This randomized clinical noninferiority trial assesses a novel 3-dimensional stent retriever when used in conjunction with aspiration-based mechanical thrombectomy compared with aspiration-based mechanical thrombectomy alone in patients with acute ischemic stroke.
Key Points
Question
What are the treatment effects of a 3-dimensional stent retriever in conjunction with local aspiration-based mechanical thrombectomy vs aspiration-based thrombectomy alone as a primary modality for endovascular stroke intervention?
Findings
In this randomized clinical trial of 198 patients, aspiration-assisted stent retrieval was demonstrated to be noninferior in safety and effectiveness compared with direct aspiration for stroke intervention.
Meaning
Aspiration is a reasonable frontline therapy choice in stroke thrombectomy, in addition to stent retrieval.
Abstract
Importance
The treatment effects of individual mechanical thrombectomy devices in large-vessel acute ischemic stroke (AIS) remain unclear.
Objective
To determine whether the novel 3-dimensional (3-D) stent retriever used in conjunction with an aspiration-based mechanical thrombectomy device (Penumbra System; Penumbra) is noninferior to aspiration-based thrombectomy alone in AIS.
Design, Setting, and Participants
This randomized, noninferiority clinical trial enrolled patients at 25 North American centers from May 19, 2012, through November 19, 2015, with follow-up for 90 days. Adjudicators of the primary end points were masked to treatment allocation. Patients with large-vessel intracranial occlusion AIS presenting with a National Institutes of Health Stroke Scale (NIHSS) score of at least 8 within 8 hours of onset underwent 1:1 randomization to 3-D stent retriever with aspiration or aspiration alone. The primary analyses were conducted in the intention-to-treat population.
Interventions
Mechanical thrombectomy using intracranial aspiration with or without the 3-D stent retriever.
Main Outcomes and Measures
The primary effectiveness end point was the rate of a modified Thrombolysis in Cerebral Infarction (mTICI) grade of 2 to 3 with a 15% noninferiority margin. Device- and procedure-related serious adverse events at 24 hours were the primary safety end points.
Results
Of 8082 patients screened, 198 patients were enrolled (111 women [56.1%] and 87 men [43.9%]; mean [SD] age, 66.9 [13.0] years) and randomized, including 98 in the 3-D stent retriever with aspiration group and 100 in the aspiration alone group; an additional 238 patients were eligible but not enrolled. The median baseline NIHSS score was 18.0 (interquartile range, 14.0-23.0). Eighty-two of 94 patients in the 3-D stent retriever and aspiration group (87.2%) had an mTICI grade of 2 to 3 compared with 79 of 96 in the aspiration alone group (82.3%; difference, 4.9%; 90% CI, −3.6% to 13.5%). None of the other measures were significantly different between the 2 groups. Device-related serious adverse events were reported by 4 of 98 patients in the 3-D stent retriever with aspiration group (4.1%) vs 5 of 100 patients in the aspiration only group (5.0%); procedure-related serious adverse events, 10 of 98 (10.2%) vs 14 of 100 (14.0%). A 90-day modified Rankin Scale score of 0 to 2 was reported by 39 of 86 patients in the 3-D stent retriever with aspiration group (45.3%) vs 44 of 96 patients in the aspiration only group (45.8%).
Conclusions and Relevance
The present study provides class 1 evidence for the noninferiority of the 3-D stent retriever with aspiration vs aspiration alone in AIS. Future trials should evaluate whether these results can be generalized to other stent retrievers.
Trial Registration
clinicaltrials.gov Identifier: NCT01584609
Introduction
Current US Food and Drug Administration (FDA)–cleared reperfusion therapies for acute ischemic stroke (AIS) are limited to the intravenous administration of alteplase, which is a human tissue plasminogen activator, within 3 hours from symptom onset and the use of endovascular mechanical thrombectomy devices within 8 hours from ictus, including stent retrievers and an aspiration-based mechanical thrombectomy device (Penumbra System; Penumbra). Until recently, only intravenous alteplase was supported by class 1A evidence as a treatment for AIS, whereas the utility of mechanical thrombectomy devices was not widely accepted. Subsequently, 6 randomized clinical trials (RCTs), including Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands (MR CLEAN), Endovascular Treatment for Small Core and Proximal Occlusion Ischemic Stroke (ESCAPE), Extending the Time for Thrombolysis in Emergency Neurological Deficits—Intra-Arterial (EXTEND-IA), Solitaire With the Intention for Thrombectomy as Primary Endovascular Treatment (SWIFT PRIME), Endovascular Revascularization With Solitaire Device Versus Best Medical Therapy in Anterior Circulation Stroke Within 8 Hours (REVASCAT), and Trial and Cost Effectiveness Evaluation of Intra-arterial Thrombectomy in Acute Ischemic Stroke (THRACE), confirmed the superiority of mechanical thrombectomy over best medical therapy alone in improving clinical outcomes after large-vessel occlusion (LVO) strokes. In recognition, the American Heart Association updated its guidelines and recommended that for patients with anterior circulation stroke due to confirmed LVO affecting the internal carotid artery or middle cerebral artery M1 segment, mechanical thrombectomy should be undertaken as soon as possible for maximal benefit within 6 hours from symptom onset.
