Abstract
Background and Aims:
The synergism between epidural local anesthetic agent and opioids is well established, but evidence for the combination of local anesthetic agent with dexmedetomidine in epidurals is limited. This study evaluates the clinical efficacy of dexmedetomidine versus fentanyl as an additive to ropivacaine for epidural anesthesia.
Material and Methods:
Patients undergoing infraumbilical surgeries were divided randomly into three groups - Group R (n = 25): received 18 ml of 0.5% ropivacaine for epidural anesthesia and 10 ml of 0.1% ropivacaine boluses for postoperative analgesia; Group RF (n = 25): received 18 ml of 0.5% ropivacaine with 20 μg fentanyl for epidural anesthesia and 10 ml of 0.1% ropivacaine with 10 μg fentanyl boluses for postoperative analgesia; and Group RD (n = 25): received 18 ml of 0.5% ropivacaine with 10 μg dexmedetomidine for epidural anesthesia and 10 ml of 0.1% ropivacaine with 5 μg dexmedetomidine boluses for postoperative analgesia.
Results:
The mean time for onset of sensory block, in minutes, was 18.6 ± 4.4 in R Group, 12.8 ± 1.8 in RF Group and 10.8 ± 2.7 in RD Group (P < 0.001). There was a statistically significant difference with regard to degree of motor block, with RD Group faring better than RF Group and R Group. The mean time to rescue analgesia, in minutes, was 139.8 ± 21.4 in Group R, 243 ± 29.7 in Group RF, and 312.4 ± 30.2 in Group RD (P < 0.001). Incidence of hypotension at 10 min was 4% and 48% in RF and RD Groups, respectively (P < 0.001).
Conclusions:
Epidural anesthesia achieved with 10 μg dexmedetomidine as an additive to 0.5% ropivacaine is more effective with respect to duration and intensity of analgesia when compared to 0.5% ropivacaine alone or addition of 20 μg fentanyl to 0.5% ropivacaine.
Keywords: Dexmedetomidine, epidural anesthesia, ropivacaine
Introduction
Epidural anesthesia with local anesthetics is performed for providing intraoperative surgical anesthesia and postoperative analgesia. Ropivacaine, when used for epidural anesthesia, requires higher doses than bupivacaine, but adjuvants decrease its dose and side effects. Fentanyl, when added to ropivacaine in epidural, confers better analgesia and lesser systemic toxicity.[1] However, the addition of opioids to local anesthetics has disadvantages of pruritus and respiratory depression. Dexmedetomidine, an alpha-2 adrenoreceptor agonist, acts on the spinal cord and has been used as an effective adjuvant to ropivacaine for regional and central neuraxial blocks.[2] This study evaluates the effect of addition of fentanyl or dexmedetomidine to ropivacaine for epidural anesthesia and analgesia and also compares the adverse effects.
Material and Methods
This prospective randomized study was conducted with the consent of Hospital Ethical Committee. Written and informed consent, after explaining the effects of drugs being used, was obtained from the patients, for their participation in the study. Patients of both sexes, with American Society of Anesthesiologists (ASA) physical status I or II, between 18 and 60 years, who underwent infraumbilical surgeries such as lower abdominal, lower limb, gynecological, and urogenital surgeries, were included in the study. Patients refusing consent and patients with coagulopathy, spinal deformity, infection at the puncture site, allergy to local anesthetics, and morbid obesity were excluded from the study.
The patients, who consented, were divided into three groups, by allocating them a random number by a computer-generated table. Seventy-five patients were allocated into one of the three groups:
Group R (n = 25): Received 18 ml of 0.5% ropivacaine for epidural anesthesia and 10 ml of 0.1% ropivacaine boluses for postoperative analgesia
Group RF (n = 25): Received 18 ml of 0.5% ropivacaine with 20 μg fentanyl for epidural anesthesia and 10 ml of 0.1% ropivacaine with 10 μg fentanyl boluses for postoperative analgesia
Group RD (n = 25): Received 18 ml of 0.5% ropivacaine with 10 μg dexmedetomidine for epidural anesthesia and 10 ml of 0.1% ropivacaine with 5 μg dexmedetomidine boluses for postoperative analgesia.
