Abstract
Background and Aims:
Several formulae are available to estimate endotracheal tube (ETT) size in children. This study was designed to compare the ETT estimated by the Broselow tape (BT) with age-based estimation of ETT size and to identify the most accurate formula for the prediction of uncuffed ETT size in Indian children.
Material and Methods:
Pediatric patients aged 1 month–6.5 years undergoing emergency or elective surgery under general anesthesia requiring endotracheal intubation with uncuffed ETT were included in this study. The ETT size was selected based on the age formula (Penlington formula). The ETT used was deemed to be of correct fit based on the delivery of adequate tidal volume and presence of minimal leak at 20 cm H2O. The actual ETT used was compared with that predicted by age, length of the child, BT, and fifth fingernail width of the child using Pearson's correlation.
Results:
In children aged <6 months, the ETT used was found to correlate with length (r = 0.286, P = 0.044) and finger nail width (r = 0.542, P < 0.001) of the children. In children >6 months, the ETT used correlated with that predicted from age, BT, length, and fingernail width of the children. In our study, BT has an overall correct predictability rate of 50.3% whereas the age-based formula has a correct prediction rate of 59.8% and length-based formula is 48.7% accurate.
Conclusion:
Length of the child has a good correlation with size of the ETT to be used in Indian children across all age groups. BT is an effective tool to predict ETT size in children >6 months.
Keywords: Key words: Broselow tape, endotracheal tube, endotracheal tube size
Introduction
Endotracheal intubation may be required in pediatric patients in the elective or emergent setting. It is necessary to choose the best fit endotracheal tube (ETT) to provide effective ventilation. An undersized ETT would cause gas leak and loss of tidal volume with risk of aspiration whereas an oversized ETT might lead to postoperative pharyngolaryngeal complications including stridor, croup, and dysphonia.[1] Several formulae are available to predict the ETT size based on either the child's age, length, weight, fifth fingernail width, tracheal diameter obtained from skiagram or ultrasound, or a combination of these parameters.[2] The pediatric Broselow emergency tape is a length-based tool to predict body weight during emergency. In a pediatric emergency department, it may often not be possible to weigh a sick child. The BT has nine color-coded zones and uses height-weight correlation to predict body weight from height and hence determine standardized emergency drug doses and equipment size including ETT, urinary catheter, intercostals drain, nasogastric tube, and defibrillation energy. It greatly reduces the strain on emergency personnel in recollecting formulae and calculating doses in a crisis situation. It is recommended by the Advanced Trauma Life Support and Pediatric Advanced Life Support and has been validated in the US and Europe.[3,4] In choosing an appropriate ETT, the formula must be simple to use with good accuracy and precision. Radiological parameters and complicated mathematical formulae may not be appropriate in the emergency setting. Reintubation rates are higher with uncuffed ETTs.[5] High tube exchange rate and prolonged intubation time may increase the possibility of hypoxia and aspiration. The primary outcome of this study is to compare the size of ETT selected using the age-based formula (ABF) with that using the BT. The secondary outcome is to identify the most accurate formula for predicting ETT size in the Indian pediatric population.
Material and Methods
After obtaining Institutional Review Board approval, this prospective, observational study was conducted at a tertiary care pediatric hospital in India. One hundred ninety nine children of the American Society of Anesthesiologists physical status I–III aged 1 month–6.5 years undergoing emergency or elective surgery with orotracheal intubation with uncuffed ETT were enrolled, after obtaining parental consent. Children with known difficult airway, congenital airway anomalies, those weighing <3 kg or >25 kg, and those with length <46 cm or >125 cm were excluded from the study.
During the preanesthetic examination, a detailed airway examination was done; the length and weight were recorded. The length was measured in centimeter using a measuring tape as well as by BT. The color zone indicated by the BT was recorded. The fifth fingernail width was also noted.
