Abstract
Background
Paired box gene 8 (PAX8) is expressed in and indispensable to thyroid development. MiR-144-3p is found dys-regulated in cancers, and it can block the expression of target gens. This study sought to understand the effect of MiR-144-3p in papillary thyroid carcinoma (PTC) as well as the associated mechanisms.
Materials and methods
Real-time PCR, immunohistochemical and Western blot assays were performed to examine the expression of target miRNA and/or genes. CCK-8 and flow cytometry analysis was used to respectively test cell growth, cell cycle progression and apoptosis. Luciferase reporter assay was performed to find out whether miR-144-3p could bind to the 3′ untranslated region of PAX8 or not.
Results
We found that PAX8 decreased in PTC, while miR-144-3p increased in PTC. Over-expression of miR-144-3p promoted the cell viability and cell cycle progression. The expressions of cell-cycle-related genes, cyclin D1, cyclin-dependent kinase 2 and CDC25A were modulated by miR-144-3p. Meanwhile, the presence or absence of miR-144-3p both affected epithelial-mesenchymal transition of PTC by regulating the expression of E-cadherin, N-cadherin and vimentin. Moreover, PAX8 may be a potential direct target of miR-144-3p. Mechanically, the activation of extracellular signal–regulated kinases 1/2, Akt and c-Jun N-terminal kinases may be associated with the tumor-promoting effect of miR-144-3p. In addition, the blockage of miR-144-3p forced the anti-tumor effect delivered by X-ray exposure or paclitaxel.
Conclusion
MiR-144-3p promoted the growth of tumor and the metastasis of PTC by targeting PAX 8. The study provided promising prognosis markers and valuable treatment strategy for PTC.
Keywords: Papillary thyroid carcinoma (PTC), Paired box gene 8 (PAX8), miR-144-3p, Cell cycle progression
Background
Papillary thyroid carcinoma (PTC), as a type of well-differentiated malignant tumor, accounts for approximately 80% of all primary thyroid cancers [1], which arises from the thyroid follicular epithelial cells. PTC is frequently found among women and children [2]. In the early stage of PTC, the symptoms of thyroid benign disease are often shown and such a phenomenon could easily lead to misdiagnosis, alternatively the most effective period may be missed. Various genetic and environmental factors contribute to the occurrence of PTC. Though PTC is highly curable due to the application of standard surgical treatment in combination with proper radioiodine ablation therapy, however, the rate of PTC recurrence remains very high and some patients even die from this condition [3]. Furthermore, the possibility of mortality increases in PTC patients if the tumor becomes surgically inoperable and is resistant to radioiodine. Thus, It is critical to develop accurate risk evaluation methods with the aim of preventing the recurrence of thyroid cancer.
The current diagnosis of PTC may be challenged by specimens with low cellularity. The detection sensitivity of PTC may be increased by using immunohistochemical stains. As a member of paired box (PAX) family, paired box gene 8 (PAX8) is a thyroid specific transcription factor. The PAX family are highly conserved in evolution, and it has indispensable functions in the development progression [4]. The critical role of PAX8 in the thyroid development and organogenesis was first reported in 1998 [5]. Various studies have observed that the expression of PAX8 sharply dropped in PTC [6–9], which is considered as a valuable marker for thyroid carcinoma. Based on these investigations, the strategy of affecting the distribution of PAX8 may be of scientific significance.
MicroRNAs (miRNAs), as small non-coding RNAs, have been the focus of researches for decades due to its vital role in gene regulation [10, 11]. The two mechanisms of miRNAs consist of the mRNA degradation and translation inhibition by binding to the 3′untranslational region (3′UTR) of target mRNAs [12]. Different miRNA expression profiles have been found in tumors and normal tissues, and such a phenomenon suggests the key role of miRNA in tumorgenesis [13, 14]. MiRNAs have critical roles in PTC progression [15, 16]. The phenomenon of abnormal miR-144-3p expression has been reported in colorectal cancer (CRC), nonsmall-cell lung cancer (NSCLC), osteosarcoma (OS) and hepatocellular carcinoma HCC [17–20]. However, very little is currently known about and reported on the effect of miR-144-3p. Therefore, it is interesting to investigate the role and relevant mechanisms of miR-144-3p in PTC, and to explore whether PAX8 expression can be regulated by miR-144-3p or not. This study will show a new regulation pathway in PTC development and provide potential prognosis and treatment targets for PTC.
Materials and methods
Tissue sample
Thirty paired tumor and adjacent normal tissue samples (at least 5 cm from the tumor loci) were collected from patients who had received surgical resections at The First Affiliated Hospital of China Medical University from December 2014 to January 2016. Informed written consents were obtained from all recruited patients, and the procedures in this study was been approved by the Ethics Committee of Cancer Institute of The First Affiliated Hospital of China Medical University.
Immunohistochemical (IHC) assay
The samples were treated with paraformaldehyde (4%) and were incubated in 20% sucrose solution at 4 °C overnight. Paraffin embedded tissue Sections (3–4 μm) were used for IHC analysis. After being deparaffinized in xylene and dehydration with graded ethanol, 3.0% hydrogen peroxide in methanol was incubated with the slides at room temperature for 15 min (min) to block endogenous peroxidase. The immunostaining was carried out using primary mouse monoclonal antibodies against PAX8 (1:20, ab53940, abcam, USA).Then the slides were incubated at 4 °C overnight. The primary antibody was first checked by anti-mouse IgG-horseradish peroxidase (HRP)-labeled polymer (ImmunoDetector HRP, CA), and then incubated with 3-3′-diaminobenzidine (DAB) chromogen. The immunostaining score was recorded according to the following criteria [21]: 0—no staining, 1—weak staining, 2—moderate staining, 3—strong staining by two pathologists in a blinded manner.
Cell culture and treatment
Human PTC cell line (B-CPAP) was purchased from the Chinese Academy of Sciences (Shanghai, China). RPMI 1640 medium containing 10% newborn bovine serum (FBS) were used for the culture of B-CPAP cells. The culture condition was set at 37 °C with 5% CO2. The cell grouping was as follows: Control, untreated PTC cells; mimics, PTC cells transfected with miR-144-3p mimics; inhibitor: PTC cells transfected with miR-144-3p inhibitors; NC, PTC cells transfected with miRNA negative control. For X-ray exposure, according to a previous study [22] irradiation dose was 3 Gy at 1.37 Gy/min at room temperature on an industrial portable at 150 kV X-ray unit (Philips Medical Systems). For paclitaxel treatment, cells were treated with 40 nM paclitaxel for 24 h [23].
Cell transfection
MiRNA scramble control vector (CmiR0001-MR04), has-miR-144 mimics vector (HmiR0275) and has-miR-144-3p inhibitor vector (HmiR-AN0189) were purchased from Guangzhou FulenGen Co., Ltd. Cell transfection was carried out using Lipofectamine 3000 (L3000008, Invitrogen) according to the manufacturer’s instruction.
