Abstract
Importance
The Early Treatment Diabetic Retinopathy Study (ETDRS) alphabet chart is not feasible for measuring best-corrected visual acuity (BCVA) for individuals who are unfamiliar with the Roman alphabet. The ETDRS Landolt C chart is an alternative, but it may not reflect true BCVA among those with confusion between left and right. The ETDRS number chart might overcome these limitations, but little is known regarding its reliability.
Objective
To evaluate repeatability and agreement of BCVA using the ETDRS number chart or Landolt C chart compared with ETDRS alphabet charts in healthy and diseased eyes.
Design, Setting, and Participants
A cross-sectional study was conducted in Thailand from July 1, 2015, to June 30, 2016, among 154 adult Thai individuals. Those who could read Roman alphabets were classified into the following 4 groups, using 1 eye per participant: group A, which comprised 60 healthy eyes (BCVA, 20/20-20/25); group B, which comprised 40 eyes with age-related cataract, diabetic macular edema, or age-related macular degeneration (BCVA, 20/20-20/40); group C, which comprised 40 eyes with age-related cataract, diabetic macular edema, or age-related macular degeneration (BCVA, 20/50-20/100); and group D, which comprised 14 eyes with age-related cataract, diabetic macular edema, or age-related macular degeneration (BCVA, 20/125-20/200).
Interventions
Two standardized 4-m BCVA measurements with 3 different Precision Vision ETDRS charts (PV number, Landolt C, and alphabet), in random sequence, performed 30 minutes apart.
Main Outcomes and Measures
Repeatability, agreement, and testing duration of BCVA.
Results
Of 154 Thai participants (82 women and 72 men; mean [SD] age, 52.9 [18.2] years), the ETDRS number chart had strong repeatability coefficients (group A, 0.61 [95% CI, 0.42-0.75]; group B, 0.87 [95% CI, 0.78-0.93]; group C, 0.81 [95% CI, 0.67-0.90]; and group D, 0.81 [95% CI, 0.49-0.94]). Concordance correlation coefficients between the number and alphabet charts were also strong (group A, 0.89 [95% CI, 0.82-0.93]; group B, 0.97 [95% CI, 0.94-0.98]; group C, 0.92 [95% CI, 0.86-0.96]; and group D, 0.96 [95% CI, 0.87-0.99]), while the concordance correlation coefficients between the Landolt C and alphabet charts were lower (group A, 0.72 [95% CI, 0.52-0.83]; group B, 0.83 [95% CI, 0.68-0.91]; group C, 0.79 [95% CI, 0.61-0.89]; and group D, 0.89 [95% CI, 0.66-0.97]). The mean letter score difference between the number and alphabet charts was 1 (95% limits of agreement, −4 to +6) compared with −7 (95% limits of agreement, −18 to +5; P < .001) between the Landolt C and alphabet charts.
Conclusions and Relevance
The repeatability coefficients and concordance correlation coefficients suggest that ETDRS number charts are viable for measuring BCVA in clinical practice and trials for individuals who are unfamiliar with the Roman alphabet.
This cross-sectional study evaluates the repeatability and agreement of best-corrected visual acuity using the Early Treatment Diabetic Retinopathy Study number chart or Landolt C chart compared with the Early Treatment Diabetic Retinopathy Study alphabet chart in healthy and diseased eyes.
Key Points
Question
How does best-corrected visual acuity measured with a commercially available Early Treatment Diabetic Retinopathy Study (ETDRS) number chart compare with the ETDRS Roman alphabet chart?
Findings
In this cross-sectional study, the ETDRS number chart had high repeatability and very good agreement with the alphabet chart. Compared with the ETDRS Landolt C chart, the ETDRS number chart provided a higher agreement with the alphabet chart and shorter testing duration.
Meaning
The ETDRS number chart can be used to measure best-corrected visual acuity in clinical practice when needed and in clinical trials for individuals who are not familiar with Roman alphabets, with good repeatability and agreement with the ETDRS alphabet chart.
Introduction
Early Treatment Diabetic Retinopathy Study (ETDRS) visual acuity (VA) charts, modified from Bailey-Lovie charts, are often used to measure best-corrected VA (BCVA) owing to their high repeatability and accuracy. However, these charts cannot be used in individuals who are unfamiliar with Roman alphabets. The ETDRS Landolt C chart, Tumbling E chart, and automated Landolt C chart are alternatives with proven repeatability and agreement; however, they may not reflect true BCVA in individuals with confusion between left and right.