The ETT size was estimated using the following formulae and recorded by one anesthesiologist:
-
Age based (Penlington formula):[6]
- >6.5 years: Age/3 + 3.5 = ID of ETT in mm
- <6.5 years: Age/4 + 4.5 = ID of ETT in mm
-
Length based:[7]
- 2+ length/30 = ID of ETT in mm
Length based: as predicted by Broselow tape (BT)[4]
Fifth fingernail maximum width = ID of ETT in mm.[8]
In calculating the ETT size, children <6 months were taken as 0.5 year; those between 6 months and 1 year 6 months were considered 1 year and so on. Since the calculated values may not be multiples of 0.5, they were approximated to the nearest 0.5 or 0.0.
The attending anesthesiologist was blind to the various estimations made regarding ETT size selection. General anesthesia was induced with sevoflurane in an O2/N2O mixture or propofol as appropriate and maintained with fentanyl and isoflurane in O2/N2O mixture. Standard monitors were applied including electrocardiogram, pulse oximetry, end-tidal CO2, and noninvasive blood pressure.
Tracheal intubation was done after muscle relaxation with atracurium 0.5 mg/kg followed by bag-mask ventilation for 3 min. The size of the ETT was selected by the attending anesthesiologist according to the age-based (Penlington) formula, which is the practice in our institute. The correct position of the ETT was confirmed by capnography and auscultation for bilateral breath sounds. The ABF gives the size of the uncuffed ETT to the nearest 0.5 mm. If the ETT chosen was too large for the glottis or resistance was met with at intubation, a 0.5 mm size smaller tube was chosen and this was recorded as a tube change.
The tracheal tube was considered to be appropriate by the attending anesthesiologist if the ETT passed smoothly through the glottis and there was minimal air leak at 20 cm H2O. The leak test was done by connecting the ventilator with a peak inspiratory pressure of 20 cm H2O, zero positive end-expiratory pressure, gas flow 3 L/min, and respiratory rate appropriate for the patient's age. The presence of minimal leak by palpation/auscultation, expired tidal volume of >7 ml/kg, and square wave capnogram were considered acceptable.
If there was an unacceptable large leak with insufficient delivered tidal volume, the ETT was exchanged with a 0.5 mm larger size tube and recorded as a tube change.
The end point of the study was reached once the ETT inserted has found to be the best fit.
The sample size was chosen assuming a difference of 0.22 between mean of ETT used and that estimated from BT, with a two-tailed alpha value of 0.05 and power of 80%. The data were analyzed using statistical software SAS version 9.2, SPSS version 15.0 (SPSS-IBM Inc., Chicago, IL, USA), MedCalc version 9.0.1 [Medcalc Software, Belgium], SYSTAT version 12.0 [Systat Software Inc, SanJose, California, USA], and R Environment version 2.11.1 (The R foundation for statistical computing, Vienna, Austria). Data are represented as mean ± standard deviation, number (%) as appropriate. Pearson's correlation between study variables was performed to find the degree of relationship. Regression analysis was employed to find the relationship between ETT used and ETT estimated by the various formulae. The P < 0.05 was considered significant.
Results
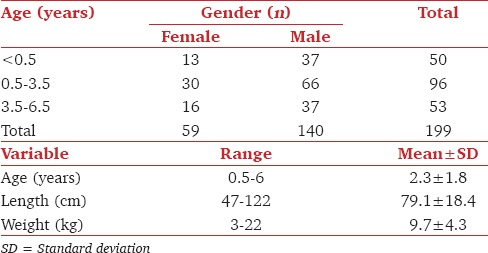
A total of 203 children were recruited in this study. Four were excluded from the analysis as they had fixed flexion deformity of the knees and length could not be accurately measured. 199 were included in the final analysis. The demographic data of the patients are given in Table 1.
Table 1.
