This population-based study examines changes in the prevalence of severe obesity in US children aged 2 to 4 years enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children from 2000 to 2014.
Key Points
Question
What were the trends in prevalence of severe obesity among children aged 2 to 4 years who were enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children during 2010 to 2014?
Findings
In this cross-sectional study of 22.6 million children aged 2 to 4 years, the overall adjusted prevalence of severe obesity increased during 2000 to 2004, decreased slightly during 2004 to 2010, and decreased further during 2010 to 2014; all changes were statistically significant. During 2010 to 2014, the prevalence decreased significantly among all demographic groups.
Meaning
The findings indicate recent progress in reducing the prevalence of severe obesity among young children in the United States enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children.
Abstract
Importance
Severe obesity in childhood is associated with negative health consequences. A previous study examined trends in severe obesity among preschool-aged children in low-income families during 1998 to 2010. No recent trends have been reported.
Objective
To examine trends in severe obesity by age, sex, and race/ethnicity among enrollees in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) aged 2 to 4 years during 2000 to 2014.
Design, Setting, and Participants
Serial cross-sectional data from 22.6 million young children enrolled in WIC from 50 states, the District of Columbia, and 5 US territories from 2000 to 2014. Data analysis was conducted from February 16, 2017, to March 9, 2017.
Main Outcomes and Measures
Prevalence of severe obesity. Severe obesity was defined as a sex-specific body mass index-for-age 120% or more of the 95th percentile on the 2000 Centers for Disease Control and Prevention growth charts. Children’s weights and heights were measured. Children whose sex, weight, height, or body mass index was missing or biologically implausible were excluded.
Results
The prevalence of severe obesity was 1.96% in 2014. During 2000 to 2004, the prevalence increased significantly overall from 1.80% to 2.11% (adjusted prevalence difference [APD], 0.26%) and among all the age, sex, and racial/ethnic groups except for Asian/Pacific Islander (APD, 0.05%-0.54% across groups with increases). The largest relative increase occurred in children aged 4 years (adjusted prevalence ratio [APR], 1.21) and non-Hispanic white (APR, 1.22) and American Indian/Alaska Native children (APR, 1.19). During 2004 to 2010, the prevalence decreased significantly overall (APD, −0.05%), among boys, children aged 2 and 3 years, and non-Hispanic black and Asian/Pacific Islander children (APD, −0.05% to −0.18%). During 2010 to 2014, the prevalence decreased significantly overall from 2.12% to 1.96% (APD, −0.14%) and among all demographic groups (APD, −0.04% to −0.30% across groups). The largest relative decrease occurred in children aged 2 years (APR, 0.88) and Hispanic (APR, 0.92), American Indian/Alaska Native (APR, 0.89), and Asian/Pacific Islander (APR, 0.87) children.
Conclusions and Relevance
This study provides updated prevalence and trends of severe obesity among young children enrolled in WIC and reports recent modest declines in severe obesity in all subgroups. Ongoing surveillance can assess whether declines continue into the future among low-income children.
Introduction
Childhood obesity remains a public health concern. Data from the National Health and Nutrition Examination Survey (NHANES) indicated that obesity prevalence increased from 7.2% in 1988 to 1994 to 13.9% in 2003-2004 and then decreased to 9.4% in 2013 to 2014 among children aged 2 to 5 years. Despite the recent declines, the prevalence of childhood obesity remains high, especially among children living in low-income families because obesity disproportionally affects this vulnerable group. According to a previous Centers for Disease Control and Prevention (CDC) study, the prevalence of obesity was 14.5% among young children who were enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in 2014. Obesity and severe obesity in childhood have been associated with other cardiovascular risk factors, impaired glucose tolerance, respiratory problems, increased health care costs, and premature death. Those who have obesity or severe obesity during early childhood are also likely to have obesity during middle or late childhood, and obesity often persists into adulthood. Adults who have obesity and severe obesity are at increased risk for stroke, coronary heart disease, diabetes, and many other common and costly chronic diseases.
In the United States, 1.7% of children aged 2 to 5 years had severe obesity in 2011 to 2014. Children with severe obesity face even greater health and social challenges; for example, the prevalence of cardiovascular risk factors increases with the severity of childhood obesity. Children with a body mass index (BMI) over the 99th percentile (calculated as weight in kilograms divided by height in meters squared) are at increased risk for cardiovascular disease, and the likelihood of adiposity tracking into adulthood is extremely high. These lifelong health risks associated with severe obesity during early childhood indicate the importance of preventing and identifying severe obesity. Ongoing surveillance among children enrolled in WIC can help to evaluate the effectiveness of obesity prevention efforts among children from low-income families. One previous analysis using CDC Pediatric Nutrition Surveillance System (PedNSS) data found that the prevalence of severe obesity increased during 1998 to 2003 and decreased slightly during 2003 to 2010 among children aged 2 to 4 years who were enrolled in WIC and other nutrition and health programs. The CDC stopped operation of PedNSS in 2012, and no updated prevalence and secular trends have been reported since then. In this study, we used the WIC Participant and Program Characteristics (WIC PC) data collected by the US Department of Agriculture to examine the prevalence and trends of severe obesity among children aged 2 to 4 years who were enrolled in WIC from 2000 through 2014.