CCK-8 method
The proliferation of PTC cells was determined by CCK-8 method according to the manufacturer’s instructions. At a density of 1 × 103 cells per well, cells were seeded in 96-well plates and transfected. After being transfected for 48 h, cells were then mixed with 10 μl CCK-8 solution (C0038, Beyotime, China) and put into incubation for 4 h at 37 °C. Finally, the optical density at a wavelength of 450 nm was recorded by a microplate reader (Biorad, USA).
Flow cytometric assay
Cell cycle distribution was determined using a propidium iodide (PI) staining. The cells were starved overnight in order to acquire the synchronizated cells, which were seeded into a 6-well plate at a density of 2 × 106 cells per well. After listed treatments, the cells were collected and fixed with 75% ethanol at 4 °C overnight. The next day, the cells were stained with PI (Sigma-Aldrich) and RNase A (Sigma-Aldrich). Fluorescein isothiocyanate (FITC)-annexin V/PI staining kit was applied (V13241, Invitrogen, USA). The cells were harvested and stained with Annexin V-FITC for 15 min and with PI for 5 min in the dark. The fluorescence signals were collected by FACSCanto (BD Bioscience, San Jose, CA) and then analyzed by FlowJo 8.7.1 software (Ashland, OR).
Luciferase reporter assay
At a density of 2 × 104 cells per well, PTC cells were cultured in a 96-well plate. 3′UTR-PAX8 firefly luciferase reporter (HmiT018794-MT06) was co-transfected with miR-144-3p mimics or inhibitors by using Lipofectamine 3000. The pRL-TK (Promega, Madison, WI) was seen as normalized control. The mutated (mut)-3′UTR-PAX8 firefly luciferase reporter was generated using a site-directed mutagenesis kit (KM131204, Tiangen, China) according to the manufacturer’s instructions. This mutated vector was treated as negative control. After 24 h, luciferase substrates for firefly and renilla were added into the cell lysate in each group. The Dual-Glo Luciferase Assay System (E2920, Promega) was adopted for measuring luciferase activity on a Turner BioSystems 20/20n luminometer.
Real-time PCR
Total RNA was isolated using Trizol regent (15596018, Invitrogen, USA) following the protocols. The M-MLV reverse transcriptase (promega, USA) and oligodT (or miRNA first-strand cDNA synthesis kit (Invitrogen)) were employed to synthesis cDNAf from mRNA or miRNA. The quantification of cDNA was performed on 7500-fast RT-PCR System (Applied Biosystems, USA) using SYBR Mixture (CWBio, China). Relative expression levels of U6, β-actin or GAPDH endogenous control were calculated by 2 − ΔΔCT method [24]. The primers used were as follows:
CDK2 forward 5′-CCTGGATGAAGATGGACGGA-3′,
CDK2 reverse 5′-GGAGAGGGTGAGATTAGGGC-3′;
CDC25A forward 5′-ACAACCGATGCAAGCTGTTT-3′,
CDC25A reverse 5′-CTCATGGGCCTTCTCTGGAT-3′;
Cyclin D1 forward 5′-CCCTCGGTGTCCTACTTCAA-3′,
Cyclin D1 reverse 5′-CTTAGAGGCCACGAACATGC-3′;
E-cadherin forward 5′-TCACATCCTACACTGCCCAG-3′;
E-cadherin reverse 5′-AGTGTCCCTGTTCCAGTAGC-3′;
N-cadherin forward 5′-ATATTTCCATCCTGCGCGTG-3′;
N-cadherin reverse 5′-GTTTGGCCTGGCGTTCTTTA-3′;
Vimentin forward 5′-AATAAGATCCTGCTGGCCGA-3′;
Vimentin reverse 5′-GGTGTTTTCGGCTTCCTCTC-3′;
PAX8 forward 5′-GCCTTCTCCCTCTGCCTTTA-3′;
PAX8 reverse 5′-TTATGCAGGCTCCAGTCACA-3′;
Bax forward 5′-GTGCCGGAACTGATCAGAAC-3′;
Bax reverse 5′- CCAAAGTAGGAGAGGAGGCC-3′;
Bcl-2 forward 5′-GCCTTCTTTGAGTTCGGTGG-3′;
Bcl-2 reverse 5′-GAAATCAAACAGAGGCCGCA-3′;
β-actin forward: 5′-CTCCATCCTGGCCTCGCTGT-3′;
β-actin reverse: 5′-GCTGTCACCTTCACCGTTCC-3′;
U6 Forward 5′-CTCGCTTCGGCAGCACA-3′;
U6 Reverse 5′-AACGCTTCACGAATTTGCGT-3′;
GAPDH forward: 5′-CACAGTCCATGCCATCACTG-3′;
GAPDH reverse: 5′-ATCTCGCTCCTGGAAGATGG-3′;
Western blot
Protein extraction kit (Solarbio, China) was used to isolate proteins, and then the concentration of the proteins was detected by BCA Protein Assay kit (Cwbio, China). The cell lysate was loaded on 10% SDS-PAGE after being boiled for 5 min to denaturation and then transferred onto a PVDF membrane (Millipore, USA). The non-specific antigens were blocked using 5% skimmed milk. Primary antibodies were incubated at 4 °C overnight. After removing the appropriate horseradish peroxidase-conjugated secondary antibody (ab97051, 1:3000, Abcam, USA), the blots were detected using Enhanced Chemiluminescence Detection kit (GE Healthcare Biosciences). The primary antibodies used in the experiment were as follows: N-cadherin (ab18203, 1:1000), Vimentin (ab137321, 1:1500), anti-PAX8 (ab53940,1:200), anti-p-Erk1/2 (ab201015, 1:1000), anti-Bcl-2 (ab593480, 1:700), anti-Bax (ab53154, 1:1000), anti-Bak (ab32371, 1:10,000) purchased from Abcam. E-cadherin (3195, 1:1000), anti-p-Akt (Thr308) (13,038, 1:1000), p-JNK1/2(4668, 1:2000), anti-GAPDH (5174, 1:1000), anti-β-actin (4970, 1:1000) purchased from Cell Signaling Technology.
Statistics
Student’s t-tests or one-way analysis of variance (ANOVA) was performed to analyze the differences among groups. P < 0.05 was considered statistically significant. The statistical analysis were conducted using GraphPad Prism 5.0 software (GraphPad Software, Inc., La Jolla, CA, USA).