An ETDRS number chart is available, but, to our knowledge, its repeatability and agreement with the alphabet ETDRS chart is unknown. Therefore, we evaluated the repeatability and agreement of BCVA using ETDRS number charts and ETDRS Landolt C charts compared with ETDRS alphabet charts in eyes with normal and reduced VA.
Methods
This cross-sectional study was conducted at Chiang Mai University Hospital, Chiang Mai, Thailand, from July 1, 2015, to June 30, 2016. Adult Thai volunteers with at least a secondary school education who passed a screening test of the Roman alphabet were invited to participate. At screening, BCVA measurements were performed following a standardized refraction protocol, with only 1 study eye per participant, followed by a complete eye examination. If both eyes were eligible, the right eye was the study eye. The study was approved by the Research Ethics Committee, Faculty of Medicine, Chiang Mai University, and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from each study participant.
Participants were classified into the following 4 groups: group A, which comprised 60 healthy eyes with normal vision (BCVA, 20/20-20/25); group B, which comprised 40 eyes with pathologic findings not judged clinically relevant due to age-related cataract, diabetic macular edema, or age-related macular degeneration (BCVA, 20/20-20/40); group C, which comprised 40 diseased eyes due to age-related cataract, diabetic macular edema, or age-related macular degeneration (BCVA, 20/50-20/100); and group D, which comprised 14 diseased eyes due to age-related cataract, diabetic macular edema, or age-related macular degeneration (BCVA, 20/125-20/200). Eyes with age-related cataract, diabetic macular edema, or age-related macular degeneration were recruited in a ratio of 2:1:1 for groups B, C, and D.
Participants underwent standardized 4-m BCVA measurements after standardized refraction using 3 types of ETDRS charts (Precision Vision), including a PV number chart (No. 2702A), Landolt C chart (No. 2210), and Roman alphabet chart (No. 2111), in 2 rounds in random sequence, with at least 30 minutes between the first and second round and at least 2 minutes between charts. Participants were asked to read as many optotypes as possible. They either stopped reading when they could not read anymore, or the technician asked them to stop when they made 5 incorrect answers in a row. Each optotype of each chart could be read only once. The 3 chart measurements were performed and recorded by a single technician in the same testing room with similar lighting conditions. The ETDRS letter scores and testing durations of each participant were recorded.
Repeatability between the first and second round of each ETDRS chart among participants with impaired VA and those in group A was measured by Pearson correlation coefficients. Agreement among the 3 types of charts was assessed using intraclass correlation coefficients, which were compared using the F test. Owing to dependency and nonnormal distribution of the letter scores, differences in letter scores between charts were compared using Wilcoxon signed rank tests. Differences in testing duration were explored using the Friedman test. All statistical analyses were performed in R, version 3.2.4 (R Foundation for Statistical Computing). P values were 2-sided. No P value was considered statistically significant as there was no a priori correction for multiple analyses.
Results
A total of 154 participants (82 women and 72 men; 154 eyes; mean [SD] age, 52.9 [18.2] years) enrolled in the study. Eye conditions included age-related cataract (46 eyes [29.9%]), diabetic macular edema (27 eyes [17.5%]), and age-related macular degeneration (21 eyes [13.6%]), as well as 60 healthy eyes (39.0%).
Repeatability
The ETDRS number chart repeatability coefficients were 0.61 (95% CI, 0.42-0.75) for group A, 0.87 (95% CI, 0.78-0.93) for group B, 0.81 (95% CI, 0.67-0.90) for group C, and 0.81 (95% CI, 0.49-0.94) for group D. The ETDRS Landolt C chart and ETDRS alphabet chart had strong repeatability coefficients (Table 1).
Table 1. Repeatability Coefficients of ETDRS Letter Scores Across 3 Charts in Each Subgroup.