Methods
Study Population
The WIC PC is a biennial census of US WIC enrollees who are certified to receive benefits in April of the even years. It is used to monitor the nutritional status of low-income pregnant, postpartum, and breastfeeding women and children younger than 5 years who are enrolled in WIC. The program is administered in each state or territory by state health departments or Indian tribal organizations. To be eligible, WIC applicants must live in the state where they apply and have certain medical or dietary conditions. Furthermore, applicants need to have a gross household income 185% or less of the US poverty level or have proof of participation in the Supplemental Nutrition Assistance Program, Temporary Assistance for Needy Families, or Medicaid.
The initial study population contained 22.8 million children aged 2 to 4 years who were enrolled in WIC state agencies in 50 states, the District of Columbia, and 5 US territories during 2000 to 2014. Because certain prevalence in a state differed substantially from the estimates in adjacent years, we used a robust regression model to predict annual prevalence for each state. We excluded all 24 472 (0.11%) children from Hawaii in 2002 and 2004 because these prevalence estimates differed by more than 10 percentage points from the values predicted by a robust regression model. In addition, we excluded 1062 (0.005%) children whose weight and height were measured more than 1 year before the reporting year, and 194 526 (0.85%) whose sex, weight, height, or BMI were missing or biologically implausible. Biologically implausible z Scores were defined as height for age less than −5.0 or above 4.0, weight for age less than −5.0 or above 8.0, and BMI for age less than −4.0 or more than 8.0. The final analytic sample included 22 553 518 children. Annual sample sizes ranged from 2 352 648 in 2000 to 3 307 442 in 2010. The study was exempt from ethics reviews by the CDC and the US Department of Agriculture.
Children’s Anthropometric Measurements
Children’s anthropometric measurements were taken by trained staff during their certification or recertification visits. Standard data collection and recording protocols were used in all participating jurisdictions. Weights were reported to the nearest quarter pound and heights to the nearest eighth inch. Approximately 75% of the anthropometric data in the present study were collected within 6 months before April of the reporting year.
Documenting severe obesity has been inconsistent in the past because of lack of a standard definition. One study proposed that children with BMI over the 99th percentile be considered as having severe obesity because they are at elevated risk for cardiovascular diseases and adulthood obesity. Because CDC growth charts are based on data between the 3rd and 97th percentiles and are not intended for use beyond this range, Flegal and colleagues suggested approximating the empirical 99th BMI percentile by multiplying the BMI values at the 95th percentile by 120%. In 2013, experts convened by the American Heart Association recommended that severe obesity in children aged 2 years or older and adolescents be defined as BMI 35 kg/m2 or more or 120% of the 95th percentile, whichever is lower, based on age and sex. Because BMI 35 kg/m2 is a higher threshold than BMI 120% or more of the 95th percentile for young children, the CDC uses a cutoff of 120% of the 95th BMI percentile for severe obesity. In this study, we adopted the CDC definition and defined severe obesity as sex-specific BMI for age of 120% or more of the 95th percentile on the 2000 CDC growth charts. We further defined class II severe obesity as a BMI of 140% or more of the 95th percentile.
Statistical Analysis
SAS software, version 9.3 (SAS Institute) was used to estimate the annual unadjusted prevalence of severe obesity from 2000 to 2014, both overall and by age (2, 3, or 4 years), sex, and race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, American Indian/Alaska Native [AIAN], or Asian/Pacific Islander [PI]).
We identified statistically significant changes in overall secular trend of severe obesity using Joinpoint, version 4.3.1 (National Cancer Institute, https://surveillance.cancer.gov/joinpoint). The Joinpoint regression fits a series of joined straight lines on a logarithmic scale and identifies the best joint points where statistically significant changes occur. The number and location of significant join points is determined with Monte Carlo samples from permuted data sets, with Bonferroni adjustments to control for increases in type 1 errors. Data analysis was conducted from February 16, 2017, to March 9, 2017.
Because Joinpoint regression identified 2004 and 2010 as the inflection years for overall trend of severe obesity, changes in prevalence were further analyzed for 3 periods—2000 to 2004, 2004 to 2010, and 2010 to 2014—using SAS. To account for annual differences in population distribution, log binomial regression controlling for age, sex, and race/ethnicity was used to estimate adjusted prevalence ratios (APRs), which represent relative changes in prevalence for the 3 periods. Adjusted prevalence differences (APDs) were then calculated ([prevalence at beginning of period] × [APR] − [prevalence at beginning of period]). We considered increases or decreases in prevalence statistically significant if the 95% CIs for APD did not include 0.
