Key Points
Question
How much dietary sodium do US adults consume?
Findings
In this nationally representative survey of 827 US adults aged 20 to 69 years, mean 24-hour urinary sodium excretion was 3608 mg overall, and was significantly higher among men (4205 mg) than women (3039 mg). Mean 24-hour urinary potassium excretion was 2155 mg overall.
Meaning
These findings may provide a benchmark for future studies.
Abstract
Importance
In 2010, the Institute of Medicine (now the National Academy of Medicine) recommended collecting 24-hour urine to estimate US sodium intake because previous studies indicated 90% of sodium consumed was excreted in urine.
Objective
To estimate mean population sodium intake and describe urinary potassium excretion among US adults.
Design, Setting, and Participants
In a nationally representative cross-sectional survey of the US noninstitutionalized population, 827 of 1103 (75%) randomly selected, nonpregnant participants aged 20 to 69 years in the examination component of the National Health and Nutrition Examination Survey (NHANES) collected at least one 24-hour urine specimen in 2014. The overall survey response rate for the 24-hour urine collection was approximately 50% (75% [24-hour urine component response rate] × 66% [examination component response rate]).
Exposures
24-hour collection of urine.
Main Outcomes and Measures
Mean 24-hour urinary sodium and potassium excretion. Weighted national estimates of demographic and health characteristics and mean electrolyte excretion accounting for the complex survey design, selection probabilities, and nonresponse.
Results
The study sample (n = 827) represented a population of whom 48.8% were men; 63.7% were non-Hispanic white, 15.8% Hispanic, 11.9% non-Hispanic black, and 5.6% non-Hispanic Asian; 43.5% had hypertension (according to 2017 hypertension guidelines); and 10.0% reported a diagnosis of diabetes. Overall mean 24-hour urinary sodium excretion was 3608 mg (95% CI, 3414-3803). The overall median was 3320 mg (interquartile range, 2308-4524). In secondary analyses by sex, mean sodium excretion was 4205 mg (95% CI, 3959-4452) in men (n = 421) and 3039 mg (95% CI, 2844-3234) in women (n = 406). By age group, mean sodium excretion was 3699 mg (95% CI, 3449-3949) in adults aged 20 to 44 years (n = 432) and 3507 mg (95% CI, 3266-3748) in adults aged 45 to 69 years (n = 395). Overall mean 24-hour urinary potassium excretion was 2155 mg (95% CI, 2030-2280); by sex, 2399 mg (95% CI, 2253-2545) in men and 1922 mg (95% CI, 1757-2086) in women; and by age, 1986 mg (95% CI, 1878-2094) in adults aged 20 to 44 years and 2343 mg (95% CI, 2151-2534) in adults aged 45 to 69 years.
Conclusions and Relevance
In cross-sectional data from a 2014 sample of US adults, estimated mean sodium intake was 3608 mg per day. The findings provide a benchmark for future studies.
This study uses NHANES data to estimate the mean population sodium intake and describe urinary potassium excretion among US adults aged 20 to 69 years.
Introduction
Randomized clinical trials indicate reducing sodium intake can significantly lower blood pressure with greater effects among adults with hypertension. In 2010, the Institute of Medicine (IOM; now the National Academy of Medicine), in its report on strategies to reduce sodium intake in the United States, stated, “a more accurate measure of total sodium intake such as 24-hour urine collection should be employed in national population surveys, specifically, NHANES (the National Health and Nutrition Examination Survey).” This recommendation was based on a review of studies that suggested that 24-hour urinary excretion, when complete, reflects about 90% of sodium consumed from all sources. Historically, NHANES employed 24-hour recalls to estimate sodium intake but dietary data typically exclude the amount consumed from salt added at the table (estimated at 5% of intake) and estimates can be affected by errors in self-report or inaccurate estimates of the nutrient content of foods consumed. Previous studies using 24-hour urine collection among adults living in the United States were based on convenience samples or were not national in scope.
Potassium intake is associated with blood pressure and is inextricably linked with sodium in biology and physiology, and potassium chloride is used as a substitute for salt. Thus, concurrent estimation of 24-hour urinary potassium was efficient even though the amount of potassium intake excreted in 24-hour urine collection in previous studies was variable (50% to 90%).
The main objective of this study was to estimate mean sodium intake among US adults from 24-hour urinary excretion. Secondary objectives were to provide estimates of mean 24-hour urinary potassium excretion and the sodium-to-potassium molar ratio.
Methods
Data Source
Details about NHANES are available elsewhere, including the protocol and data collection procedures. In brief, NHANES 2014 was 1 year of an ongoing, cross-sectional survey of the US noninstitutionalized population, with household interview, examination, and postexamination components. A nationally representative sample was selected using a complex, multistage design. Participants were enrolled and data collected across all days of the week and seasons of the year. Data are publicly released every 2 years. In 2013-2014, 66% of adults aged 20 to 69 years screened for NHANES were examined. In 2014, half of these screened participants were randomly selected and, if eligible (ie, nonpregnant), asked to participate in 24-hour urine collection, postexamination. All participants provided written informed consent. This study was reviewed and approved by the research ethics review board for the National Center for Health Statistics, Centers for Disease Control and Prevention (CDC).
24-Hour Urine Collection
A detailed 24-hour urine collection protocol, based on previous population-based studies, was successfully piloted in 2013. In 2014, each participant selected and eligible for this component was asked to collect a timed 24-hour urine specimen. Timed collections were started in the urine mobile examination center and completed at the mobile center the following day, with detailed verbal, written, and pictorial instruction on collection provided to participants (Supplement). Upon completion of the first 24-hour urine collection, participants were eligible for a second 24-hour urine collection scheduled 3 to 10 days later. About half of the eligible participants were selected and asked to collect a second 24-hour urine specimen (details in the Supplement). A complete 24-hour urine collection was defined as (1) recorded start and stop times; (2) 22 hours or more duration (from start to stop of collection); (3) total urine volume of 400 mL or more; (4) reported no more than a few drops of urine lost during collection; and (5) for women, no reported menstruation during collection. Details on urine specimen processing, storage, shipping, quality assurance, and control procedures are available elsewhere. To protect the confidentiality of survey respondents, the data from the 2014 24-hour urine collection were accessed and analyzed in the National Center for Health Statistics Research Data Center.
Urinary Electrolyte and Creatinine Excretion
Urine specimens were analyzed for electrolytes (ie, sodium, potassium, chloride) using the ion-selective electrode technique (Mod PE analyzer; Roche) and for creatinine using the enzymatic assay (Cobas 6000 Analyzer; Roche). The urinary sodium and potassium measurements showed low analytical imprecision (<3% coefficient of variation for 2 quality control pools analyzed over a period of 14 months) and satisfactory agreement with the National Institute of Standards and Technology standard reference materials: 2201 mg for sodium chloride (mean bias for sodium of 3.4% [SD, 3.8%] over a concentration range of 25-200 mEq/L) and 2202 mg for potassium chloride (mean bias for potassium of 1.6% [SD, 3.9%] over a concentration range of 12-100 mEq/L). The total amount of the analyte (eg, electrolyte, excreted in each 24-hour urine specimen) was standardized to 24 hours by multiplying the analyte concentration by the adjusted 24-hour urine volume based on duration of collection (hours from start to stop). Data from 2 convenience samples of US adults indicate the within-individual (day-to-day) coefficient of variation in 24-hour urinary sodium excretion was 19% to 23% for adults aged 18 to 39 years and 31% to 38% for adults aged 45 to 79 years.
Analyses by Participant Subgroups
In secondary analyses, data on urinary electrolyte excretions were analyzed by sex and age group (20-44 years and 45-69 years). Additional exploratory analyses were conducted on 24-hour urinary sodium excretion by 10-year age groups and on 24-hour electrolyte excretion by other demographic and cardiovascular disease (CVD) risk subgroups based on nonmissing values for the specified participant characteristic. Previous studies indicate urinary excretion of electrolytes can vary by sex, age, and race or ethnic origin. Demographic characteristics (subgroups) for exploratory analyses included race or Hispanic origin (non-Hispanic white, non-Hispanic black, non-Hispanic Asian, and Hispanic); education (≤12 years or General Educational Development certificate, >12 years); and family income as a percentage of poverty guidelines (≤130%, >130%). Demographic characteristics were based on participant, self-reported information. Participants reported their sex, race, ethnic origin, and education level using standardized categories, including options for “other,” “do not know,” or refusal. Participants who reported “other” non-Hispanic race or more than 1 race were included in total population estimates, but excluded from subpopulation analyses by race and Hispanic origin due to small sample size. Age and family income were reported in years and dollar amounts, respectively, then categorized into analytic subgroups.