| ETDRS Chart Type | Group A (BCVA, 20/20-20/25) | Group B (BCVA, 20/20-20/40)a | Group C (BCVA, 20/50-20/100)a | Group D (BCVA, 20/125-20/200)a | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First Test | Second Test | Repeatability (95% CI)b | First Test | Second Test | Repeatability (95% CI)b | First Test | Second Test | Repeatability (95% CI)b | First Test | Second Test | Repeatability (95% CI)b | |
| Number | 87.1 | 87.8 | 0.61 (0.42-0.75) | 77.1 | 78.4 | 0.87 (0.78-0.93) | 58.1 | 59.5 | 0.81 (0.67-0.90) | 38.9 | 42.4 | 0.81 (0.49-0.94) |
| Landolt C | 80.9 | 82.1 | 0.73 (0.59-0.83) | 68.9 | 70.0 | 0.87 (0.77-0.93) | 49.3 | 50.3 | 0.85 (0.73-0.92) | 33.0 | 35.1 | 0.91 (0.73-0.97) |
| Alphabet | 85.8 | 86.8 | 0.7 (0.54-0.81) | 76.9 | 77.2 | 0.92 (0.78-0.93) | 57.3 | 58.4 | 0.88 (0.79-0.94) | 40.3 | 40.6 | 0.93 (0.78-0.98) |
Abbreviations: BCVA, best-corrected visual acuity; ETDRS, Early Treatment Diabetic Retinopathy Study.
Individuals with sight-threatening conditions including age-related cataract, diabetic macular edema, and age-related macular degeneration.
Repeatability coefficients were analyzed using Pearson correlation coefficient (interpretation: 00-0.19, very weak; 0.20-0.39, weak; 0.40-0.59, moderate; 0.60-0.79, strong; and 0.80-1.00, very strong).
Agreement With Alphabet Chart
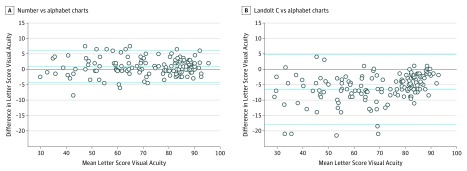
Concordance correlation coefficients between the ETDRS number and alphabet charts were strong (group A, 0.89 [95% CI, 0.82-0.93]; group B, 0.97 [95% CI, 0.94-0.98]; group C, 0.92 [95% CI, 0.86-0.96]; and group D, 0.96 [95% CI, 0.87-0.99]). Concordance correlation coefficients between the ETDRS Landolt C and alphabet charts were also strong (group A, 0.72 [95% CI, 0.52-0.83]; group B, 0.83 [95% CI, 0.68-0.91]; group C, 0.79 [95% CI, 0.61-0.89]; and group D, 0.89 [95% CI, 0.66-0.97]). Agreement between number and alphabet charts was higher than agreement between the Landolt C and alphabet charts in all ocular conditions and all VA subgroups but group D (Table 2 and Table 3). Overall, the mean VA difference between the number and alphabet charts (1 letter [95% limits of agreement, −4 to +6 letters]) was smaller than the mean difference between the Landolt C and alphabet charts (−7 letters [95% limits of agreement, −18 to +5 letters]; P < .001) (Figure).
Table 2. Agreement and Differences in BCVA Letter Score: Number or Landolt C Charts vs Alphabet Charts.
| ETDRS Chart Type | Concordance Correlation Coefficient (95% CI)a | Difference in Letter Scores (95% CI)b | ||||||
|---|---|---|---|---|---|---|---|---|
| Group A (20/20-20/25) | Group B (20/20-20/40) | Group C (20/50-20/100) | Group D (20/125-20/200) | Group A (20/20-20/25) | Group B (20/20-20/40) | Group C (20/50-20/100) | Group D (20/125-20/200) | |
| Number vs alphabet | 0.89 (0.82 to 0.93) | 0.97 (0.94 to 0.98) | 0.92 (0.86 to 0.96) | 0.96 (0.87 to 0.99) | 1.16 (−2.98 to 5.29) | 0.70 (−3.96 to 5.36) | 0.94 (−6.17 to 8.05) | 0.21 (−4.98 to 5.41) |
| Landolt C vs alphabet | 0.72 (0.52 to 0.83) | 0.83 (0.68 to 0.91) | 0.79 (0.61 to 0.89) | 0.89 (0.66 to 0.97) | −4.80 (−13.5 to 3.91) | −7.56 (−20.12 to 5.00) | −8.04 (−21.33 to 5.26) | −6.36 (−14.07 to 1.35) |
| P valuec | .003 | <.001 | .01 | .11 | <.001 | <.001 | <.001 | .001 |
Abbreviations: BCVA, best-corrected visual acuity; ETDRS, Early Treatment Diabetic Retinopathy Study.
Concordance correlation coefficients were calculated from intraclass correlation (interpretation: <0.40, poor; 0.40-0.59, fair; 0.60-0.74, good; and 0.75-1.00, excellent).
Negative sign indicated that the ETDRS letter scores were less than those measured with the alphabet chart.
