Abstract
The diagnostic role of echocardiographic and hemodynamic assessment in acute mitral regurgitation (AMR) remains unclear. The central question of this study was to determine if echocardiographic and hemodynamic parameters can predict early clinical events in AMR. AMR was induced by percutaneously severing the mitral valve chordae tendineae in 39 Yorkshire pigs. Immediately after AMR induction, echocardiographic and hemodynamic exams were performed, and compared between those who died and those who survived within 30-days of the procedure. Echocardiographic indices of MR severity as well as the left atrial pressure showed significant differences between survivors and non-survivors in univariate analysis. Multivariate logistic regression analysis revealed that echocardiography-derived regurgitant fraction and vena contracta as well as mean left atrial pressure could be used to segment the cohort into survivors and non-survivors. Our study demonstrated, for the first time, that echocardiographic and hemodynamic assessment of AMR provides predictive information on early clinical events in a clinically relevant animal model of AMR.
Keywords: Acute heart failure, MR, Pig model
Introduction
Severe acute mitral regurgitation (AMR) is found infrequently, but is a challenging disease requiring emergent care and proper management [1, 2]. Rupture of mitral valve chordae tendineae is the predominant cause of AMR from infectious endocarditis, myxomatous degeneration, and mitral valve prolapse as common etiologies [1, 3]. Methods of segmenting the AMR patient population into those that require emergent repair and conservative medical management with an elective repair remains an unmet need. In fact, there are no established clinical or diagnostic criteria for AMR surgical indication and clinical management of this patient population relies solely on the clinician’s discretion unless it is hemodynamically unstable [4]. In this study, using a clinically relevant animal model of AMR, we examined the value of echocardiographic and hemodynamic assessment for predicting early clinical events in order to identify candidates likely to benefit from emergent AMR repair.
Methods
The animal protocols complied with the National Institutes of Health Guide for the Care and Use of Laboratory Animals and standards of the US regulatory agencies. They were approved by the Institutional Animal Care and Use Committee.
AMR was induced in Yorkshire pigs (weighing 19.2 ± 2.6 kg; 3 males, 36 females) by percutaneous severing of mitral valve chordae tendineae as described previously [5]. Briefly, a cardiac biopsy catheter (BIOPAL 7, Cordis Corp., Miami, FL) was advanced to the left ventricle (LV) and the chordae tendineae of the posterior mitral valve apparatus was grasped under echocardiographic and fluoroscopic guidance (Fig. 1). The chordae tendineae was severed by retracting the bioptome into the guide sheath. Sequential chordae severing with mitral regurgitation (MR) assessments were continued until angiographic contrast reflux entered the pulmonary veins, and/or the echocardiographic mitral regurgitant jet reached the left atrium (LA) roof, and/or the hemodynamic LV end-diastolic pressure increased to 150% of baseline. More complete echocardiographic and hemodynamic exams of the LA and the LV were conducted before and after the AMR induction and the animals were recovered after hemodynamic stability was confirmed. The degree of MR was calculated from these exams according to the recommendation from Journal of American Society of Echocardiography [6]. During follow-up, all animals presenting any symptoms were carefully evaluated and those with refractory heart failure symptoms after furosemide treatment were euthanized humanely under a deep anesthesia. Data are expressed as the mean ± standard deviation for continuous variables, and p < 0.05 was considered statistically significant. Statistical comparisons between the groups were performed by the Student t test, while the paired t test was used for within animal comparisons. Areas under the receiver operating characteristic (ROC) curves to segment the pigs that died or survived the 30-days follow-up period were calculated. Multiple logistic regression analysis was conducted with the variables that were significantly different between the survivors and non-survivors. The most representative parameters were chosen for the parameters that had a correlation co-efficient of greater than 0.8.
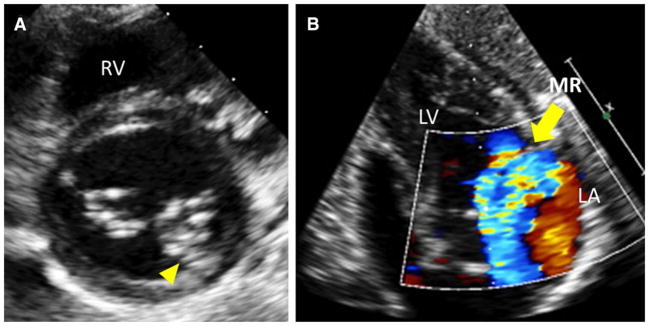
Fig. 1.