To assess the extent to which the trend in overall prevalence of severe obesity was due to the cutoffs for biologically implausible z Scores, we conducted sensitivity analyses by performing additional log binomial regressions using the narrower World Health Organization z Score cutoffs (height for age,<−5.0 or >3.0; weight for age,<−5.0 or >5.0; and BMI for age,<−4.0 or >5.0) and wider z Score cutoffs (height for age,<−5.0 or >7.0, weight for age,<−5.0 or >9.0, and BMI for age,<−4.0 or >9.0).
Results
The demographic distribution of the study population was slightly different in 2000, 2004, 2010, and 2014 (Table 1). In 2010 and 2014, there was a lower proportion of non-Hispanic white children and higher proportions of Hispanic and Asian/PI children. Additionally, the 2004 and 2010 WIC enrollees had a slightly lower proportion of non-Hispanic black children than the enrollees in other years (Table 1).
Table 1. Characteristics of US Children Aged 2 to 4 Years Enrolled in WICa.
| Characteristic | No. (%) | |||
|---|---|---|---|---|
| 2000 | 2004 | 2010 | 2014 | |
| Total | 2 352 648 | 2 648 564 | 3 307 442 | 3 016 487 |
| Sex | ||||
| Male | 1 190 751 (50.6) | 1 336 373 (50.5) | 1 676 395 (50.7) | 1 532 467 (50.8) |
| Female | 1 161 897 (49.4) | 1 312 191 (49.5) | 1 631 047 (49.3) | 1 484 020 (49.2) |
| Age, y | ||||
| 2 | 942 316 (40.1) | 1 058 761 (40.0) | 1 333 334 (40.3) | 1 198 411 (39.7) |
| 3 | 830 402 (35.3) | 935 090 (35.3) | 1 166 350 (35.3) | 1 106 205 (36.7) |
| 4 | 579 930 (24.7) | 654 713 (24.7) | 807 758 (24.4) | 711 871 (23.6) |
| Race/ethnicity | n = 2 340 261 | n = 2 624 894 | n = 3 282 225 | n = 3 011 888 |
| Non-Hispanic white | 842 692 (36.0) | 877 449 (33.4) | 966 673 (29.5) | 841 132 (27.9) |
| Non-Hispanic black | 489 333 (20.9) | 512 529 (19.5) | 618 580 (18.8) | 615 395 (20.4) |
| Hispanic | 904 901 (38.7) | 1 126 184 (42.9) | 1 536 644 (46.8) | 1 389 135 (46.1) |
| American Indian/Alaska Native | 23 141 (1.0) | 27 806 (1.1) | 38 661 (1.2) | 36 456 (1.2) |
| Asian/Pacific Islander | 80 194 (3.4) | 80 926 (3.1) | 121 667 (3.7) | 129 770 (4.3) |
Abbreviation: WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Includes children who were enrolled in WIC state agencies in 50 states, the District of Columbia, and 5 US territories, except Hawaii in 2004.
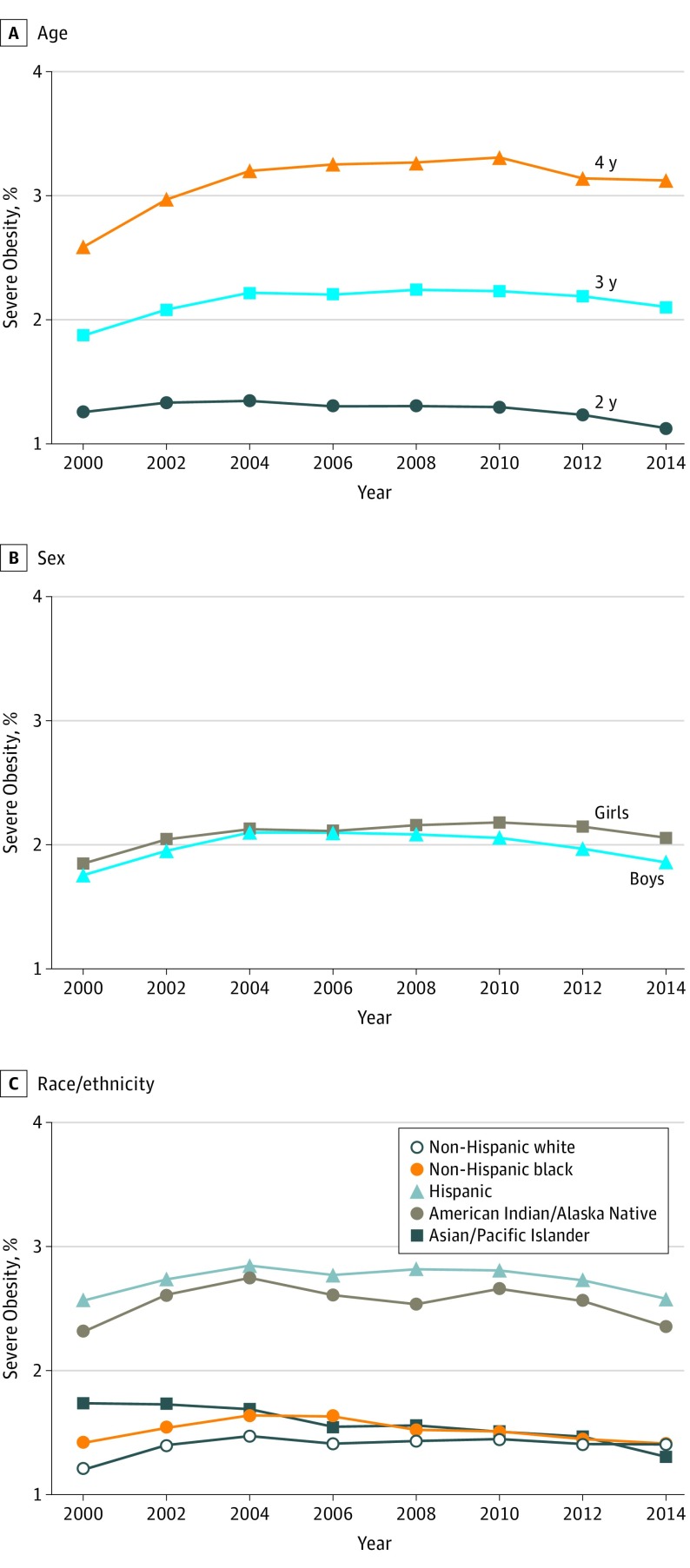
During 2000 to 2004, the overall prevalence of severe obesity increased significantly from 1.80% to 2.11% (APD, 0.26%) (Figure and Table 2). The crude prevalence was similar in 2004 and 2010; however, there was a small but significant decrease from 2004 to 2010 after adjusting for age, sex, and race/ethnicity (APD, −0.05%). During 2010 to 2014, the overall prevalence decreased significantly from 2.12% to 1.96% (APD, −0.14%) (Figure and Table 2).