CVD risk subgroups included weight status subgroups based on body mass index (BMI; calculated as weight in kilograms divided by height in meters squared); physical activity level based on standard questions; reported action to reduce sodium or salt intake; hypertension status based on blood pressure measurements and use of antihypertensive medication; diagnosed diabetes (self-reported diagnosis by a clinician or use of a diabetes medication); chronic kidney disease (estimated glomerular filtration rate <60 mL/min/1.73 m2 or urinary albumin/creatinine ratio >30 mg/g), and self-reported history of CVD (congestive heart failure, coronary heart disease, angina or angina pectoris, myocardial infarction, or stroke). Reported action to reduce sodium or salt intake was determined by an affirmative response to 1 part of a multipart question, “To lower your risk for certain diseases, are you now doing any of the following:…?” One of “the following” items was “reducing the amount of sodium or salt in your diet?” Mean blood pressure was calculated from 2 or 3, consecutive, brachial blood pressure readings. Before measurement, maximum inflation level was determined and participants rested quietly in a seated position for 5 minutes. A calibrated mercury sphygmomanometer with the cuff appropriate for the participant’s arm circumference was used by a trained technician. Hypertension status was defined based on the 2017 hypertension guidelines and based on the previous definition in a sensitivity analysis. Detailed descriptions of BMI, physical activity level, and hypertension status assessment and definitions are available in the Supplement.
Dietary Sodium and Energy Intake
Sodium and energy intake for nonpregnant adults aged 20 to 69 years for this study was based on the initial dietary recall in NHANES 2013-2014. The initial 24-hour dietary recall was collected in-person by trained interviewers using the United States Department of Agriculture (USDA) automated multiple-pass method with food models. The nutrient values for each reported food were assigned using the USDA Food and Nutrient Database for Dietary Studies. Dietary sodium intake calculations excluded salt added at the table as the amount of salt added was not quantified.
Statistical Analysis
The target sample size in the 24-hour urine collection component in 2014 was based on the minimum number per sociodemographic subgroup (n = 100-160 participants) required to estimate a prevalence of 90%, and for survey design effects of 1.25 to 2.00. A minimum effective sample size of 38 to 60 participants per group was recommended for estimating a mean with a survey design effect of 1.25 to 2.00, respectively.
Analyses were conducted to compare the weighted distributions of population characteristics represented by nonpregnant NHANES 2013-2014 examination participants aged 20 to 69 years (n = 4656) among participants who completed a 24-hour urine collection in 2014 and among those who did not. Additional analyses were conducted to describe the distributions of population characteristics represented by participants who completed 24-hour urine collection in 2014, among men and women, further weighted for selection and nonresponse to this component.
The initial 24-hour urine collection was used to estimate, among a group of US adults, 24-hour urinary sodium and potassium excretion and their molar ratio. A single 24-hour urine collection is an indicator of short-term sodium intake and can vary from day to day within individuals with foods consumed, as well as with biological factors and rhythms independent of intake. Given a sufficient number of participants, within-individual day-to-day variability does not affect estimates of population means. Individuals with “usual” high or low levels of intake or excretion, however, can have even higher or lower levels based on a single 24-hour urinary excretion, which can increase the variance around a population mean. The interquartile range and proportion with intake above a specific threshold reflect the distribution of acute intake or excretion on any given day.
In this study, the weighted means (95% CIs) and percentiles of 24-hour urinary electrolyte excretions were estimated, and, for sodium, the weighted proportion of the population with 24-hour urinary excretion greater than or equal to 2300 mg (the sodium tolerable upper intake level according to the 2005 IOM panel on dietary reference intakes for electrolytes and water). Analyses of weighted urinary electrolyte excretion among population subgroups were conducted based on nonmissing values for the specified demographic or health characteristic.
Four sensitivity analyses were conducted. First, urinary sodium and potassium excretion and 95% CIs were estimated after excluding additional participants with potentially incomplete collection based on observed-to-expected 24-hour urinary creatinine levels (Supplement). Second, multiple imputation was used to classify participants into subgroups who had missing values for demographic characteristics or CVD risk factors (Supplement). Mean sodium and potassium excretion were then estimated for population subgroups based on imputed values. Third, weighted mean 24-hour urinary sodium and potassium excretion and their molar ratio were examined by hypertension status using the previous, higher, thresholds for blood pressure, now called stage 2 hypertension (for definition, see the Supplement). Fourth, mean population dietary intake of sodium, energy, and sodium density were described using data from 4246 nonpregnant adults aged 20 to 69 years who participated in NHANES 2013-2014 and had a reliable initial dietary recall.
Estimated distributions of population characteristics, urinary electrolytes, and dietary data were based on weighted data to obtain national estimates representative of nonpregnant US adults aged 20 to 69 years. For distributions of population characteristics estimated with nonpregnant participants in NHANES 2013-2014 by completion of 24-hour urine collection, the 2013-2014 examination sample weights were used. For estimates of sodium and energy intake based on NHANES 2013-2014 dietary recall data, the initial day dietary sample weights were used. For the distribution of characteristics and urinary electrolyte excretion estimated using data from those who completed 24-hour urine collection, the 24-hour urine sample weights were used to account for additional sampling and nonresponse. Rao-Scott F-adjusted χ2 statistics were used for comparing proportions, and t tests for comparing means. Statistical testing and 95% CI accounted for the complex survey sample design.
In addition, unweighted analyses were conducted. These analyses included completion rates for 24-hour urine collection; within-individual variability and differences in urinary electrolyte and creatinine excretion; and unweighted means, standard deviation, and percentiles of 24-hour urinary sodium and potassium excretion. Among the subset of participants with two 24-hour urine specimens, within-individual to between-individual variability in urinary electrolyte and creatinine excretion was estimated using methods described previously. χ2 Tests were used for comparing unweighted 24-hour completion rates by participant characteristics.
All analyses were conducted with SAS (SAS Institute), version 9.3, and SAS-callable SUDAAN (RTI International), version 11.0. A 2-sided P value of less than .05 was considered statistically significant for all statistical comparisons between groups. No adjustments were made for multiple comparisons. Estimates with a relative standard error (standard error/estimate [mean or proportion]) more than 30% were deemed statistically unreliable and not reported.
Results
Completion of 24-Hour Urine Collection
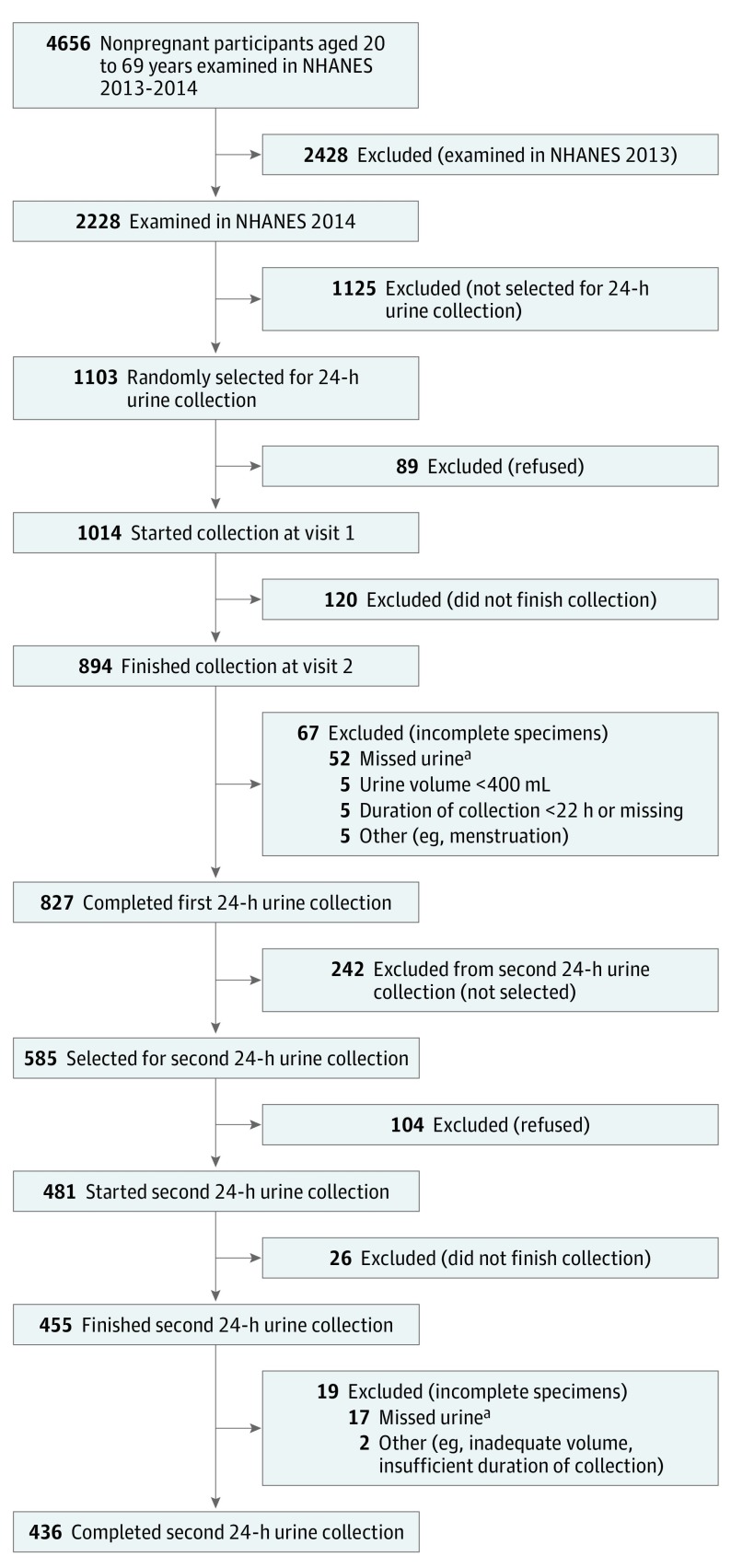
In 2013-2014, 4656 nonpregnant adults aged 20 to 69 years participated in the examination component of NHANES, with 2228 participating in 2014 (Figure). Among these 2228 participants in 2014, 1103 were randomly selected and asked to participate in 24-hour urine collection postexamination (Figure). Of those asked to participate, 827 participants (75%; men, 421; women, 406) completed an initial 24-hour urine collection (eTable 1 in the Supplement; Figure). Completion rates differed by sex, race and Hispanic origin, education, BMI, and hypertension status categories (eTable 2 in the Supplement). Across subgroups, completion was more than 70% except among non-Hispanic Asians (62.5%) and participants with a BMI less than 25.0 (68.8%) (eTable 2 in the Supplement). The overall survey response rate for the 24-hour urine collection was estimated at approximately 50% (75% [24-hour urine completion rate] × 66% [NHANES examination response rate]).