AMR induction. a Short axis echocardiographic view of the LV base below the mitral valve from left intercostal space. Yellow arrow head shows the tip of the biopsy catheter. The chordae tendineae connected to P2/P3 were aimed. Generally, severing of 1–3 cordae was sufficient to induce severe MR. b Representative echocardiographic image after AMR induction (substernal view)
Results
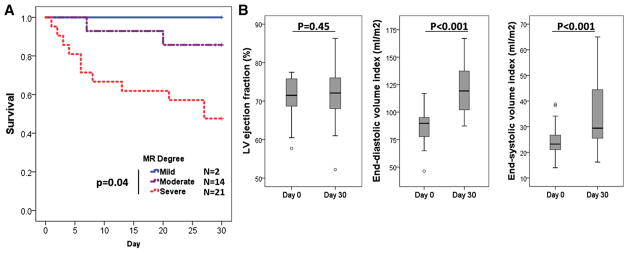
Among the 39 pigs, 2 pigs died during the procedure due to massive MR with cardiogenic shock and were excluded from the analysis. AMR pigs that survived more than 30-days were otherwise unremarkable unless they developed infectious endocarditis (n = 4). These pigs did not have any evidence of infectious endocarditis at the day-30 time point, however developed a fever afterwards suggesting the infection from the catheter procedures at day-30. Based on good survival after day-30, we classified the pigs that did not survive for 30-days would likely have benefited from emergency or sub-emergency surgery. Among these 37 pigs, 13 pigs died before reaching day-30 (Fig. 2). At day-30, surviving pigs had increased LV end-diastolic as well as end-systolic volume indices, however ejection fraction was maintained (Fig. 2).
Fig. 2.
Survival curves and LV changes. a Survival curves of animals after AMR according to visual MR assessment. b Changes in LV function and volumes. While both end-diastolic and end-systolic volume adjusted to the body surface area increased significantly, LV ejection fraction was maintained at 1 month
Table 1 shows the comparison of available variables between the groups, along with the area under the curve derived from drawing the receiver operating characteristic curves using death as the endpoint. Echocardiographic indices of MR severity including effective regurgitant orifice area, regurgitant fraction, vena contracta, and ratio of MR/LA area showed significant differences between the groups. LA mean and v wave pressure were also higher in the non-surviving group, whereas the LV end-systolic and end-diastolic pressures failed to reach statistical difference. We next conducted a multivariate logistic analysis using these variables and found that regurgitant fraction [odds ratio (OR) 1.18, 95% confidence interval (CI) 1.02–1.35, p = 0.02], vena contracta (OR 3.2, 95% CI 1.14–9.00, p = 0.03), and mean LA pressure (OR 1.48, 95% CI 1.04–2.12, p = 0.03) were all significant predictors of death within 30-days. The linear regression model assigned 84% of pigs to the correct group. Removal of 2 surviving mild MR pigs from the analysis did not change the overall results (Supplemental Table 1).
Table 1.