Demographic characteristics of the study population
The candidates were divided into three age groups (<0.5 years, 0.5–3.5 years, >3.5 years) to compare the ETT used with that estimated by age, BT, length, and fifth fingernail width of the child. There are seven color-coded zones in the BT which advocate use of an uncuffed ETT. These were divided into three categories with the first three zones (which predict ETT size 3.5 mm) to be the first group, the next two zones (predicting ETT size 4.0 and 4.5, respectively) forming the second group, and the last two zones (predicting ETT size 5.0 and 5.5, respectively) forming the third group. The corresponding age distribution would be ≤0.5 years, 0.5–3.5 years, and 3.5 years to 6.5 years if the ABF was used instead to estimate the ETT size.
The most common ETT used in each age group is given in Figure 1. Linear regression showed good correlation (R2 = 0.87) between ETT used and length of the child. 30/199 (15.1%) of patients required a reintubation due to inappropriate tube size of which 26 patients required a larger size ETT and 4 patients required change to a smaller ETT. No patient required more than one tube exchange. The most common ETT requiring a change was 4.0 mm ID ETT (10/30).
Figure 1.
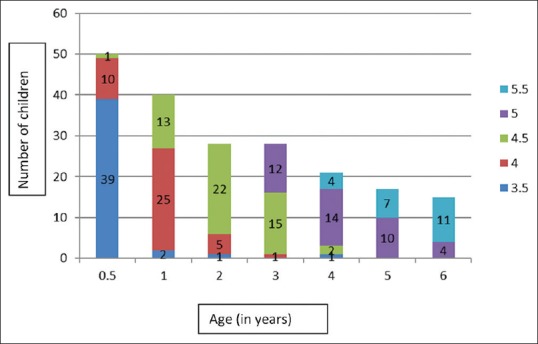
Endotracheal tube used versus age: Graph showing most common endotracheal tube used in each age
Pearson's correlation test was used to evaluate the extent of correlation between ETT used and ETT estimated [Table 2]. In children <6 months, the ETT used was found to correlate with length (r = 0.286, P = 0.044) and fifth fingernail width (r = 0.542, P < 0.001) of the child. In children >6 months, the ETT used correlated with that predicted from age, BT, length, and fingernail width of the child [Table 3].
Table 2.
Pearson's correlation between endotracheal tube used and estimated endotracheal tube size, Broselow tape, estimated endotracheal tube size age, estimated endotracheal tube size length, and estimated endotracheal tube size fifth fingernail width
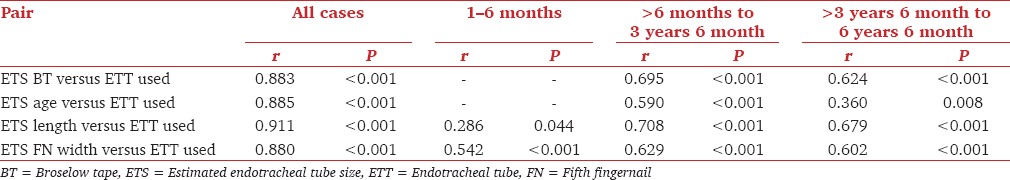
Table 3.
Comparison between endotracheal tube used and endotracheal tube predicted
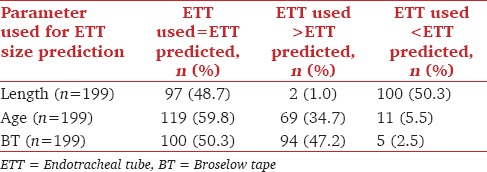
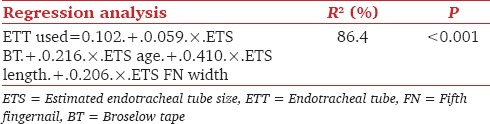
Step-wise regression analysis showed that the ETT used showed strongest correlation with the length-based estimation [Table 4]. The ABF underestimated ETT size in 34.7% of cases while the BT underestimated ETT size in 47.2% of patients. If the length-based formula was used, the ETT size was overestimated in 50.3% of children [Table 3].
Table 4.