All patients included in the study received 15 ml/kg Ringer lactate solution intravenously. Baseline hemodynamic parameters, heart rate, noninvasive blood pressure, mean arterial pressure (MAP), pulse oximetry, respiratory rate, and temperature were recorded. The patients were administered epidural anesthesia in sitting position with 16-gauge Touhy needle in L2–L3 epidural space, using loss of resistance technique. Epidural catheter was secured 3–5 cm into the epidural space. Confirmation for correct placement of the catheter was done by injecting epidural test dose of 3 ml of 2% lignocaine hydrochloride with adrenaline 1:200,000. The patients were positioned for surgery after 30 min.
The following parameters were documented and analyzed. Onset of sensory blockade at T10 level was noted by sensory loss to temperature by ether-soaked swab and painful stimuli by pinprick. Time to complete motor blockade was noted. Degree of motor blockade was noted using modified Bromage scale from 0 to 3. For quantification of pain, the conventional visual analog scale (VAS) score from 0 to 10 was used. Complications such as bradycardia, hypotension, pruritus, nausea, vomiting, and allergic reaction were documented. Pulse rate <60/min and mean blood pressure <20% of basal value were treated with atropine and intravenous fluids or vasopressors. Mean duration for rescue analgesia was taken as the duration from administration of epidural to the time when the patient recorded a VAS of 4 for pain. Epidural top-ups were given when the VAS score for pain was 4 or more. Repeat top-ups of the same dosage were administered as and when necessary to keep VAS <4. All cases were followed up to 48 h postsurgery, and epidural catheter was then removed.
Statistical analysis
Data were analyzed using IBM® SPSS® Statistics 20 statistical software package, Chi-square tests were applied for categorical variables, and continuous variables were compared using one-way ANOVA test. Data are expressed in terms of mean ± standard deviation (SD). P value was reported at the 95% confidence interval, and P < 0.05 was considered significant. Sample size was calculated based on literature search for variation in studied data. The sample size was calculated using effect size of 5 and SD of 6 with alpha error at 5% and power at 80%. Required sample size was 23 per group, and 25 patients per group were included in the study.
Results
A total of 75 patients were included in the study. The demographic profile, sex, and ASA grade of the three groups were comparable.
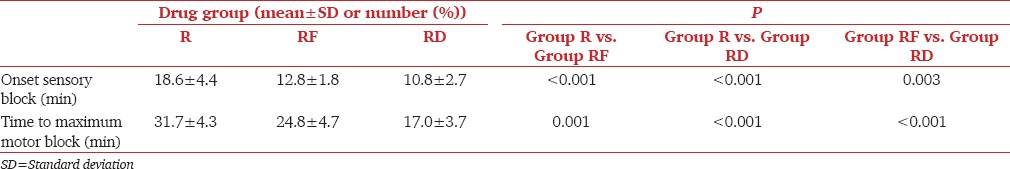
The onset of sensory analgesia and time to complete maximum motor block were significantly faster in RD Group in comparison to R and RF Groups. These times were also faster in Group RF compared to Group R [Table 1].
Table 1.
Onset of sensory block and motor block
Maximum degree of motor blockade was measured by modified Bromage scale. All patients in RD Group reached a modified Bromage of 3. Only 80% of patients in RF Group reached a modified Bromage of 3, and no patient in Group R reached a modified Bromage of 3. Degree of motor block was significantly greater in RF and RD Group compared to R Group, and degree of motor block was significantly greater in RD Group compared to RF Group [Table 2].
Table 2.