Echocardiographic and hemodynamic differences between the groups
| Early death (n = 13) | Survived (n = 24) | p value | AUC | |
|---|---|---|---|---|
| LVEF (%) | 77.6 ± 6.6 | 77.4 ± 7.4 | 0.93 | 0.50 |
| EROA (cm2) | 0.20 ± 0.06 | 0.14 ± 0.07 | 0.01 | 0.74 |
| RF (%) | 60.2 ± 9.3 | 48.2 ± 12.8 | 0.005 | 0.76 |
| MR volume (ml) | 22.5 ± 7.1 | 17.0 ± 6.9 | 0.03 | 0.73 |
| MR degree | 0.04 | 0.72 | ||
| Mild | 0 | 2 | ||
| Moderate | 2 | 12 | ||
| Severe | 11 | 10 | ||
| MR jet | 0.08 | 0.61 | ||
| Central | 11 | 13 | ||
| Eccentric | 2 | 11 | ||
| Vena contracta (mm) | 5.9 ± 1.4 | 4.9 ± 1.3 | 0.05 | 0.68 |
| MR area (cm2) | 4.0 ± 1.1 | 3.5 ± 1.3 | 0.31 | 0.64 |
| LA area (cm2) | 7.1 ± 1.3 | 7.9 ± 1.8 | 0.19 | 0.62 |
| MR/LA ratio (%) | 57 ± 16 | 44 ± 10 | 0.004 | 0.77 |
| mean LAP (mmHg) | 19.5 ± 7.7 | 12.5 ± 4.4 | 0.007 | 0.77 |
| LA a wave (mmHg) | 27.8 ± 8.1 | 23.9 ± 8.0 | 0.16 | 0.64 |
| LA v wave (mmHg) | 32.2 ± 11.9 | 22.8 ± 8.1 | 0.02 | 0.72 |
| LV ESP (mmHg) | 87 ± 19 | 92 ± 12 | 0.32 | 0.56 |
| LV EDP(mmHg) | 19.7 ± 7.6 | 15.9 ± 6.6 | 0.13 | 0.66 |
| LV DP (mmHg) | 66.9 ± 22.3 | 75.9 ± 13.0 | 0.13 | 0.62 |
| HR (bpm) | 112 ± 24 | 97 ± 21 | 0.06 | 0.66 |
AUC area under the receiver operating characteristic curve, DP developed pressure, EDP end-diastolic pressure, EF ejection fraction, ESP end-systolic pressure, EROA effective regurgitant orifice area, HR heart rate, LA left atrium, LV left ventricle, MR mitral regurgitation, RF regurgitant fraction
Discussion
In this study, we show for the first time that echocardiographic and hemodynamic parameters of AMR can have prognostic value on early clinical events. To have saved these animals, emergent or sub-emergent valve repair either by surgery or percutaneous intervention would have been necessary, whereas those that survived up to 30-days likely required an elective valve repair.
To our knowledge, no data exist on the impact of regurgitation degree on clinical outcomes in AMR. Lorusso et al [7] demonstrated that after emergency surgical repair in patients with AMR, the 30-day mortality rate was as high as 22.5%. Meanwhile, Gabbay et al. [1] reported, in their systematic literature review, that mitral chordae tendineae rupture is a relatively frequent reason for elective mitral valve surgery suggesting that many patients do not require emergent surgery. The gap between these studies was a lack of information on how to identify those who should receive emergent surgical repair vs those that should be considered for delayed elective procedures. Moreover, both of these studies did not provide indicators of MR severity, thus their prognostic value of evaluating MR severity prior to surgery was unclear. Our study thus, fills this gap and supports the use of echocardiographic and hemodynamic MR assessment in segmenting this patient population for emergent and elective MR repair. In general, use of semiquantitative parameters of MR evaluation did not result in significant differences between the groups in our study, whereas several quantitative parameters of echocardiographic MR evaluation, including effective regurgitant orifice area, regurgitant fraction, and MR volume, were found to be different between the groups. This suggests that pigs with severe MR can be better identified with quantitative assessments and the addition of the mean LA pressure on top of echocardiography-derived regurgitant fraction and vena contracta improves the predictive value. It needs to be realized, however, that the predictive value is still suboptimal even with a multivariate model, indicating the difficulty in accurately predicting outcomes in AMR.
Our study has some limitations. First, we used direct LA pressure measurement via trans-septal puncture, but this variable is not readily available in patients. Nevertheless, this can be replaced by pulmonary capillary wedge pressure by right heart catheterization since good correlation between these variables has been shown in various settings [8]. Second, although all the animals underwent the same anesthesia protocol, we cannot exclude its impact on the degree of MR as well as hemodynamic parameter assessments [9]. Third, different etiologies of AMR may significantly impact patient segmentation, especially for active endocarditis cases with large or unstable vegetation. Our animal model creation method precluded inclusion of etiology as a variable. However, mitral valve prolapse and myxomatous degeneration seems to be increasing in clinical populations [1], thus our data could be applied to this population. Finally, since our study was conducted in a pig model, future clinical studies are warranted to determine the reproducibility of our results in a clinical AMR population with an inclusion of clinical characteristics as variables.