Step-wise regression analysis to predict endotracheal tube used using estimated endotracheal tube size, Broselow tape, estimated endotracheal tube size age, estimated endotracheal tube size length, estimated endotracheal tube size fifth fingernail width
Discussion
Until 2009, as many as 19 different formulae for selection of uncuffed ETTs in children have been published.[2] Among the commonly used ABF, the Cole formula has been derived from data obtained in American children and is useful for children >2 years while the Penlington formula has been derived from British children.[6,9] Neither has been validated in Indian children though they are widely used. Children of the same age differ in weight and height due to nutritional, racial, and developmental differences. Hence, any attempt to internationalize these formulae needs validation in the local population. In Korean children, the ABF was able to predict appropriate ETT size in less than one-third of the patients.[10] King et al. concluded that the ABF was superior to fifth fingernail dimensions in determining ETT size.[8] However, Turkistani et al. observed that the ABF and fifth fingernail width predicted the best fit ETT more accurately than length and multivariate formula.[11] In a study by Park et al., the Penlington formula had a better success rate than the Cole formula (43% vs. 32%), but both ABF were inferior to a radiograph-based formula that calculated ETT size from the tracheal diameter at C7 from a chest X-ray.[12]
In Chinese children, the length-based formula derived from a previous study in the same population had a high accuracy of 82.4%.[7,13] Keep and Manford, from whose work the Penlington formula is derived, also established a better correlation between height and ETT size but rejected the cumbersome formula (tube size [mm] = height [cm] × 0.045 + 0.8) in favor of the simpler ABF.[14] The weight-based formula was also found to be less reliable than the ABF.[15]
The Broselow pediatric emergency tape has 55%–77% accuracy in correctly predicting ETT size.[3,13] The BT-based ETT estimation was correct in 86.9% of Korean children.[16] In our study, BT has a correct predictability rate of 50.3% whereas the ABF has a correct prediction rate of 59.8% and length-based formula is 48.7% accurate.
Several studies across the globe have sought to validate the length-weight correlation of the BT in their respective population. Only few have studied the BT length – ETT size relationship. Varghese et al. analyzed the correctness of BT measurements in 500 children requiring resuscitation in the emergency room.[17] They found the BT to have greater accuracy in the 0.1–6.7 years age group and in children weighing <15 kg. In this group, the BT underestimated ETT size by 0.5. It must be noted that the number of children weighing <15 kg was ten times more than those with higher weights in this study.
Asskaryar and Shankar have developed a new Indian pediatric weight estimation tool, based on the BT, by adding an 8% correction factor to the existing tape. Yet again, they have exclusively examined the height-weight association and hence dose calculation.[18] Mishra et al. found the tape to be more reliable in predicting the weight in <10 kg and 10–18 kg groups in urban Indian children.[19]
Agarwal et al. evaluated the ease of use of the “Broselow cart” (where intubation and emergency equipment are placed according to the BT color-coded drawers) versus the “standard pediatric resuscitation cart.” In a simulated scenario, health-care providers found the Broselow cart to be more simple and convenient to use. This study has not examined the clinical correctness of the equipment chosen.[20]
The reintubation rate in our study is similar to that in literature for uncuffed ETT.[11]
In the quest to develop an easy and uncomplicated method to predict the accurate uncuffed ETT, Cho et al. have used the recursive partitioning analysis to develop a decision tree. This flowchart is simple, visually attractive with a correct predictability rate of 59.5%, and a close prediction rate of 93.7%.[21]
The multivariate formula (ETT size = 2.44+ [age × 0.1] + [height × 0.02] + [weight × 0.016]) was derived using linear regression analysis on data collected retrospectively.[22] Shiroyama et al. developed another multiple regression formula with age and height as variables to calculate ETT size.[23] The existence of several such formulae indicates the regional and racial differences in predicting ETT size and that “one size does not fit all.” The disadvantage of these complex formulae is that they cannot be calculated quickly during a crisis or emergency.