Degree of motor block and quality of analgesia
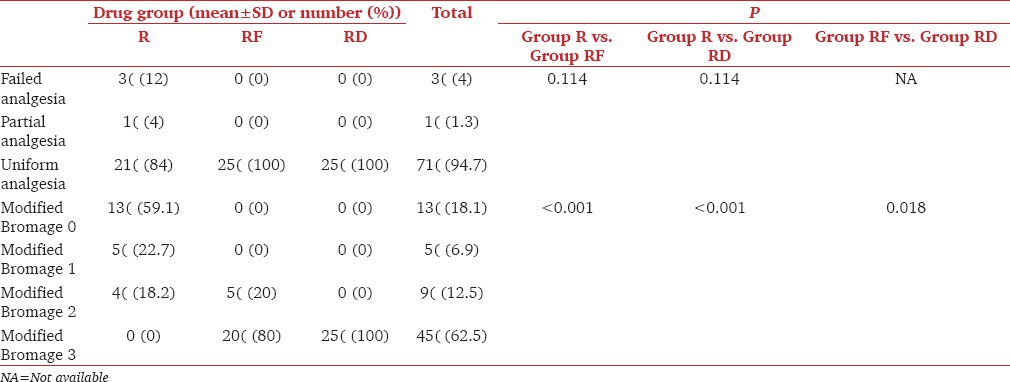
Quality of anesthesia was labeled as “failed” when conversion to general anesthesia was required; “partial” when supplementation with sedation and analgesia was required and “uniform” for complete analgesia and anesthesia. In Group R, there was failed anesthesia in 12% of cases and partial anesthesia in 4% of cases. In RF and RD Groups, there was no failed or partial anesthesia, and all cases achieved “uniform” analgesia and anesthesia. However, this difference was not significant [Table 3].
Table 3.
Mean arterial pressure and heart rate
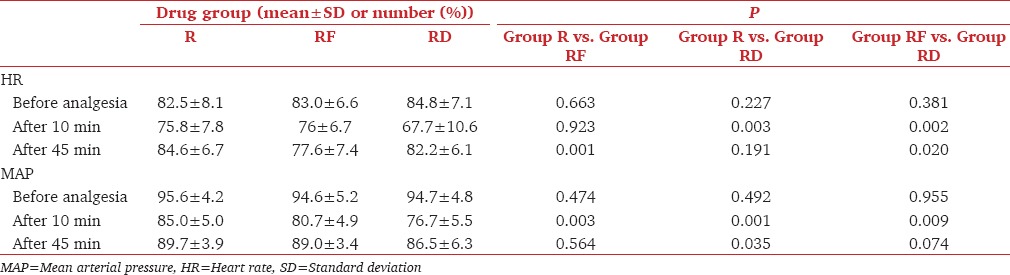
Mean heart rate after 10 min was significantly lower in Group RD when compared with Group R and Group RF. Mean heart rate after 45 min was 84.6 ± 6.7 in Group R, 77.6 ± 7.4 in Group RF, and 82.2 ± 6.1 in Group RD. Mean heart rate after 45 min was significantly lower in Group RF compared to Group R and RD.
MAP after 10 min was significantly lower in RF and RD Groups compared to R Group. It was also significantly lower in RD Group compared to RF Group. There was no statistically significant difference in MAP at 45 min in the three groups [Table 3].
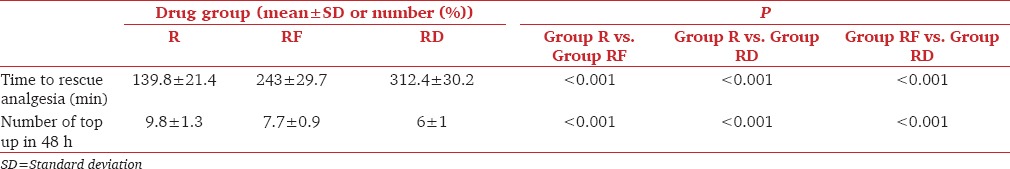
Time to rescue analgesia was significantly longer in RD Group compared to the other two groups. The total number of top-ups was significantly less in RD Group compared to other groups and was also less in RF Group compared to R Group [Table 4].
Table 4.
Time to rescue analgesia and top ups
Incidence of hypotension was significantly higher in Group RD compared to Groups R and RF. There was no statistically significant difference in the incidence of hypotension between R and RF Groups. Bradycardia (HR <60/min) occurred in 40% cases in RD Group, with no cases of bradycardia in R and RF Groups. There was a significantly higher incidence of bradycardia in RD Group compared to the other groups [Table 5].
Table 5.
