A 19-year-old male presented with a swelling on the posterior part of tongue of 2 months duration. The swelling was of insidious onset and not associated with pain or trauma. On intraoral examination, the swelling was cystic in consistency and measured 1.5 × 1.5 cm. [Figure 1a]. Fine needle aspiration cytology (FNAC) was done from the swelling. The aspirate was mucinous and smears showed scattered mucinophages and lymphocytes in a mucinous background [Figure 1b and c]. A diagnosis of mucocele was suggested based on the clinical and cytological findings. The swelling was surgically excised. Grossly, it measured 1.5 × 1.5 cm. On the cut section, it was cystic and milled with mucinous material. Histopathological examination revealed both hypocellular and hypercellular areas with cystic areas [Figure 1d]. On immunohistochemistry (IHC), the cells were strongly positive for S100. A final diagnosis of cystic schwannoma was made. The patient was discharged on the third postoperative day and is on regular follow-up. There was no recurrence at 1 year of follow-up.
Figure 1.
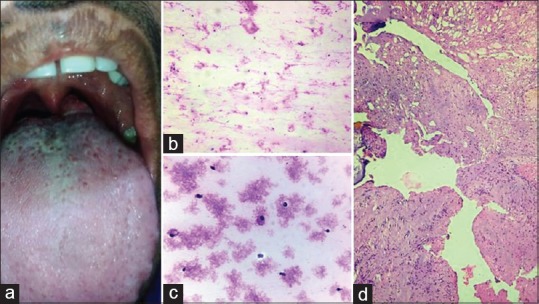
(a) Swelling in the posterior part of the tongue. (b and c) Smears showed scattered mucinophages and lymphocytes in a mucinous background. (b: Giemsa stain x100; c: Pap stain x400). (d) Histopathology revealed both hypocellular and hypercellular areas with cystic areas. (H and E stain ×100)
DISCUSSION
Schwannomas are benign, encapsulated nerve sheath neoplasm developed from Schwann cells. Schwannomas usually occur between 20 and 50 years of age; however, it may occur at any age and show equal sex predilection.[1] Schwannomas usually present as solitary, painless, and slow-growing mass of variable size usually 2–4 cm. However, multiple lesions may be seen in association with von-Recklinghausen's neurofibromatosis. Of all extracranial schwannomas, head and neck region accounts for 25– 45% of the cases whereas intraoral schwannomas are extremely rare and account for only 1% of cases.[2] Intraoral schwannomas most commonly affect the tongue, followed by palate, buccal mucosa, lip, and gingiva.[3] Schwannomas affecting the tongue arise from the hypoglossal nerve and vagus nerve.[1]
Schwannomas are usually solid; however, cystic changes are seen in approximately 4% of the cases. Cystic schwannomas are often comparatively large and appear to have a more rapid growth because of their cystic expansion. Mucinous degeneration, necrosis, hemorrhage, and microcysts formation are thought to be the reasons for these cystic changes.[2] FNAC in such cases may yield hypocellular fluid altogether missing the solid cellular areas. The aspirated fluid may contain individual spindle cells, fibroblasts, histiocytes, or lymphocytes but in the absence of characteristic cellular architecture, such schwannomas may escape diagnosis. FNAC has been found to be of limited value in achieving a preoperative diagnosis in such cystic lesions.[2,3]
Differential diagnosis that should be considered while dealing with a small, slow-growing cystic mass in tongue are mucocele, epidermoid cyst, dermoid cyst, lymphoepithelial cyst, lingual cyst, schwannoma, neurofibroma, and minor salivary gland tumor.[4] Histologically, schwannomas show alternating pattern of hypercellular Antoni A and hypocellular Antoni B areas, nuclear palisading, whorling of cells, and Verocay bodies. Sometimes, cystic schwannomas are difficult to diagnose even on histopathology due to secondary changes. In such situations, IHC plays a pivotal role in the definitive diagnosis. Schwannomas are strongly positive for S100.[1,2]
It is of paramount importance to differentiate between these two entities both preoperatively and postoperatively. Mucocele is managed by marsupialization whereas surgical excision is recommended in case of schwannoma. Schwannoma rarely recurs if completely excised.[1,2]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bansal R, Trivedi P, Patel S. Schwannoma of the tongue. Oral Oncol Extra. 2005;41:15–7. [Google Scholar]
- 2.Bohara S, Dey B, Agarwal S, Gupta R, Khurana N, Gulati A. A case of cystic schwannoma in the neck masquerading as branchial cleft cyst. Rare Tumors. 2014;6:5355. doi: 10.4081/rt.2014.5355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Satarkar RN, Kolte SS, Vujhini SK. Cystic schwannoma in neck: Fallacious diagnosis arrived on fine needle aspiration cytology. Diagn Cytopathol. 2010;36:866–7. doi: 10.1002/dc.21565. [DOI] [PubMed] [Google Scholar]
- 4.Walstad WR, Solomon JM, Schow SR, Ochs MW. Midline cystic lesion of the floor of the mouth. J Oral Maxillofac Surg. 1998;56:70–4. doi: 10.1016/s0278-2391(98)90919-3. [DOI] [PubMed] [Google Scholar]