Most of the interventions in these trials used stent retrievers, with primary aspiration being used in only a few patients. However, current common practice combines stent retrievers and local aspiration or starts with direct aspiration alone. To date, data from RCTs are lacking a comparison of the safety and effectiveness of these 2 principal modalities in acute stroke intervention. The aim of this RCT was to determine whether the safety and efficacy of the novel Penumbra 3-dimensional (3-D) stent retriever (Penumbra, Inc) when used in conjunction with an aspiration-based mechanical thrombectomy device, was noninferior to the aspiration-base mechanical thrombectomy device alone in acute stroke intervention.
Methods
Study Design
The Penumbra Separator 3D trial was a prospective, randomized, single-blinded, active controlled, noninferiority design, multicenter study at 25 centers in the United States. The full study protocol is available in Supplement 1. Patients presenting with symptoms of AIS who had evidence of an LVO (≥2.5 mm in diameter) in the cerebral circulation underwent 1:1 randomization to the 3-D stent retriever with aspiration arm or the aspiration only arm, with the latter serving as the active control group. At the time of the trial design, no reference standards existed against which a novel stent retriever should be tested because the current state of knowledge about the superiority of the Solitaire and Trevo stent retrievers over medical treatment alone was only subsequently established. As such, the Penumbra aspiration system alone was an acceptable choice for an active control. Each treated patient was followed up for 90 days after randomization. The US FDA approved the trial protocol, and each participating center obtained local institutional review board approval. Procedures followed were in accordance with institutional guidelines. The participants or their legal representatives provided signed written informed consent.
The purpose of this study was to assess the safety and effectiveness of the 3-D stent retriever as a component of the Penumbra System in the revascularization of LVO in AIS. The goal was to demonstrate the noninferiority of the 3-D stent retriever with aspiration to aspiration alone in effecting reperfusion in ischemic stroke as defined by a posttreatment modified Thrombolysis in Cerebral Infarction (mTICI) grade of 2 to 3 (range, 0-3, with higher scores indicating a greater degree of revascularization). The margin of inferiority was set at 15%.
A data safety monitoring board (DSMB) and clinical events committee reviewed the incoming safety data on an ongoing basis, and if the DSMB thought that the risks of the intervention outweighed the benefits, the DSMB had the authority to request examination of efficacy results to assess the risk of the technology and recommend a modification to the device, a revision of the protocol, or termination of the study at its discretion. On June 23, 2016, the DSMB voted unanimously to halt further enrollment in the 3-D trial after concluding that based on the available adjudicated data for 86% of the target enrollment, the prespecified primary end points had been met and recruiting additional participants would not change the outcome of the trial.
Participants
To be included, patients had to be 18 to 85 years of age; demonstrate symptoms consistent with an AIS with a National Institutes of Health Stroke Scale (NIHSS) score of at least 8.0 (range, 0-42, with higher scores indicating greater stroke severity), be refractory to or not eligible for intravenous alteplase therapy, be expected to undergo arterial puncture within 8 hours from symptom onset, and demonstrate radiographically an LVO (≥2.5 mm in diameter) in the intracranial circulation. Exclusion criteria are described in the eMethods in Supplement 2.
Each center was required to complete 2 initial cases with the 3-D stent retriever with aspiration that were not included in trial analytics. Before enrollment, angiographic confirmation of LVO was required.
Randomization and Masking
Participants were randomly assigned using an online access tool in a 1:1 ratio to 3-D stent retriever with aspiration or aspiration alone using randomly ordered blocks of sizes 2 and 4. The schedule was stratified by center. A patient was considered to be enrolled after a treatment arm was assigned from the randomization system. Owing to the nature of the procedure, involved investigators were not masked to the treatment arm. Imaging review was performed while masked to all clinical information except stroke side.
Procedures
For patients assigned to the 3-D stent retriever with aspiration arm, the thrombectomy procedure has been previously described in detail. Similarly to other stent retrievers, the 3-D stent retriever is a laser-cut nitinol device attached to a wire pusher, but it possesses significantly less metal on its circumference and has 4 intraluminal, 3-D chambers designed to maximize clot engagement and extraction into the reperfusion catheter while minimizing contact with vessel intima. In contrast, the other stent retrievers on the market rely on their radial expansion to push the clot against the vessel wall and into the stent struts. For patients assigned to the aspiration only arm, the thrombectomy procedure by aspiration has also been described in detail elsewhere. The trial aspiration system included the second-generation 4MAX, 5MAX, and 5MAX ACE reperfusion catheters (Penumbra, Inc). In summary, an appropriately sized reperfusion catheter, with or without a separator, was used to remove the clot via pump aspiration; many cases did not involve a separator because the direct aspiration as a first pass technique (ADAPT) principle was used. The reperfusion catheter was designed to capture and evacuate the clot using aspiration, whereas the separator was designed to prevent the reperfusion catheter from clogging for automated, continuous aspiration. When used, the separator was passed back and forth at the tip of the reperfusion catheter at the proximal margin of the occlusion under aspiration. If the 3-D stent retriever with aspiration or aspiration alone was unable to revascularize the target vessel, the use of other rescue therapies was considered to be a protocol deviation. Moreover, any use of intra-arterial tissue plasminogen activator or non–FDA-approved treatments was considered to be a treatment failure.