Results
The expressions of miR-144-3p and PAX8 in patients diagnosed with PTC
The expressions of miR-144-3p and PAX8 in tumor and the corresponding normal tissues were detected first. The RT-PCR results showed that compared to those in normal tissues, in tumor tissues the expression of miR-144-3p was increased but PAX8 expression was dropped (P < 0.001, Fig. 1a–d). The protein levels of PAX8 in 8 randomly selected PTC patients were examined by Western blot. The results showed that the expression of PAX8 was blocked at the translational level (P < 0.001, Fig. 1e–f), and that the distribution of PAX8 reduced in PTC tissues compared to that of the normal tissues (P < 0.05, Fig. 2a, b).
Fig. 1.
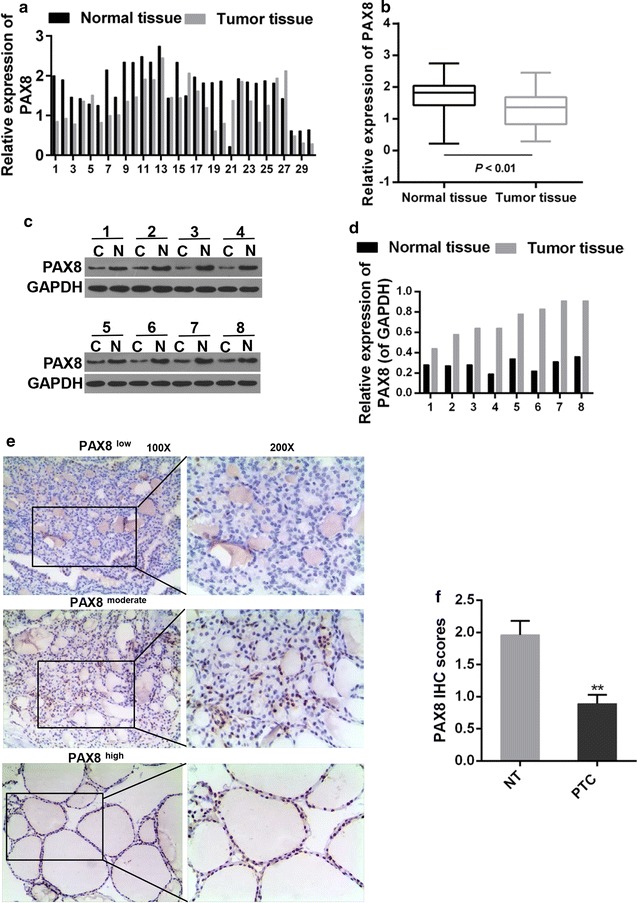
a Quantitative analysis was applied for expression level of PAX8 in cancer and adjacent normal tissues. b Paired T test was adopted for PAX8 expression between cancer and normal tissues. ***P < 0.001. c, d Western blot was used for PAX8 expression in 8 randomly selected patients out of the 30 matched initial samples. C, cancer tissues; N, normal tissues (e, f) IHC analysis for the distribution of PAX8. **P < 0.01 vs. NT. NT normal tissue, PTC cancer tissue
Fig. 2.
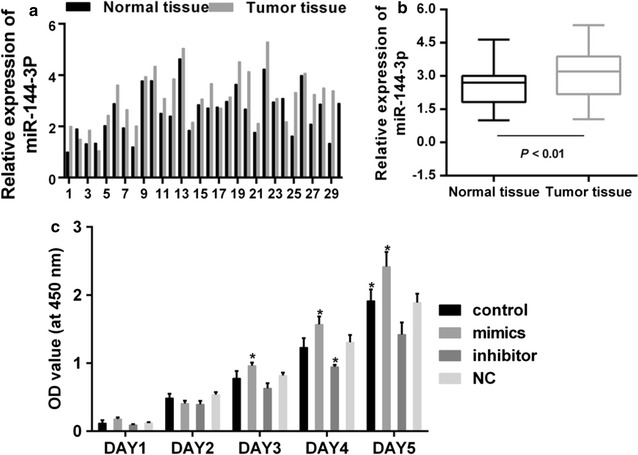
a Quantitative analysis was performed for expression level of miR-144-3p in cancer and adjacent normal tissues. b Paired T test was carried out for miR-144-3p expression between cancer and normal tissues. ***P < 0.001. c Cell viability of PTC cells. *P < 0.05 vs. control
MiR-144-3p inhibitors reduced proliferation and induced cell cycle arrest of PTC cells
Un-controlled growth is a typical character of tumor cells. The cells were treated and grouped as follows: Control, untreated PTC cells; mimics, PTC cells transfected with miR-144-3p mimics; inhibitor: PTC cells transfected with miR-144-3p inhibitors; NC, PTC cells transfected with miRNA negative control. The CCK-8 assay result indicated that the increased expression of miR-144-3p augmented the cell viability of PTC cells, while its suppressed expression reduced the cell viability (Fig. 2c). Researchers pointed out that the cell proliferation was largely dependent on the normal progression of cell cycle [25], therefore, the cell cycle progression was tested (Fig. 3a, b). The results from our tested showed that in miR-144-3p inhibitor group the cell populations at G1 phase increased significantly but decreased largely at G2/M, if being compared to control group. The proportion of cell in S phase was less in miR-144-3p inhibitor group than that those in control group. However, the effect of miR-144-3p mimics was the opposite, although no significant differences was observed. The expression of cell-cycle-related proteins, including CDK2, CDC25A and cycline D1, were also determined. Noticeably, the mRNA and protein expression of these factors was increased by miR-144-3p mimics but decreased by inhibitor (Fig. 3c, d).
Fig. 3.
