and 2 of 14 had pyramidal signs, although they were classified as metabolic. Six of 8 patients with SACS mutations (75.0%) presented with spastic ataxia, and 1 presented with pyramidal signs and demyelinating neuropathy. One patient harbouring possibly causative variants had a less classic phenotype of peripheral neuropathy, epilepsy, and myoclonus. Testing for a trait biomarker, such as an alteration of mitochondrial network morphology in fibroblasts,33 might help to reach a definite conclusion.
Convincing genetic data, however, usually correlated with a characteristic phenotype. In some cases, the clinical features reinforced the genetic diagnostic presumption. We did not use the clinicogenetic correlation as an exclusion criterion when the variant was genetically convincing, as suggested by others,9,34 although we classified patients with discordant clinical signs as possibly diagnosed, except for 1 CACNA1A frameshift. Instead, we used clinicogenetic correlation to strenghten evidence of pathogenicity. Genotype-phenotype correlations are highly challenged by next-generation sequencing,7 but clinical presentation, including neuroimaging findings, such as the degree of cerebellar atrophy or abnormal basal ganglia signal, should remain a prominent criterion in deciphering the pathogenicity of a given variant for a given patient.35
When available, trait biomarkers also aid the establishment of the pathogenicity of variants, as shown by the well-known example of elevated α-fetoprotein levels in ataxia-telangiectasia linked to ATM mutations. Oxysterol levels in patients harbouring CYP7B1 mutations are usually elevated, as in 1 patient carrying a homozygous nonsense variant (NM_004820.4:c.524G>A:p.W175X). Individuals with mutations in HEXA have low levels of hexaminidase A, as in 1 patient with an AOA-like presentation and a homozygous missense mutation (NM_000520.5:c.1511G>A:p.R504H) who was considered to be diagnosed despite discordant in silico pathogenicity estimates. Another patient with a spastic phenotype carried 2 missense variants (NM_000520.5:c.739C>T:p.R247W;c.1033G>A:p.G345S) for which pathogenicity could not be confirmed by hexaminidase dosage and that we thus labeled possibly pathogenic. TTPA mutations are usually accompanied by vitamin E deficiency. This was confirmed in one patient with a homozygous frameshift (NM_000370.3:c.744delA:p.E248fs) but not in another with compound heterozygous missense variants and a slightly divergent clinical profile (NM_000370.3:c.265C>T:p.P89S;c.515C>G:p.T172S). The characteristic magnetic resonance imaging sign of a pallidal T2-weighted hyposignal was observed on reexamination for 1 patient with PLA2G6 mutations (NM_003560.3:c.1903C>T:p.R635X;c.T2411C:p.L804P), allowing us to classify the variants as probably causative. Trait biomarkers, although not obligatory, are invaluable diagnostic tools when present. In the absence of such biomarkers, it is often difficult to reach a definite conclusion, as for the 49 VUS that we identified (eTable 3 in the Supplement).
Limitations
The major limitations of our approach rely in the fact that we missed some variants (ie, trinucleotide repeats expansions that cannot be detected by short-read sequencing and variants in genes not included in our design). The first fallback is inherent to the sequencing technique and can only be avoided by choosing another sequencing approach. The second limitation is a bioinformatics issue that can be solved by updating the gene list. Compared with the panel techniques, the coverage of all human genes might also not be optimized and the sequencing might be more expensive.
Conclusions
We aimed at assessing the efficacy of exome-targeted capture sequencing followed by analysis of genes known to be broadly linked to ataxia to identify mutations in undiagnosed patients. This technique is not optimized for sequencing a specific subset of genes, contrary to focused resequencing arrays, but is commonly available and allows the post hoc reanalysis of data as new causative genes are identified and the inclusion of a broader range of genes in the study design. We focused on a set of 209 genes, which allowed 30% of additional diagnoses in our otherwise extensively prescreened cohort. Our results confirm the genetic heterogeneity of CA, with many genes still to discover in ongoing work with this large cohort. Our strategy may be efficacious for obtaining results for known genes and for future development.
eTable 1. Known CA Genes
eTable 2. List of Possibly to Definitely Causative Variants
eTable 3. Variants of Unknown Significance
References
- 1.Anheim M, Tranchant C, Koenig M. The autosomal recessive cerebellar ataxias. N Engl J Med. 2012;366(7):636-646. [DOI] [PubMed] [Google Scholar]
- 2.Campuzano V, Montermini L, Lutz Y, et al. Frataxin is reduced in Friedreich ataxia patients and is associated with mitochondrial membranes. Hum Mol Genet. 1997;6(11):1771-1780. [DOI] [PubMed] [Google Scholar]
- 3.Savitsky K, Bar-Shira A, Gilad S, et al. A single ataxia telangiectasia gene with a product similar to PI-3 kinase. Science. 1995;268(5218):1749-1753. [DOI] [PubMed] [Google Scholar]
- 4.Lecocq C, Charles P, Azulay JP, et al. Delayed-onset Friedreich’s ataxia revisited. Mov Disord. 2016;31(1):62-69. [DOI] [PubMed] [Google Scholar]
- 5.Méneret A, Ahmar-Beaugendre Y, Rieunier G, et al. The pleiotropic movement disorders phenotype of adult ataxia-telangiectasia. Neurology. 2014;83(12):1087-1095. [DOI] [PubMed] [Google Scholar]
- 6.Durr A. Autosomal dominant cerebellar ataxias: polyglutamine expansions and beyond. Lancet Neurol. 2010;9(9):885-894. [DOI] [PubMed] [Google Scholar]
- 7.Coutelier M, Stevanin G, Brice A. Genetic landscape remodelling in spinocerebellar ataxias: the influence of next-generation sequencing. J Neurol. 2015;262(10):2382-2395. [DOI] [PubMed] [Google Scholar]