Figure. Flow of Participants Through the Study.
NHANES indicates National Health and Nutrition Examination Survey.
aParticipants who “missed” urine included those who spilled or missed more than a few drops of urine during the 24-hour collection period as determined from a series of standardized questions with fixed response categories administered at visit 2 for each urine collection. For further details, see the eMethods in the Supplement.
Estimated Population Demographic and Health Characteristics
Among the nonpregnant adults aged 20 to 69 years who participated in the examination component of NHANES 2013-2014 (n = 4656), distributions of population demographic characteristics and cardiovascular disease risk factors were not statistically significantly different among participants who completed 24-hour urine collection in 2014 vs those who did not (Table 1). Those who completed the 24-hour urine collection, represented a population of US adults of whom 52.5% (95% CI, 48.3%-56.8%) were men compared with 48.9% (95% CI, 57.0%-50.7%) men based on those who did not complete a 24-hour urine collection, P = .14. The percentages for race and Hispanic origin distributions were 65.4% (95% CI, 55.3%-75.4%) non-Hispanic white, 15.2% (95% CI, 7.4%-23.1%) non-Hispanic black, 10.9% (95% CI, 7.7%-14.1%) Hispanic, and 5.5% (95% CI, 2.5%-8.6%) non-Hispanic Asian, based on those who completed a 24-hour urine collection. The percentages based on those who did not complete a 24-hour urine collection were 63.5% (95% CI, 54.9%-72.1%) among non-Hispanic white, 11.0% (95% CI, 7.7%-14.2%) non-Hispanic black, 17.2% (95% CI, 10.7%-23.7%) Hispanic, and 5.5% (95% CI, 4.1%-6.9%) non-Hispanic Asian participants, P = .18. In addition, the percentages of adults who had more than 12 years of education were 60.2% (95% CI, 54.0%-66.5%) based on those who completed a 24-hour urine collection and 64.4% (95% CI, 59.3%-69.4%) based on those who did not, P = .18; and 44.9% (95% CI, 39.7%-48.8%) of adults who completed a 24-hour urine collection were estimated to have hypertension based on 2017 guidelines vs 40.1% (95% CI, 38.5%-41.8%) for those who did not, P = .08.
Table 1. Estimated Population Characteristics, NHANES 2013-2014, by Completion of 24-Hour Urine Collection in 2014.
| Characteristica | Nonpregnant Adults Aged 20-69 yb | Did Not Complete 24-Hour Urine Collection in 2014c | Completed 24-Hour Urine Collection in 2014d | P Valuee | |||
|---|---|---|---|---|---|---|---|
| No. of Participantsf | % (95% CI)g | No. of Participantsf | % (95% CI)g | No. of Participantsf | % (95% CI)g | ||
| Overall | 4656 | 100 | 3829 | 100 | 827 | 100 | |
| Sex | .14 | ||||||
| Men | 2263 | 49.5 (48.0-51.1) | 1842 | 48.9 (47.0-50.7) | 421 | 52.5 (48.3-56.8) | |
| Women | 2393 | 50.5 (48.9-52.0) | 1987 | 51.1 (49.3-53.0) | 406 | 47.5 (43.2-51.7) | |
| Age, y | .76 | ||||||
| 20-44 | 2349 | 51.5 (49.1-54.0) | 1917 | 51.3 (48.8-53.9) | 432 | 52.4 (45.7-59.0) | |
| 45-69 | 2307 | 48.5 (46.0-50.9) | 1912 | 48.7 (46.1-51.2) | 395 | 47.6 (41.0-54.3) | |
| Race and Hispanic origin | .18 | ||||||
| Non-Hispanic white | 1834 | 63.9 (56.5-71.3) | 1495 | 63.5 (54.9-72.1) | 339 | 65.4 (55.3-75.4) | |
| Non-Hispanic black | 984 | 11.7 (8.1-15.3) | 759 | 11.0 (7.7-14.2) | 225 | 15.2 (7.4-23.1) | |
| Non-Hispanic Asian | 569 | 5.5 (4.1-6.9) | 469 | 5.5 (4.1-6.9) | 100 | 5.5 (2.5-8.6) | |
| Hispanic | 1118 | 16.1 (10.7-21.5) | 981 | 17.2 (10.7-23.7) | 137 | 10.9 (7.7-14.1) | |
| Family income, % federal poverty index | .25 | ||||||
| ≤130% | 1475 | 24.7 (19.2-30.1) | 1193 | 24.3 (18.7-30.0) | 282 | 26.3 (20.8-31.8) | |
| >130% | 2790 | 75.3 (69.9-80.8) | 2295 | 75.7 (70.0-81.3) | 495 | 73.7 (68.2-79.2) | |
| Education, y | .18 | ||||||
| ≤12 or GED | 2002 | 36.4 (31.6-41.1) | 1630 | 35.6 (30.6-40.7) | 372 | 39.8 (33.5-46.0) | |
| >12 | 2651 | 63.6 (58.9-68.4) | 2196 | 64.4 (59.3-69.4) | 455 | 60.2 (54.0-66.5) | |
| BMI | .55 | ||||||
| <25.0 | 1405 | 29.5 (27.5-31.4) | 1167 | 29.8 (27.8-31.9) | 238 | 27.9 (22.6-33.2) | |
| 25.0-29.9 | 1427 | 31.9 (30.0-33.9) | 1182 | 32.1 (29.8-34.4) | 245 | 30.9 (27.0-34.8) | |
| ≥30.0 | 1776 | 38.6 (36.5-40.7) | 1437 | 38.0 (35.2-40.9) | 339 | 41.2 (35.7-46.6) | |
| Physical activityh | .59 | ||||||
| Recommended | 2909 | 64.0 (62.3-65.7) | 2400 | 64.5 (62.7-66.4) | 509 | 61.6 (55.5-67.7) | |
| Intermediate | 673 | 14.1 (12.9-15.3) | 553 | 13.8 (12.5-15.1) | 120 | 15.6 (11.2-19.9) | |
| Low | 1074 | 21.9 (20.4-23.3) | 876 | 21.6 (20.3-23.0) | 198 | 22.9 (17.7-28.1) | |
| Reported reducing sodium or salt intake | .25 | ||||||
| Yes | 2336 | 45.7 (42.3-49.1) | 1936 | 46.0 (42.6-49.4) | 400 | 44.3 (38.8-51.0) | |
| No | 2319 | 54.3 (50.9-57.7) | 1892 | 54.0 (50.6-57.4) | 427 | 55.7 (49.0-61.2) | |
| Hypertension | .08 | ||||||
| Yes | 1980 | 41.0 (38.9-43.1) | 1608 | 40.1 (38.5-41.8) | 372 | 44.9 (39.7-48.8) | |
| No | 2566 | 59.0 (56.9-61.1) | 2127 | 59.9 (58.2-61.5) | 439 | 55.1 (51.2-60.3) | |
| Diabetes diagnosis | .22 | ||||||
| Yes | 500 | 8.7 (7.6-9.9) | 410 | 8.4 (7.0-9.7) | 90 | 10.4 (7.4-13.4) | |
| No | 4154 | 91.3 (90.1-92.4) | 3418 | 91.6 (90.3-93.0) | 736 | 89.6 (86.6-92.6) | |
| Chronic kidney disease | .95 | ||||||
| Yes | 591 | 12.1 (10.6-13.6) | 488 | 12.0 (10.6-13.5) | 103 | 12.2 (8.4-15.9) | |
| No | 3836 | 87.9 (86.4-89.4) | 3141 | 88.0 (86.5-89.4) | 695 | 87.8 (84.1-91.6) | |
| History of CVD | .55 | ||||||
| Yes | 300 | 5.7 (4.6-6.8) | 250 | 5.8 (4.7-6.9) | 50 | 5.3 (3.3-7.2) | |
| No | 4348 | 94.3 (93.2-95.4) | 3575 | 94.2 (93.1-95.3) | 773 | 94.7 (92.8-96.7) | |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CVD, cardiovascular disease; GED, General Educational Development; NHANES, National Health and Nutrition Examination Survey.