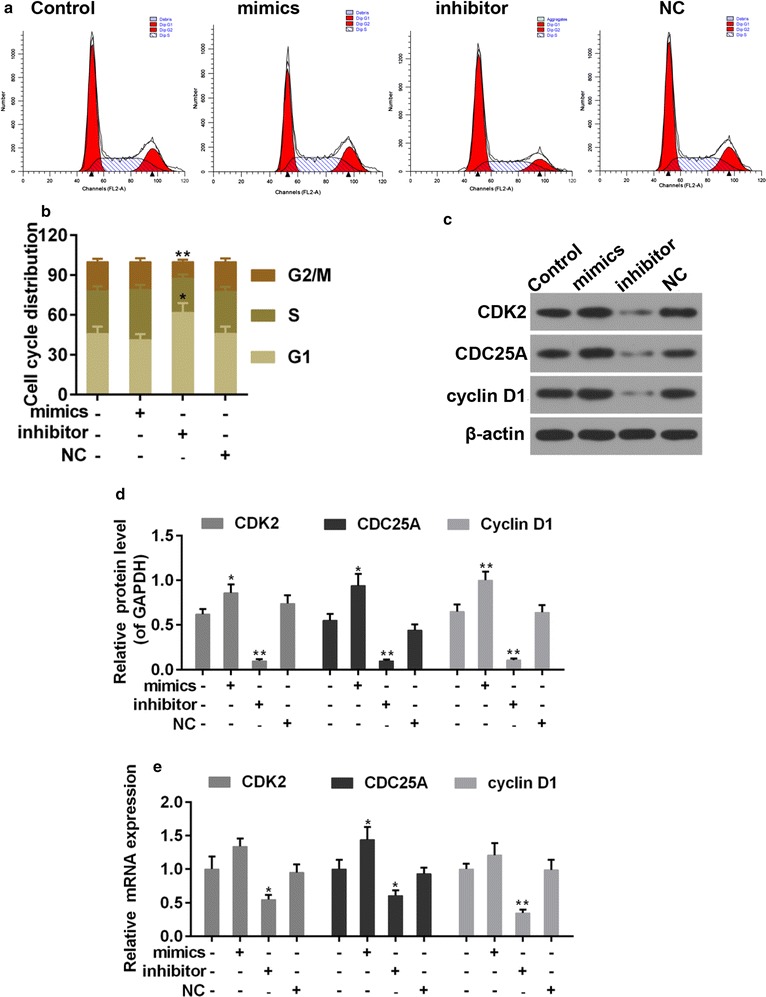
a, b Flow cytometry analysis was applied for cell cycle distribution. c, d Western blot was used for expression of CDK2, CDC25A and cyclin D1. e Quantitative analysis was used for expression of CDK2, CDC25A and cyclin D1. *P < 0.05 and **P < 0.01 vs. control
MiR-144-3p modulated the expression of metastasis associated proteins in PTC cells
Another feature of cancer cells is the ability of metastasis. Epithelial-mesenchymal transition (EMT) is a primary mechanism responsible for metastasis, which is accompanied with the acquirement of mesenchymal phenotypes and the loss of cell polarity. E-cadherin, N-cadherin and vimentin are the proteins participate in EMT [26]. Thus, we applied RT-PCR and Western blot assays to analyse the expressions of EMT-associated proteins (Fig. 4a–c). Data showed that the expression of E-cadherin was reduced by miR-144-3p, while the expressions of N-cadherin and vimentin were increased by miR-144-3p. By contrast, the expressions of E-cadherin, N-cadherin and vimentin in miR-144-3p inhibitor group were reversed.
Fig. 4.
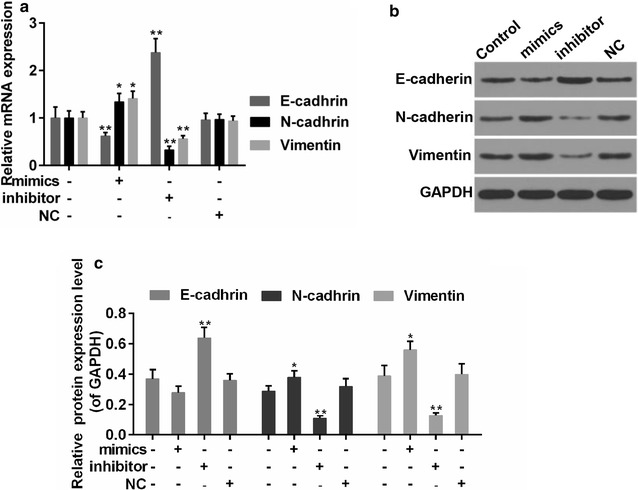
a Quantitative analysis was performed for expression of E-cadherin, N-cadherin, and vimentin. b, c Western blot analysis was carried out for E-cadherin, N-cadherin, and vimentin. *P < 0.05 and **P < 0.01 vs. control
PAX8 was a potential direct target of miR-144-3p
To understand the mechanisms that underlie the effect of miR-144-3p on PTC cells, the available database TargetScan was adopted to help predict the potential target of miR-144-3p. The data suggested that there were possible binding sites of miR-144-3p in the 3′UTR region of PAX8 (Fig. 5a). Thus, luciferase reporter assay was performed to confirm such a prediction. The transfection of miR-144-3p mimic and its inhibitors was effective in PTC cells (Fig. 5b). Moreover, the luciferase activity of PAX8-3′UTR was markedly inhibited by over-expression of miR-144-3p. Nevertheless, the luciferase activity of PAX8-3′UTR-mut was not affected (Fig. 5c). Furthermore, while miR-144-3p inhibitors enhanced the luciferase activity of PAX8-3′UTR, it produced no effect on that of PAX8-3′UTR-mut (Fig. 5d). To further confirm the effect of miR-144-3p on the translation of PAX8, the expression of PAX8 was determined in the presence of miR-144-3p or the miR-144-3p inhibitors. We observed that the mRNA and protein levels of PAX8 were decreased and forced by miR-144-3p mimics and inhibitors, respectively (Fig. 5e–g).
Fig. 5.
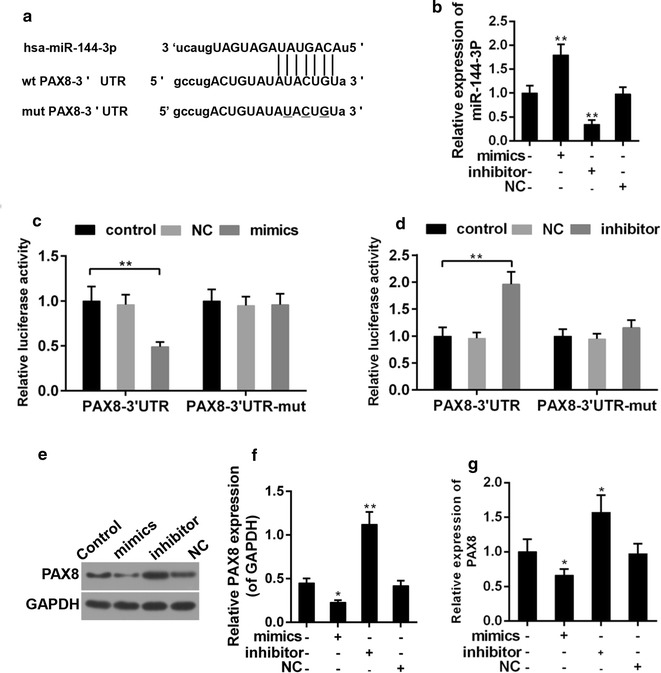
a The prediction binding sequence of miR-144-3p in PAX8 mRNA 3′-UTR. wt: wild-type; mut: mutated. b Transfection efficiency of miR-144-3p mimics and inhiitors. c, d Relative luciferase activity of TLR4 mRNA 3′-UTR after transfection with miR-144-3p mimics or inhiitors. **P < 0.01. e, f The effect of miR-144-3p on the protein expression of PAX8. **P < 0.01 vs. control. g The effect of miR-144-3p on the mRNA expression of PAX8. **P < 0.01 vs. control
MiR-144-3p suppressed the activity of ERK1/2, Akt and JNK signals
The activities of ERK1/2, Akt and JNK were studied in order to further investigate the underlying molecular mechanism. The results showed that the phosphorylation of these signal proteins was enhanced in the presence of miR-144-3p but otherwise declined in the absence of miR-144-3p (Fig. 6a–c).