In a mixed population of rural and urban Canadian children, the reliability of BT in estimating weight has been investigated and concerns raised on the serious underestimation of length-based derivatives in obese children.[24] The accuracy of ETT size estimation in this cohort of patients is yet to be detailed. There were no obese children in our study.
One limitation of this study is the underrepresentation of children in the older age group. The second is that it is a single-center study and may not be representative of population from other regions. No attempt has been made to differentiate between urban and rural population. Third, the results may not be extrapolated to ETT of other manufacturers if discrepancy in outer diameter exists.
Conclusion
It may be said that length of the child has a good correlation with ETT size in Indian children across all age groups. BT may be used to predict ETT size in Indian children >6 months. It is a useful tool to estimate ETT size in emergency when age or length of the child is not known.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr. K. P. Suresh, scientist (Biostatistics), National Institute of Veterinary Epidemiology and Disease Informatics, Bengaluru - 560 024, Karnataka, India, for reviewing the research methodology and statistical results of the study.
References
- 1.Shibasaki M, Nakajima Y, Ishii S, Shimizu F, Shime N, Sessler DI. Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology. 2010;113:819–24. doi: 10.1097/ALN.0b013e3181ef6757. [DOI] [PubMed] [Google Scholar]
- 2.von Rettberg M, Thil E, Genzwürker H, Gernoth C, Hinkelbein J. Endotracheal tubes in pediatric patients. Published formulas to estimate the optimal size. Anaesthesist. 2011;60:334–42. doi: 10.1007/s00101-010-1756-0. [DOI] [PubMed] [Google Scholar]
- 3.Hofer CK, Ganter M, Tucci M, Klaghofer R, Zollinger A. How reliable is length-based determination of body weight and tracheal tube size in the paediatric age group? The Broselow tape reconsidered. Br J Anaesth. 2002;88:283–5. doi: 10.1093/bja/88.2.283. [DOI] [PubMed] [Google Scholar]
- 4.Luten RC, Wears RL, Broselow J, Zaritsky A, Barnett TM, Lee T, et al. Length-based endotracheal tube and emergency equipment in pediatrics. Ann Emerg Med. 1992;21:900–4. doi: 10.1016/s0196-0644(05)82924-5. [DOI] [PubMed] [Google Scholar]
- 5.Weiss M, Dullenkopf A, Fischer JE, Keller C, Gerber AC, European Paediatric Endotracheal Intubation Study Group Prospective randomized controlled multi-centre trial of cuffed or uncuffed endotracheal tubes in small children. Br J Anaesth. 2009;103:867–73. doi: 10.1093/bja/aep290. [DOI] [PubMed] [Google Scholar]
- 6.Penlington GN. Letter: Endotracheal tube sizes for children. Anaesthesia. 1974;29:494–5. doi: 10.1111/j.1365-2044.1974.tb00698.x. [DOI] [PubMed] [Google Scholar]
- 7.Wang TK, Wu RS, Chen C, Chang TC, Hseih FS, Tan PP. Endotracheal tube size selection guidelines for Chinese children: Prospective study of 533 cases. J Formos Med Assoc. 1997;96:325–9. [PubMed] [Google Scholar]
- 8.King BR, Baker MD, Braitman LE, Seidl-Friedman J, Schreiner MS. Endotracheal tube selection in children: A comparison of four methods. Ann Emerg Med. 1993;22:530–4. doi: 10.1016/s0196-0644(05)81937-7. [DOI] [PubMed] [Google Scholar]
- 9.Cole F. Pediatric formulas for the anesthesiologist. AMA J Dis Child. 1957;94:672–3. doi: 10.1001/archpedi.1957.04030070084009. [DOI] [PubMed] [Google Scholar]