See Methods for definitions of participant characteristics.
Estimates based on nonpregnant US adults aged 20 to 69 years who participated in the examination component in NHANES 2013-2014.
Estimates based on the subset of participants described in footnote b who participated in 2013 or did not complete a 24-hour urine collection in 2014.
Estimates based on the subset of participants described in footnote b who completed at least one 24-hour urine collection in 2014.
Rao-Scott F-adjusted χ2 statistic comparing frequencies of participant characteristics by completion of 24-hour urine collection in 2014.
Unweighted sample size. Numbers may not add up to the totals due to missing information.
Weighted estimates and 95% CI.
Recommended physical activity was defined as 150 minutes or more per week of moderate intensity, 75 minutes or more per week of vigorous intensity, or the equivalent combination; intermediate, 10 to 149 minutes per week of moderate intensity, 5 to 74 minutes of vigorous intensity, or the equivalent combination; low, neither recommended nor moderate activity.
With further weighting of the 24-hour urine sample in 2014 for selection and nonresponse (Table 2), the study sample represented a population of whom 48.8% (95% CI, 44.8%-52.9%) were men; 63.7% (95% CI, 51.6%-75.8%) were non-Hispanic white, 15.8% (95% CI, 10.0%-21.6%) were Hispanic, 11.9% (95% CI, 5.1%-18.7%) were non-Hispanic black, and 5.6% (95% CI, 2.3%-8.9%) were non-Hispanic Asian, 43.5% (95% CI, 37.4%-49.7%) had hypertension, and 10.0% (95% CI, 6.9%-13.0%) reported diabetes diagnosis. The number of participants with missing values on demographic characteristics or CVD risk factors varied from 0 (sex, age, race and ethnic origin, physical activity, reported reducing sodium or salt intake) to 50 participants (family income). A higher percentage of men (47.6% [95% CI, 39.8%-55.4%]) than women (39.7% [95% CI, 33.2%-46.1%]) were estimated to have hypertension, P = .03.
Table 2. Estimated Population Characteristics of Those Completing the 24-Hour Urine Collection, by Sex, United States, NHANES 2014a.
| Characteristicb | No. of Participants (%) [95% CI]c | P Valued | ||
|---|---|---|---|---|
| Overall | Men | Women | ||
| Overall | 827 (100) | 421 (48.8) [44.8-52.9] | 406 (51.2) [47.1-55.2] | |
| Age, y | .50 | |||
| 20-44 | 432 (52.7) [45.6-59.7] | 217 (54.1) [47.7-60.6] | 215 (51.3) [41.6-61.0] | |
| 45-69 | 395 (47.3) [40.3-54.4] | 204 (45.9) [39.4-52.3] | 191 (48.7) [39.0-58.4] | |
| Race and Hispanic origin | .93 | |||
| Non-Hispanic white | 339 (63.7) [51.6-75.8] | 179 (64.5) [52.9-76.1] | 160 (62.9) [49.5-76.3] | |
| Non-Hispanic black | 225 (11.9) [5.1-18.7] | 114 (11.0) [4.8-17.2] | 111e | |
| Non-Hispanic Asian | 100 (5.6) [2.3-8.9] | 49e | 51 (6.0) [2.9-9.1] | |
| Hispanic | 137 (15.8) [10.0-21.6] | 66 (16.3) [10.4-22.2] | 71 (15.3) [8.8-21.9] | |
| Family income, % federal poverty guidelines | .10 | |||
| ≤130% | 282 (27.9) [20.9-34.8] | 126 (24.8) [16.3-33.4] | 156 (30.7) [23.6-37.9] | |
| >130% | 495 (72.1) [65.2-79.1] | 270 (75.2) [66.6-83.7] | 225 (69.3) [62.1-76.4] | |
| Education, y | .11 | |||
| ≤12 or GED | 372 (40.9) [33.9-47.8] | 206 (45.6) [36.1-55.1] | 166 (36.4) [27.9-44.8] | |
| >12 | 455 (59.1) [52.2-66.1] | 215 (54.4) [44.9-63.9] | 240 (63.6) [55.2-72.1] | |
| BMI | .06 | |||
| <25.0 | 238 (28.3) [23.1-33.6] | 122 (26.0) [18.6-33.4] | 116 (30.5) [24.0-37.1] | |
| 25.0-29.9 | 245 (31.1) [27.1-35.1] | 144 (36.6) [30.0-43.3] | 101 (25.9) [20.7-31.2] | |
| ≥30.0 | 339 (40.5) [34.9-46.1] | 153 (37.4) [29.1-45.7] | 186 (43.5) [36.9-50.2] | |
| Physical activityf | .17 | |||
| Recommended | 509 (61.7) [55.4-68.1] | 290 (66.8) [56.9-76.6] | 219 (56.9) [50.4-63.5] | |
| Intermediate | 120 (15.3) [10.1-20.4] | 45e | 75 (17.8) [13.5-22.2] | |
| Low | 198 (23.0) [18.2-27.7] | 86 (20.6) [15.1-26.1] | 112 (25.2) [19.1-31.4] | |
| Reported reducing sodium or salt intake | .46 | |||
| Yes | 400 (44.8) [40.6-49.0] | 195 (42.5) [33.1-52.0] | 205 (46.9) [41.9-52.0] | |
| No | 427 (55.2) [51.0-59.4] | 226 (57.5) [48.0-66.9] | 201 (53.1) [48.0-58.1] | |
| Hypertension | .03 | |||
| Yes | 372 (43.5) [37.4-49.7] | 203 (47.6) [39.8-55.4] | 169 (39.7) [33.2-46.1] | |
| No | 439 (56.5) [50.3-62.6] | 208 (52.4) [44.6-60.2] | 231 (60.3) [53.9-66.8] | |
| Diabetes diagnosis | .86 | |||
| Yes | 90 (10.0) [6.9-13.0] | 45 (9.7) [5.0-14.4] | 45 (10.2) [6.4-14.0] | |
| No | 736 (90.0) [87.0-93.1] | 376 (90.3) [85.6-95.0] | 360 (89.8) [86.0-93.6] | |
| Chronic kidney disease | .12 | |||
| Yes | 103 (11.2) [7.5-15.0] | 41 (7.9) [3.2-12.6] | 62 (14.4) [8.0-20.7] | |
| No | 695 (88.8) [85.0-92.5] | 363 (92.1) [87.4-96.8] | 332 (85.6) [79.3-92.0] | |
| History of CVD | .45 | |||
| Yes | 50 (4.4) [2.9-6.0] | 28 (5.1) [2.4-7.8] | 22 (3.8) [1.7-5.9] | |
| No | 773 (95.6) [94.0-97.1] | 390 (94.9) [92.2-97.6] | 383 (96.2) [94.1-98.3] | |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CVD, cardiovascular disease; GED, General Educational Development; NHANES, National Health and Nutrition Examination Survey.
Estimates based on nonpregnant participants aged 20 to 69 years in NHANES 2014 who completed the initial 24-hour urine collection.
See Methods for definitions of participant characteristics.
Unweighted sample size. Numbers may not add to the totals due to missing information. Weighted estimates and 95% CIs differ from Table 1. Estimates additionally weighted for selection and nonresponse in the 24-hour urine collection survey component.
Rao Scott F-adjusted χ2 statistic comparing frequency of participant characteristics by sex.
Estimate not shown, statistically unreliable based on relative standard error more than 30%.
Recommended physical activity was defined as 150 minutes or more per week of moderate intensity, 75 minutes or more per week of vigorous intensity, or the equivalent combination; intermediate, 10 to 149 minutes per week of moderate intensity, 5 to 74 minutes of vigorous intensity, or the equivalent combination; low, neither recommended nor moderate activity.
Second 24-Hour Urine Collection
Of 585 participants who were selected, 436 (75%; men, 255; women, 211) completed a second 24-hour urine collection (eTable 1 in the Supplement; Figure), 53% of the 827 participants who completed the first collection. Population characteristics, mean initial 24-hour urine volume, and mean urinary electrolyte and creatinine excretion did not vary significantly when estimated based on participants who collected 1 vs 2 complete 24-hour urine specimens (eTable 3 in the Supplement). Among participants with two 24-hour urine specimens, the ratio of within-individual to between-individual variability in sodium excretion was 1.08 overall, 0.76 among men, and 1.99 among women (eTable 4 in the Supplement). Within-individual to between-individual variability was similarly high for chloride (0.88 to 1.67), somewhat lower for potassium (0.50 to 0.66), and lowest for creatinine (0.37 to 0.40). The mean within-individual difference in 24-hour urinary sodium excretion was −47 mg (SD, 1739), and the interquartile range (IQR) was −1020 to 950. The standard deviation of within-individual differences were similar for men (1734 mg) and women (1745 mg) (eTable 5 in the Supplement).