Figure. Prevalence of Severe Obesity Among US Children Aged 2 to 4 Years Enrolled in Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) From 2000 to 2014.
Severe obesity was defined as sex-specific body mass index for age 120% or more of the 95th percentile on the 2000 Centers for Disease Control and Prevention growth charts by age (A), sex (B), and race/ethnicity (C). Includes data from all WIC state agencies in 50 states, the District of Columbia, and 5 territories; Hawaii was excluded in 2002 and 2004.
Table 2. Prevalence of Severe Obesitya Among US Children Aged 2 to 4 Years Enrolled in WIC.
| Demographic Characteristic | Prevalence, %b | Adjusted Prevalence Ratio (95% CI)c | Adjusted Prevalence Difference (95% CI)d | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2000 | 2004 | 2010 | 2014 | 2004 vs 2000 | 2010 vs 2004 | 2014 vs 2010 | 2004 vs 2000 | 2010 vs 2004 | 2014 vs 2010 | |
| Overalle | 1.80 | 2.11 | 2.12 | 1.96 | 1.14 (1.13 to 1.16)f | 0.98 (0.97 to 0.99)f | 0.93 (0.92 to 0.94)f | 0.26 (0.23 to 0.28)f | −0.05 (−0.07 to −0.03)f | −0.14 (−0.17 to −0.12)f |
| Sex | ||||||||||
| Male | 1.75 | 2.10 | 2.06 | 1.86 | 1.16 (1.14 to 1.18)f | 0.96 (0.94 to 0.97)f | 0.91 (0.90 to 0.93)f | 0.28 (0.25 to 0.32)f | −0.09 (−0.12 to −0.06)f | −0.18 (−0.21 to −0.15)f |
| Female | 1.85 | 2.13 | 2.18 | 2.06 | 1.12 (1.10 to 1.14)f | 1.01 (0.99 to 1.02) | 0.95 (0.94 to 0.97)f | 0.23 (0.19 to 0.27)f | 0.01 (−0.02 to 0.04) | −0.11 (−0.14 to −0.08)f |
| Age, y | ||||||||||
| 2 | 1.26 | 1.35 | 1.30 | 1.13 | 1.04 (1.01 to 1.06)f | 0.94 (0.92 to 0.96)f | 0.88 (0.86 to 0.90)f | 0.05 (0.02 to 0.08)f | −0.08 (−0.11 to −0.05)f | −0.16 (−0.19 to −0.13)f |
| 3 | 1.87 | 2.22 | 2.23 | 2.10 | 1.15 (1.13 to 1.18)f | 0.98 (0.96 to 0.997)f | 0.95 (0.93 to 0.96)f | 0.29 (0.25 to 0.33)f | −0.05 (−0.09 to −0.01)f | −0.12 (−0.16 to −0.08)f |
| 4 | 2.59 | 3.20 | 3.31 | 3.12 | 1.21 (1.18 to 1.23)f | 1.01 (0.99 to 1.03) | 0.95 (0.93 to 0.97)f | 0.54 (0.47 to 0.60)f | 0.03 (−0.03 to 0.08) | −0.16 (−0.22 to −0.11)f |
| Race/ethnicity | ||||||||||
| Non-Hispanic white | 1.20 | 1.47 | 1.45 | 1.41 | 1.22 (1.19 to 1.26)f | 0.99 (0.97 to 1.02) | 0.97 (0.95 to 0.997)f | 0.27 (0.23 to 0.31)f | −0.01 (−0.05 to 0.02) | −0.04 (−0.17 to −0.005)f |
| Non-Hispanic black | 1.42 | 1.64 | 1.51 | 1.41 | 1.16 (1.12 to 1.19)f | 0.93 (0.90 to 0.96)f | 0.94 (0.91 to 0.97)f | 0.22 (0.17 to 0.27)f | −0.11 (−0.16 to −0.07)f | −0.09 (−0.13 to −0.05)f |
| Hispanic | 2.56 | 2.85 | 2.81 | 2.58 | 1.11 (1.09 to 1.13)f | 0.99 (0.97 to 1.00) | 0.92 (0.91 to 0.93)f | 0.29 (0.24 to 0.34)f | −0.04 (−0.08 to 0.00) | −0.22 (−0.26 to −0.19)f |
| American Indian/Alaska Native | 2.31 | 2.75 | 2.66 | 2.35 | 1.19 (1.07 to 1.33)f | 0.97 (0.89 to 1.07) | 0.89 (0.81 to 0.97)f | 0.43 (0.15 to 0.75)f | −0.07 (−0.31 to 0.18) | −0.30 (−0.50 to −0.07)f |