Fig. 6.
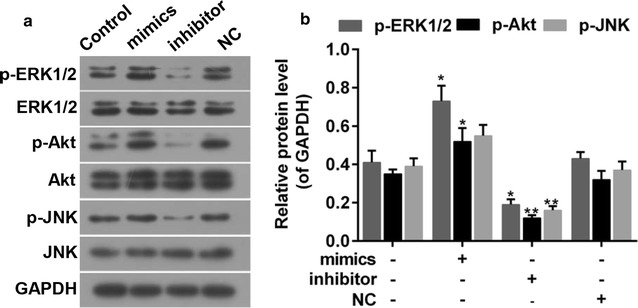
a, b The effect of miR-144-3p on the activations of ERK1/2, Akt and JNK signals. *P < 0.05 and **P < 0.01 vs. control
Down-regulation of miR-144-3p enhanced the effect of X-ray exposure and paclitaxel in PTC cells
X-ray irradiation and paclitaxel are common options for the treatment of cancer. To further confirm the effect of miR-144-3p on PTC, the apoptosis rate of PTC cells, which were treated with appropriate X-ray or paclitaxel, was examined in the presence and absence of miR-144-3p. Our experiment observed that in both the X-ray exposure and paclitaxel treatment group (Fig. 7a–d), apoptosis was depressed by miR-144-3p but induced by its inhibitors. The transfection efficiency of miRNA was demonstrated (Fig. 7e–f). We also found that the expression of PAX8 was inhibited after the transfection of miR-144-3p, and that the expressions of pro-apoptotic proteins, Bax and BAK, were increased by miR-144-3p inhibitors. However, the anti-apoptotic protein, Bcl-2 was depressed in miR-144-3p inhibitor group (Fig. 8a–f). Thus, the down-regulation of miR-144-3p synergistically enhanced the anti-tumor effect of X-ray exposure and paclitaxel.
Fig. 7.
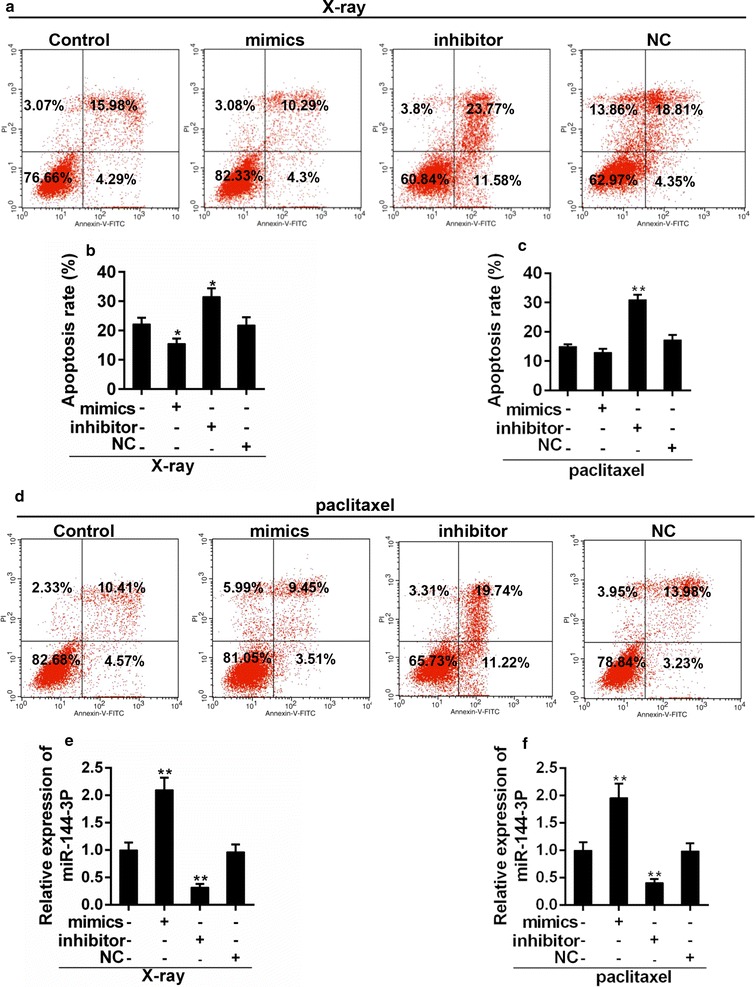
a, b Flow cytometry analysis for apoptosis of PTC cells treated with X-ray and miR-144-3p. *P < 0.05 vs. control. c, d Flow cytometry analysis was carried out for apoptosis of PTC cells that were treated with paclitaxel and miR-144-3p. **P < 0.01 vs. control. e, f Transfection efficiency of miR-144-3p mimics and inhiitors in PTC cells that were treated with X-ray (e) or paclitaxel (f). **P < 0.01 vs. control
Fig. 8.
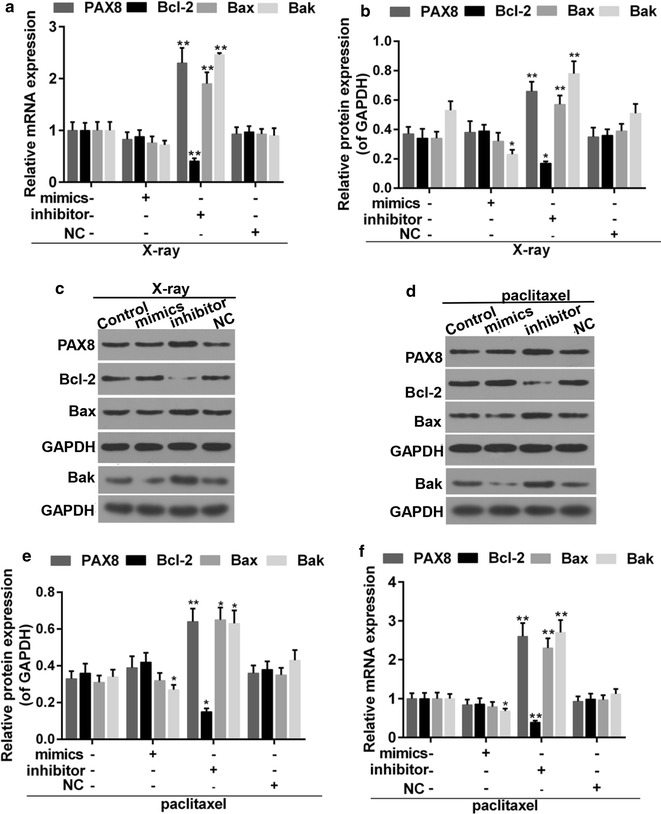
a Quantitative analysis was carried out for expressions of PAX8, Bax, Bcl-2 and Bak in PTC cells that were treated with X-ray and miR-144-3p. b, c Western blot was performed for expression of PAX8, Bax Bcl-2 and Bak. d, e Western blot was used for expressions of PAX8, Bax Bcl-2 and Bak in PTC cells that were treated with paclitaxel and miR-144-3p. f Quantitative analysis was performed for expression of PAX8, Bax Bcl-2 and Bak. *P < 0.05, **P < 0.01 vs. control
Discussion
Accurate stratification and prognostic evaluation play critical roles in terms of reducing the occurrence of PTC. The use of immunohistochemical stains may enhance the diagnostic sensitivity of PTC in cells from thyroid fine-needle aspiration [27]. PAX8 is important and indispensable in the thyroid development. Increased expression of PAX8 was observed in ovarian cancer, bladder, prostate and endometrial carcinomas [28], however, its reduced expression was found in thyroid organogenesis [29]. The study proved the decreased expression of PAX8 both in the transcriptional and translational levels in patients diagnosed with PTC. As a transcriptional factor, the expression of PAX8 target genes in PTC have been studied [30]. Although this study enriches the understanding of the mechanisms that take part in thyroid tumorigenesis, to investigate the upstream regulator of PAX8 may be more urgent and effective in combating t the reoccurrence of PTC.