24-Hour Urinary Sodium Excretion
Weighted mean 24-hour urinary sodium excretion was 3608 mg (95% CI, 3414-3803), n = 827 (Table 3). The median 24-hour urinary sodium excretion was 3320 mg (IQR, 2308-4524). In secondary analyses by sex, mean 24-hour urinary sodium excretion was 4205 mg (95% CI, 3959-4452) in men and 3039 mg (95% CI, 2844-3234) in women, between-group P < .001 (Table 3; eTable 6 in the Supplement). By age group, mean sodium excretion was 3699 mg (95% CI, 3449-3949) in adults aged 20 to 44 years (n = 432), and 3507 mg (95% CI, 3266-3748) in adults aged 45 to 69 years (n = 395), P = .20 (Table 3; eTable 6 in the Supplement).
Table 3. Weighted Mean and Interquartile Ranges of 24-Hour Urinary Sodium Excretion Among Nonpregnant US Adults Aged 20 to 69 Years, 2014a.
| Groupb | Overallc | Menc | Womenc | |||
|---|---|---|---|---|---|---|
| Mean (95% CI), mg | Median (IQR), mg | Mean (95% CI), mg | Median (IQR), mg | Mean (95% CI), mg | Median (IQR), mg | |
| All participants | 3608 (3414-3803) | 3320 (2308-4524) | 4205 (3959-4452) | 4050 (2813-5202) | 3039 (2844-3234) | 2857 (2131-3753) |
| Age, y | ||||||
| 20-44 | 3699 (3449-3949) | 3385 (2437-4578) | 4284 (3988-4580) | 4006 (2710-5543) | 3110 (2888-3332) | 2950 (2223-3817) |
| 45-69 | 3507 (3266-3748) | 3312 (2241-4407) | 4112 (3802-4423) | 4163 (3153-5030) | 2964 (2679-3248) | 2678 (2040-3643) |
| Race and Hispanic origin | ||||||
| Non-Hispanic white | 3602 (3354-3850) | 3371 (2271-4511) | 4241 (3960-4523) | 4059 (2982-5169) | 2977 (2745-3209) | 2667 (2000-3700) |
| Non-Hispanic black | 3606 (3281-3931) | 3121 (2334-4472) | 4009 (3718-4300) | 3613 (2544-4912) | 3272 (2849-3695) | 2965 (2218-3990) |
| Non-Hispanic Asian | 3646 (3172-4120) | 3579 (2440-4327) | 4160 (3413-4907) | 3989 (2194-4978) | 3225 (2852-3598) | 3262 (2522-3957) |
| Hispanic | 3647 (3262-4032) | 3399 (2531-4621) | 4206 (3654-4758) | 4181 (2734-5249) | 3080 (2761-3399) | 3027 (2261-3735) |
| Family income, % federal poverty index | ||||||
| ≤130% | 3475 (3207-3743) | 3139 (2169-4466) | 4085 (3623-4546) | 3911 (2547-5207) | 3010 (2781-3240) | 2719 (2021-3738) |
| >130% | 3681 (3440-3922) | 3383 (2439-4558) | 4300 (3992-4607) | 4083 (2952-5268) | 3046 (2796-3297) | 2859 (2210-3729) |
| Education, y | ||||||
| ≤12 or GED | 3728 (3431-4025) | 3504 (2316-4808) | 4270 (3930-4609) | 4193 (2891-5380) | 3080 (2794-3367) | 2896 (2180-3788) |
| >12 | 3526 (3236-3816) | 3302 (2292-4379) | 4151 (3744-4559) | 3907 (2791-4935) | 3015 (2777-3254) | 2783 (2034-3729) |
| BMI | ||||||
| <25.0 | 2841 (2643-3040) | 2591 (2016-3598) | 3064 (2728-3399) | 2784 (2194-4005) | 2662 (2480-2843) | 2526 (1885-3507) |
| 25.0-29.9 | 3691 (3378-4003) | 3484 (2334-4510) | 4245 (3920-4569) | 4193 (3046-5230) | 2948 (2620-3277) | 2675 (2133-3534) |
| ≥30.0 | 4065 (3744-4386) | 3775 (2676-5134) | 4943 (4656-5231) | 4729 (3628-5934) | 3350 (2979-3720) | 2994 (2275-4139) |
| Physical activityd | ||||||
| Recommended | 3643 (3394-3892) | 3372 (2421-4555) | 4211 (3840-4581) | 3968 (2814-5278) | 3008 (2812-3205) | 2854 (2156-3771) |
| Intermediate | 3422 (3126-3717) | 3062 (2196-4160) | 4244 (3236-5252) | 4005 (2529-4816) | 2866 (2638-3094) | 2822 (1983-3642) |
| Low | 3640 (3285-3995) | 3323 (2225-4796) | 4164 (3616-4713) | 4370 (2658-5136) | 3231 (2613-3848) | 2878 (2170-3729) |
| Reported reducing sodium or salt intake | ||||||
| Yes | 3633 (3445-3822) | 3428 (2297-4514) | 4212 (3919-4505) | 4153 (2976-5025) | 3134 (2862-3405) | 2935 (2203-4052) |
| No | 3588 (3305-3871) | 3220 (2312-4541) | 4200 (3823-4578) | 3978 (2787-5278) | 2955 (2779-3131) | 2678 (2100-3550) |
| Hypertension | ||||||
| Yes | 3757 (3518-3996) | 3319 (2239-4741) | 4465 (4116-4814) | 4026 (3024-5382) | 2956 (2599-3314) | 2676 (1953-3754) |
| No | 3452 (3252-3652) | 3275 (2364-4346) | 3904 (3622-4187) | 3985 (2645-4919) | 3082 (2900-3263) | 2859 (2243-3739) |
| Diabetes diagnosis | ||||||
| Yes | 4322 (3891-4753) | 4175 (2884-5133) | 5248 (4575-5922) | 4762 (4195-6593) | 3481 (2878-4084) | 3109 (2256-4164) |
| No | 3530 (3346-3713) | 3256 (2287-4381) | 4093 (3846-4341) | 3935 (2718-5159) | 2989 (2813-3165) | 2770 (2116-3726) |
| Chronic kidney disease | ||||||
| Yes | 3527 (3250-3804) | 3260 (2197-4783) | 4425 (3843-5007) | 4753 (3207-5056) | 3064 (2653-3474) | 2938 (1953-3959) |
| No | 3620 (3417-3823) | 3367 (2320-4508) | 4195 (3924-4466) | 4008 (2737-5230) | 3037 (2812-3262) | 2834 (2136-3741) |
| History of CVD | ||||||
| Yes | 3377 (2699-4054) | 2917 (2008-4196) | 3579 (2628-4531) | 2945 (2167-4764) | 3119 (2366-3872) | 2778 (1880-3850) |
| No | 3623 (3416-3830) | 3343 (2327-4553) | 4243 (3973-4514) | 4085 (2836-5240) | 3039 (2846-3233) | 2857 (2142-3741) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CVD, cardiovascular disease; GED, General Educational Development; IQR, interquartile range.
Based on the initial 24-hour urine specimen. Nonpregnant participants aged 20 to 69 years in the 2014 National Health and Nutrition Examination Survey who completed the initial 24-hour urine collection. See Table 2 for sample sizes. See eTable 7 in the Supplement for unweighted data.
See Methods for definitions of participant characteristics and groups.
Weighted estimates and 95% CIs.
Recommended physical activity was defined as 150 minutes or more per week of moderate intensity, 75 minutes or more per week of vigorous intensity, or the equivalent combination; intermediate, 10 to 149 minutes per week of moderate intensity, 5 to 74 minutes of vigorous intensity, or the equivalent combination; low, neither recommended nor moderate activity.
In exploratory analyses, mean 24-hour urinary sodium excretion appeared to be generally higher for adults aged 20 to 59 years compared with adults aged 60 to 69 years (eFigures 1 and 2 in the Supplement). Mean 24-hour urinary sodium excretion also appeared to vary significantly by BMI, hypertension status, and diabetes status groups (Table 3; eTable 6 in the Supplement). Unweighted means and percentiles were similar to weighted values (Table 3, eTable 7 in the Supplement).
The proportion of adults with 24-hour urinary sodium excretion greater than or equal to 2300 mg on any given day was 75.1% (95% CI, 72.0%-78.2%) overall (n = 827), 83.5% (95% CI, 79.9%-87.0%) in men (n = 421), and 67.1% (95% CI, 62.1%-72.0%) in women (n = 406) (eTable 8 in the Supplement).