Complications
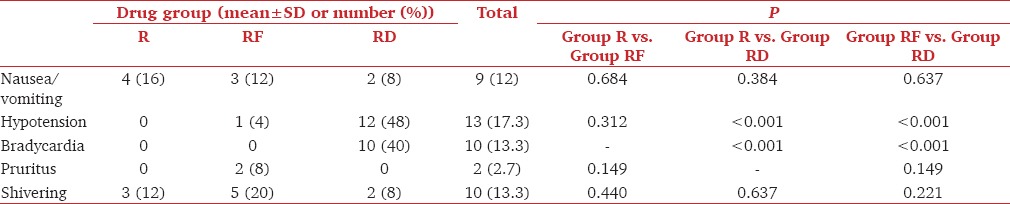
There was no incidence of respiratory depression or hypoxemia in any of the groups. There was no statistically significant difference in the incidence of nausea and vomiting, pruritus, or shivering among these three groups. There were no other complications in any of these three groups [Table 5].
Discussion
The synergism between epidural local anesthetic agents such as ropivacaine and opioids such as fentanyl is well established but evidence regarding combination of local anesthetic agent with dexmedetomidine through epidural route is limited in literature. This study compares the effect of addition of dexmedetomidine and fentanyl to epidural ropivacaine.
Dexmedetomidine is an alpha-2 agonist drug, which has got numerous beneficial effects when used through epidural route. It acts on both presynaptic and postsynaptic nerve terminal in central nervous system by decreasing the sympathetic outflow and norepinephrine release, leading to sedation, anxiolysis, and analgesia. It produces analgesia by depressing the release of C-fiber neurotransmitters and by hyperpolarization of postsynaptic dorsal horn neurons. The prolongation of motor block is the result of binding of alpha-2 adrenergic agonists to the motor neurons in the dorsal horn. Unlike opioids, dexmedetomidine does not cause side effects such as respiratory depression, pruritus, nausea, and vomiting, but it may cause hypotension and bradycardia.[2]
Alpha-2 agonist agents when used as adjuvants have been shown to augment the actions of local anesthetics both in regional blocks and central neuraxial blockade with no adverse neurological effects.[4,5] Some studies have shown synergism between epidural dexmedetomidine and ropivacaine.[6] Dexmedetomidine has been shown to increase sensory and motor block duration during epidural anesthesia with ropivacaine, prolongs postoperative analgesia, and does not cause significant hemodynamic instability.[7] Studies have shown that the addition of alpha-2 agonists to epidural ropivacaine results in longer, complete, and effective analgesia and helps to reduce the dose of epidural ropivacaine for cesarean sections.[8]
Most studies have used dexmedetomidine in dose of 1 μg/kg epidurally as an adjuvant to local anesthetics.[7,9] A pilot study carried out at our center with addition of lower doses of dexmedetomidine ranging from 5 to 20 μg, as adjuvant to local anesthetics intrathecally and epidurally, showed acceptable quality and duration of analgesia with minimal hemodynamic variation. Hence, addition of 10 μg dexmedetomidine was chosen, to compare with 20 μg fentanyl, as an adjuvant to 0.5% ropivacaine epidurally. Studies of intrathecal dexmedetomidine as an additive to local anesthetics have observed a dose-dependent prolongation of sensory block, increase in motor block, along with prolongation of the postoperative analgesia, thus allowing for a decrease in the local anesthetic dose in high-risk group of patients.[10]
In this study, the mean time for onset of sensory block and motor block was significantly shorter with both dexmedetomidine and fentanyl compared to plain ropivacaine. Furthermore, onset of both sensory and motor block was faster with addition of dexmedetomidine to ropivacaine compared to addition of fentanyl. These results were similar with the results of Salgado et al.[6] In this study, without adjuncts, ropivacaine 0.5% epidurally did not result in motor blockade, with 59% of patients having a modified Bromage score of 0. The degree of motor block was complete, with a modified Bromage score of 3, only with addition of either dexmedetomidine or fentanyl to ropivacaine. Motor block achieved with the addition of dexmedetomidine was superior compared to motor block achieved with addition of fentanyl, with all patients having complete motor block. There were cases of “failed” anesthesia cases in plain ropivacaine group; however, with addition of either dexmedetomidine or fentanyl, all patients had “uniform” anesthesia.