- 10.Kim Ko, Lee YM, Choi JK, Cho H. Appropriateness of age-based formula to determine endotracheal tube size in Korean children. Korean J Anesthesiol. 2007;52:275–7. [Google Scholar]
- 11.Turkistani A, Abdullah KM, Delvi B, Al-Mazroua KA. The ‘best fit’ endotracheal tube in children – Comparison of four formulae. Middle East J Anaesthesiol. 2009;20:383–7. [PubMed] [Google Scholar]
- 12.Park HP, Hwang JW, Lee JH, Nahm FS, Park SH, Oh AY, et al. Predicting the appropriate uncuffed endotracheal tube size for children: A radiograph-based formula versus two age-based formulas. J Clin Anesth. 2013;25:384–7. doi: 10.1016/j.jclinane.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Shih MH, Chung CY, Su BC, Hung CT, Wong SY, Wong TK. Accuracy of a new body length-based formula for predicting tracheal tube size in Chinese children. Chang Gung Med J. 2008;31:276–80. [PubMed] [Google Scholar]
- 14.Keep PJ, Manford ML. Endotracheal tube sizes for children. Anaesthesia. 1974;29:181–5. doi: 10.1111/j.1365-2044.1974.tb00619.x. [DOI] [PubMed] [Google Scholar]
- 15.Eipe N, Barrowman N, Writer H, Doherty D. A weight-based formula for tracheal tube size in children. Paediatr Anaesth. 2009;19:343–8. doi: 10.1111/j.1460-9592.2008.02916.x. [DOI] [PubMed] [Google Scholar]
- 16.Jang HY, Shin SD, Kwak YH. Can the Broselow tape be used to estimate weight and endotracheal tube size in Korean children? Acad Emerg Med. 2007;14:489–91. doi: 10.1197/j.aem.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 17.Varghese A, Vasudevan VK, Lewin S, Indumathi CK, Dinakar C, Rao SD. Do the length-based (Broselow) Tape, APLS, Argall and Nelson's formulae accurately estimate weight of Indian children? Indian Pediatr. 2006;43:889–94. [PubMed] [Google Scholar]
- 18.Asskaryar F, Shankar R. An Indian pediatric emergency weight estimation tool: Prospective adjustment of the Broselow tape. Int J Emerg Med. 2015;8:78. doi: 10.1186/s12245-015-0078-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mishra DG, Kole T, Nagpal R, Smith JP. A correlation analysis of Broselow™ Pediatric Emergency Tape-determined pediatric weight with actual pediatric weight in India. World J Emerg Med. 2016;7:40–3. doi: 10.5847/wjem.j.1920-8642.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agarwal S, Swanson S, Murphy A, Yaeger K, Sharek P, Halamek LP. Comparing the utility of a standard pediatric resuscitation cart with a pediatric resuscitation cart based on the Broselow tape: A randomized, controlled, crossover trial involving simulated resuscitation scenarios. Pediatrics. 2005;116:e326–33. doi: 10.1542/peds.2005-0320. [DOI] [PubMed] [Google Scholar]
- 21.Cho AR, Kim ES, Lee DW, Hong JM, Kwon JY, Kim HK, et al. Comparisons of recursive partitioning analysis and conventional methods for selection of uncuffed endotracheal tubes for pediatric patients. Paediatr Anaesth. 2015;25:698–704. doi: 10.1111/pan.12620. [DOI] [PubMed] [Google Scholar]
- 22.Eck JB, De Lisle Dear G, Phillips-Bute BG, Ginsberg B. Prediction of tracheal tube size in children using multiple variables. Paediatr Anaesth. 2002;12:495–8. doi: 10.1046/j.1460-9592.2002.00894.x. [DOI] [PubMed] [Google Scholar]
- 23.Shiroyama K, Tanaka H, Kawamoto M, Yuge O. Prediction of the appropriate uncuffed endotracheal tube size for pediatric anesthesia. J Jpn Soc Clin Anesth. 1998;18:693–7. [Google Scholar]
- 24.Milne WK, Yasin A, Knight J, Noel D, Lubell R, Filler G. Ontario children have outgrown the Broselow tape. CJEM. 2012;14:25–30. doi: 10.2310/8000.2011.110523. [DOI] [PubMed] [Google Scholar]