P values for the differences in agreement (intraclass correlation coefficients) were calculated using the F test, and the P values for the differences in letter scores across charts were calculated using the Wilcoxon signed rank test.
Table 3. Agreement and Differences in BCVA Letter Score: Number or Landolt C Charts vs Alphabet Charts.
| ETDRS Chart Type | Concordance Correlation Coefficient (95% CI)a | Difference in Letter Scores (95% CI)b | ||||||
|---|---|---|---|---|---|---|---|---|
| Healthy Eyes | Cataract | AMD | DME | Healthy Eyes | Cataract | AMD | DME | |
| Number vs alphabet | 0.89 (0.82 to 0.93) | 0.99 (0.98 to 1.00) | 0.99 (0.97 to 1.00) | 0.99 (0.98 to 1.00) | 1.16 (−2.98 to 5.29) | 0.21 (−5.61 to 6.02) | 2.10 (−3.86 to 8.06) | 0.51 (−4.95 to 5.99) |
| Landolt C vs alphabet | 0.72 (0.52 to 0.83) | 0.95 (0.91 to 0.97) | 0.99 (0.97 to 1.00) | 0.96 (0.90 to 0.98) | −4.80 (−13.5 to 3.91) | −8.56 (−22.94 to 5.81) | −4.90 (−10.82 to 1.02) | −7.98 (−19.09 to 3.13) |
| P valuec | .003 | .34 | >.99 | .46 | <.001 | <.001 | <.001 | <.001 |
Abbreviations: AMD, age-related macular degeneration; BCVA, best-corrected visual acuity; DME, diabetic macular edema; ETDRS, Early Treatment Diabetic Retinopathy Study.
Concordance correlation coefficients were calculated from intraclass correlation (interpretation: <0.40, poor; 0.40-0.59, fair; 0.60-0.74, good; and 0.75-1.00, excellent).
Negative sign indicated that the ETDRS letter scores were less than those measured with the alphabet chart.
P values for the differences in agreement (intraclass correlation coefficients) were calculated using the F test, and the P values for the differences in letter scores across charts were calculated using the Wilcoxon signed rank test.
Figure. Difference in Letter Score Acuity Comparing Number vs Alphabet Charts and Landolt C vs Alphabet Charts.
A, Bland-Altman plot showing the mean letter score difference between the number and alphabet charts. B, Bland-Altman plot showing the mean letter score difference between the Landolt C and alphabet charts. The mean difference between the number and alphabet charts is smaller than the mean difference between the Landolt C and alphabet charts. The middle horizontal dashed line represents the mean letter score difference, while the dashed lines at the top and the bottom represent the 95% CI.
Testing Duration
In group A, the testing duration with the Landolt C chart was 1.6 times longer than with the alphabet chart and 2 times longer than with the number chart. In groups B through D, on average, the testing duration with the Landolt C chart was 1.6 times longer than with the alphabet chart and 1.7 times longer than with the number chart (Table 4).
Table 4. Testing Durations Across 3 Charts in Each Subgroup.
| ETDRS Chart Type | Testing Duration, s | |||||||
|---|---|---|---|---|---|---|---|---|
| Group A (BCVA, 20/20-20/25) | Group B (BCVA, 20/20-20/40)a | Group C (BCVA, 20/50-20/100)a | Group D (BCVA, 20/125-20/200)a | |||||
| First Test | Second Test | First Test | Second Test | First Test | Second Test | First Test | Second Test | |
| Number | 33 | 33 | 38 | 36 | 37 | 37 | 51 | 43 |
| Landolt C | 58 | 53 | 64 | 61 | 76 | 66 | 74 | 73 |
| Alphabet | 39 | 37 | 41 | 41 | 42 | 42 | 48 | 52 |
| P valueb | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | .001 | .002 |
Abbreviations: BCVA, best-corrected visual acuity; ETDRS, Early Treatment Diabetic Retinopathy Study.
Individuals with sight-threatening conditions including age-related cataract, diabetic macular edema, and age-related macular degeneration.
Testing durations were calculated using the Friedman test.
Discussion
These results suggest that commercially available ETDRS number charts (PV number Precision Vision chart) provide high repeatability coefficients and excellent agreement with ETDRS alphabet charts. For the ETDRS Landolt C and alphabet charts, although this study found excellent agreement as previously reported, such agreement between the Landolt C and the alphabet charts was lower than agreement between the number and alphabet charts in all but group D (BCVA, 20/125-20/200). The small sample size of this latter subgroup may have made it less likely to detect a true difference between charts.