In conclusion, we report that quantitative assessment of mitral regurgitation using echocardiographic and hemodynamic evaluations provide predictive information, albeit modestly, on early clinical events in a pig AMR model. Our results prompt more systematic evaluation of AMR patients in clinic to improve outcomes of this infrequent but important disease.
Supplementary Material
Acknowledgments
This study was supported by NIH P50 HL112324, R01 HL119046, R01 HL117505, R01HL128099, R01 HL129814, R01HL131404, & R43HL108581 (R. J. H.), and a Transatlantic Leducq Foundation grant. We would like to acknowledge the Gene Therapy Resource Program (GTRP) of the National Heart, Lung, and Blood Institute, National Institutes of Health. K. I. is supported by a Grant from American Heart Association 17SDG33410873. G. B. was supported by the French Federation of Cardiology.
Footnotes
Compliance with Ethical Standards
Conflict of interest None.
Electronic supplementary material The online version of this article (doi:10.1007/s10554-017-1215-y) contains supplementary material, which is available to authorized users.
References
- 1.Gabbay U, Yosefy C. The underlying causes of chordae tendinae rupture: a systematic review. Int J Cardiol. 2010;143(2):113–118. doi: 10.1016/j.ijcard.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 2.Horstkotte D, Schulte HD, Niehues R, Klein RM, Piper C, Strauer BE. Diagnostic and therapeutic considerations in acute, severe mitral regurgitation: experience in 42 consecutive patients entering the intensive care unit with pulmonary edema. J Heart Valve Dis. 1993;2(5):512–522. [PubMed] [Google Scholar]
- 3.Shiraishi I, Nishimura K, Sakaguchi H, Abe T, Kitano M, Kurosaki K, Kato H, Nakanishi T, Yamagishi H, Sagawa K, Ikeda Y, Morisaki T, Hoashi T, Kagisaki K, Ichikawa H. Acute rupture of chordae tendineae of the mitral valve in infants: a nationwide survey in Japan exploring a new syndrome. Circulation. 2014;130(13):1053–1061. doi: 10.1161/CIRCULATIONAHA.114.008592. [DOI] [PubMed] [Google Scholar]
- 4.Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, 3rd, Guyton RA, O’Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM, 3rd, Thomas JD, Members AATF. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521–e643. doi: 10.1161/CIR.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 5.Kawase Y, Ly HQ, Prunier F, Lebeche D, Shi Y, Jin H, Hadri L, Yoneyama R, Hoshino K, Takewa Y, Sakata S, Peluso R, Zsebo K, Gwathmey JK, Tardif JC, Tanguay JF, Hajjar RJ. Reversal of cardiac dysfunction after long-term expression of SERCA2a by gene transfer in a pre-clinical model of heart failure. J Am Coll Cardiol. 2008;51(11):1112–1119. doi: 10.1016/j.jacc.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 6.Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16:777–802. doi: 10.1016/S0894-7317(03)00335-3. [DOI] [PubMed] [Google Scholar]
- 7.Lorusso R, Gelsomino S, De Cicco G, Beghi C, Russo C, De Bonis M, Colli A, Sala A. Mitral valve surgery in emergency for severe acute regurgitation: analysis of postoperative results from a multicentre study. Eur J Cardiothorac Surg. 2008;33(4):573–582. doi: 10.1016/j.ejcts.2007.12.050. [DOI] [PubMed] [Google Scholar]
- 8.Nagy AI, Venkatesharan AI, Merkely B, Winter R, Barooah B, Dash PK, Manouras AI. The pulmonary capillary wedge pressure accurately reflects both normal and elevated left atrial pressure. Eur Heart J. 2014;35:1184–1184. doi: 10.1016/j.ahj.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 9.Sanfilippo F, Johnson C, Bellavia D, Morsolini M, Romano G, Santonocito C, Centineo L, Pastore F, Pilato M, Arcadipane A. Mitral regurgitation grading in the operating room: a systematic review and meta-analysis comparing preoperative and intraoperative assessments during cardiac surgery. J Cardiothorac Vasc Anesth. 2017 doi: 10.1053/j.jvca.2017.02.046. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.