MiRNAs have been observed participating in the progressive event that associated with complex gene expression and regulation [31]. More and more researchers are interested in studying the role of miR-144-3p in cancer development and treatment. It has reported that the expression of miR-144-3p was depressed in several cancers, such as CRC, OS and NSCLC [17–20]. However, the effect of miR-144-3p on PTC varies from cancers to cancers. In this study, the expression of miR-144-3p showed an increased trend in PTC patients. Such a phenomenon was in line with the up-regulation of miR-144-3p in Clear cell renal cell carcinoma [32]. It was indicated miR-144-3p may have positive role in the PTC carcinogenesis. Results from CCK-8 assay were consistent with this speculation. Unlimited proliferation is a hallmark of cancer, which is caused by the aberrant cell cycle progression [25]. G1/S transition is regarded as a key step during cell cycle, and it promotes cell proliferation [33]. Our results showed that miR-144-3p promoted G1/S transition, however, miR-144-3p inhibitor induced G1/S transition arrest. Cyclins and cyclin-dependent kinases (CDKs) are the important regulatory proteins during cell cycle progression, in which progress CDK2 and cyclin D1 are involved. CDC25A is also able to control G1/S and G2/M transition [34]. Thus, we went further to determine the expression of these transition regulators in order to investigate the cell cycle promotion effect of miR-144-3p. The results revealed that the expression of cyclin D1, CDK2 and CDC25A was forced by miR-144-3p mimics but alleviated by inhibitors. Researches reported that EMT was related to tumor metastasis [35, 36]. The over-expression of miR-144-3p facilitated EMT, which is a consequence of the up-regulation of mesenchymal markers (N-cadherin, and vimentin) and down-regulation of epithelial marker (E-cadherin). Thus, we concluded that miR-144-3p was positive to promote the tumorgenesis of PTC. However, studies have indicated the anti-tumor function of miR-144-3p [37–39]. The distinct effect of miR-144-3p may vary dependent on cell context and microenvironments around.
Luciferase reporter assay was carried out To explore the mechanisms that underlie the role of miR-144-3p in PTC. The results suggested that miR-144-3p repressed the activity of 3′UTR-PAX8, which was enhanced by miR-144-3p inhibitors. In addition, the expression of PAX8 was repressed by miR-144-3p. The results demonstrated that PAX8 expression may be directly regulated by miR-144-3p. Accordingly, miR-144-3p may be a candidate to prevent PTC. To a large extent, biological events are the consequences of signal transduction. ERK1/2, Akt and JNK have been reported by previous studies due to their important roles in living cells, including in cancer cells [40, 41]. Our findings showed that to suppress these signals was at least partly related to the mechanism via which miR-144-3p forced the progression of PTC. The activation of Erk1/2, JNK has been reported in prostate cancer and colon cancer [42, 43], and the activation of ERK1/2 and Akt and inactivation of JNK were found in lung cancer [44]. These findings implied the complexity of the signal cascades in carcinogenesis.
To further test the effect of miR-144-3p, the treatment model was set up in vitro. The cluster formations of Bax and Bak could be induced upon apoptosis stimuli, which exerts pro-apoptotic effect [45]. Bcl-2 is considered as an anti-apoptotic factor [46]. We found that miR-144-3p inhibitor increased the expression of Bax/Bak but decreased the expression of Bcl-2. Such an observation suggested that the the treatment in combination with miR-144-3p inhibitor promoted the sensitivity to apoptosis of PTC,if being compared to treatment with the use of X-ray or paclitaxel only. These results strongly indicated the tumor-promoting function of mir-144-3p and its potential clinical significance in the treatment of PTC. Thus, to continue the studies in vivo should be encouraged.
The sample size of the PTC patients was another limitation of this study. Investigation with larger-scale samples would be more convincing and closer to the reality. In addition, exploring, ipso facto, the regulation mechanisms between miR-144-3p and the signal cascades (ERK1/2, Akt and JNK) was beneficial in understanding the accuracy molecular events that happened during the progression of PTC.
Conclusion
The current study unveiled the tumor-promoting effect of miR-144-3p in PTC mainly through promoting cell cycle progression and EMT. Our findings also suggested that PAX8 may be a direct target of miR-144-3p, and that the effect of miR-144-3p may be partially related to the activations of ERK1/2, Akt and JNK signals. In addition, the blockage of miR-144-3p could synergistically force the effect of X-ray exposure and paclitaxel. To conclude, this study provided promising prognosis markers and valuable treatment strategy for PTC.
Authors’ contributions
CL wrote the main manuscript. CL and CS performed the experiments. GL designed the study. CS and YC performed data analysis. All authors contributed to manuscript revisions. All authors read and approved the final manuscript.
Acknowledgements
None.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Chang Liu, Email: Liuchang_LC01@163.com.
Chang Su, Email: Suchang_CS22@163.com.
Yanchun Chen, Email: Yanchun_Chen_YCS@163.com.
Guang Li, Phone: 86-024-961200, Email: Guangli_GL11@163.com.