24-Hour Urinary Potassium Excretion and the Sodium-to-Potassium Molar Ratio
Weighted overall mean 24-hour urinary potassium excretion was 2155 mg (95% CI, 2030-2280) (Table 4). The median was 2000 mg (IQR, 1392-2756). In secondary analyses, mean 24-hour urinary potassium excretion was 2399 mg (95% CI, 2253-2545) among men, and 1922 mg (95% CI, 1757-2086) among women, P < .001 (Table 4; eTable 9 in the Supplement). In addition, mean 24-hour urinary potassium excretion was lower among adults aged 45 to 69 years vs adults aged 20 to 44 years (Table 4; eTable 9 in the Supplement).
Table 4. Weighted Means and Percentiles of 24-Hour Urinary Potassium Excretion, US Adults, 2014a.
| Groupb | Both Sexesc | Menc | Womenc | |||
|---|---|---|---|---|---|---|
| Mean (95% CI), mg | Median (IQR), mg | Mean (95% CI), mg | Median (IQR), mg | Mean (95% CI), mg | Median (IQR), mg | |
| Overall | 2155 (2030-2280) | 2000 (1392-2756) | 2399 (2253-2545) | 2363 (1648-3102) | 1922 (1757-2086) | 1740 (1267-2345) |
| Age, y | ||||||
| 20-44 | 1986 (1878-2094) | 1853 (1278-2483) | 2194 (2067-2320) | 2211 (1499-2860) | 1777 (1627-1927) | 1674 (1200-2189) |
| 45-69 | 2343 (2151-2534) | 2145 (1532-3030) | 2642 (2405-2879) | 2521 (1890-3361) | 2074 (1832-2315) | 1879 (1328-2592) |
| Race and Hispanic origin | ||||||
| Non-Hispanic white | 2282 (2139-2424) | 2145 (1529-3026) | 2529 (2297-2762) | 2480 (1736-3237) | 2039 (1857-2221) | 1806 (1318-2493) |
| Non-Hispanic black | 1771 (1614-1928) | 1646 (1167-2216) | 1842 (1610-2074) | 1710 (1273-2188) | 1713 (1552-1873) | 1545 (1545-2235) |
| Non-Hispanic Asian | 2102 (1819-2386) | 1980 (1485-2468) | 2479 (2137-2822) | 2426 (1896-2955) | 1793 (1558-2027) | 1715 (1302-2081) |
| Hispanic | 2025 (1839-2210) | 1976 (1349-2466) | 2273 (2054-2493) | 2306 (1637-2844) | 1773 (1526-2019) | 1691 (1275-2103) |
| Family income, % federal poverty index | ||||||
| ≤130% | 1799 (1682-1917) | 1671 (1189-2350) | 1929 (1738-2120) | 1939 (1335-2484) | 1700 (1562-1839) | 1551 (1145-2124) |
| >130% | 2301 (2162-2440) | 2177 (1536-3021) | 2568 (2389-2746) | 2521 (1804-3250) | 2029 (1831-2226) | 1803 (1298-2439) |
| Education, y | ||||||
| ≤12 or GED | 1959 (1799-2119) | 1809 (1299-2454) | 2188 (2040-2335) | 2090 (1521-2797) | 1685 (1504-1867) | 1544 (1202-2011) |
| >12 | 2290 (2116-2465) | 2157 (1533-3026) | 2576 (2343-2810) | 2529 (1819-3238) | 2057 (1872-2241) | 1857 (1307-2462) |
| BMI | ||||||
| <25.0 | 2051 (1817-2284) | 1916 (1274-2640) | 2140 (1920-2360) | 2246 (1369-2861) | 1978 (1636-2321) | 1751 (1243-2375) |
| 25.0-29.9 | 2053 (1821-2285) | 1998 (1365-2585) | 2302 (2021-2583) | 2295 (1690-2858) | 1719 (1456-1982) | 1582 (1171-2152) |
| ≥30.0 | 2313 (2099-2526) | 2084 (1539-2984) | 2701 (2449-2953) | 2682 (1947-3440) | 1996 (1721-2271) | 1797 (1328-2375) |
| Physical activityd | ||||||
| Recommended | 2181 (2027-2335) | 2033 (1471-2812) | 2410 (2254-2566) | 2381 (1625-3130) | 1925 (1728-2122) | 1748 (1312-2366) |
| Intermediate | 2248 (1921-2574) | 2145 (1584-2765) | 2430 (2169-2692) | 2288 (1673-3135) | 2124 (1711-2537) | 1952 (1489-2545) |
| Low | 2022 (1820-2225) | 1844 (1173-2509) | 2345 (1893-2798) | 2350 (1641-2910) | 1770 (1452-2088) | 1488 (1145-2251) |
| Reported reducing sodium or salt intake | ||||||
| Yes | 2163 (1981-2346) | 2032 (1380-2836) | 2411 (2233-2589) | 2385 (1687-3130) | 1949 (1712-2186) | 1725 (1328-2413) |
| No | 2148 (2016-2280) | 1977 (1389-2644) | 2390 (2232-2549) | 2313 (1626-3036) | 1897 (1718-2176) | 1752 (1171-2314) |
| Hypertension | ||||||
| Yes | 2204 (2052-2356) | 2068 (1447-2761) | 2423 (2289-2558) | 2397 (1616-3040) | 1956 (1712-2199) | 1788 (1336-2329) |
| No | 2114 (1954-2274) | 1976 (1342-2726) | 2369 (2163-2575) | 2305 (1673-3129) | 1905 (1711-2100) | 1736 (1226-2367) |
| Diabetes diagnosis | ||||||
| Yes | 2346 (1909-2784) | 1816 (1398-3125) | 2560 (1900-3220) | 2400 (1508-3266) | 2152 (1642-2662) | 1596 (1369-2614) |
| No | 2134 (1987-2282) | 2001 (1391-2730) | 2382 (2225-2539) | 2349 (1671-3036) | 1896 (1726-2067) | 1754 (1228-2341) |
| Chronic kidney disease | ||||||
| Yes | 2128 (1765-2491) | 1788 (1335-2567) | 2035 (1655-2415) | 1623 (1363-2456) | 2176 (1707 2645) | 1981 (1330-2576) |
| No | 2167 (2031-2302) | 2043 (1446-2765) | 2436 (2285-2586) | 2402 (1714-3130) | 1895 (1739-2051) | 1736 (1270-2314) |
| History of CVD | ||||||
| Yes | 2325 (1821-2828) | 2128 (1146-3442) | 2436 (1476-3396) | 2257 (1108-3461) | 2184 (1485-2882) | 1812 (1223-3442) |
| No | 2146 (2022-2271) | 1995 (1405-2747) | 2399 (2253-2546) | 2379 (1689-3080) | 1909 (1752-2065) | 1737 (1268-2339) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CVD, cardiovascular disease; GED, General Educational Development; IQR, interquartile range.
Based on the initial 24-hour urine specimen. Nonpregnant participants aged 20 to 69 years in the 2014 National Health and Nutrition Examination Survey who completed an initial 24-hour urine collection. See Table 2 for sample sizes. See eTable 10 in the Supplement for unweighted data.
See Methods for definitions of participant characteristics and groups.
Weighted estimates and 95% CIs.
Recommended physical activity was defined as 150 minutes or more per week of moderate intensity, 75 minutes or more per week of vigorous intensity, or the equivalent combination; intermediate, 10 to 149 minutes per week of moderate intensity, 5 to 74 minutes of vigorous intensity, or the equivalent combination; low, neither recommended nor moderate activity.
In exploratory analyses, mean 24-hour urinary potassium excretion varied significantly between groups defined by race and Hispanic origin, income, education, and BMI (in men) (Table 4; eTable 9 in the Supplement). Unweighted means and percentiles were generally similar to weighted values (Table 4; eTable 10 in the Supplement).
The overall mean sodium-to-potassium molar ratio was 3.17 (95% CI, 2.91-3.43); the median was 2.87 (IQR, 2.05-3.93) (eTable 11 in the Supplement). In secondary analyses, the mean sodium-to-potassium molar ratio was similar by sex (eTables 11 and 12 in the Supplement). Both overall and among sex subgroups, the molar ratio was higher among adults aged 20 to 44 years vs 45 to 69 years (eTables 11 and 12 in the Supplement).
Sensitivity Analyses
The estimated percentage of adults with potentially complete 24-hour urine collection, defined as measured 24-hour urinary creatinine more than 70% of expected, varied by criteria for estimating expected urinary creatinine (eg, based on sex and weight) and among population subgroups (eTable 13 in the Supplement). After excluding 24-hour urine specimens for potentially incomplete collection based on 0.7 or less of observed divided by expected urinary creatinine based on equations published by Joossens and Geboers and Mage et al equations, mean 24-hour urinary sodium excretion was 3879 mg (95% CI, 3637-4121) and 3688 mg (95% CI, 3461-3915) and mean potassium excretion was 2305 mg (95% CI, 2162-2448) and 2229 mg (95% CI, 2099-2359), respectively (eTable 14 in the Supplement).
With and without multiple imputation for missing values, population estimates for mean urinary electrolyte excretion were similar (eg, mean 24-hour urinary sodium excretion: 3506 mg [95% CI, 3223-3789] with multiple imputation and 3527 mg [95% CI, 3250-3820] without multiple imputation) for adults with chronic kidney disease (eTable 15 in the Supplement).