| Asian/Pacific Islander | 1.74 | 1.69 | 1.51 | 1.31 | 0.98 (0.91 to 1.05) | 0.89 (0.83 to 0.96)f | 0.87 (0.81 to 0.93)f | −0.04 (−0.16 to 0.09) | −0.18 (−0.28 to −0.07)f | −0.20 (−0.28 to −0.11)f |
Abbreviation: WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Defined as sex-specific body mass index for age 120% or more of the 95th percentile on the 2000 Centers for Disease Control and Prevention growth charts.
Crude prevalence of severe obesity.
Represents relative changes in prevalence of severe obesity between 2 inflection years; calculated from log binomial regression models adjusted for age, sex, and race/ethnicity.
Calculated as ([prevalence at beginning of period] × [adjusted prevalence ratio] − [prevalence at beginning of period]).
Includes data from all the WIC state agencies in 50 states, District of Columbia, and 5 US territories except for Hawaii data in 2002 and 2004.
Statistically significant change based on log binomial regression model adjusted for age, sex, and race/ethnicity.
Girls had a slightly higher prevalence of severe obesity in all years than boys (Figure and Table 2). From 2000 to 2004, the adjusted prevalence of severe obesity increased significantly among boys and girls; the relative increase was greater among boys than girls based on APRs (Table 2). From 2004 to 2010, the adjusted prevalence decreased significantly among boys but remained relatively unchanged among girls. However, from 2010 to 2014, the adjusted prevalence decreased significantly among both groups (Figure and Table 2); the relative decrease was greater among boys than girls.
The prevalence of severe obesity increased with age. Among children aged 2 and 3 years, the adjusted prevalence increased significantly from 2000 to 2004 and decreased significantly afterward. For children aged 4 years, the adjusted prevalence went up from 2000 to 2004, levelled between 2004 and 2010, and declined significantly from 2010 to 2014 (Figure and Table 2). Children aged 2 years had the smallest relative increase during 2000 to 2004 and the greatest relative decrease during 2010 to 2014 based on APRs (Table 2).
The prevalence of severe obesity in all years was highest among AIAN and Hispanic children. During 2000 to 2004, the adjusted prevalence increased significantly among all the racial/ethnic groups except Asian/PI, for which the adjusted prevalence remained relatively unchanged. The largest relative increase occurred in non-Hispanic white and AIAN children based on APRs (Table 2). During 2004-2010, the adjusted prevalence declined significantly among non-Hispanic black and Asian/PI children and levelled among the remaining racial/ethnic groups. During 2010 to 2014, the adjusted prevalence decreased significantly among all the racial/ethnic groups (Figure and Table 2). The relative decline was greater among Hispanic, AIAN, and Asian/PI children than that among non-Hispanic white and non-Hispanic black children.