- 8.Németh AH, Kwasniewska AC, Lise S, et al. ; UK Ataxia Consortium . Next generation sequencing for molecular diagnosis of neurological disorders using ataxias as a model. Brain. 2013;136(pt 10):3106-3118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fogel BL, Lee H, Deignan JL, et al. Exome sequencing in the clinical diagnosis of sporadic or familial cerebellar ataxia. JAMA Neurol. 2014;71(10):1237-1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gomez CM, Das S. Clinical exome sequencing: the new standard in genetic diagnosis. JAMA Neurol. 2014;71(10):1215-1216. [DOI] [PubMed] [Google Scholar]
- 11.Sawyer SL, Schwartzentruber J, Beaulieu CL, et al. ; FORGE Canada Consortium . Exome sequencing as a diagnostic tool for pediatric-onset ataxia. Hum Mutat. 2014;35(1):45-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pyle A, Smertenko T, Bargiela D, et al. Exome sequencing in undiagnosed inherited and sporadic ataxias. Brain. 2015;138(pt 2):276-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKenna A, Hanna M, Banks E, et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010;20(9):1297-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van der Auwera GA, Carneiro MO, Hartl C, et al. From FastQ data to high confidence variant calls: the Genome Analysis Toolkit best practices pipeline. Curr Protoc Bioinform. 2013;(suppl 43):11.10.1-11.10.33. [DOI] [PMC free article] [PubMed]
- 15.DePristo MA, Banks E, Poplin R, et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat Genet. 2011;43(5):491-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25(14):1754-1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010;38(16):e164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cingolani P, Patel VM, Coon M, et al. Using Drosophila melanogaster as a model for genotoxic chemical mutational studies with a new program, SnpSift. Front Genet. 2012;3:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Renaud M, Anheim M, Kamsteeg EJ, et al. Autosomal recessive cerebellar ataxia type 3 due to ANO10 mutations: delineation and genotype-phenotype correlation study. JAMA Neurol. 2014;71(10):1305-1310. [DOI] [PubMed] [Google Scholar]
- 20.Synofzik M, Smets K, Mallaret M, et al. SYNE1 ataxia is a common recessive ataxia with major non-cerebellar features: a large multi-centre study. Brain. 2016;139(pt 5):1378-1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jezierska J, Stevanin G, Watanabe H, et al. Identification and characterization of novel PDYN mutations in dominant cerebellar ataxia cases. J Neurol. 2013;260(7):1807-1812. [DOI] [PubMed] [Google Scholar]
- 22.Zafeiriou DI, Thorel F, Andreou A, et al. Xeroderma pigmentosum group G with severe neurological involvement and features of Cockayne syndrome in infancy. Pediatr Res. 2001;49(3):407-412. [DOI] [PubMed] [Google Scholar]
- 23.Drury S, Boustred C, Tekman M, et al. A novel homozygous ERCC5 truncating mutation in a family with prenatal arthrogryposis: further evidence of genotype-phenotype correlation. Am J Med Genet A. 2014;164A(7):1777-1783. [DOI] [PubMed] [Google Scholar]
- 24.Calmels N, Greff G, Obringer C, et al. Uncommon nucleotide excision repair phenotypes revealed by targeted high-throughput sequencing. Orphanet J Rare Dis. 2016;11:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marelli C, Guissart C, Hubsch C, et al. Mini-exome coupled to read-depth based copy number variation analysis in patients with inherited ataxias. Hum Mutat. 2016;37(12):1340-1353. [DOI] [PubMed] [Google Scholar]
- 26.Taylor JC, Martin HC, Lise S, et al. Factors influencing success of clinical genome sequencing across a broad spectrum of disorders. Nat Genet. 2015;47(7):717-726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Novarino G, Fenstermaker AG, Zaki MS, et al. Exome sequencing links corticospinal motor neuron disease to common neurodegenerative disorders. Science. 2014;343(6170):506-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Y, Hersheson J, Lopez D, et al. Defects in the CAPN1 gene result in alterations in cerebellar development and cerebellar ataxia in mice and humans. Cell Rep. 2016;16(1):79-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hammer MB, Ding J, Mochel F, et al. SLC25A46 mutations associated with autosomal recessive cerebellar ataxia in North African families. Neurodegener Dis. 2017;17(4-5):208-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ophoff RA, Terwindt GM, Vergouwe MN, et al. Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4. Cell. 1996;87(3):543-552. [DOI] [PubMed] [Google Scholar]
- 31.Coutelier M, Coarelli G, Monin ML, et al. ; SPATAX network . A panel study on patients with dominant cerebellar ataxia highlights the frequency of channelopathies. Brain. 2017;140(6):1579-1594. [DOI] [PubMed] [Google Scholar]
- 32.Pfeffer G, Pyle A, Griffin H, et al. SPG7 mutations are a common cause of undiagnosed ataxia. Neurology. 2015;84(11):1174-1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pilliod J, Moutton S, Lavie J, et al. New practical definitions for the diagnosis of autosomal recessive spastic ataxia of Charlevoix-Saguenay. Ann Neurol. 2015;78(6):871-886. [DOI] [PubMed] [Google Scholar]
- 34.MacArthur DG, Manolio TA, Dimmock DP, et al. Guidelines for investigating causality of sequence variants in human disease. Nature. 2014;508(7497):469-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davydov EV, Goode DL, Sirota M, Cooper GM, Sidow A, Batzoglou S. Identifying a high fraction of the human genome to be under selective constraint using GERP++. PLoS Comput Biol. 2010;6(12):e1001025. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Known CA Genes
eTable 2. List of Possibly to Definitely Causative Variants
eTable 3. Variants of Unknown Significance