References
- 1.Sherman SI. Thyroid carcinoma. Lancet. 2003;361(9356):501–511. doi: 10.1016/S0140-6736(03)12488-9. [DOI] [PubMed] [Google Scholar]
- 2.Dinets A, Hulchiy M, Sofiadis A, Ghaderi M, Hoog A, Larsson C, Zedenius J. Clinical, genetic, and immunohistochemical characterization of 70 Ukrainian adult cases with post-Chornobyl papillary thyroid carcinoma. Eur J Endocrinol. 2012;166(6):1049–1060. doi: 10.1530/EJE-12-0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xing M. BRAF mutation in papillary thyroid cancer: pathogenic role, molecular bases, and clinical implications. Endocr Rev. 2007;28(7):742–762. doi: 10.1210/er.2007-0007. [DOI] [PubMed] [Google Scholar]
- 4.Walther C, Guenet JL, Simon D, Deutsch U, Jostes B, Goulding MD, Plachov D, Balling R, Gruss P. Pax: a murine multigene family of paired box-containing genes. Genomics. 1991;11(2):424–434. doi: 10.1016/0888-7543(91)90151-4. [DOI] [PubMed] [Google Scholar]
- 5.Nonaka D, Tang Y, Chiriboga L, Rivera M, Ghossein R. Diagnostic utility of thyroid transcription factors Pax8 and TTF-2 (FoxE1) in thyroid epithelial neoplasms. Mod Pathol. 2008;21(2):192–200. doi: 10.1038/modpathol.3801002. [DOI] [PubMed] [Google Scholar]
- 6.Lacroix L, Mian C, Barrier T, Talbot M, Caillou B, Schlumberger M, Bidart JM. PAX8 and peroxisome proliferator-activated receptor gamma 1 gene expression status in benign and malignant thyroid tissues. Eur J Endocrinol. 2004;151(3):367–374. doi: 10.1530/eje.0.1510367. [DOI] [PubMed] [Google Scholar]
- 7.Arturi F, Russo D, Bidart JM, Scarpelli D, Schlumberger M, Filetti S. Expression pattern of the pendrin and sodium/iodide symporter genes in human thyroid carcinoma cell lines and human thyroid tumors. Eur J Endocrinol. 2001;145(2):129–135. doi: 10.1530/eje.0.1450129. [DOI] [PubMed] [Google Scholar]
- 8.Ros P, Rossi DL, Acebron A, Santisteban P. Thyroid-specific gene expression in the multi-step process of thyroid carcinogenesis. Biochimie. 1999;81(4):389–396. doi: 10.1016/S0300-9084(99)80086-8. [DOI] [PubMed] [Google Scholar]
- 9.Raman P, Koenig RJ. Pax-8-PPAR-gamma fusion protein in thyroid carcinoma. Nat Rev Endocrinol. 2014;10(10):616–623. doi: 10.1038/nrendo.2014.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Axtell MJ, Bartel DP. Antiquity of microRNAs and their targets in land plants. Plant Cell. 2005;17(6):1658–1673. doi: 10.1105/tpc.105.032185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tanzer A, Stadler PF. Molecular evolution of a microRNA cluster. J Mol Biol. 2004;339(2):327–335. doi: 10.1016/j.jmb.2004.03.065. [DOI] [PubMed] [Google Scholar]
- 12.Guo H, Ingolia NT, Weissman JS, Bartel DP. Mammalian microRNAs predominantly act to decrease target mRNA levels. Nature. 2010;466(7308):835–840. doi: 10.1038/nature09267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Calin GA, Ferracin M, Cimmino A, Di Leva G, Shimizu M, Wojcik SE, Iorio MV, Visone R, Sever NI, Fabbri M, et al. A MicroRNA signature associated with prognosis and progression in chronic lymphocytic leukemia. N Engl J Med. 2005;353(17):1793–1801. doi: 10.1056/NEJMoa050995. [DOI] [PubMed] [Google Scholar]
- 14.Esquela-Kerscher A, Slack FJ. Oncomirs—microRNAs with a role in cancer. Nat Rev Cancer. 2006;6(4):259–269. doi: 10.1038/nrc1840. [DOI] [PubMed] [Google Scholar]
- 15.Boufraqech M, Zhang L, Jain M, Patel D, Ellis R, Xiong Y, He M, Nilubol N, Merino MJ, Kebebew E. miR-145 suppresses thyroid cancer growth and metastasis and targets AKT3. Endocr Relat Cancer. 2014;21(4):517–531. doi: 10.1530/ERC-14-0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carvalheira G, Nozima BH, Cerutti JM. microRNA-106b-mediated down-regulation of C1orf24 expression induces apoptosis and suppresses invasion of thyroid cancer. Oncotarget. 2015;6(29):28357–28370. doi: 10.18632/oncotarget.4947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iwaya T, Yokobori T, Nishida N, Kogo R, Sudo T, Tanaka F, Shibata K, Sawada G, Takahashi Y, Ishibashi M, et al. Downregulation of miR-144 is associated with colorectal cancer progression via activation of mTOR signaling pathway. Carcinogenesis. 2012;33(12):2391–2397. doi: 10.1093/carcin/bgs288. [DOI] [PubMed] [Google Scholar]
- 18.Zha W, Cao L, Shen Y, Huang M. Roles of Mir-144-ZFX pathway in growth regulation of non-small-cell lung cancer. PLoS ONE. 2013;8(9):e74175. doi: 10.1371/journal.pone.0074175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Namlos HM, Meza-Zepeda LA, Baroy T, Ostensen IH, Kresse SH, Kuijjer ML, Serra M, Burger H, Cleton-Jansen AM, Myklebost O. Modulation of the osteosarcoma expression phenotype by microRNAs. PLoS ONE. 2012;7(10):25. doi: 10.1371/journal.pone.0048086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katayama Y, Maeda M, Miyaguchi K, Nemoto S, Yasen M, Tanaka S, Mizushima H, Fukuoka Y, Arii S, Tanaka H. Identification of pathogenesis-related microRNAs in hepatocellular carcinoma by expression profiling. Oncol Lett. 2012;4(4):817–823. doi: 10.3892/ol.2012.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanteti R, El-Hashani E, Dhanasingh I, Tretiakova M, Husain AN, Sharma S, Sharma J, Vokes EE, Salgia R. Role of PAX8 in the regulation of MET and RON receptor tyrosine kinases in non-small cell lung cancer. BMC Cancer. 2014;14:185. doi: 10.1186/1471-2407-14-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diao WL, Luo L, Luo Q. Effect of X-ray irradiation on epithelial-mesenchymal transition of colorectal cancer SW480 cells. J Biol Regul Homeost Agents. 2016;30(2):553–558. [PubMed] [Google Scholar]
- 23.Li R, Moudgil T, Ross HJ, Hu HM. Apoptosis of non-small-cell lung cancer cell lines after paclitaxel treatment involves the BH3-only proapoptotic protein Bim. Cell Death Differ. 2005;12(3):292–303. doi: 10.1038/sj.cdd.4401554. [DOI] [PubMed] [Google Scholar]