The mTICI grades were assessed before mechanical thrombectomy and at completion of the revascularization. All patients were followed up for 90 days from the time of randomization. Patients underwent evaluation for neurologic and/or functional status immediately before randomization, at 24 hours and at 7 days (or day of discharge from the hospital, whichever was earlier) after randomization, and at 30 days (±10 days) and 90 days (±10 days) after randomization.
Outcomes
The primary study end points were angiographic revascularization of the occluded target vessel immediately after the procedure as defined by an mTICI grade of 2 or 3 and incidence of device- and procedure-related serious adverse events within 24 hours after the procedure. Angiograms were sent to an independent core laboratory masked to treatment allocation for adjudication of mTICI flow. The secondary study end points were the proportion of patients with functional independence as defined by a modified Rankin Scale (mRS) score of no greater than 2 at 90 days after the procedure (range, 0-6, with higher scores indicating greater functional disability), all-cause mortality, and the incidence of symptomatic intracranial hemorrhage (ICH). Other secondary measures included good clinical outcome at 30 days after the procedure as defined by an improvement in the NIHSS score of 10.0 points or more at discharge, an NIHSS score of 0 to 1.0 at discharge, or a 30-day mRS score of 0 to 2 and good neurologic outcome at 90 days after the procedure as defined by an mRS score of no greater than 2 or an improvement on the NIHSS score of 10.0 or more points. Follow-up non–contrast-enhanced computed tomography was performed a mean (SD) of 24 (12) hours after randomization, and scans were reviewed by the core laboratory to assess ICH based on European Cooperative Acute Stroke Study definitions. A symptomatic ICH was defined as 24-hour evidence on computed tomography of any ICH that was associated with a worsening of 4.0 points or more in the NIHSS score. In the event of death (n = 5) or unavailable NIHSS score (n = 2) at the 24-hour follow-up, the clinical events committee adjudicated the ICH.
Statistical Analysis
The sample size calculations assumed that 80% of the patients in the 3-D stent retriever with aspiration and aspiration only groups would experience success (mTICI grade, 2-3). Based on a binomial noninferiority analysis with a margin of 15%, a study of 103 patients per group would have 85% power with a 1-sided α of .05. The sample size was adjusted to 230 patients to account for attrition.
The objective of the statistical analysis was to assess whether the effectiveness of 3-D stent retriever with aspiration was noninferior to aspiration alone as defined by an mTICI grade of 2 to 3. The primary effectiveness analysis was the difference between the 3-D stent retriever with aspiration and the aspiration alone (control) groups. A binomial comparison was used to test the null hypothesis that the difference in the proportions of the groups (3-D stent retriever with aspiration minus aspiration alone) was no greater than −0.15 (ie, revascularization in the 3-D stent retriever with aspiration group is worse than in the aspiration alone group) vs the 1-sided alternative that differences in the proportions of the groups were at least −0.15. This comparison was equivalent to evaluating that the lower bound of the 90% CI for the difference was greater than −15%.
Baseline characteristics were summarized by treatment group and for the total population. Comparisons among treatment groups were performed using the Fisher exact test for categorical data and Wilcoxon rank sum test for continuous data. Exact binomial 95% CIs and comparisons are 2-sided. The level of significance was set at P < .05. Patients with intra-arterial thrombolytic use or with vessel access failure underwent analysis as treatment failures for the primary end point (mTICI grades). Most patients had the primary end point, but more patients in the 3-D stent retriever with aspiration than aspiration alone arms were missing 90-day mRS scores. Sensitivity analyses were performed, imputing participants as treatment failures. Additional details of the statistical analysis, including the statistical analysis plan, are found in eMethods in Supplement 2. Analyses were conducted using SAS software (version 9.2; SAS Institute).
Results
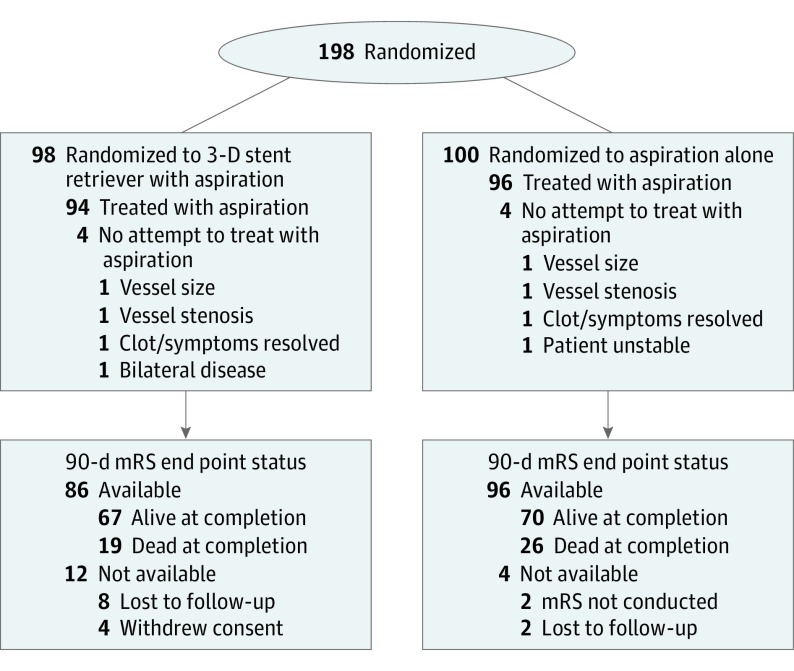
A total of 8082 patients underwent screening, of whom 198 were enrolled at 25 centers in the United States from May 19, 2012, to November 19, 2015 (87 men [43.9%] and 111 women [56.1%]; mean [SD] age, 66.9 [13.0] years). Among the enrolled patients, 98 (49.5%) were randomized to the 3-D stent retriever with aspiration arm and 100 (50.5%) to the aspiration alone arm. The CONSORT flowchart (Figure 1) summarizes patient enrollment and follow-up in the trial.