There were prolonged postoperative analgesia, lesser need for top-ups, and lesser total dose of postoperative local anesthetic with addition of dexmedetomidine to ropivacaine as compared to fentanyl, and this was similar to the findings in the study by Bajwa et al.[9] Furthermore, the time to rescue analgesia was longer, and the number of top-ups needed in 48 h was lesser with addition of dexmedetomidine, compared to addition of fentanyl.
The incidence of hypotension was significantly more with addition of dexmedetomidine and required treatment with intravenous fluids or vasopressors. MAP fell initially at 10 min with dexmedetomidine, but there was no difference in MAP from the ropivacaine group or the ropivacaine with fentanyl group at 45 min. Hypotension, which occurred, was transient and not severe enough to warrant prolonged treatment. Heart rate fell initially at 10 min with addition of dexmedetomidine, but there was no difference from the ropivacaine group or the ropivacaine with fentanyl group at 45 min. Pruritus, a known side effect of opioids, was higher with the use of fentanyl. Other complications such as nausea, vomiting, and shivering were comparable in all the groups.
Conclusions
Dexmedetomidine and fentanyl as additives to ropivacaine augment the duration and quality of epidural anesthesia and analgesia provided by ropivacaine with 10 μg dexmedetomidine being more effective than 20 μg fentanyl.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Turner G, Scott DA. A comparison of epidural ropivacaine infusion alone and with three different concentration of fentanyl for 72 hours of postoperative analgesia following major abdominal surgery. Reg Anesth. 1998;23:A39. [Google Scholar]
- 2.Grewal A. Dexmedetomidine: New avenues. J Anaesthesiol Clin Pharmacol. 2011;27:297–302. doi: 10.4103/0970-9185.83670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McClellan KJ, Faulds D. Ropivacaine: An update of its use in regional anaesthesia. Drugs. 2000;60:1065–93. doi: 10.2165/00003495-200060050-00007. [DOI] [PubMed] [Google Scholar]
- 4.Marhofer D, Kettner SC, Marhofer P, Pils S, Weber M, Zeitlinger M. Dexmedetomidine as an adjuvant to ropivacaine prolongs peripheral nerve block: A volunteer study. Br J Anaesth. 2013;110:438–42. doi: 10.1093/bja/aes400. [DOI] [PubMed] [Google Scholar]
- 5.Bajwa SJ, Bajwa SK, Kaur J, Singh G, Arora V, Gupta S, et al. Dexmedetomidine and clonidine in epidural anaesthesia: A comparative evaluation. Indian J Anaesth. 2011;55:116–21. doi: 10.4103/0019-5049.79883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salgado PF, Sabbag AT, Silva PC, Brienze SL, Dalto HP, Módolo NS, et al. Synergistic effect between dexmedetomidine and 0.75% ropivacaine in epidural anesthesia. Rev Assoc Med Bras. 2008;54:110–5. doi: 10.1590/s0104-42302008000200011. [DOI] [PubMed] [Google Scholar]
- 7.Kaur S, Attri JP, Kaur G, Singh TP. Comparative evaluation of ropivacaine versus dexmedetomidine and ropivacaine in epidural anesthesia in lower limb orthopedic surgeries. Saudi J Anaesth. 2014;8:463–9. doi: 10.4103/1658-354X.140838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bajwa SJ, Bajwa SK, Kaur J. Comparison of epidural ropivacaine and ropivacaine clonidine combination for elective cesarean sections. Saudi J Anaesth. 2010;4:47–54. doi: 10.4103/1658-354X.65119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bajwa SJ, Arora V, Kaur J, Singh A, Parmar SS. Comparative evaluation of dexmedetomidine and fentanyl for epidural analgesia in lower limb orthopedic surgeries. Saudi J Anaesth. 2011;5:365–70. doi: 10.4103/1658-354X.87264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Mustafa MM, Abu-Halaweh SA, Aloweidi AS, Murshidi MM, Ammari BA, Awwad ZM, et al. Effect of dexmedetomidine added to spinal bupivacaine for urological procedures. Saudi Med J. 2009;30:365–70. [PubMed] [Google Scholar]