- 24.Arocho A, Chen B, Ladanyi M, Pan Q. Validation of the 2− ΔΔCt calculation as an alternate method of data analysis for quantitative PCR of BCR-ABL P210 transcripts. Diagn Mol Pathol. 2006;15(1):56–61. doi: 10.1097/00019606-200603000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Evan GI, Vousden KH. Proliferation, cell cycle and apoptosis in cancer. Nature. 2001;411(6835):342–348. doi: 10.1038/35077213. [DOI] [PubMed] [Google Scholar]
- 26.Zavadil J, Haley J, Kalluri R, Muthuswamy SK, Thompson E. Epithelial-mesenchymal transition. Cancer Res. 2008;68(23):9574–9577. doi: 10.1158/0008-5472.CAN-08-2316. [DOI] [PubMed] [Google Scholar]
- 27.Nga ME, Lim GS, Soh CH, Kumarasinghe MP. HBME-1 and CK19 are highly discriminatory in the cytological diagnosis of papillary thyroid carcinoma. Diagn Cytopathol. 2008;36(8):550–556. doi: 10.1002/dc.20841. [DOI] [PubMed] [Google Scholar]
- 28.Sharma R, Sanchez-Ferras O, Bouchard M. Pax genes in renal development, disease and regeneration. Semin Cell Dev Biol. 2015;44:97–106. doi: 10.1016/j.semcdb.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 29.Puglisi F, Cesselli D, Damante G, Pellizzari L, Beltrami CA, Di Loreto C. Expression of Pax-8, p53 and bcl-2 in human benign and malignant thyroid diseases. Anticancer Res. 2000;20(1A):311–316. [PubMed] [Google Scholar]
- 30.Rosignolo F, Sponziello M, Durante C, Puppin C, Mio C, Baldan F, Di Loreto C, Russo D, Filetti S, Damante G. Expression of PAX8 target genes in papillary thyroid carcinoma. PLoS ONE. 2016;11(6):e0156658. doi: 10.1371/journal.pone.0156658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Rooij E, Kauppinen S. Development of microRNA therapeutics is coming of age. EMBO Mol Med. 2014;6(7):851–864. doi: 10.15252/emmm.201100899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lou N, Ruan AM, Qiu B, Bao L, Xu YC, Zhao Y, Sun RL, Zhang ST, Xu GH, Ruan HL, et al. miR-144-3p as a novel plasma diagnostic biomarker for clear cell renal cell carcinoma. Urol Oncol. 2017;35(1):12. doi: 10.1016/j.urolonc.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 33.Flemington EK, Speck SH, Kaelin WG., Jr E2F-1-mediated transactivation is inhibited by complex formation with the retinoblastoma susceptibility gene product. Proc Natl Acad Sci USA. 1993;90(15):6914–6918. doi: 10.1073/pnas.90.15.6914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang JD, Levin PA. Metabolism, cell growth and the bacterial cell cycle. Nat Rev Microbiol. 2009;7(11):822–827. doi: 10.1038/nrmicro2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Du R, Wu S, Lv X, Fang H, Wu S, Kang J. Overexpression of brachyury contributes to tumor metastasis by inducing epithelial-mesenchymal transition in hepatocellular carcinoma. J Exp Clin Cancer Res. 2014;33(1):105. doi: 10.1186/s13046-014-0105-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yoshida GJ. Emerging role of epithelial-mesenchymal transition in hepatic cancer. J Exp Clin Cancer Res. 2016;35(1):141. doi: 10.1186/s13046-016-0419-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pan H-L, Wen Z-S, Huang Y-C, Cheng X, Wang G-Z, Zhou Y-C, Wang Z-Y, Guo Y-Q, Cao Y, Zhou G-B. Down-regulation of microRNA-144 in air pollution-related lung cancer. Sci Rep. 2015;5:14331. doi: 10.1038/srep14331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang SY, Lu ZM, Lin YF, Chen LS, Luo XN, Song XH, Chen SH, Wu YL. miR-144-3p, a tumor suppressive microRNA targeting ETS-1 in laryngeal squamous cell carcinoma. Oncotarget. 2016;7(10):11637–11650. doi: 10.18632/oncotarget.7025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lan F, Yu H, Hu M, Xia T, Yue X. miR-144-3p exerts anti-tumor effects in glioblastoma by targeting c-Met. J Neurochem. 2015;135(2):274–286. doi: 10.1111/jnc.13272. [DOI] [PubMed] [Google Scholar]
- 40.Yacoub A, Gupta P, Park MA, Rhamani M, Hamed H, Hanna D, Zhang G, Sarkar D, Lebedeva IV, Emdad L, et al. Regulation of GST-MDA-7 toxicity in human glioblastoma cells by ERBB1, ERK1/2, PI3K, and JNK1-3 pathway signaling. Mol Cancer Ther. 2008;7(2):314–329. doi: 10.1158/1535-7163.MCT-07-2150. [DOI] [PubMed] [Google Scholar]
- 41.Brand S, Olszak T, Beigel F, Diebold J, Otte J-M, Eichhorst ST, Göke B, Dambacher J. Cell differentiation dependent expressed CCR6 mediates ERK-1/2, SAPK/JNK, and Akt signaling resulting in proliferation and migration of colorectal cancer cells. J Cell Biochem. 2006;97(4):709–723. doi: 10.1002/jcb.20672. [DOI] [PubMed] [Google Scholar]
- 42.Caron RW, Yacoub A, Mitchell C, Zhu X, Hong Y, Sasazuki T, Shirasawa S, Hagan MP, Grant S, Dent P. Radiation-stimulated ERK1/2 and JNK1/2 signaling can promote cell cycle progression in human colon cancer cells. Cell Cycle. 2005;4(3):456–464. doi: 10.4161/cc.4.3.1249. [DOI] [PubMed] [Google Scholar]
- 43.Uzgare AR, Kaplan PJ, Greenberg NM. Differential expression and/or activation of P38MAPK, erk1/2, and jnk during the initiation and progression of prostate cancer. Prostate. 2003;55(2):128–139. doi: 10.1002/pros.10212. [DOI] [PubMed] [Google Scholar]
- 44.Chen JH, Lin SS, Wang WX, Yuan ST, Shi JS, Jia AQ. The extract, LXB-1, from the barks of Liriodendron× hybrid, induced apoptosis via Akt, JNK and ERK1/2 pathways in A549 lung cancer cells. Z Naturforsch C. 2015;70(11–12):305–311. doi: 10.1515/znc-2015-0126. [DOI] [PubMed] [Google Scholar]
- 45.Nasu Y, Benke A, Arakawa S, Yoshida GJ, Kawamura G, Manley S, Shimizu S, Ozawa T. In situ characterization of bak clusters responsible for cell death using single molecule localization microscopy. Sci Rep. 2016;6:27505. doi: 10.1038/srep27505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muhammad EM, Ahmad AN, Guirguis MN, Ali AEM. Evaluation of immunohistochemical anti-apoptotic Bcl-2 and pro-apoptotic Bax gene products in breast carcinoma. Egypt J Med Sci. 2009;30(2):1199–1227. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.