Figure 1. CONSORT Flow Diagram.
mRS indicates modified Rankin Scale; 3-D, 3-dimensional.
Baseline characteristics for the primary analysis are shown in Table 1. The intention-to-treat population included all 198 patients. The median baseline NIHSS score was 18.0 (interquartile range [IQR], 14.0-23.0), with 76 patients (38.4%) having a score of 20.0 or greater. Overall, 133 patients (67.2%) received intravenous alteplase. The median baseline non–contrast-enhanced computed tomographic Alberta Stroke Program Early CT Score was 8 (IQR, 7-9; possible range, 0-10, with higher scores indicating lack of completed infarct). Of the target vessels, 153 (77.3%) were the middle cerebral artery and 39 (19.7%) were the internal carotid artery (Table 1). Before onset of treatment, 185 of 197 patients (93.9%) had angiographic core laboratory–assessed flow mTICI grade of 0 or 1 at the site of the target occlusion. Patients presented to the participating hospital 0 to 459 minutes after symptom onset, with a median time of 111 minutes (IQR, 45-226 minutes).
Table 1. Baseline Patient Characteristics.
| Characteristic | Patient Group | ||
|---|---|---|---|
| All (N = 198) |
3-D Stent Retriever With Aspiration (n = 98) |
Aspiration Alone (n = 100) |
|
| Age, mean (SD), y | 66.9 (13.0) | 67.3 (13.6) | 66.5 (12.5) |
| Female, No./total No. (%) | 111/198 (56.1) | 57/98 (58.2) | 54/100 (54.0) |
| Baseline NIHSS scorea | |||
| Median (IQR) | 18.0 (14.0-23.0) | 18.0 (14.0-21.0) | 18.0 (14.5-23.5) |
| ≥20.0, No./total No. (%) | 76/198 (38.4) | 35/98 (35.7) | 41/100 (41.0) |
| Baseline ASPECTS, median (IQR)b | 8 (7-9) | 8 (7-9) | 8 (7-9) |
| Admission systolic blood pressure, mean (SD), mm Hg | 142.5 (20.4) | 143.1 (20.8) | 141.8 (20.1) |
| Prestroke mRS score, No. (%)c | |||
| 0 | 192/197 (97.5) | 95/97 (97.9) | 97/100 (97.0) |
| 1 | 4/197 (2.0) | 2/97 (2.1) | 2/100 (2.0) |
| Hypertension, No./total No. (%) | 155/198 (78.3) | 74/98 (75.5) | 81/100 (81.0) |
| Admission glucose level, median (IQR), mg/dL | 120 (104-146) | 122 (104-145) | 119 (104-147) |
| Diabetes, No./total No. (%) | 53/198 (26.8) | 24/98 (24.5) | 29/100 (29.0) |
| Atrial fibrillation, No./total No. (%) | 96/198 (48.5) | 52/98 (53.1) | 44/100 (44.0) |
| Site of primary occlusion determined by core laboratory, No./total No. (%) | |||
| ICA | 39/198 (19.7) | 15/98 (15.3) | 24/100 (24.0) |
| MCA M1 | 126/198 (63.6) | 65/98 (66.3) | 61/100 (61.0) |
| MCA M2 | 27/198 (13.6) | 15/98 (15.3) | 12/100 (12.0) |
| PCA | 2/198 (1.0) | 1/98 (1.0) | 1/100 (1.0) |
| Basilar | 2/198 (1.0) | 1/98 (1.0) | 1/100 (1.0) |
| Left hemisphere occlusion | 98/198 (49.5) | 39/98 (39.8) | 59/100 (59.0) |
| Stenosis proximal to the primary occlusion, No./total No. (%) | 20/197 (10.2) | 8/98 (8.2) | 12/99 (12.1) |
| Pretreatment mTICI grade 0 or 1, No./total No. (%)d | 185/197 (93.9) | 89/98 (90.8) | 96/99 (97.0) |
| Treatment with alteplase, No./total No. (%) | 133/198 (67.2) | 64/98 (65.3) | 69/100 (69.0) |
| Time from symptom onset to intravenous alteplase, median (IQR), min | 104 (85-137) | 103.5 (84-133.5) | 105 (85-155) |
| Time from onset to ED arrival, median (IQR), min | 111 (45.0-226.0) | 115.5 (43.0-205.0) | 105 (48.0-233.5) |
| Time from onset to puncture, median (IQR), min | 225.5 (171.5-327.0) | 231 (175.0-322.0) | 220.5 (165.0-329.0) |
| Time from ED arrival to puncture, median (IQR), min | 103 (60.5-143.0) | 102 (50.0-142.0) | 106 (69.0-144.0) |
| Time from CT to arterial puncture, median (IQR), min | 94 (56.0-129.0) | 95.5 (53.0-134.0) | 92 (57.0-128.0) |
| Time from puncture to mTICI reperfusion grade 2-3, median (IQR), min | 46 (31-72) | 48 (32.5-73.5) | 44 (28-70) |
| Time from puncture to mTICI reperfusion grade 2b-3, median (IQR), min | 44 (28-69) | 49 (32-73) | 39 (24-65) |
Abbreviations: ASPECTS, Alberta Stroke Program Early CT (computed tomography) Score; ED, emergency department; ICA, internal carotid artery; IQR, interquartile range; MCA, middle cerebral artery; M1, main MCA stem; M2, second-order MCA branch; mRS, modified Rankin Scale; mTICI, modified Thrombolysis in Cerebral Infarction; NIHSS, National Institutes of Health Stroke Scale; PCA, posterior cerebral artery; 3-D, 3-dimensional.