The trend in overall prevalence of class II severe obesity was similar to that for severe obesity overall. The prevalence of class II severe obesity increased significantly from 0.27% in 2000 to 0.33% in 2004, decreased slightly but significantly to 0.32% in 2010, and then further decreased to 0.30% in 2014.
Discussion
Our analyses found that the prevalence of severe obesity among US WIC enrollees aged 2 to 4 years increased from 2000 to 2004 and decreased from 2004 to 2014. For the first time, we found that the decrease between 2010 and 2014 was statistically significant in all age, sex, and racial/ethnic subgroups.
Previous research based on PedNSS data from 30 states and the District of Columbia found that the prevalence of severe obesity increased significantly during 1998 to 2003 overall and in all racial/ethnic groups except Asian/PI and decreased significantly during 2003 to 2010 overall and in all racial/ethnic groups except AIAN. Unlike WIC PC, PedNSS collected data in January through December calendar years and did not have consistent data for all state agencies over time. In addition to WIC enrollees (>80%), PedNSS also included participants in other child health and nutrition programs in certain states. Although the present study based on WIC PC is not directly comparable with the previous PedNSS research because of differences in methodology, the present study also found a similar upward trend until 2004 and a downward trend afterward for severe obesity overall. Furthermore, the present study suggested that the overall decline continued to 2014 and a significant decrease between 2010 and 2014 occurred in all WIC population subgroups.
Previous studies have examined the prevalence of severe obesity among young children from US families of all income levels. One study by Koebnick and colleagues using the same definition for severe obesity as the present study found that 2.5% of the children aged 2 to 5 years who were enrolled in a prepaid health plan in south California were severely obese in 2007 to 2008. The results of NHANES studies using the same definition showed that the prevalence of severe obesity among US children aged 2 to 5 years was 2.2% in 1999 to 2006 and 1.7% in 2011 to 2014. To compare our study results with the NHANES prevalence estimate in a comparable age group, we estimated the prevalence of severe obesity based on a sample of 5000 children aged 2 to 4 years who participated in NHANES from 1999 to 2014. We found that 1.4% of US children had severe obesity, which was lower than the prevalence among WIC enrollees included in our study. Skelton et al (severe obesity defined as BMI≥99th percentile) and Claire Wang et al (severe obesity defined the same way as in the present study) examined trends in severe obesity among NHANES participants aged 2 to 5 years and reported that the prevalence markedly increased from the 1970s to 2004 or 2006. Two recent NHANES studies that used the same definition for severe obesity as the present study found no significant change in the prevalence of severe obesity among US children aged 2 to 5 years from families of all income levels during 1999 to 2014.
The explanation for the observed downward trends is likely complex. Differences in genetic, behavioral, and environmental factors across years may have contributed to the decreases in prevalence of severe obesity. A number of federal programs promoted healthful food choices and increased support for families and communities. For example, the US Department of Agriculture promotes healthy eating and nutrition education through many of its child nutrition programs, including the Federal WIC Program. The US Department of Agriculture published an interim rule in 2007 to revise the WIC food packages by October 2009 to align more closely with updated nutrition science, the 2010 Dietary Guidelines for Americans, and the infant feeding practice guidelines of the American Academy of Pediatrics. The revised food packages promoted fruits, vegetables, and whole wheat product purchases, included more variety of healthy food options, supported breastfeeding, and provided WIC state agencies with greater flexibility in prescribing food packages to accommodate enrollees’ cultural food preferences. Studies have found that changes to the WIC food packages have led to reductions in fruit juice purchases, increases in Healthy Eating Index scores and fruit, vegetable, and whole grain consumptions, better access to healthy foods in communities, and improved WIC staff competence in providing counseling for children with overweight.
Recommendations and activities from CDC and comprehensive public health strategies from the Institute of Medicine to prevent and manage childhood obesity may have also played important roles for the declining trends in severe obesity. The CDC provided funding, training, and technical assistance to a variety of state and community agencies to increase access to healthful foods and more opportunities for physical activity. The State Public Health Actions grant funded all 50 states and the District of Columbia on promoting breastfeeding, implementing nutrition standards, and improving physical activity in communities. The CDC provided technical support for states to work with hospitals, and there have been improved food and beverage and physical activity environments in hospitals and enhanced maternity care policies and practices supportive of breastfeeding in birth facilities. Furthermore, the CDC provided resources and support for Early Care and Education providers to embed Caring for Our Children Standards for obesity prevention into state Early Care and Education systems and increase their knowledge about nutrition, breastfeeding, screen time, and physical activity standards.