Twenty-nine percent (95% CI, 22.3%-35.8%) of adults were estimated to have hypertension when it was defined by systolic blood pressure of 140 mm Hg or more or diastolic blood pressure of 90 mm Hg or more or antihypertensive medication use (eTable 16 in the Supplement). Mean 24-hour urinary sodium excretion was higher among hypertensive vs normotensive men and potassium excretion was higher among prehypertensive vs normotensive adults overall, but not among sex subgroups (eTable 16 in the Supplement).
In NHANES 2013-2014, means based on 24-hour dietary recall data for nonpregnant adults aged 20 to 69 years were 3607 mg (95% CI, 3541-3672) for dietary sodium, 2189 kcal (95% CI, 2148-2231) for energy, and 1699 mg/1000 kcal (95% CI, 1670-1729) for sodium density (eTable 17 in the Supplement). Mean dietary sodium intake was higher in men (4175 mg [95% CI, 4061-4290]) than women (3044 [95% CI, 2994-3094]), P < .001. Mean sodium density in men (1696 mg/1000 kcal [95% CI, 1668-1723]) was similar to that for women (1703 [95% CI, 1653-1754]), P = .78.
Discussion
In a 2014 cross-sectional sample of US adults aged 20 to 69 years, mean sodium intake was estimated based on 24-hour urinary sodium excretion. Given studies indicating about 90% of sodium consumed was excreted in urine, mean intake may be about 4000 mg per day (ie, 3608 mg/0.90 = 4008 mg). Mean 24-hour urinary potassium excretion was 46% of the 2005 IOM adequate intake level of 4700 mg daily and less than 3510 mg per day, the minimum level suggested in 2012 by the World Health Organization to reduce blood pressure and risk of cardiovascular diseases. However, the fraction of potassium intake excreted in urine is known to be highly variable, and may be as little as half the amount consumed. In addition, organizations and individuals disagree on recommended and upper levels for dietary sodium and potassium. The recommended intake and upper levels for dietary sodium and potassium are currently under review by the National Academies.
Mean sodium intake and potassium excretion estimates among US adults in 2014, overall and among demographic and CVD risk groups, were generally within the range of previous estimates based on 24-hour urine collection in convenience-based or population-based samples representing smaller geographic areas of the US collected in 2011 or earlier. Mean 24-hour urinary sodium-to-potassium molar ratio in this study was within the range of estimates (2.77 to 4.78) from US locations in the 1984-1987 International Study of Sodium, Potassium, and Blood Pressure (INTERSALT) study. Mean sodium intake estimates from 24-hour urine specimens in 2014 also were generally comparable with intake estimates based on NHANES 2013-2014 dietary data for nonpregnant adults aged 20 to 69 years.
Based on both dietary data and previous biomarker (24-hour urinary excretion and doubly labeled water) data in other samples of US adults, higher sodium intake in men was likely related to higher energy intake, rather than a more sodium-dense diet (ie, higher consumption of sodium per calorie). The lack of a significant difference in 24-hour urinary sodium excretion by broad age groups may be related to small sample size or to the exclusion of older adults. Consistent with a previous study, 24-hour urinary sodium excretion in the current study was not significantly lower by age except among the oldest age group.
Differences and similarities in exploratory analyses of mean 24-hour urinary sodium and potassium excretion among adults with different demographic characteristics, CVD risks, or self-reported efforts to reduce sodium or salt intake may be related to several factors. These factors include, the lack of temporality due to the cross-sectional survey design, small sample sizes across subgroups, presence of confounding (eg, by weight status or older age), differences in electrolyte retention or excretion, or ineffective individual efforts to reduce dietary sodium or salt intake. A companion cross-sectional analysis with NHANES 2014 24-hour urine data indicated higher sodium and lower urinary potassium excretion were positively associated with blood pressure in a dose-response relationship after adjusting for demographic characteristics and CVD risk factors.
This study has several strengths: (1) use of a nationally representative sample; (2) in-person start and stop of 24-hour urine collection for most participants (n = 782) to try to ensure accurate timing; (3) collection of 24-hour urine across weekdays and weekends as well as all seasons of the year; and (4) collection of a second, nonconsecutive, 24-hour urine specimen by 53% of participants to estimate within-individual, day-to-day variability in 24-hour urinary electrolyte excretion.
Limitations
This study also has several limitations. Although electrolyte estimates were weighted to account for sampling and nonresponse, it was not possible to account for all potential sources of bias. Second, although the national estimates from the 24-hour urine study participants were generally similar to that of the entire sample of examined nonpregnant participants aged 20 to 69 years in the NHANES 2013-2014 cycle, nonresponse and small sample sizes could limit the generalizability of results particularly among subgroups with low response rates (eg, non-Hispanic Asians). In addition, a plausible reason for the lack of significant differences in mean 24-hour urinary sodium and potassium excretion between population subgroups was inadequate statistical power due to small sample size. Third, incomplete collection of 24-hour urine might have resulted in lower estimated sodium and potassium excretion. However, detailed verbal, pictorial, and written collection instructions, along with exclusion of participants with potentially incomplete urine collection, helped ensure complete collection, and sensitivity analyses to exclude potential incomplete collection did not meaningfully change results. Fourth, within-individual variability in 24-hour urinary sodium excretion was almost as great as or greater than between-individual variability, consistent with previous studies. Thus, a single 24-hour urine collection may not represent an individual’s usual long-term daily sodium intake. The population estimates of the mean and medians should not be affected by random within-individual variability, but the proportion of adults in the population with usual sodium intake of 2300 mg or more may be underestimated based on a single 24-hour urine. Fifth, unaccounted variability in potassium excretion (eg, due to diuretic use and exclusion of adults 70 years or older) could reduce generalizability to all US adults.
Conclusions
In cross-sectional data from a 2014 sample of US adults, estimated mean sodium intake was 3608 mg per day. The findings provide a benchmark for future studies.
eMethods.
eTable 1. Participation Status and 24-Hour Urine Values by Specimen, NHANES 2014
eTable 2. 24-Hour Urine Collection Completion Rates by Participant Characteristics, NHANES 2014
eTable 3. Weighted Characteristics and Urine Values by Number of Completed 24-Hour Urine Specimens
eTable 4. Within- to Between-Individual Variance in 24-Hour Urinary Electrolyte or Creatinine Excretion
eTable 5. Within-Individual Difference in 24-Hour Urinary Sodium Excretion
eTable 6. P Value Comparing Weighted Mean 24-Hour Urinary Sodium Excretion by Group
eTable 7. Unweighted Mean and Percentiles of 24-Hour Urinary Sodium Excretion, NHANES 2014
eTable 8. Weighted Proportion of Adults With 24-Hour Urinary Sodium Excretion >2300 mg, NHANES 2014
eTable 9. P Value Comparing Weighted Mean 24-Hour Urinary Potassium Excretion by Group
eTable 10. Unweighted Mean and Percentiles of 24-Hour Urinary Potassium Excretion, NHANES 2014
eTable 11. Weighted Mean and Percentiles, Ratio of 24-Hour Urinary Sodium-to-Potassium Excretion, US Adults, 2014
eTable 12. P Value Comparing Weighted Mean Ratio of 24-Hour Urinary Sodium-to-Potassium Excretion by Group
eTable 13. Weighted Proportion of Adults With >70% of Expected 24-Hour Urinary Creatinine Excretion
eTable 14. Weighted Mean Urinary Electrolyte Excretion, Adults With >70% of Expected Creatinine Excretion
eTable 15. Weighted Mean 24-Hour Urinary Electrolyte Excretion With and Without Multiple Imputation
eTable 16. Weighted Mean 24-Hour Urinary Electrolyte Excretion by Hypertension Status, US Adults, 2014
eTable 17. Weighted Mean Dietary Sodium, Energy, and Sodium Density, NHANES 2013-2014
eFigure 1. Weighted Mean 24-Hour Urinary Sodium Excretion by Age Group, NHANES 2014
eFigure 2. Weighted Mean 24-Hour Urinary Sodium Excretion by Age Group and Sex, NHANES 2014
eFigure Legends.
eReferences.