SI conversion factor: To convert glucose to millimoles per liter, multiply by 0.0555.
Scores range from 0 to 42, with higher scores indicating greater stroke severity.
Scores range from 0-10, with higher scores indicating lack of completed infarct.
Scores range from 0 to 6, with higher scores indicating greater functional disability.
Scores range from 0 to 3, with higher scores indicating a greater degree of revascularization.
In general, the baseline characteristics were similar in both treatment groups. No significant between-group differences were noted except the affected hemisphere; 39 patients in the 3-D stent retriever with aspiration group (39.8%) had a left hemisphere occlusion vs 59 in the of the aspiration only group (59.0%; P = .01). Age, baseline NIHSS and Alberta Stroke Program Early CT scores, site of arterial occlusion, and glucose levels were comparable across both treatment groups. The median time from symptom onset to reperfusion mTICI grades of 2 to 3 for all patients was 305 minutes (IQR, 221-400 minutes) (314 minutes [IQR, 221-398 minutes] for 3-D stent retriever with aspiration vs 290 minutes [IQR, 230-400 minutes] for aspiration alone). Table 1 shows additional procedural times. Stenosis was observed proximal to the primary occlusion in 20 of 197 patients (10.2%); of these 20 patients, interventions to address the stenosis were performed in 6.
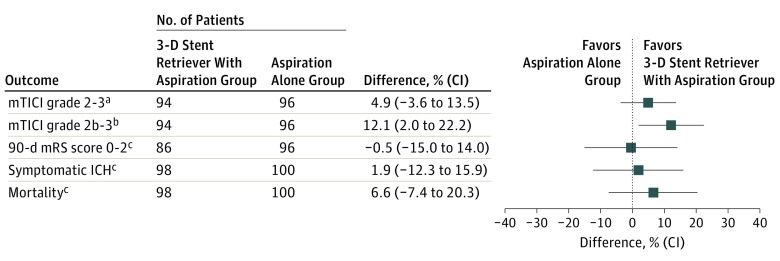
After treatment with the assigned device, the primary effectiveness outcome (flow mTICI grade, 2-3) was achieved in 161 of 190 patients (84.7%) (3-D stent retriever with aspiration: 82 of 94 [87.2%]; aspiration only: 79 of 96 [82.3%]; difference, 4.9% [90% CI, −3.6% to 13.5%]). Substantial reperfusion (mTICI grade, 2b-3) was achieved in 144 of 190 patients (75.8%) (3-D stent retriever with aspiration: 77 of 94 [81.9%]; aspiration alone: 67 of 96 [69.8%]; difference, 12.1% [90% CI, 2.0%-22.2%]) (Figure 2). End-of-procedure revascularization to an mTICI grade of 2 to 3 was achieved in 175 of 192 patients (91.1%) (3-D stent retriever with aspiration: 87 of 95 [91.6%]; aspiration alone: 88 of 97 [90.7%]; difference, −1.1% [90% CI, −11.3% to 12.6%]), with substantial improvement (mTICI grade, 2b-3) in 158 of 192 patients (82.3%) (3-D stent retriever with aspiration: 83 of 95 [87.4%]; aspiration alone: 75 of 97 [77.3%]; difference, 10.1% [90% CI, −2.0% to 21.6%]). Table 2 summarizes the immediate postprocedure results in both treatment groups.
Figure 2. Primary and Key Secondary End Point Differences Between Treatment Groups.
ICH indicates intracranial hemorrhage; mRS, modified Rankin Scale; mTICI, modified Thrombolysis in Cerebral Infarction; and 3-D, 3-dimensional.
aIndicates primary end point (with 90% CI).
bIndicates post hoc end point (with 90% CI).
cIndicates secondary end point (with 95% CI).
Table 2. Primary and Post Hoc Efficacy Outcomes.
| mTICI Grade (Analysis)a | No (%) of Patients | Difference, % (90% CI) | ||
|---|---|---|---|---|
| All (n = 198) |
3-D Stent Retriever With Aspiration (n = 98) |
Aspiration Alone (n = 100) |
||
| 2-3 (ITT) | 161/190 (84.7) | 82/94 (87.2) | 79/96 (82.3) | 4.9 (−3.6 to 13.5) |
| 2b-3 (ITT)b | 144/190 (75.8) | 77/94 (81.9) | 67/96 (69.8) | 12.1 (2.0 to 22.2) |
| 2-3 (PP) | 151/173 (87.3) | 77/87 (88.5) | 74/86 (86.0) | 2.5 (−5.9 to 10.8) |
| 2b-3 (PP)b | 137/173 (79.2) | 73/87 (83.9) | 64/86 (74.4) | 9.5 (−0.6 to 19.6) |
Abbreviations: ITT, intention to treat; mTICI, modified Thrombolysis in Cerebral Infarction; PP, per protocol; 3-D, 3-dimensional.