Limitations
Our study is subject to at least 3 limitations. First, the study is not representative of US children from families of all income levels. Furthermore, only approximately 50% of WIC-eligible young children were enrolled in WIC, so our findings may not be representative of all low-income US children aged 2 to 4 years. In addition, we included only children enrolled in nontribal WIC programs; the observed trend in severe obesity among AIAN children may not be representative of WIC enrollees in AIAN tribes. Second, although there is a high correlation between BMI and body fat for children with higher BMI levels, BMI does not precisely approximate adiposity or percentage of body fat in children. For example, the level of body fat is lower among non-Hispanic black children than that among non-Hispanic white children with the same BMI levels. Our study findings did not account for differences in body fat distributions across racial/ethnic groups. Third, our findings may have been affected by our inclusion of children with high BMIs but whose weight or height entries were incorrect. We may have also excluded children valid for study because their weight or BMI exceeded our upper cutoff points for biological implausible values. However, our sensitivity analyses using the narrower World Health Organization cutoffs or the wider cutoffs for biologically implausible z Scores indicated the same rate of increase from 2000 to 2004 and the same rate of decrease from 2010 to 2014 in overall prevalence of severe obesity. However, the results based on the narrower World Health Organization cutoffs showed no statistically significant change between 2004 and 2010 and the analysis using the wider z Score cutoffs indicated a slightly greater decrease in overall prevalence than the findings of the present study for this time.
Conclusions
Our findings indicate recent progress in reducing the prevalence of severe obesity among young US children enrolled in WIC. However, severe obesity in early childhood remains a serious public health concern because of its common adverse health and social consequences. Future surveillance that monitors severe obesity and related behavioral risk factors will help to determine whether the downward trends in severe obesity are continuing in all groups and whether racial/ethnic gaps in prevalence are narrowing. More evaluative research could determine whether the recent reversal in the prevalence of severe obesity may be attributable to obesity prevention initiatives for all children or to initiatives specifically targeting children enrolled in WIC. Continued implementation of population-based strategies to support environmental and policy change in health care, Early Care and Education, and community settings, and culturally appropriate intervention efforts focusing on low-income children and their caregivers may be important for further reducing the prevalence of severe obesity among young children.
References
- 1.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315(21):2292-2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freedman DS; Centers for Disease Control and Prevention (CDC) . Obesity—United States, 1988-2008. MMWR Suppl. 2011;60(1)(suppl):73-77. [PubMed] [Google Scholar]
- 3.Pan L, Freedman DS, Sharma AJ, et al. Trends in obesity among participants aged 2-4 years in the Special Supplemental Nutrition Program for Women, Infants, and Children—United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;65(45):1256-1260. [DOI] [PubMed] [Google Scholar]
- 4.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362(6):485-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(1):12-17.e2. [DOI] [PubMed] [Google Scholar]
- 6.Sen Y, Kandemir N, Alikasifoglu A, Gonc N, Ozon A. Prevalence and risk factors of metabolic syndrome in obese children and adolescents: the role of the severity of obesity. Eur J Pediatr. 2008;167(10):1183-1189. [DOI] [PubMed] [Google Scholar]
- 7.Trasande L, Elbel B. The economic burden placed on healthcare systems by childhood obesity. Expert Rev Pharmacoecon Outcomes Res. 2012;12(1):39-45. [DOI] [PubMed] [Google Scholar]
- 8.Nader PR, O’Brien M, Houts R, et al. ; National Institute of Child Health and Human Development Early Child Care Research Network . Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3):e594-e601. [DOI] [PubMed] [Google Scholar]
- 9.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869-873. [DOI] [PubMed] [Google Scholar]
- 10.National Institutes of Health Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults–The Evidence Report. Obes Res. 1998;6(suppl 2):51S-209S. [PubMed] [Google Scholar]
- 11.Pan L, Blanck HM, Sherry B, Dalenius K, Grummer-Strawn LM. Trends in the prevalence of extreme obesity among US preschool-aged children living in low-income families, 1998-2010. JAMA. 2012;308(24):2563-2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.US Department of Agriculture Food and Nutrition Service Women, Infants and Children. WIC eligibility requirements. Washington, DC: US Department of Agriculture. https://www.fns.usda.gov/wic/wic-eligibility-requirements. Updated May 4, 2017. Accessed September 20, 2017.
- 13.Centers for Disease Control and Prevention (CDC) A SAS program for the 2000 CDC growth charts (ages 0 to <20 years). Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention. http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Updated December 16, 2016. Accessed September 20, 2017.
- 14.Pennsylvania Department of Health Anthropometric training manual. Division of Women, Infants and Children. 2010. https://wicworks.fns.usda.gov/wicworks/Sharing_Center/PA/Anthro/lib/pdf/Anthropometric_Training_Manual.pdf. Accessed September 20, 2017.