Discrepancies of VA scores between the Landolt C and the alphabet charts was reported previously. Treacy et al reported a 1-line difference between VA obtained from the Landolt C chart and an ETDRS alphabet chart. Kuo et al found a 4-line difference in VA between the Landolt C and the alphabet charts, especially in eyes with maculopathy and VA of 20/200 or less. Our study found a mean difference of 7 letters (approximately 1.5-line difference) between the ETDRS Landolt C and alphabet charts (mean difference, −7 letters [95% limits of agreement, −18 to +5 letters]). This outcome was a relatively larger difference compared with the smaller mean difference between the number and alphabet charts (1 letter [95% limits of agreement, −4 to +6 letters]; P < .001). This finding suggests the potential superiority of the ETDRS number chart for individuals who are not familiar with Roman alphabets used in clinical trials. Visual acuity scores obtained from these 2 charts might be pooled in future trials, and some adjustment of VA scores obtained from the ETDRS Landolt C chart (eg, 7 letters) might be needed for pooled analyses.
The longer testing duration with the Landolt C chart was consistent with a previous report. Testing duration with number charts was the shortest, perhaps owing to the design of number optotypes, which are relatively easier to identify compared with the Sloan letter chart or Landolt C chart, or owing to familiarity of number charts among Thai individuals because Snellen charts with number optotypes are used widely in Thailand.
Limitations
This study has some limitations, including the small number of participants in group D. Also, number chart results might be different among individuals who are not familiar with alphabet charts.
Conclusions
These results suggest that the ETDRS number chart gives high repeatability and very good agreement with the original ETDRS alphabet chart. Compared with the ETDRS Landolt C chart, the ETDRS number chart provided better agreement with the ETDRS alphabet chart with shorter testing duration in those with or without VA loss. These findings suggest that the ETDRS number chart can measure VA reliably in clinical trials, including regions in which most people are not familiar with the Roman alphabet. However, for illiterate individuals, the Landolt C chart may still be used to measure VA.
References
- 1.Bailey IL, Lovie JE. New design principles for visual acuity letter charts. Am J Optom Physiol Opt. 1976;53(11):740-745. [DOI] [PubMed] [Google Scholar]
- 2.Ferris FL III, Bailey I. Standardizing the measurement of visual acuity for clinical research studies: guidelines from the Eye Care Technology Forum. Ophthalmology. 1996;103(1):181-182. [DOI] [PubMed] [Google Scholar]
- 3.Ferris FL III, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94(1):91-96. [PubMed] [Google Scholar]
- 4.Ferris FL III, Sperduto RD. Standardized illumination for visual acuity testing in clinical research. Am J Ophthalmol. 1982;94(1):97-98. [DOI] [PubMed] [Google Scholar]
- 5.Kuo HK, Kuo MT, Tiong IS, Wu PC, Chen YJ, Chen CH. Visual acuity as measured with Landolt C chart and Early Treatment of Diabetic Retinopathy Study (ETDRS) chart. Graefes Arch Clin Exp Ophthalmol. 2011;249(4):601-605. [DOI] [PubMed] [Google Scholar]
- 6.Koenig S, Tonagel F, Schiefer U, Bach M, Heinrich SP. Assessing visual acuity across five disease types: ETDRS charts are faster with clinical outcome comparable to Landolt Cs. Graefes Arch Clin Exp Ophthalmol. 2014;252(7):1093-1099. [DOI] [PubMed] [Google Scholar]
- 7.Treacy MP, Hurst TP, Conway M, et al. The Early Treatment in Diabetic Retinopathy study chart compared with the Tumbling-E and Landolt-C. Ophthalmology. 2015;122(5):1062-1063.e1. [DOI] [PubMed] [Google Scholar]
- 8.Ruamviboonsuk P, Tiensuwan M, Kunawut C, Masayaanon P. Repeatability of an automated Landolt C test, compared with the Early Treatment of Diabetic Retinopathy Study (ETDRS) chart testing. Am J Ophthalmol. 2003;136(4):662-669. [DOI] [PubMed] [Google Scholar]
- 9.National Research Council Committee on Vision Recommended standard procedures for the clinical measurement and specification of visual acuity: report of working group 39: committee on vision: Assembly of Behavioral and Social Sciences, National Research Council, National Academy of Sciences, Washington, DC. Adv Ophthalmol. 1980;41:103-148. [PubMed] [Google Scholar]
- 10.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. [DOI] [PubMed] [Google Scholar]