Scores range from 0 to 3, with higher scores indicating a greater degree of revascularization.
Indicates post hoc end points.
The primary safety end point was the incidence of device- and procedure-related serious adverse events within 24 hours of the procedure. As shown in Table 3, no significant difference occurred between treatment groups in the 24-hour device-related serious adverse event rates, including 4 of 98 patients (4.1%) in the 3-D stent retriever with aspiration group vs 5 of 100 (5.0%) in the aspiration only group. eTable 1 in Supplement 2 shows the types of device-related adverse events. The between-group differences were unremarkable. The overall rate of functional independence (mRS score, 0-2) at 90 days was 83 of 182 (45.6%), with no significant differences between the 3-D stent retriever with aspiration and aspiration alone groups (39 of 86 [45.3%] vs 44 of 96 [45.8%]; P > .99). Similarly, no significant differences in 90-day mortality occurred (3-D stent retriever with aspiration: 19 of 98 [19.4%]; aspiration alone: 26 of 100 [26.0%]; P = .31) or in the rates of symptomatic ICH (3-D stent retriever with aspiration: 3 of 98 [3.1%]; aspiration alone: 5 of 100 [5.0%]; P = .72). Good clinical outcomes at 30 days after the procedure were achieved in 113 of 197 patients (57.4%); good neurologic outcome at 90 days, in 111 of 182 patients (61.0%) (Table 3); with no difference between treatment groups.
Table 3. Safety and Secondary Outcomes.
| Outcome | No. (%) of Patients | Difference, % (95% CI) | ||
|---|---|---|---|---|
| All (n = 198) |
3-D Stent Retriever With Aspiration (n = 98) |
Aspiration Alone (n = 100) |
||
| Device-related SAE at 24 h | 9/198 (4.5) | 4/98 (4.1) | 5/100 (5.0) | −0.92 (−6.71 to 4.88) |
| Procedure-related SAE at 24 h | 24/198 (12.1) | 10/98 (10.2) | 14/100 (14.0) | −3.80 (−12.86 to 5.27) |
| All-cause mortality at 90 d | 45/198 (22.7) | 19/98 (19.4) | 26/100 (26.0) | −6.61 (−18.24 to 5.01) |
| Symptomatic ICH within 24 h | 8/198 (4.0) | 3/98 (3.1) | 5/100 (5.0) | −1.94 (−7.40 to 3.53) |
| 30-d Good clinical outcomea | 113/197 (57.4) | 58/97 (59.8) | 55/100 (55.0) | 4.79 (−9.00 to 18.59) |
| 90-d mRS score 0-2 | 83/182 (45.6) | 39/86 (45.3) | 44/96 (45.8) | −0.48 (−14.98 to 14.01) |
| 90-d Good neurologic outcomeb | 111/182 (61.0) | 56/86 (65.1) | 55/96 (57.3) | 7.82 (−6.30 to 21.94) |
Abbreviations: ICH, intracranial hemorrhage; mRS, modified Rankin Scale; SAE, serious adverse event; 3-D, 3-dimensional.
Indicates a National Institutes of Health Stroke Scale (NIHSS) score of no more than 1 or at least a 10.0-point improvement at discharge (range, −28 to 27, with positive values indicating less impairment at discharge), or a 30-d mRS score of no more than 2 (range, 0 to 6, with higher scores indicating greater functional disability).
Indicates an mRS score of no more than 2 or at least a 10.0-point improvement on the NIHSS score.
To evaluate the effect of baseline conditions on treatment effect and functional outcome, subgroup analyses were performed for the primary variable, mTICI grades of 2 to 3. The subgroups used for these analyses were age (<65 or ≥65 years), baseline NIHSS score (<20.0 or ≥20.0), and site of occlusion. We found no evidence of any significant heterogeneity of treatment effect in any of the prespecified subgroups (eFigure 1 in Supplement 2). Kaplan-Meier estimates of the probability of death among patients (per protocol) are shown in eFigure 2 in Supplement 2. There was no significant difference in mRS score distributions (eFigure 3 in Supplement 2) or baseline characteristics and process times (eTable 2 in Supplement 2). Per-protocol analyses of primary and secondary outcomes are detailed in Supplement 2 (eTables 3 and 4). Additional study details are provided in eTables 5 to 10 in Supplement 2.
Discussion
Despite the evidence supporting endovascular treatment in AIS, the comparative safety and effectiveness of the individual FDA-approved mechanical thrombectomy devices remain unclear. Furthermore, growing evidence suggests that aspiration might be an equally safe and effective initial strategy during mechanical thrombectomy.