- 15.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1-190. [PubMed] [Google Scholar]
- 16.Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90(5):1314-1320. [DOI] [PubMed] [Google Scholar]
- 17.Kelly AS, Barlow SE, Rao G, et al. ; American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young, Council on Nutrition, Physical Activity and Metabolism, and Council on Clinical Cardiology . Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689-1712. [DOI] [PubMed] [Google Scholar]
- 18.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for Joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-351. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization Physical Status: The Use and Interpretation of Anthropometry: Report of a WHO Expert Committee. Geneva, Switzerland: World Health Organization; 1995. [PubMed] [Google Scholar]
- 20.Dalenius K, Borland E, Smith B, Polhamus B, Grummer-Strawn L Pediatric Nutrition Surveillance 2010 report. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2012. https://stacks.cdc.gov/view/cdc/11951. Accessed September 20, 2017. [Google Scholar]
- 21.Koebnick C, Smith N, Coleman KJ, et al. Prevalence of extreme obesity in a multiethnic cohort of children and adolescents. J Pediatr. 2010;157(1):26-31.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Claire Wang Y, Gortmaker SL, Taveras EM. Trends and racial/ethnic disparities in severe obesity among US children and adolescents, 1976-2006. Int J Pediatr Obes. 2011;6(1):12-20. [DOI] [PubMed] [Google Scholar]
- 23.Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009;9(5):322-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Skinner AC, Perrin EM, Skelton JA. Prevalence of obesity and severe obesity in US children, 1999-2014. Obesity (Silver Spring). 2016;24(5):1116-1123. [DOI] [PubMed] [Google Scholar]
- 25.Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr. 2014;168(6):561-566. [DOI] [PubMed] [Google Scholar]
- 26.US Department of Agriculture Food and Nutrition Service. Women, Infants and Children (WIC) final rule: revisions in the WIC food packages. http://www.fns.usda.gov/wic/benefitsandservices/foodpkg.htm. Updated August 14, 2017. Accessed September 20, 2017.
- 27.US Department of Agriculture, US Department of Health and Human Services Dietary Guidelines for Americans, 2010. http://health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf. Published December 2010. Accessed September 20, 2017.
- 28.Lockner DW, Kibbe D, Marley SC, Trowbridge F. Get healthy together: a program to improve counseling for childhood obesity in community-based WIC clinics. J Health Care Poor Underserved. 2014;25(2):771-786. [DOI] [PubMed] [Google Scholar]
- 29.Andreyeva T, Luedicke J, Middleton AE, Long MW, Schwartz MB. Positive influence of the revised Special Supplemental Nutrition Program for Women, Infants, and Children food packages on access to healthy foods. J Acad Nutr Diet. 2012;112(6):850-858. [DOI] [PubMed] [Google Scholar]
- 30.Chiasson MA, Findley SE, Sekhobo JP, et al. Changing WIC changes what children eat. Obesity (Silver Spring). 2013;21(7):1423-1429. [DOI] [PubMed] [Google Scholar]
- 31.Tester JM, Leung CW, Crawford PB. Revised WIC food package and children’s diet quality. Pediatrics. 2016;137(5):e20153557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McGuire S. Institute of Medicine, 2012: accelerating progress in obesity prevention: solving the weight of the nation. Washington, DC: National Academies Press. Adv Nutr. 2012;3(5):708-709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC) Division of Nutrition, Physical Activity, and Obesity. State Public Health Actions (1305). https://www.cdc.gov/nccdphp/dnpao/state-local-programs/state-public-health-action.html. Updated April 21, 2017. Accessed September 20, 2017.
- 34.Centers for Disease Control and Prevention (CDC) Healthy Hospital Environments. https://www.cdc.gov/obesity/strategies/healthy-hospital-env.html. Updated July 13, 2017. Accessed September 20, 2017.
- 35.Perrine CG, Galuska DA, Dohack JL, et al. ; MLIS . Vital signs: improvements in maternity care policies and practices that support breastfeeding—United States, 2007-2013. MMWR Morb Mortal Wkly Rep. 2015;64(39):1112-1117. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention (CDC) Early Care and Education (ECE). https://www.cdc.gov/obesity/strategies/childcareece.html. Updated September 19, 2017. Accessed September 20, 2017.
- 37.Nutrition Assistance and Support Series. Office of Research Analysis National and State-Level Estimates of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Eligibles and Program Reach, 2000–2009. https://www.fns.usda.gov/sites/default/files/WICEligibles2000-2009Vol2_0.pdf. Published December 2011. Accessed September 20, 2017.
- 38.Freedman DS, Wang J, Maynard LM, et al. Relation of BMI to fat and fat-free mass among children and adolescents. Int J Obes (Lond). 2005;29(1):1-8. [DOI] [PubMed] [Google Scholar]
- 39.Flegal KM, Ogden CL, Yanovski JA, et al. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. Am J Clin Nutr. 2010;91(4):1020-1026. [DOI] [PMC free article] [PubMed] [Google Scholar]