References
- 1.Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325. [DOI] [PubMed] [Google Scholar]
- 3.Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet vs high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2017;4:CD004022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine Strategies to Reduce Sodium Intake in the United States. Washington, DC: National Academies Press; 2010. [Google Scholar]
- 5.Institute of Medicine Institute of Medicine, Panel on Dietary Reference Intakes for Electrolytes and Water: Dietary Reference Intakes for Water, Potassium Sodium, Chloride, and Sulfate. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 6.Thompson FE, Kirkpatrick SI, Subar AF, et al. The National Cancer Institute’s dietary assessment primer: a resource for diet research. J Acad Nutr Diet. 2015;115(12):1986-1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harnack LJ, Cogswell ME, Shikany JM, et al. Sources of sodium in US adults from 3 geographic regions. Circulation. 2017;135(19):1775-1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernstein AM, Willett WC. Trends in 24-h urinary sodium excretion in the United States, 1957-2003: a systematic review. Am J Clin Nutr. 2010;92(5):1172-1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Freedman LS, Commins JM, Moler JE, et al. Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for potassium and sodium intake. Am J Epidemiol. 2015;181(7):473-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turban S, Thompson CB, Parekh RS, Appel LJ. Effects of sodium intake and diet on racial differences in urinary potassium excretion: results from the Dietary Approaches to Stop Hypertension (DASH)-Sodium trial. Am J Kidney Dis. 2013;61(1):88-95. [DOI] [PubMed] [Google Scholar]
- 11.Cogswell ME, Wang CY, Chen TC, et al. Validity of predictive equations for 24-h urinary sodium excretion in adults aged 18-39 y. Am J Clin Nutr. 2013;98(6):1502-1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allen NB, Zhao L, Loria CM, et al. The validity of predictive equations to estimate 24-hour sodium excretion: the MESA and CARDIA Urinary Sodium Study. Am J Epidemiol. 2017;186(2):149-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Angell SY, Yi S, Eisenhower D, et al. Sodium intake in a cross-sectional, representative sample of New York City adults. Am J Public Health. 2014;104(12):2409-2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National health and nutrition examination survey: plan and operations, 1999-2010. Vital Health Stat 1. 2013;(56):1-37. [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention National Center for Health Statistics: National Health and Nutrition Examination Survey: NHANES 2013-2014. https://wwwn.cdc.gov/nchs/nhanes/ContinuousNhanes/Default.aspx?BeginYear=2013. Accessed May 1, 2017.
- 16.Centers for Disease Control and Prevention. National Center for Health Statistics: National Health and Nutrition Examination Survey: questionnaires, datasets, and related documentation. response rates. https://wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx. Accessed May 2, 2017.
- 17.National Center for Health Statistics, Centers for Disease Control and Prevention National Health and Nutrition Examination Survey: 24-hour urine study procedures manual. https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/manuals/24_Hour_Urine_Study_Procedures_Manual.pdf. Accessed May 1, 2017.
- 18.Terry AL, Cogswell ME, Wang CY, et al. Feasibility of collecting 24-h urine to monitor sodium intake in the National Health and Nutrition Examination Survey. Am J Clin Nutr. 2016;104(2):480-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention National Center for Environmental Health: laboratory procedures manual. https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/labmethods/URLT_H_R_MET_Electrolytes.pdf. Accessed May 5, 2017.
- 20.National Health and Nutrition Examination Survey Laboratory procedure manual. https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/labmethods/U1KM_H_R_MET_CREATININE.pdf. Accessed May 5, 2017.
- 21.National Center for Health Statistics, Centers for Disease Control and Prevention National Health and Nutrition Examination Survey: 2014-2014 Data documentation, codebook, and frequencies. https://wwwn.cdc.gov/Nchs/Nhanes/limited_access/UR1_H_R.htm. Accessed May 1, 2017.
- 22.Kidney Disease: Improving Global Outcomes (KDIGO) CKD WorkGroup KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1-150. https://guideline.gov/summaries/summary/46510/kdigo-2012-clinical-practice-guideline-for-the-evaluation-and-management-of-chronic-kidney-disease. Accessed February 20, 2018. [Google Scholar]
- 23.Levey AS, Stevens LA, Schmid CH, et al. ; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) . A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604-612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whelton P, Carey RM, Aronow WS, et al. 2107 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online November 13, 2017]. Hypertension. doi: 10.1161/HYP.0000000000000065 [DOI] [Google Scholar]
- 25.Crim MT, Yoon SS, Ortiz E, et al. National surveillance definitions for hypertension prevalence and control among adults. Circ Cardiovasc Qual Outcomes. 2012;5(3):343-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.US Department of Agriculture, Agricultural Research Service Food Surveys Research Group: AMPM—USDA automated multiple-pass method. https://www.ars.usda.gov/services/docs.htm?docid=7710. Accessed February 20, 2018.
- 27.US Department of Agriculture, Agricultural Research Service Food Surveys Research Group: Food and Nutrient Database for Dietary Studies. https://www.ars.usda.gov/northeast-area/beltsville-md/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fndds/. Accessed February 20, 2018.
- 28.Johnson CL, Paulose-Ram R, Ogden CL, et al. National Health and Nutrition Examination Survey: analytic guidelines, 1999-2010. Vital Health Stat 2. 2013:(161):1-24. [PubMed] [Google Scholar]
- 29.Sun Q, Bertrand KA, Franke AA, Rosner B, Curhan GC, Willett WC. Reproducibility of urinary biomarkers in multiple 24-h urine samples. Am J Clin Nutr. 2017;105(1):159-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lerchl K, Rakova N, Dahlmann A, et al. Agreement between 24-hour salt ingestion and sodium excretion in a controlled environment. Hypertension. 2015;66(4):850-857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Joossens JV, Geboers J. Monitoring salt intake of the population: methodological considerations. In: de Backer HvGG, Pedoe HT, Ducimetière P, eds. Surveillance of the dietary habits of the population with regard to cardiovascular diseases, EURO Nut Report 2. 1984;61-73. doi: 10.1002/food.19840281012 [DOI]
- 32.Mage DT, Allen RH, Kodali A. Creatinine corrections for estimating children’s and adult’s pesticide intake doses in equilibrium with urinary pesticide and creatinine concentrations. J Expo Sci Environ Epidemiol. 2008;18(4):360-368. [DOI] [PubMed] [Google Scholar]
- 33.Berglund PA. Multiple imputation using the fully condition specification method: a comparison of SAS, Stata, IVEware, and R. https://support.sas.com/resources/papers/proceedings15/2081-2015.pdf. Accessed January 1, 2018.
- 34.Liu K, Cooper R, Soltero I, Stamler J. Variability in 24-hour urine sodium excretion in children. Hypertension. 1979;1(6):631-636. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization Guideline: potassium intake for adults and children. http://apps.who.int/iris/bitstream/10665/77986/1/9789241504829_eng.pdf. Accessed February 20, 2018. [PubMed]
- 36.World Health Organization Guideline: sodium intake for adults and children. http://apps.who.int/iris/bitstream/10665/77985/1/9789241504836_eng.pdf. Accessed February 20, 2018. [PubMed]
- 37.National Academies of Sciences, Engineering, and Medicine Review of the dietary reference intakes for sodium and potassium. http://nationalacademies.org/hmd/Activities/Nutrition/ReviewDRIforSodiumandPotassium.aspx. Accessed January 1, 2018.
- 38.Intersalt Cooperative Research Group Intersalt: an international study of electrolyte excretion and blood pressure: results for 24-hour urinary sodium and potassium excretion. BMJ. 1988;297(6644):319-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jackson SL, Cogswell ME, Zhao L, et al. Association between urinary sodium and potassium excretion and blood pressure among adults in the United States. Circulation. 2018;137(3):237-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eTable 1. Participation Status and 24-Hour Urine Values by Specimen, NHANES 2014
eTable 2. 24-Hour Urine Collection Completion Rates by Participant Characteristics, NHANES 2014
eTable 3. Weighted Characteristics and Urine Values by Number of Completed 24-Hour Urine Specimens
eTable 4. Within- to Between-Individual Variance in 24-Hour Urinary Electrolyte or Creatinine Excretion
eTable 5. Within-Individual Difference in 24-Hour Urinary Sodium Excretion
eTable 6. P Value Comparing Weighted Mean 24-Hour Urinary Sodium Excretion by Group
eTable 7. Unweighted Mean and Percentiles of 24-Hour Urinary Sodium Excretion, NHANES 2014
eTable 8. Weighted Proportion of Adults With 24-Hour Urinary Sodium Excretion >2300 mg, NHANES 2014
eTable 9. P Value Comparing Weighted Mean 24-Hour Urinary Potassium Excretion by Group
eTable 10. Unweighted Mean and Percentiles of 24-Hour Urinary Potassium Excretion, NHANES 2014
eTable 11. Weighted Mean and Percentiles, Ratio of 24-Hour Urinary Sodium-to-Potassium Excretion, US Adults, 2014
eTable 12. P Value Comparing Weighted Mean Ratio of 24-Hour Urinary Sodium-to-Potassium Excretion by Group
eTable 13. Weighted Proportion of Adults With >70% of Expected 24-Hour Urinary Creatinine Excretion
eTable 14. Weighted Mean Urinary Electrolyte Excretion, Adults With >70% of Expected Creatinine Excretion
eTable 15. Weighted Mean 24-Hour Urinary Electrolyte Excretion With and Without Multiple Imputation
eTable 16. Weighted Mean 24-Hour Urinary Electrolyte Excretion by Hypertension Status, US Adults, 2014
eTable 17. Weighted Mean Dietary Sodium, Energy, and Sodium Density, NHANES 2013-2014
eFigure 1. Weighted Mean 24-Hour Urinary Sodium Excretion by Age Group, NHANES 2014
eFigure 2. Weighted Mean 24-Hour Urinary Sodium Excretion by Age Group and Sex, NHANES 2014
eFigure Legends.
eReferences.