Our study demonstrates that aspiration-assisted stent retrieval using the 3-D stent retriever is not inferior to direct aspiration alone for revascularization of LVO strokes. Our results indicate that the difference in achieving mTICI grades of 2 to 3 between intervention arms was small at 4.9%, with a lower bound of the 90% CI of −3.6%, well within the prespecified margin for noninferiority of −15% (Table 2 and Figure 1). Similarly, the rates of device-related serious adverse events were almost identical, and other safety measures were comparable (Table 3). Based on these data, we conclude that the 3-D stent retriever used in conjunction with aspiration is noninferior to the aspiration system alone.
In the control arms of 5 recently published RCTs, functional independence rates were found to range from 26% to 32%. In the meta-analysis of MR CLEAN, ESCAPE, EXTEND-IA, SWIFT PRIME, and REVASCAT from the Highly Effective Reperfusion evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration, in the control group (n = 653), 26.5% achieved functional independence, whereas in the endovascular thrombectomy group (n = 634), which primarily used currently available stent retrievers, 46% achieved functional independence and 71% achieved reperfusion to mTICI grades of 2b or 3. The HERMES authors highlighted that “stent-retrievers were the main device used across all 5 trials thus stent-retrievers constitute the benchmark against which future thrombectomy approaches should be measured.”(p1729) A single RCT that focused on thromboaspiration as the primary endovascular treatment modality vs best medical therapy (The Randomized, Concurrent Controlled Trial to Assess the Penumbra System’s Safety and Effectiveness in the Treatment of Acute Stroke [THERAPY]) was halted early after loss of equipoise. Although failing to reach significance for aspiration, the directions of effect for all prespecified outcomes were suggestive of a potential benefit.
Our study compares well with the HERMES analyses of efficacy. Functional independence as measured using an mRS score of no greater than 2 occurred in 45.6%, with no significant differences between the 3-D stent retriever with aspiration and aspiration alone groups (45.3% vs 45.8%; P > .99). Similarly, we achieved reperfusion using the benchmark of mTICI grades of 2b to 3 in 75.8% (3-D stent retriever with aspiration: 81.9%; aspiration alone: 69.8%; P = .06). These findings suggest that primary stent retrieval with aspiration and primary aspiration alone may be reasonable initial strategies for revascularization during mechanical thrombectomy for LVO causing AIS. Aspiration as a primary treatment modality may acquire greater significance if the initial studies suggesting that aspiration alone may be a more cost-effective choice as frontline therapy are confirmed. Larger studies are therefore needed to further explore the clinical efficacy and cost-effectiveness of the different mechanical strategies.
Limitations
Similar to recent randomized endovascular stroke trials, a major limitation of this study is that the participating investigators were not masked to the treatment arm. Use of masked core laboratory staff for the primary trial end points and a clinical events committee minimizes any potential bias inherent in an open label trial. In addition, although at the time of the planning of our trial an mTICI reperfusion grade of 2 to 3 was an acceptable primary end point, the current standards are higher and include mTICI grades 2b and 3 only. As such, we performed a post hoc analysis for the mTICI grade 2b to 3 end point, which suggested that we would have similarly met the stipulated noninferiority requirements. Of importance, although this trial provides the first direct comparison of a stent retriever vs aspiration system, these results are specific to the 3-D stent retriever and should not be extrapolated to other stent retriever devices. This issue has been addressed by another confirmatory trial. Finally, our noninferiority margin of 15% may have been too wide, because such a difference in reperfusion rates could lead to significant differences in clinical outcomes.
Conclusions
The Penumbra Separator 3D RCT provides the first class 1 evidence, to our knowledge, comparing the treatment effects of a 3-D stent retriever when used with aspiration vs aspiration alone. The results of both arms appear comparable and seem to be within a similar range of outcomes from the treatment arms of the recent positive endovascular RCTs.
Trial Protocol
eMethods. Exclusion Criteria, Device Use, and Statistical Analysis
eTable 1. Device-Related Adverse Events (Intention to Treat)
eTable 2. Baseline Patient Characteristics and Process Times (Per Protocol)
eTable 3. Primary Outcomes (Per Protocol)
eTable 4. Safety and Secondary Outcomes (Per Protocol)
eTable 5. Definition and Distribution of mTICI Scores (Intention to Treat)
eTable 6. Number of Patients Randomized by Center
eTable 7. Comparison of Baseline Characteristics of Analyzed and Missing Data (Intention to Treat)
eTable 8. mRS Sensitivity Analyses (Intention to Treat)
eTable 9. Screening Results
eTable 10. Classification of Intracebral Hemorrhages
eFigure 1. Distribution of Primary End Point (mTICI 2-3) Treatment Effect Across the Prespecified Subgroups (Intention to Treat)
eFigure 2. Kaplan-Meier Estimates of the Probability of Death in Patients (Intention to Treat)
eFigure 3. Functional outcomes at 90 days, According to Modified Rankin Scale Score (Intention to Treat)
References
- 1.Hacke W, Kaste M, Bluhmki E, et al. ; ECASS Investigators . Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-1329. [DOI] [PubMed] [Google Scholar]
- 2.Smith WS, Sung G, Starkman S, et al. ; MERCI Trial Investigators . Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke. 2005;36(7):1432-1438. [DOI] [PubMed] [Google Scholar]
- 3.Penumbra Pivotal Stroke Trial Investigators The Penumbra Pivotal Stroke Trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009;40(8):2761-2768. [DOI] [PubMed] [Google Scholar]
- 4.Saver JL, Jahan R, Levy EI, et al. ; SWIFT Trialists . Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012;380(9849):1241-1249. [DOI] [PubMed] [Google Scholar]
- 5.Nogueira RG, Lutsep HL, Gupta R, et al. ; TREVO 2 Trialists . Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012;380(9849):1231-1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berkhemer OA, Fransen PS, Beumer D, et al. ; MR CLEAN Investigators . A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20. [DOI] [PubMed] [Google Scholar]
- 7.Goyal M, Demchuk AM, Menon BK, et al. ; ESCAPE Trial Investigators . Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030. [DOI] [PubMed] [Google Scholar]
- 8.Campbell BC, Mitchell PJ, Kleinig TJ, et al. ; EXTEND-IA Investigators . Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018. [DOI] [PubMed] [Google Scholar]
- 9.Saver JL, Goyal M, Bonafe A, et al. ; SWIFT PRIME Investigators . Stent-retriever thrombectomy after intravenous t-PA vs t-PA alone in stroke. N Engl J Med. 2015;372(24):2285-2295. [DOI] [PubMed] [Google Scholar]
- 10.Jovin TG, Chamorro A, Cobo E, et al. ; REVASCAT Trial Investigators . Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296-2306. [DOI] [PubMed] [Google Scholar]
- 11.Bracard S, Ducrocq X, Mas JL, et al. ; THRACE investigators . Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15(11):1138-1147. [DOI] [PubMed] [Google Scholar]
- 12.Powers WJ, Derdeyn CP, Biller J, et al. ; American Heart Association Stroke Council . 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(10):3020-3035. [DOI] [PubMed] [Google Scholar]
- 13.Behme D, Kowoll A, Mpotsaris A, et al. . Multicenter clinical experience in over 125 patients with the Penumbra Separator 3D for mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. 2016;8(1):8-12. [DOI] [PubMed] [Google Scholar]
- 14.Mpotsaris A, Bussmeyer M, Weber W. Mechanical thrombectomy with the Penumbra 3D separator and lesional aspiration: technical feasibility and clinical outcome. Clin Neuroradiol. 2014;24(3):245-250. [DOI] [PubMed] [Google Scholar]
- 15.Turk AS, Spiotta A, Frei D, et al. . Initial clinical experience with the ADAPT technique: a direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg. 2014;6(3):231-237. [DOI] [PubMed] [Google Scholar]
- 16.Turk AS, Frei D, Fiorella D, et al. . ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2014;6(4):260-264. [DOI] [PubMed] [Google Scholar]
- 17.Zaidat OO, Yoo AJ, Khatri P, et al. ; Cerebral Angiographic Revascularization Grading (CARG) Collaborators; STIR Revascularization Working Group; STIR Thrombolysis in Cerebral Infarction (TICI) Task Force . Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44(9):2650-2663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berger C, Fiorelli M, Steiner T, et al. . Hemorrhagic transformation of ischemic brain tissue: asymptomatic or symptomatic? Stroke. 2001;32(6):1330-1335. [DOI] [PubMed] [Google Scholar]
- 19.SAS Institute, Inc. SAS/STAT(R) 9.2 User’s Guide. 2nd ed Cary, NC: SAS Institute; 2009. [Google Scholar]
- 20.Goyal M, Menon BK, van Zwam WH, et al. ; HERMES collaborators . Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723-1731. [DOI] [PubMed] [Google Scholar]
- 21.Mocco J, Zaidat OO, von Kummer R, et al. ; THERAPY Trial Investigators* . Aspiration thrombectomy after intravenous alteplase versus intravenous alteplase alone. Stroke. 2016;47(9):2331-2338. [DOI] [PubMed] [Google Scholar]
- 22.Turk AS, Turner R, Spiotta A, et al. . Comparison of endovascular treatment approaches for acute ischemic stroke: cost effectiveness, technical success, and clinical outcomes. J Neurointerv Surg. 2015;7(9):666-670. [DOI] [PubMed] [Google Scholar]
- 23.ClinicalTrials.gov Interest of Direct Aspiration First Pass Technique (ADAPT) for Thrombectomy Revascularisation of Large Vessel Occlusion in Acute Ischaemic Stroke (ASTER). NCT02523261. https://clinicaltrials.gov/ct2/show/NCT02523261. Accessed August 1, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eMethods. Exclusion Criteria, Device Use, and Statistical Analysis
eTable 1. Device-Related Adverse Events (Intention to Treat)
eTable 2. Baseline Patient Characteristics and Process Times (Per Protocol)
eTable 3. Primary Outcomes (Per Protocol)
eTable 4. Safety and Secondary Outcomes (Per Protocol)
eTable 5. Definition and Distribution of mTICI Scores (Intention to Treat)
eTable 6. Number of Patients Randomized by Center
eTable 7. Comparison of Baseline Characteristics of Analyzed and Missing Data (Intention to Treat)
eTable 8. mRS Sensitivity Analyses (Intention to Treat)
eTable 9. Screening Results
eTable 10. Classification of Intracebral Hemorrhages
eFigure 1. Distribution of Primary End Point (mTICI 2-3) Treatment Effect Across the Prespecified Subgroups (Intention to Treat)
eFigure 2. Kaplan-Meier Estimates of the Probability of Death in Patients (Intention to Treat)
eFigure 3. Functional outcomes at 90 days, According to Modified Rankin Scale Score (Intention to Treat)